![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
135 Cards in this Set
- Front
- Back
|
What is included in a neurovascular assessment?
|
- Assess for pain: * Assess pain level * Use an age appropriate rating scale, and have the child describe the pain
- Assess sensation: * Assess for numbness or a tingling sensation * Loss of sensation may indicate nerve damage
- Assess skin temperature: * Assess the extremity for temperature - should be warm, NOT COOL to the touch
- Assess skin color: * Assess the color * Check distal to the injury, check for changes in pigmentation
- Assess capillary refill: * Place pressure on nail beds of the affected extremity until blanching occurs (should be 3 seconds)
- Assess pulses: * Pulses should be palpable and strong - pulses should be equal to the pulses of the unaffected extremity
- Assess movement: * The child should be able to move the affected extremity in passive motion |
|
|
How would the nurse instruct the client to treat a sprain? |
- R: rest - I: ice - C: compress (ACE bandage) - E: elevate |
|
|
What causes juvenille rheumatoid arthritis? |
- Susceptible individuals who have an autoimmune response to internal or external triggers |
|
|
What is the priority of care for a child with leukemia? |
- Protect the child from infection! - Reverse isolation |
|
|
What are the signs and symptoms of rheumatic fever? What is the treatment? |
- Rheumatic fever: an inflammatory disease that occurs as a reaction to Group A-B hemolytic streptococcus (GABHS) infection of the throat
- Signs and symptoms: * History of recent upper respiratory infection * Fever * Fatigue * Sore throat * Tachycardia * Large joints (knees, ankles, wrists and shoulders) |
|
|
What is Kawasaki's disease? How is it treated? |
- Kawasaki's disease: a febrile multisystem disorder, resulting in inflammation of blood vessels (vasculitis) - Usually occurs in children under 5 years
- Signs and symptoms: * A high, spiking fever over 102.2 that persists for 5 days or longer * Strawberry tongue * Cracked dry lips * Edema of hands and feet, erythema * Elevated ESR
- Treatment: * Anti-inflammatory medications (ASPIRIN, gamma globulin - IVIG)
- Nursing care: * Frequent and gentle oral care * Promote comfort and cool baths * Small, frequent feedings * Skin care |
|
|
What are the symptoms of hemophilia? Which lab test is usually abnormal in a child with hemophilia? |
- Hemophilia: a disorder that results in impaired ability to control bleeding, bleeding time is extended due to lack of clotting factors, bleeding may be internal or external
- Symptoms: * Episodes of bleeding, excessive bleeding, reports of joint pain and stiffness, impaired mobility, and activity tolerance * Active bleeding, which includes bleeding gums, epistaxis, hematuria and/or tarry stools * Hematomas and/or bruising * Hemarthrosis as evidenced by joint pain, stiffness, warmth, swelling, redness, loss of range of motion and deformities
- Lab tests: * Patient will have a PROLONGED partial thromboplastic time |
|
|
What is a vaso-occlusive crisis? |
- Vaso-occlusive crisis is a painful episode resulting from ischemia - Usually lasts 4-6 days |
|
|
Whats are the signs and symptoms of a acute vaso-occlusive crisis, and a chronic vaso-occlusive crisis? |
- Acute: * Severe abdominal pain * Hematuria * Swollen and extremely painful joints
- Chronic: * Increased risk of respiratory infections and/or osteomyelitis * Retinal detachment * Blindness * Seizures |
|
|
What teaching should be given to the sickel cell anemia patient to prevent a future vaso-occlusive crisis? |
- Advise families of the importance of promoting rest - Advise families the importance of promoting adequate nutrition for their child - Give specific directions regarding fluid intake requirements, such as how many bottles, glasses, or fluids should be consumed daily - Instruct families to identify signs and symptoms of a vaso-occlusive crisis and infection |
|
|
What is developmental hip dysplasia? |
- Developmental hip dysplasia is also known as congenital hip dysplasia - May be affected by family history, gender, birth order, intrauterine position, and/or laxity of a joint |
|
|
What is the subjective and objective data the nurse will assess in a child with congenital hip dysplasia (developmental dysplasia of the hip)? |
- Asymmetrical gluteal thigh folds - Limited abduction of the hips - One knee appears shorter
|
|
|
What tests are used to diagnose congenital hip dysplasia (developmenta dysplasia of the hip)? |
- For infants from birth to 3 months of age, the provider performs the Barlow and Ortolani tests (best done on a non-crying infant) - For children that are able to walk, observe postural gait - Assess for uneven skin folds |
|
|
What is a Palvik harness? |
- The most common treatment for congenital hip dysplasia in a child under 3 months of age - Can be used from birth up to 5 or 6 months of age - A noninvasive device used for keeping hips in an abducted position; allows the femoral head to remain in contact with the acetabulum
|
|
|
What discharge teaching would the nurse give parents about the caring for their child in a Palvik harness? |
- Advise parents, the infant will wear the harness CONTINUOUSLY for 3-5 months, until the hip is determined by radiograph to be stable - Advise parents that frequent follow-up will needed for strap adjustment - Advise parents a shirt should be worn under the harness to PREVENT skin irritation |
|
|
What is a hip sica used for? |
- A hip spica is used for children who are 6 months of age - A hip spica is used in children whose hips were not stabilized by the use of a Palvik harness - Short course of traction may be used PRIOR to the application of a spica cast - An infant will be in a hip spica cast most likely after surgery |
|
|
What is scoliosis characterized by? |
- Scoliosis is characterized by a lateral curvature of the spine and spinal rotation that causes rib asymmetry - Idiopathic or structural scoliosis is the most common form of scoliosis - Idiopathic scoliosis can be congenital, idiopathic or acquired as a result of neuromusuclar disorders - Idiopathic scoliosis may be present at birth or occur early in childhood, onset usually occurs during the preadolescent growth spurt |
|
|
What is the treatment for scoliosis? |
- Mild scoliosis (curvature of 10-20 degrees), is treated with BRACING and EXERCISE to maintain strength, and maintain muscles of the abdomen and spine |
|
|
What is a Milwaukee brace? And the discharge teaching for the brace? |
- A Milwaukee brace is used for patients who have MILD scloiosis (curvature of 10-20 degrees)
- Discharge teaching: * Reinforce to the parents, that the brace will NOT correct the curve, but will help to stabilize it until growth is completed * Suggest parents or thr adolescent to decorate the brace to encourage acceptance * Instruct the child and family of the importance of adherance * Instruct the child to wear the brace 23 out of 24 hours a day * Reinforce the need to exercise along with use of the brace * Educate the child and family of the importance of wearing a cotton shirt UNDER the brace, and to avoid the use of powders and lotions under the brace * Reinforce the need to assess for skin breakdown |
|
|
At what point is surgery needed for a child with scoliosis? |
- Surgery is generally needed for curves GREATER than 40 degrees |
|
|
What is juvenille rheumatoid arthritis (JIA)? |
- Juvenille rhuematoid arthritis includes: * Systemic arthritis * Oligoarthritis * Polyarthritis (with or without rheumatoid factor)
- No definitive diagnosis - Onset begins < 16 years of age - Symptoms will occur in 1 or more joints and last for 6 weeks or longer with no other cause identified - Peak incidence is between 1-3 years of age - JIA is rarely life threatening, may subside over time, but can result in residual joint deformities and altered joint function |
|
|
What is the subjective and objective data for a child with rheumatoid arthritis? |
- Joint swelling, stiffness, redness, warmth - Mobility limitations - Fever - Rash - Nodules under the skin - Delayed growth and development |
|
|
What is the nursing care for the child with juvenille rheumatoid arthritis? |
- Nursing care is primarily outpatient - Evaluate the child's pain and response to prescribed analgesics - Encourage the child to participate in a physical therapy program to increase mobility and prevent deformities - Teach parents to apply splints for nighttime sleep - Splints should be applied to the knees, wrists and hands to decrease pain and prevent flexion deformities - Apply heat, or warm moist packs to the child's affected joints prior to exercise - Encourage a well-balanced diet that is high in fiber, and contains adequate fluids to prevent constipation from immobility |
|
|
What is iridocyclitis/uveitis? |
- Inflammation of the iris and the ciliary body (you don't see this in adults, this is specific to juevenille rheumatoid arthritis) - Requires treatment by an opthalmologist |
|
|
What is muscular dystrophy? |
- The largest group of diseases that affects muscle function - Loss of muscular strength is progressive - Developmental milestones are likely to be met until the onset of the disease
- Duchenne (pseudohypertrophic) muscular dystrophy is the most common form of muscular dystrophy (DMD) - Inherited as an x-linked recessive trait - DMD has an onset between 3 and 7 years of age - Life expectancy with current technology for DMD reaches until early adulthood |
|
|
What is the subjective and objective data for a child who may have DMD? |
- Family reports of a delay in walking; changes in gait; difficulties with running, climbing stairs and riding a bike - Muscular weakness in lower extremities - Muscular hypertrophy, especially in calves - Mild delay in motor skill development - Mobility wth general muscle strength declining over time - Unsteady, wide-based or waddling gait, and loss of walking ability (usually by age 12) - Difficulty riding a tricycle, running and rising from a seated position (Gower maneuver) - Cardiovascular complications (associated with progression of DMD) - weight loss, increased fatigue during usual ADL's and orthopnea |
|
|
What lab tests are done to diagnose muscular dystrophy (MD)? |
- Lab tests: * DNA analysis using peripheral blood, serum polymerase chain reaction (PCR) from the dystropin gene mutation * Muscle tissue biopsy * Serum creatine phosphokinase (CK) will be ELEVATED * Electromyography (EMG) |
|
|
What is the nursing care for the child with muscular dystrophy? |
- Assess and monitor: * The child's ability to perform ADL's * The child's respiratory function, including depth, rhythm and rate of respirations during sleep and daytime hours * The child's cardiac function * The child and parent's understanding of long-term affects * The child and parent's coping and support * Mantain optimal physical function as long as possible * Encourage the child to be independent for as long as possible and to perform ADL's * Perform range of motion exercises * Encourage adequate fluid intake * Maintain respiratory functioning * Position the child to to enhance expansion of the lungs * Avoid skin breakdown by helping to reposition the child |
|
|
What is congenital heart disease (CHD)? |
- Anatomic defects of the heart prevent normal blood flow to the pulmonary and/or systemic system - Many defects will spontaneously close, but some will require surgical repair - Most children with CHD will be diagnosed within the 1st year of life, but certain children may not exhibit manifestations until later
- A congenital heart defect is one that develops in the womb and is present at birth - After birth, congenital heart defects can be broadly categorized into 2 groups: 1. Acacyanotic defetcs (pink babies) 2. Cyanotic heart defects (blue babies) |
|
|
What is a ventricular septal defect? |
- Hole between 2 ventricles - LEFT to RIGHT SHUNT: majority due to higher pressure in the LEFT ventricle - Dilated right heart: too much blood to the lungs, increase in pulmonary pressure
- Symptoms: * Loud, harsh murmur * Heart failure * Failure to thrive |
|
|
What is a atrial septal defect? |
- Hole between the 2 atria - Blood flows LEFT to RIGHT (shunting) - Right heart becomes dilates - Too much blood in the lungs
- Symptoms: * Loud, harsh, murmur * MILD heart failure * Poss. enlarged right atrium * Increased O2 saturation in RIGHT arium |
|
|
What is a patent ductus arteriosus? |
- PDA - Connective structure between the aorta and pulmonary artery - Normal fetal structure, allows blood to bypass circulation to the lungs (O2 provided by the placenta) - Normally closes 24 hours AFTER birth (few hours - 3 weeks) - Can correct several months AFTER birth - 6th most common defect
- Symptoms: * Murmur (machine hum) * Wide pulse pressure * Bounding pulse |
|
|
What does pulmonary stenosis mean? |
- Narrowing at the area around the pulmonary valve resulting in an obstruction that interferes with blood flow out of the RIGHT ventricle
- Symptoms: * Systolic ejection murmur * Dyspnea * Cyanosis * Fatigue * Symptoms of congestive heart failure |
|
|
What does aortic stenosis mean? |
- Narrowing at, above or below the aortic valve
- Symptoms: * Murmur * LEFT ventricular enlargement * Chest pain * Exercise intolerance, dizziness, syncope * Weak, thready pulses * Hypotension |
|
|
What does coarctation of the aorta mean? |
- Narrowing of the DESCENDING aorta - RESTRICTS blood flow LEAVING the heart - SEVERE coarctation requires IMMEDIATE treatment
- Symptoms: * Increased BP and O2 saturation in upper extremities compared to lower * Nosebleeds * Headaches * Vertigo * Leg pain * Weak or absent lower extremity pulses |
|
|
What is transposition of the great arteries? |
- Pulmonary arteries supplied by left ventricle - Aorta by right ventricle - Right to left shunting - Transposition of the great arteries is NOT compatible with life
- Symptoms: * Murmur * Severe cyanosis quickly * Cardiomegaly * Heart failure |
|
|
What is the treatment for transposition of the great arteries? |
- Prostaglandin E1 to maintain open ductus arteriosus - Corrective surgery - Prophylactic antibiotic - Promote nutrition |
|
|
What does tricuspid atresia mean? |
- COMPLETE CLOSURE of the TRICUSPID valve
- Symptoms: * NO BLOOD FLOW from the RIGHT ATRIUM to the RIGHT VENTRICLE * Severe cyanosis within hours of birth (increases as PDA closes) * Heart failure * Chronic hypoxemia * Failure to thrive and growth retardation |
|
|
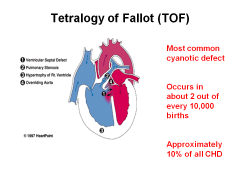
What are the 4 related defects of tetralogy of fallot (TOF)? |
1. Pulmonary stenosis 2. Ventricular septal defect (VSD) 3. Overriding aorta (aorta is positioned directly over a ventricular septal, instead of left ventricle) 4. Right ventricular hypertrophy (RVH)
- Tetralogy of fallot (TOF) is the most common CYANOTIC DEFECT
- Symptoms: * Murmur * Cyanosis * Reduced blood flow to the lungs * Severe dyspnea * Clubbing of fingers * Hypercyanotic spells (TET spells, transient periods in an increase of of right to left shunting) * Acidosis * Polycythemia * Clot formation * Squatting position * Failure to thrive |
|
|
Tetralogy of fallot (TOF): |
|
|
|
What does a "blue baby" mean? |
- Cyanotic baby - Children with TOF exhibit BLUISH skin during episodes of crying or feeding |
|
|
Why would a child with a cyanotic heart assume a squatting position? |
- Squatting position decreases blood return from lower extremities, thus helping to relieve cyanotic spells - Treament: knee-chest position, morphine, propanolol and oxygen |
|
|
* Heart Failure*
What are the symptoms of imaired myocardial function? |
- Tachycardia, murmurs, extra heart sounds - Decreased urinary output, diaphoresis, fatigue - Cool extremities, weak peripheral pulses - Slow capillary refill - Cardiomegaly - Anorexia |
|
|
* Heart Failure *
What are the symptoms of pulmonary congestion? |
- Tachypnea, dyspnea, crackles heard in lungs - Retractions, nasal flaring - Recurrent respiratory functions - Stridor, grunting |
|
|
* Heart Failure *
What are the symptoms of systemic venous congestion? |
- Hepatomegaly - Enlarged spleen - Peripheral edema - Ascites - Neck vein distention (seen in infants) |
|
|
What are the signs and symptoms of hypoxemia? |
- Cyanosis - Poor weight gain - Clubbing - Polycythemia - Hypercyanotic (TET) spells |
|
|
What is included in the management of heart failure? |
- Improve cardiac function: * Digoxin * Captopril, Vasotec (ACE inhibitor)
- Rid body of excess fluid: * Diuretics
- Decrease workload of the heart: * Bed rest * Semi-fowler's position * Maintain body temperature
- Increase tissue oxygenation: * Cool, humidified oxygen |
|
|
What is a cardiac catheterization? |
- INVASIVE test used for diagnosing, repairing some defects, and evaluating some dysrhythmias - CHECK FOR ALLERGIES TO SHELLFISH and IODINE - Patient will be NPO 4-6 hours before procedure - Locate and mark dorsalis pedis and posterior tibial pulses |
|
|
What is the post-op care for cardiac catheterization? |
- Monitor for bleeding, hematoma, thrombus - Assess pulses and temperature and color - Pressure dressing for 6 hours - Continuous cardiac monitoring, O2 sat - Maintain bed rest for 4-8 hours; keep extremity straight - Encourage oral intake, to rid dye from body |
|
|
What is the nursing care for the child with congestive heart failure (CHF)? |
- Keep child well-hydrated
- Conserve the child's energy! * Frequent rest periods, CLUSTERING CARE * Small, frequent meals * Bathing PRN * Keep crying to a minimum
- Daily weights and I&O's * Monitor HR, BP, serum electrolytes, renal function * Promote developmental growth
- Decrease workload of the heart: * Bed rest * Semi-fowler's or Fowler's while awake
- Increase tissue oxygenation: * Cool, humidified oxygen * Suction as needed
- Medications: * Digoxin: improves myocardial contractility * HOLD mediation if infant HR is < 90, and child HR is < 70 * Lasix: rids body of excess fluid and sodium (monitor for signs of hypokalemia - Lasix is potassium wasting) |
|
|
What are signs of worsening heart failure? |
- Increased sweating - Decreased urinary output (fewer wet diapers) |
|
|
What is the treatment for a child with epistaxis (bloody nose)? |
- Have child sit upright, and tilt head slightly forward - Apply steady pressure to both nostrils, just below the nasal bone for 10-15 minutes - Apply cold compress across the bridge of nose |
|
|
What is leukemia? |
- Leukemia is a group of malignancies that affects BONE MARROW and the LYMPHATIC SYSTEM - Cancer of blood forming tissues - Leukemia is classified by the type of WBC's that become neoplastic
- Acute lymphoid leukemia (ALL) - Acute myelogenous leukemia (AML) - Nonlymphoid leukemia (ANLL) |
|
|
What does leukemia cause? |
- Leukemia causes bone marrow dysfunction, leading to anemia and neutropenia - Deficient RBC's, leading to anemia - Deficient, immature WBC's (neutropenia), leading to increased risk for infection - Deficient platelets (thrombocytopenia), leading to increased risk for bleeding and bruising |
|
|
What are the risk factors of leukemia? |
- Leukemia is the most common cancer of childhood - ALL (acute lymphoid leukemia), is the MOST COMMON form of leukemia in children - Children with Trisomy 21 (down syndrome), have a greater risk of developing leukemia |
|
|
What is the subjective and objective data for a patient who has leukemia? |
- History and physical assessment findings may reveal vague reports of fatigue, anorexia and headache
- Early manifestations: * Low-grade fever * Pallor, listlessness, unsteady gait * Increased bruising and petechiae * Enlarged liver, lymph nodes, and joints * Abdominal, leg, and joint pain * Constipation * Headache * Vomiting * Anorexia
- Late manifesations: * Hematuria * Pain * Ulcerations in mouth * Enlarged kidneys and testicles * Signs of increased intracranial pressure |
|
|
What are some diagnostic procedures for leukemia? |
- Bone marrow aspiration, or biopsy analysis (MOST DEFINITIVE diagnostic procedure) - CSF analysis - Complete blood counts (shows DECREASED RBC's, WBC's, platelets) |
|
|
What is the nursing management for the child with leukemia? |
- Chemotherapy - Adequate nutirition/electrolytes - Nutritional support - Manage bleeding and pain - Platelets, and other blood products - Provide oral and skin care - PROTECT FROM INFECTION - Monitor LOC - Prepare child for hair loss |
|
|
What are some side effects of chemotherapy treatment? |
- Alopecia - Mucosal ulceration - Skin breakdown - Neuropathy - Loss of appetite |
|
|
What are some complications of leukemia? |
- INFECTION
- Bleeding: * Monitor for bleeding gums * Avoid unnecessary skin punctures * Avoid rectal temperatures
- Anemia: * Cardiotoxicity * Delayed growth and development |
|
|
What is iron deficiency anemia? |
- Most common form anemia in children 6 months-2 years - Also common in adolescent 12-20 years - RBC's with DECREASED Hgb levels have a DECREASED capacity to carry oxygen to tissue - Iron deficiency anemia usually results from an inadequate dietary supply of iron - Prolonged anemia can lead to developmental growth retardation and delays |
|
|
What is the subjective and objective data for a child who has iron deficiency anemia? |
- SOB, tachycardia - Dizziness, or fainting with exertion - Pallor, nail bed deformities - Fatigue, irritability, muscle weakness - Impaired healing |
|
|
What are the abnormal lab values for iron deficiency anemia? |
- Hemoglobin levels < 8 g/dL - Decreased levels of serum iron, or total iron binding capacity - Microcytic and hypochromic RBC's |
|
|
What is the nursing care for the child with iron deficiency anemia? |
- Provide iron supplements for PRETERM or LOW birth weight infants - Encourage BREASTFEEDING for infants < 6 months of age - Iron-fortified formula for non-breastfed infants - Include high iron, high vitamin C and protein foods - Allow frequent rest periods |
|
|
How should iron supplements be administered to children? |
- Give 1 hour before or 2 hours AFTER MILK or ANTACID to PREVENT decreased absorption - Monitor for GI side effects - Administer on an EMPTY STOMACH - Give vitamin C to help INCREASE absorption - Educate family to expect stools to be black |
|
|
What is the nutritional teaching for the child with iron deficiency anemia? |
- Increase fiber and fluids to prevent constipation
- Food sources that contain iron: * Dried legumes * Dried fruit * Green, leafy vegetables * Nuts * Poultry * Red meat |
|
|
What is sickle cell disease? |
- Sickle cell disease (SCD), is a group of diseases in which there is abnormal sickle hemoglobin (HbS) - Manifestations and complications of sickle cell anemia are the RESULT of RBC sickling, which leads to INCREASED BLOOD VISCOSITY, obstruction of blood flow and tissue hypoxia |
|
|
What is the pathophysiology of sickle cell anemia? |
- The RBC's have the ability to develop a sickled shape, this is usually precipitated by increased oxygen demands (infection, pain, emotional stress), or decreased levels of oxygen (pulmonary infections, high altitude) - Tissue hypoxia caused ischemia, which results in PAIN - Increased destruction of RBC's also occur |
|
|
What is a sickle cell crisis? |
- The EXACERBATION of sickle cell anemia |
|
|
What are the risk factors of sickle cell anemia (SCA)? |
- Primarily found in African Americans - SCA is an AUTOSOMAL RECESSIVE GENETIC DISORDER in which normal hemoglobin A (HbA) is partially, or completely replaced with HbS - Children with the sickle cell trait DO NOT manifest the disease BUT can pass the trait to their offspring |
|
|
What are the precipitating factors that lead to a sickle cell crisis? |
- Fever - Dehydration - Altitude - Extremes in temperature - Vomiting - Emotional distress - Alcohol consumption - Excessive exercise, or physical activity |
|
|
What is the subjective and objective data for the child with sickle cell anemia? |
- Family history of sickle cell anemia or sickle cell trait - Reports of pain, crisis and management - Shortness of breath, fatigue - Tachycardia - Pallor and jaundice - Nail bed deformities - Lethargy, irritability and muscle weakness - Impaired healing - Crisis manifestations |
|
|
What is hand-foot syndrome? |
- Sickle cells can block the small blood vessels in the hands or feet (hand-foot syndrome) - This leads to pain, swelling and fever - Swelling often occurs on the back of the hands and feet, and moves into the fingers and toes - Hand-foot syndrome may be the first sign of sickle cell anemia in infants |
|
|
What is a vaso-occlusive crisis? |
- Diminished levels of oxygen lead to sickle shape, which leads to cells becoming rigid, leads to obstruction of capillary blood flow, leading to congestion and tissue hypoxia, leads to additional sickling and infarctions - Hypoxia, fever, dehydration, emotional stress, or physical stress may trigger a crisis |
|
|
What are the ACUTE and CHRONIC symptoms of a vaso-occlusive crisis? |
- ACUTE: * Severe pain, usually in bones, joints and abdomen * Swollen joints, hands and feet * Anorexia, vomiting, fever * Hematuria * Obstructive jaundice * Visual disturbances
- CHRONIC: * Increased risk of respiratory infections and/or osteomyelitis * Retinal detachment and blindness * Systolic murmurs * Liver failure * Seizures * Deformities of skeleton |
|
|
What laboratory tests are used to diagnose sickle cell anemia? |
- CBC to detect anemia - Sickledex: sickle solubility test, screening tool that will detect the presence of HbS, but will NOT differentiate the trait from the disease - Hgb electrophoresis: separates the various forms of Hgb and is the DEFINTIVE diagnosis of sickle cell anemia - Transcranial doppler test (TCD): used to assess intracranial vascular flow and detect the risk of a CVA |
|
|
What is the nursing care for the child with sickle cell anemia? |
- Promote rest to DECREASE oxygen consumption of the tissue - Administer oxygen as prescribed if hypoxia is present - Maintain fluid and electrolyte balance
- Pain management: * Treat mild to moderate pain with Acetaminophen (Tylenol) or Ibuprofen (Advil) * Manage severe pain with opioid analgesics * Apply comfort measures, such as warm packs to painful joints
- Administer blood products - Encourage child to wear a medic-alert bracelet
- Treat and prevent infection: * Administer antibiotics * Give oral prophylactic penicllin
- Encourage passive range of motion exercises to prevent venous stasis |
|
|
What teaching would the nurse provide families to help prevent their child from having a vaso-occlusive crisis? |
- Teach the importance of promoting rest and adequate nutrition - Give specific directions regarding fluid intake requirements, such as how many bottles or glasses should be consumed daily
|
|
|
What are some complications of sickle cell anemia? |
- CVA: * Seizures * Vomiting * Weak extremity * Headache, changes in vision, slurred speech * Blood transfusions, shoud be performed every 3-4 weeks following a CVA
- Acute chest syndrome: * Chest pain * Dyspnea * Congested cough * Retractions * Tachycardia * Decreased O2 sats |
|
|
What is hemophilia? |
- Hemophilia is a disorder that results in an impaired ability to control bleeding - Bleeding time is extended due to lack of clotting factors, bleeding may be internal or external - Manifestations may be present in early infancy, but may not be evident until infants begin teething, sitting up, or crawling - Parents may observe excessive bruising with minor falls, or contact - Both hemophilia A & B are X-linked recessive disorders |
|
|
What is the subjective and objective data for the child with hemophilia? |
- Episodes of bleeding, excessive bleeding, reports of joint pain and stiffness, impaired mobility and activity intolerance - Active bleeding, which includes bleeding gums, epistaxis, hematuria, and/or tarry stools - Hematomas and/or bruising - Hemarthrosis as evidenced by joint pain, stiffness, warmth, swelling, redness, loss of range of motion, and deformities - Headache, slurred speech, and a decreased LOC |
|
|
What laboratory tests will be used to diagnosie hemophilia? |
- Laboratory tests: * Prolonged partial thromboplastic time (PTT) * Factor specific assays to determine deficiency
- Diagnostic procedures: * DNA testing * Detects classc hemophilia trait in females |
|
|
What is the nursing care for the child with hemophilia? |
- Avoid taking temperature rectally - Avoid uneccessary skin punctures, and use sterile aspetic technique - Apply pressure for 5 minutes after injections - Monitor stool and urine for occult blood |
|
|
What can nurse teach the parents to prevent bleeding for their child? |
- Place the infant or child in a padded crib - Dress toddlers in extra layers of clothing to provide additional padding - Set activity restrictions to avoid injury
- Appropriate and acceptable activities: * Swimming * Tennis * Golf
- Unacceptable and innappropriate activities: * Football * Basketball
- Use a soft bristled tooth brush to avoid bleeding gums |
|
|
What are some complications of hemophilia? |
- Uncontrolled bleeding: * Intracranial hemorrhage * Airway obstruction from bleeding in mouth, neck, or chest * Take measures to control bleeding, apply pressure and ice * Conduct neurological assessment for evidence of intracranial bleed
- Joint deformity: * Most often the elbows, knees, and ankles * Repeated episodes of hemarthrosis (bleeding into joint spaces) lead to impaired range of motion, pain, tenderness, and swelling, which can develop into joint deformities * Take appropriate measures to rest, immobilize, elevate, and apply ice to the affected joints during active bleeding |
|
|
What is Rheumatic fever? |
- Rheumatic fever is an inflammatory disease that occurs as a reaction to Group A-B hemolytic streptococcus (GABHS) infection of the throat - Rheumatic fever usually occurs within 2-6 weeks following an untreated or partially treated upper respiratory infection (strep throat) with GABHS |
|
|
What is the subjective and objective data for a child with rheumatic fever? |
- History of recent upper respiratory infection - Fever - Fatigue - Sore throat - Activity intolerance - Poor appetite - Tachycardia, cardiomegaly, prolonged PR interval, reports of chest pain - CNS involvement (chorea), including involuntary purposeless muscle movements |
|
|
What types of laboratory tests are used to diagnose rheumatic fever? |
- Throat culture GABHS - Elevated or rising serum antistreptolysin-O (ASO) titer - MOST RELIABLE
- Cardiac function: * ECG to reveal the presence of conduction disturbances and to evaluate the function of the heart and valves |
|
|
What is erythema marginatum? |
- A macular rash on the trunk, and proximal limbs |
|
|
What type of medications are used to treat rheumatic fever? |
- Penicilin (Pen V) or erythromycin (EryPed) - Stress the importance of finishing the entire course of the medication |
|
|
What are some complications of rheumatic fever? |
- Bacterial endocarditis - Damage to mitral and aortic heart valves |
|
|
What is Wilm's tumor? |
- Wilm's tumor (nephroblastoma) is a malignancy that occurs in the kidneys or abdomen - Wilm's tumor presents as an abdominal swelling or mass, usually firm, non-tender and unilateral - Metastasis is rare |
|
|
What is a symptoms of Wilm's tumor? |
- Abdominal swelling or mass that is usually FIRM, non-tender and unilateral |
|
|
What are some nursing considerations for chemotherapy treatment? |
- Handle chemotherapeutic agents carefully - Medicate the child with an anti-emetic prior to administration - Allow the child several food choices, allow the child to choose favorite foods - Observe mouth for mucosal ulcerations - Offer cool fluids to prevent dehydration, and soothe sore mucous membranes |
|
|
What is a neuroblastoma? |
- Neuroblastoma is a malignancy that occurs in the ADRENAL gland, sympathetic chain of the retroperitoneal area, head, neck, pelvis and chest - Most tumors have spread by metastasis at the time of diagnosis |
|
|
What is the subjective and objective data for the child with neuroblastoma? |
- Lymphadenopathy - Weight loss, anemia and fatigue - Neuroblastoma presents as an asymmetrical, firm, non-tender mass in the abdomen that crosses the midline |
|
|
What is osteosarcoma and Ewing's sarcoma? |
- Osteosarcoma: * Occurs in long bones * Treatment frequently involves amputation
- Ewing's sarcoma: * Occurs in the shaft of long bones * Treatment includes radiation to the tumor site and chemotherapy * DOES NOT require amputation |
|
|
What is Kawasaki's disease?
|
- A febrile multi-system disorder, resulting in inflammation of blood vessels - vasculitis - Usually occurs in children under 5 years of age
|
|
|
What are the signs and symptoms of Kawasaki's disease? |
- A high spiking fever of 102.2 degrees that lasts up to 5 days - Strawberry tongue - Cracked, dry lips - Elevated ESR - Edema of hands and feet, erythema - Swollen lymph nodes |
|
|
What is the treatment for Kawasaki's disease? |
- Anti-inflammatory: * Aspirin * Gamma globulin (IVIG)
- Nursing: * Frequent, gentle oral care * Promote comfort, cool baths
|
|
|
What is meningitis? |
- An acute inflammation of the meninges of the brain - VIRAL or ASPETIC meningitis usually only requires supportive care for recovery - BACTERIAL or SEPTIC meningitis is a CONTAGIOUS infection, the prognosis depends on how quickly the care is initiated |
|
|
What are the risk factors of meningitis? |
- VIRAL ILLNESSES: * Mumps * Measles * Herpes
- UPPER RESPIRATORY INFECTIONS: * Otitis media (caused by bacterial infections) * Tonsillitis (caused by bacterial infections)
- Immunosuppression - Injuries that provide direct access to CSF (skull fracture, penetrating head wound)
- Overcrowded living conditions |
|
|
What is the subjective and objective data for the child who may have meningitis? |
- Subjective: * Child may report photophobia or headache * Parents may report that child is irritable, has vomited and is drowsy
- Objective (newborns): * NO illness present at birth, but progresses within a few days * Clinical signs may be VAGUE and difficult to diagnose * Poor muscle tone, weak cry, poor feeding * Fever or hypothermia * Nuchal rigidity is NOT usually present * Bulging fontanels is a LATE sign
- Objective (2 months-2 years): * Seizures, with a HIGH PITCHED CRY * Fever and irritability * Bulging fontanels * Possible nuchal rigidity * Poor feeding * Vomiting * Brudzinki and Kernig's sign do NOT assist with the diagnosis
- Objective (2 years-Adolescence): * Seizures (often initial sign) * Nuchal rigidity * Positive Brudzinki's sign (flexion of extremities) * Positive Kernig's sign (resistance to extension of child's leg from flexed position) * Fever and chills
- Objective data: * Headache * Photophobia * Irritability and restlessness, that may progress to drowsiness or delirium, stupor and coma * Petechiae or purpuric rash (seen with meningococcal infection) * Chronic draining ear |
|
|
What is a meningococcal rash? |
- Meningococcal rash are characteristic purpuric lesions of meningococcal meningitis - The presence of petechiae our a purpuric-type rash requires IMMEDIATE medical attention |
|
|
What are the laboratory tests done to diagnose meningitis? |
- Laboratory tests: * Blood culture and sensitivity to identify appropriate broad-spectrum antibiotic * Lumbar puncture: CSF that appears cloudy (bacterial) or clear (viral), elevated protein levels, elevated CSF pressure are indicative of meningitis
- Diagnostic tests: * Cerebrospinal fluid analysis (BEST diagnostic test for meningitis) |
|
|
What is the nursing care for the child with meningits? |
- The presence of petechiae or a purpuric type rash requires immediate medical attention - Initiate and maintain isolation precautions (continue for 24 hours AFTER antibiotics have been administered) - Frequent monitoring of vital signs - Initiate IV fluids to maintain hydration - Decrease environmental stimuli - Maintain safety (keep bed in low position, take seizure precautions) |
|
|
What type of medications are used to treat meningitis? |
- IV antibiotics - Corticosteroids - Anticonvulsants (prophylactic for seizures) - Analgesics (NON-OPIOID to avoid masking changes in LOC) |
|
|
What are some complications of meningitis? |
- Increased intracranial pressure: * Could lead to brain damage * Monitor for signs of ICP |
|
|
- What are the symptoms of increased ICP? |
- Infants: * Lethargy, poor feeding * HIGH-PITCHED CRY * Tense, bulging fontanel * Increased head circumference
- Children: * Anorexia * Headache * Blurred vision * Separation of cranial sutures
- Late signs: * Altered LOC * Pupil dilation and sluggish response to light * Altered respiratory rate then apnea |
|
|
What is Reye syndrome? |
- Reye syndrome primarily affects the liver and brain causing: * Liver dysfunction (bleeding and poor clotting) * Cerebral edema (increased ICP) * Lethargy progressing to coma * Hypoglycemia * Shock
- The prognosis of Reye syndrome is BEST with early recognition and treatment |
|
|
What are the risk factors to Reye syndrome? |
- The exact cause of Reye syndrome is unknown - An association between using aspirin (salicylate) products for treating viral infections and the development of Reye syndrome - Symptoms most often appear at the end of a viral illness |
|
|
What is the nursing care for the child with Reye syndrome? |
- Maintain hydration: * Administer IV fluids and prescribed * Maintain accurate I&O
- Position the child: * Avoid extreme flexion, extension, rotation * Maintain head in a midline neutral position * Keep HOB elevated at 30 degrees |
|
|
What type of medications are used to treat Reye syndrome? |
- Osmotic diuretic: * Mannitol (Osmitrol): to decrease cerebral swelling
- Insulin: * Administer to increase glucose metabolism |
|
|
What important teaching should the nurse give parents when discharging a child who has recovered from Reye syndrome? |
- Teach parents to AVOID giving salicylates for pain or fever in children - Teach parents to read labels of over the counter medications to check for the presence of salicylates |
|
|
What are seizures? |
- Seizures are abrupt, abnormal, excessive, and uncontrolled electrical discharges of neurons within the brain that may cause alterations in LOC |
|
|
What is the nursing care for the child during a seizure? |
- Protect the child from injury (move furniture away) - Position the child to provide a patent airway - Place child on side (to prevent aspiration) - DO NOT attempt to restrain the child - Do not attempt to place anything into the child's mouth, DO NOT use padded tongue blades - Lossen restrictive clothing |
|
|
What is status epilepticus? |
- Prolonged seizure activity that lasts longer than 30 minutes or a continuous seizure without a postictal phase - Requires IMMEDIATE treatment to PREVENT brain damage |
|
|
What is cerebral palsy? |
- A non-progressive impairment of motor function, muscle control, coordination and posture - CP is the MOST COMMON permanent physical disability in children - CP may cause abnormal perception and sensation; visual, hearing, and speech impairments; seizures, and cognitive disabilities |
|
|
What are the risk factors of cerebral pasly? |
- Brain anomalies, cerebral infections, head trauma (shaken baby syndrome) - Extremely low birth weight |
|
|
What is the subjective and objective data for the child with cerebral palsy? |
- Subjective: * Parent may describe concerns with development * Poor head control or absence of smiling in a 3-month-old infant * Difficulty with dressing or diaper changes due to stiff legs and arms during infancy and early childhood, the child may push away or arch back
- Objective: * A floppy or limp body in infants * An inability to sit without support in an 8-month-old infant * Use of only one side of the body to play or move about * Feeding difficulties * Muscle spasms that are painful * Involuntary movements * Disturbance in gait or mobility |
|
|
What are some diagnostic procedures for the child with cerebral palsy? |
- Complete neurological assessment * MRI (to evaluate structures or abnormal areas located near bone) |
|
|
What is the nursing care for the child with cerebral palsy? |
- Monitor developmental milestones - Evaluate need for hearing or speech evaluations - Promote independence with self care activities for as long as possible - Maintain an open airway, by elevating HOB - Ensure adequate nutrition
|
|
|
What type of medications are used in the treatment of cerebral palsy? |
- Baclofen (Lioresal): * Skeletal muscle relaxant, to decrease muscle spasms and spasticity
- Diazepam (Valium): * Skeletal muscle relaxant, to decrease muscle spasms and spasticity |
|
|
What is a complication of cerebral palsy? |
- Aspiration of oral secretions: * Keep HOB elevated * Keep suction equipment available
- Potential for injury: * Initiate safety precautions * Raise bed rails
|
|
|
What does anencephaly mean? |
- A neural tube defect - No development of the brain above the brainstem |
|
|
What does encephalocele mean? |
- A neural tube defect - Protrusion of meningeal tissue or meningeal-covered brain through a defect in the skull |
|
|
What does spina bifida mean? |
- A neural tube defect - A vertebral defect in which the posterior vertebral arches fail to fuse - An incomplete closure of the vertebra and neural tube (the fetal tissue that develops in the CNS) |
|
|
What does meningocele mean? |
- Protrusion of a meningeal sac filled with CSF through a vertebral defect, associated with no abnormalities of the spinal cord |
|
|
What is a meningomyelocele? |
- Protrusion of a meningeal sac that contains CSF, portion of the spinal cord, and nerves through a vertebral defect |
|
|
What are some risk factors for neural tube defects? |
- Neural tube defects are caused by the failure of the neural tube to close in the first 3-5 weeks of gestation - Neural tube defects are linked to insufficient folic acid in the maternal diet - An elevated AFP may indicate the presence of a neural tube defect |
|
|
When would a surgical shunt be placed in an infant? |
- A surgical shunt will be placed if HYDROCEPHALUS develops - A VENTRICULOPERITONEAL SHUNT will be placed inside the brains ventricle - Hydrocephalus results from an increased production, decreased absorption, or blockage of the flow of CSF
- Postoperatively: * Observe for signs of ICP (high-pitched cry, bulging fontanel) |
|
|
What can the nurse teach the parents to assess for in their child with a shunt? |
- Vomiting - Headache - Irritability - Fever - Redness along shunt line - Fluid around shunt valve |
|
|
What is the nursing care for the child who has a shunt? |
- Measure head circumference - Monitor for symptoms of ICP - Support the head when transferring the infant - To reduce vomiting, feeding should be frequent and in small amounts |
|
|
What does strabismus mean? |
- Misaligned eyes
- Treatment: * Patch the unaffected eye to increase visual stimulation of the weaker eye * Eye exercises |
|
|
What does ambylopia mean? |
- Reduced visual acuity (clarity of sight), which cannot be corrected by glasses or contact lens - Blindness may occur if the weaker eye is left untreated
- Treatment: * Patch the unaffected eye |

