![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
Newborn or neonate ages
|
Birth to 28 days
|
|
|
Infant ages
|
Under the age of 1
|
|
|
Term infant gestation length
|
37-42 weeks
|
|
|
Preterm infant gestation length
|
Less than 37 weeks
|
|
|
Postterm infant gestation length
|
More than 42 weeks
|
|
|
Macrosomia
|
Abnormally large size of the body of the neonate.
|
|
|
Normal birth weight
|
2500 g or more, about 5.2 lbs
|
|
|
Low birth weight
|
Less than 2500 g
|
|
|
Very low birth weight
|
Less than 1500 g
|
|
|
Gestational age
|
Age of the fetus or newborn based upon the completed weeks from the date of the mother's last menstrual period (LMP).
|
|
|
What percentile is considered small or large for gestational age?
|
Weight, length or head circumference:
Small - less than 10% percentile Large - more than 90% percentile |
|
|
What is an APGAR score?
|
Scoring system comprised of five elements (Appearance, Pulse, Grimace, Activity, Respiration) that serves as a rapid method of assessing the clinical status of an infant immediately after birth.
|
|
|
Prophylactic erythromycin
|
Applied to eyes within one hour of birth to prevent gonococcal ophthalmia.
|
|
|
Vitamin K
|
Administered within 4 hours, 1 mg IM or SQ to prevent hemorrhagic disease.
|
|
|
Hepatitis B vaccine
|
Administered to newborn before 12 hours of age.
If mother is Hep B positive, Hep B vaccine and Hep B immune globulin are both administered. |
|
|
When should newborn screenings be performed?
|
At 24-28 hours after birth.
|
|
|
How often should a newborn be bathed?
|
Three times weekly is sufficient.
|
|
|
How should one care for an umbilical stump?
|
Keep clean and dry until it shrivels and falls off, usually within 1-2 weeks of birth. Sponge baths only until then.
|
|
|
Omphalitis
|
Umbilical stump infection includes foul-smelling, yellowish discharge, redness around base, crying when cord or skin is touched.
|
|
|
What is circumcision?
|
Removal of the foreskin from the penis. Elective procedure only to be performed on healthy, stable infants.
|
|
|
What are the benefits of circumcision?
|
Decreased rates of UTIs in first year, foreskin abnormalities, risk of STIs (HIV, HPV, HSV, BV), penile cancer and improved hygiene.
|
|
|
Phimosis
|
Inability to retract foreskin over the glans.
|
|
|
Paraphimosis
|
Entrapment of retracted foreskin.
|
|
|
Balanoposthitis
|
Inflammation of foreskin and glans.
|
|
|
What are the risks of circumcision?
|
Local infection, bleeding, removal of too much skin, urethral injury.
Contraindicated in infants with genital abnormalities. |
|
|
How do you care for a circumcision?
|
Takes about 7 – 10 days to heal
Apply small amount of Vaseline to gauze and change with every diaper change. Stool on penis-cleanse area with warm soapy water. Give sponge baths until circumcision is healed. After circumcision is healed, gently pull foreskin back at bath time to prevent it from adhering to the glans |
|
|
What is an appropriate weight loss after birth?
|
About 5-7% in the first few days of life.
|
|
|
Weight gain guidelines
|
Baby should regain birth weight 2 weeks after birth.
Appropriate weight gain is 1 ounce/day for the first 6 months and .5 ounce/day for the next 6 months. As a general rule, infants should triple their birth weight by their 1st birthday. |
|
|
AAP follow-up visit guidelines
|
Visit should occur within 48-72 hours for newborns discharged before 49 hours of age.
|
|
|
Subconjunctival Hemorrhage
|

Breakage of small blood vessels in the eyes of a newborn.
One or both eyes may have a bright band around the iris. Causes: traumatic delivery, spontaneous, occasionally results from severe sneezing or coughing. Rarely due to blood dyscrasia. Resolves within 1-2 weeks without any permanent damage to the eye (or eyes). |
|
|
Milia
|

Very common, benign, keratin-filled cysts that appear as superficial pearly white to yellow domed papules measuring 1-2 mm in diameter.
Usually on the face, especially the nose. Spontaneously disappear within the first few weeks of life. |
|
|
Epstein pearls
|

Milia that are located intraoral.
Small, pearly nodules along the midline of the hard palate and are benign retention cysts. |
|
|
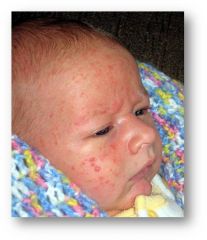
Erythema Toxicum
|

Most common neonatal skin lesion.
May occur anytime during the first week of life but most commonly presents on the second and third days. 1-2 mm white to yellowish papules/pustules on an erythematous base. Found on chest, arms, legs and back. Generally disappears within the 2 - 4 weeks of life. |
|
|
Mongolian spots
|

Areas (macules) of blue to slate gray discoloration due to uneven migration of melanocytes, resemble bruise.
Usually found on base of spine and buttocks. Affects >50% of African American, Native American and Asian infants. Most fade within 2-3 years but can persist for life. |
|
|
Nevus simplex
|

“Salmon patch” or “stork bite”
Pink-red capillary malformations found on neck, eyes, forehead or upper lip. Most fade and disappear by age 2. If persist into adolescence, they may be treated with laser therapy. |
|
|
Nevus Flammeus
|

Port-Wine Stain
Macular, sharply circumscribed, pink to purple lesions. These are vascular malformations consisting of mature, dilated dermal capillaries and represent a permanent developmental defect. Most common regions are head and neck. |
|
|
Neonatal Cephalic Pustulosis
|
Baby acne
Inflammatory papules or pustules, absence of comedomes. Generally limited to the face. Onset at 3 weeks and generally resolves around 4 months. No treatment necessary but may use soap and water, 1% hydrocortisone or 2% ketoconazole. Avoid oils and lotions. |
|
|
Lacrimal duct obstruction
|
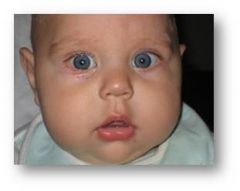
Obstruction in any part of the drainage system.
Commonly due to incomplete canalization of the duct or membranous obstructions. Risk factors include craniofacial abnormalities and amniotic band syndrome. Occurs in up to 6% of infants. Signs and symptoms include wet eye with mucoid drainage, erythema of one or both lids and conjunctivitis. |
|
|
Treatment of lacrimal duct obstruction
|
Most cases clear spontaneously but refer to opthalmologist if persists after 6 months.
Nasolacrimal massage Mainstay of surgical treatment is probing. |
|
|
Colic
|
Characterized by severe and paroxysmal crying that occurs mainly in the late afternoon.
Begins in first few weeks of life and peaks at age 2-3 months. |
|
|
Rule of Threes of Colic
|
Wessel Criteria
Infant who is healthy and well fed but cries for more than 3 hours a day, for more than 3 days per week, and for more than 3 weeks. |
|
|
Other criteria for colic
|
In addition to Wessel criteria some suggest that dx should meet three of four of the additional criteria:
Paroxysmal Qualitatively different from normal crying Associated with hypertonia Inconsolability |
|
|
Proposed etiologies of colic
|
GI: cow’s milk protein, lactose intolerance, immaturity, intestinal motility, fecal microflora
Biologic: feeding technique, motor regulation, increased serotonin, tobacco exposure Psychosocial: temperament, hypersensitivity, parental variables |
|
|
Evaluation of colic
|
During an episode infant will have knees drawn up, fists clenched, flatus may be expelled, faces appear pained and there is minimal response to soothing.
Assess: - Stooling, urination and sleeping patterns - Growth pattern - Social situation and parent-infant interactions |
|
|
Questions to ask the family regarding colic
|
When does crying occur and how long does it last?
What do you do when the baby cries? What does the cry sound like? Pain, hunger? How and what do you feed the baby? How does it make you feel when the baby cries? How has colic affected your family? What is your theory on why the baby cries? |
|
|
Management of colic
|
Educate parents about developmental characteristics of crying behavior.
Reassure the parents. Track crying patterns and weight gain. Strategies for soothing and comforting the infant. Create quiet environment w/o excessive handling. Alternate sensory stimulation such as swinging, rocking, soft music, drives in the car, warm bath, belly massage. If refractory to behavioral management, trial of hypoallergenic diet. Sedatives, antihistamines, and motion sickness medications (dicyclomine) are not safe or effective for colic treatment. - Dicyclomine can cause breathing cessation, seizures and coma. |
|
|
Neonatal jaundice
|
Yellowing of the skin, sclera and mucus membranes due to elevated bilirubin levels.
Common neonatal problem. 65% of newborns develop clinical jaundice (bilirubin >5 mg/dL) during the first week of life. 1-2% of infants have total serum bilirubin >20 mg/dL. |
|
|
How is bilirubin metabolized?
|
In the lymph nodes and spleen, heme is metabolized into iron (conserved) and carbon monoxide (exhaled).
Biliverdin - Metabolized to unconjugated bilirubin Unconjugated bilirubin is then bound to albumin and is carried to the liver where it is conjugated with two glucuronide molecules. Conjugated bilirubin is then excreted through the bile into the intestine and in the presence of normal gut flora, is excreted in the stool. If stool is not passed, conjugated bilirubin reabsorbed. Unconjugated bilirubin = indirect bilirubin Conjugated bilirubin = direct bilirubin |
|
|
What causes physiologic jaundice?
|
Absent gut flora and slowed peristalsis (as in the first few days of life) causes conjugated bilirubin to remain in the intestinal lumen rather than being readily excreted.
Due to stasis, much of the conjugated bilirubin in the intestinal lumen is hydrolyzed back to unconjugated bilirubin by an enzyme present in the intestinal mucosa. The unconjugated bilirubin is then reabsorbed into the blood stream via enterohepatic circulation, adding an additional bilirubin load to the already overstressed liver of the neonate. |
|
|
Physiologic jaundice
|

Physiologic jaundice is visible jaundice appearing after 24 hours of age.
If jaundice apparent before 24 hours it is pathologic in origin! Total bilirubin increases by <5 mg/dL per day. Peak bilirubin occurs at 3–5 days of age, with a total bilirubin of no more than 15 mg/dL. Visible jaundice resolves by 1 week in the full-term infant and by 2 weeks in the preterm infant. |
|
|
Causes of increased bilirubin production
|
Labs show elevated reticulocyte count.
Increased rate of hemolysis Presence of maternal antibodies against fetal cells (Coombs test-positive) ABO incompatibility, Rh incompatibility Abnormal RBC shape Spherocytosis Abnormal RBC enzymes G6PD deficiency, pyruvate kinase deficiency Nonhemolytic causes Extravascular hemorrhage, polycythemia, exaggerated enterohepatic circulation of bilirubin |
|
|
Breast-feeding jaundice
|
Breast feeding-associated jaundice
“Lack of breast milk jaundice” Primarily due to decreased nutritional intake combined with increased enterohepatic circulation. |
|
|
Acute Bilirubin Encephalopathy
|
Lethargy, hypotonia, poor sucking progressing to hypertonia, irritability, backward arching of the neck (retrocolis) and the trunk (opisthotonos).
|
|
|
Chronic Bilirubin Encephalopathy
|
(Kernicterus) – yellow staining and degenerative lesions in basal ganglia associated with high levels of unconjugated bilirubin in infants.
Consequences include cerebral palsy, deafness, limitation of upward gaze and dental dysplasia. |
|
|
Risk factors of jaundice
|
Pre discharge TSB or TcB in the high risk zone
Jaundice observed in the first 24 hours Blood group incompatibility Gestational age 35 – 36 weeks Previous sibling received phototherapy Cephalohematoma (or significant bruising) Exclusively breast feeding, particularly if nursing is not going well and weight loss excessive East Asian race |
|
|
Evaluation of jaundice
|
Feeding and elimination history
Weight (and comparison with birth weight) Blood type Direct Coomb’s testing CBC with smear Serum albumin Total bilirubin Clinical jaundice appears at bilirubin levels of 5mg/dL. Appears first on the head, progressing down the chest and abdomen as the level increases. If distal extremities affected, level is likely to be at least 15 mg/dL. |
|
|
Phototherapy
|
Used most commonly to treat jaundice.
Light is absorbed by unconjugated bilirubin in the skin converting it to water soluble compound that can be excreted in the bile without conjugation. Decreases or blunts the amount of total bilirubin regardless of the rise of TB, patient’s ethnicity or etiology of hyperbilirubinemia. |
|
|
Treatment of jaundice
|
When should phototherapy be initiated?
If TSB 40 – 75%ile: Recheck level in 48 hours. If TSB 75 – 95%ile: Recheck level next day. If > 95%ile: Start phototherapy and follow level every 6 hours. For TSB levels ≥ 20 mg/dL phototherapy should be administered continuously, until the TSB falls below 20 mg/dL. |
|
|
Exchange transfusion
|
Rarely needed to treat jaundice
Necessary in some cases of ABO incompatibility, Rh isoimmunization, Hereditary spherocytosis *Protoporphyrins – inhibitors of heme oxygenase, an enzyme that initiates heme catabolism. Currently not approved for use in the U.S. |
|
|
Jaundice pearls
|
Most common causes of unconjugated hyperbilirubinemia are physiologic jaundice, prematurity and breast feeding-associated jaundice.
Infants with clinical jaundice within the first 24 hours most likely have a pathologic cause. Kernicterus is yellow staining and degenerative lesions in basal ganglia associated with high levels of unconjugated bilirubin in infants. It is synonymous with chronic bilirubin encephalopathy and can lead to cerebral palsy and deafness. Phototherapy is the most commonly used intervention to treat and prevent severe hyperbilirubinemia. |
|
|
When should the APGAR be completed?
|
At 1, 5 and 10 minutes
|
|
|
How is Activity (muscle tone) scored on the APGAR?
|
0 points - activity absent
1 point - arms and legs flexed 2 points - active movement |
|
|
How is Pulse scored on the APGAR?
|
0 points - absent pulse
1 point - <100 bpm 2 points - >100 bpm |
|
|
How is Grimace (reflex irritability) scored on the APGAR?
|
0 points - no response
1 point - grimace 2 points - sneezes, coughs, pulls away |
|
|
How is Appearance (skin color) scored on the APGAR?
|
0 points - blue-gray, pale all over
1 point - pink, except extremities 2 points - pink all over |
|
|
How is Respiration scored on the APGAR?
|
0 points - absent respiration
1 point - slow, irregular 2 points - good, crying |
|
|
What are some possible causes of a newborn being small for its gestational age?
|
Maternal drug use
Chromosomal abnormalities Exposure to intrauterine viral infection Multiple gestation Advanced maternal age (>35 years old) Placental insufficiency Lack of maternal weight gain |
|
|
What are some possible causes of a newborn being large for its gestational age?
|
Most commonly large size is due to gestational diabetes.
|
|
|
When should a newborn exam be completed?
|
Within 24 hours of birth.
|
|
|
Fontanelles
|
Anterior - 1-4 cm
- closes around 4-26 months Posterior - 1 cm in size - closes around 1-3 months |
|
|
What are the most common causes of unconjugated hyperbilirubinemia?
|
Physiologic jaundice, prematurity and breast-feeding jaundice
|
|
|
Etiology of neonatal jaundice
|
Overproduction of bilirubin
Decreased rate of conjugation |
|
|
At what bilirubin levels can kernicterus result?
|
Toxicity begins at levels greater than 20-25 mg/dL
|
|
|
Complications of jaundice
|
Kernicterus can result and may cause encephalopathy, mental retardation or death.
|
|
|
When does neonatal jaundice peak?
|
Total bilirubin increases by <5 mg/dL per day.
Peak bilirubin occurs at 3–5 days of age, with a total bilirubin of no more than 15 mg/dL. |

