![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
104 Cards in this Set
- Front
- Back
|
Cardiovascular examination: 3 essential questions
|
1. General condition of the child + look for dysmorphic features
2. Assess for evidence of central cyanosis 3. Assess for evidence of congestive heart failure (hepatomegaly , tachypnoea and tachycardia) |
|
|
Cardiovascular examination: % of children with inocent murmours
|
up to 50%
|
|
|
Cardiovascular examination:: Characteristics of innocent murmours
|
a) soft
b) systolic c) no associated symptoms d) may vary with posture and respiration e) localized (usually to left sternal border) |
|
|
Innocent cardiac murmour-seen especially in preterm infants , is a physiological finding and disappears after a few weeks
|
1) Increased flow across branch pulmonary artery
|
|
|
This is a vibratory murmur Innocent cardiac murmour-found at mid LSB and is caused by turbulence around a myocardial muscle band in the left ventricle
|
Still's murmour
|
|
|
Innocent cardiac murmour-it may be easy to hear the venous blood flow returning to the heart especially at the upper LSB or aortic area . This is heart in both systole and diastole and will disappear on lying the child flat
|
Venous hum
|
|
|
Incidence of chidlren having congenital heart disease
|
8 per 1000 (just under 1%)
|
|
|
ASD contributes to ___% of congenital heart disease in children
|
30%
|
|
|
PDA is accounting for ______% of all congenital heart disease
|
12%
|
|
|
Risk of recurrence: congenital heart disease: Previous sibling with CHD
|
2%
|
|
|
Risk of recurrence: congenital heart disease: 2 siblings with CHD
|
4%
|
|
|
Risk of recurrence: congenital heart disease: FAther with CHD
|
5%
|
|
|
Risk of recurrence: congenital heart disease: Mother with CHD
|
6%
|
|
|
Clubbing is first visible from____ ________ onwards in those with cyanotic congenital heart disease and is first apparent in the ______ or _______
|
Clubbing is first visible from 6 months onwards in those with cyanotic congenital heart disease and is first apparent in the thumbs or toes
|
|
|
HS 2 is loud
|
Pulmonary hypertension
|
|
|
Usually with ____________the sounds of HS 2 separate and come together on expiration and this is termed ___________ _____________
|
Usually with inspiration the sounds of HS 2 separate and come together on expiration and this is termed physiological splitting
|
|
|
In ____________ or _____________you will hear fixed splitting of HS 2
|
In atrial septal defect (ASD) or RBBB you will hear fixed splitting of HS 2
|
|
|
CV exam: right lateral thoracotomy scar found after lifting the arms and inspecting the back
|
implies placement of a Blalock-Taussig Shunt (artificial tubing between the subclavian and pulmonary arteries)
|
|
|
CV exam: left lateral thoracotomy scar implies:
|
left BT shunt
- repair of coarctation of aorta - pulmonary artery banding - PDA ligation |
|
|
CV exam: A median sternotomy scar implies
|
a repair of intracardiac pathology with open cardiac surgery.
|
|
|
CV exam: median sternotomy scar+ lateral thoracotomy scar – think
|
Fallot’s with BT shunt and then complete repair
|
|
|
If Downs with sternotomy scar – think
|
AV canal defect with residual VSD
|
|
|
pansytolic murmur at lower LSB
|
VSD
|
|
|
ejection systolic murmur at upper LSB + fixed split HS2
|
ASD
|
|
|
Continuous murmur + collapsing pulses
Fallot –Blue + harsh long systolic murmur at upper LSB +/- scars |
PDA
|
|
|
- Ejection systolic murmur URSE + carotid + suprasternal thrill
|
AS
|
|
|
Ejection systolic murmur ULSE +/- thrill
|
PS
|
|
|
Ejection systolic murmur + weak or absent femoral pulses
|
CoA
|
|
|
Signs of respiratory distress –
|
tachypnoea, grunting, use of accessory muscles of respiration, cyanosis
|
|
|
“claw hand” what name and level?
|
Klumpke lesion C8, T1
|
|
|
“waiter tip” what name and level?
|
(Erb’s C5, C6)
|
|
|
shoulder abduction invervation level?
|
C5,C6
|
|
|
should abduction invervation level?
|
C5,C6,C7
|
|
|
elbow flexion invervation level?
|
C5,C6
|
|
|
elbow extension invervation level?
|
C7,C8
|
|
|
wrist flexion invervation level?
|
C6,C7
|
|
|
wrist extension invervation level?
|
C6,C7
|
|
|
hand grip invervation level?
|
C8,T1
|
|
|
finger abduction inervation level?
|
C8,T1
|
|
|
Biceps and brachioradialis reflex inervation level?
|
C5,C6
|
|
|
Triceps reflex inervation level?
|
C7,C8
|
|
|
Shoulder dermatome?
|
C4
|
|
|
Radial aspect of upper limb dermatome?
|
C5 arms, C6 forearm
|
|
|
Tips of fingers dermatome?
|
C7
|
|
|
Ulnar aspect of upper limb dermatome?
|
C8 forearm, T1 elbow
|
|
|
Axilla dermatome?
|
T2
|
|
|
hip flexion inervation level?
|
L1,L2,L3
|
|
|
hip extension inervation level?
|
L5,SI,S2
|
|
|
knee flexion inervation level?
|
L5,SI
|
|
|
knee extension inervation level?
|
L3,L4
|
|
|
ankle plantarflexion inervation level?
|
S1
|
|
|
ankle dorsiflexion inervation level?
|
L4,L5
|
|
|
Knee jerk reflex inervation level?
|
L3, L4
|
|
|
Ankle jerk reflex inervation level?
|
S1, S2
|
|
|
Plantar response (may be upgoing up until _____ months old)
|
Plantar response (may be upgoing up until 18 months old)
|
|
|
Groin sensation
|
L1
|
|
|
upper thigh sensation
|
L2
|
|
|
knee sensation
|
L3
|
|
|
medial aspect of leg below knee sensation
|
L4
|
|
|
lateral aspect of leg below knee and continues down onto the medial aspect of the foot
|
L5
|
|
|
sole of the foot sensation
|
S1
|
|
|
central posterior aspect of the leg and thigh sensation
|
S2
|
|
|
Normal Range of motion all movements: wrist
|
Flexion (80 degrees) and extension (70 degrees)
Radial (20 degrees) and ulnar deviation (30 degrees) Pronation (90 degrees) and supination (90 degrees) |
|
|
Normal Range of motion all movements: Elbow
|
Flexion (135 degrees) and extension (0-10 degrees)
|
|
|
Normal Range of motion all movements: Shoulder
|
Abduction (180 degrees) and adduction
Flexion (90 degrees) and extension (45 degrees) Internal (55 degrees) and external rotation (45 degrees) |
|
|
Normal Range of motion all movements: Cervical spine:
|
Flexion (45 degrees) and extension (55 degrees)
Lateral flexion (ear to shoulder – 40 degrees) Rotation (chin in line with shoulder – 80 degrees) |
|
|
Normal Range of motion all movements: Hip
|
Flexion (120 degrees) + Thomas Test for fixed flexion deformity
Extension (15 degrees) Abduction (50 degrees) and adduction (30 degrees) Internal (35 degrees) and external (45 degrees) rotation when checking all hip movements, the pelvis should be stabilised. |
|
|
Normal Range of motion all movements: Knee:
|
Flexion (135 degrees) and extension (up to 10 degrees)
|
|
|
Normal Range of motion all movements: Ankle:
|
Dorsiflexion (20 degrees) and plantar flexion (50 degrees)
Inversion (5 degrees) and eversion (5 degrees) |
|
|
normally AC>BC but if conductive deafness BC>AC
|
Rinne’s test:
|
|
|
held in midline – normally sound arises in midline if N. deafness – appears to arise on healthy side.
If conductive loss – sound referred to affected ear. |
Weber’s:
|
|

What is this?
|
NEC
|
|

What's this?
|
NEC
|
|

|
NEC
|
|
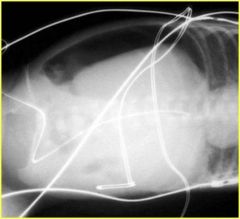
What's this?
|
NEC
|
|
|
Staging criteria for NEC
|
Bell staging
|
|
|
Stage 1 NEC
|
Non-specific signs
|
|
|
Stage 2 NEC
|
Definite disease, mild disease and abdo tenderness
|
|
|
Stage 3 NEC
|
Surgical NEC peritonitis, distension
|
|
|
Treatment options for NEC
|
Peritoneal drainage (buys time if unstable for surgery) vs. surgery (eventually needed)
|
|

Whats this?
|
Tracheo esophageal fistula. Findings in TEF include: Abdominal bowel gas confirms a distal fistula. Abdominal ‘double bubble’ confirms an associated duodenal atresia
|
|
|
Incidence of tracheo oesophageal fistula
|
1: 3000-45000
|
|
|
Tracheo esophageal fistula is associated with what 3 syndromes?
|
VATER, VACTERL, CHARGE syndrome
|
|
|
Clinical sings of tracheo esophageal fistula
|
– excessive drooling/choking on feeds; polyhydramnios only with pure atresia.
|
|
|
x-ray findings of tracheo esophageal fistula
|
Abdominal bowel gas confirms a distal fistula. Abdominal ‘double bubble’ confirms an associated duodenal atresia.
|
|
|
Scar/ approach for distal fistula operation
|
Posterolateral thoracotomy
|
|

What is the problem here?
|
Malrotation and volvulus
|
|
|
accumulation of gas in the submucosal layers of the bowel wall, which progresses to necrosis (mucosal -> full thickness). Bowel most often affected, right side of the colon and the distal ileum.
|
Necrotizing enterocolitis
|
|
|
NEC is primarily a complication of ____________
|
NEC is primarily a complication of prematurity
|
|
|
Risk factors other than prematurity (in a full term infant that can lead to NEC)
|
Sepsis, assisted ventilation, respiratory acidosis, and hypoxemia.
|
|
|
What is the onset and progression of NEC
|
Onset occurs 2 weeks to several months after birth
Progression may be rapid |
|
|
Mortality rate in:
Infants <1500g Infants>2500g |
Infants <1500g=10-44%
Infants>2500g= 0-20% |
|
|
Mortality rate of premature babies with NEC <1000g
|
40-100%
|
|
|
Signs of NEC
|
Feeding intolerance
Delayed gastric emptying Abdominal distention and/or tenderness Ileus/decreased bowel sounds Abdominal wall erythema (advanced stages) Bloody stool is observed in approximately 25% of patients |
|
|
NEC investigations
|
WCC- moderate neutropenia
Platelets- acute NEC--> thrombocytopenia ABG's- metabolic acidosis |
|
|
List 2 immediate complications of a tracheo esophageal repair
|
1. Anastomotic failure
2. Recurrent fistula |
|
|
List 4 long term complications associate with a tracheo esophageal fistula
|
Anastomotic stricture
Gastro-oesophageal reflux Oesophageal dysmotility Missed fistula (usually upper pouch) with recurrent chest infections |
|

whats this?
|
Malrotation and volvulus with necrosis
|
|

what does this clinical picture suggest?
|
Malrotation and volvulus
|
|
|
Name 4 signs of Malrotation and volvulus
|
Bilious vomiting, abdominal distension and PR bleeding.
+ abdominal tenderness |
|
|
T/F if no volvulus the surgery is urgent
|
F- non-urgent but surgery recommended
|
|

what is this?
|
Congenital Diaphragmatic Hernia, note stomach in thoracic cavity
|
|
|
In congenital diaphragmatic hernias approx. ____% of fetuses are stillborn
|
30%
|
|
|
Mortality rate for congenital diaphragmatic hernias
|
30-50%
|

