![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
• Most common congential foot deformity
• C-shaped foot deformity • Flexible Tx at home • Non-flexible serial casting • Refer if non-flexible |
Metatarsus Adductus
|
|
|
• Congenital, teratologic or positional
• ♂ more common, 75% congenital • Polygenic inheritance • Foot is in plantar flexion, hindfoot in inversion, forefoot is adducted/supinated |
Talipes Equinovarus (Club foot)
|
|
|
Who is Talipes equinovarus most common in? What is treatement?
|
• Males
• Tx: casting w/in 1st week of lift (severe cases - surgery) |
|
|
• Foot is hypermobile & pronated, asymptomatic.
• Usually improves by age 6. • Due to ligamentous laxity • What is important to check for? |
• Pes Planus (flat foot)
• Check for tight achilles tendon: cerebral palsy • mne: Planus ≈ flat, PP = pronated due to LL (ligamentous laxity) |
|
|
What is the most common osteochondrosis in the foot? Causes heel pain during adolescnt growth spurt. What is the underlying patholgoy?
|
• Sever disease
• Caused by idiopathic avascular necrosis |
|
|
• Common type of intoeing
• Dianosis made if there is IR when pt is prone and leg is flexed at knee (thigh-foot angle in the negative range) • What is the treatment? |
• Tibial torsion
• Tx= observation |
|
|
• Type of familial intoeing most common in ♀
• Child often sits in W position • Peak incidence 3-6 yo Child is clumsy, intoeing when running, patella rotated inward. What is the medial hip rotation? |
• Femoral Anteversion
• Medial Hip rotation > 70º mne: F*emoral ≈ F*emale ≈ F*amilial, AnteVersion ≈ W position |
|
|
What sign is ALWAYS a significant pediatric problem?
|
A non-traumatic limp (think hip!!!)
|
|
|
What is the most common cause of medical liability suits for pediatricians? Which side is more often affected? What demographic?
|
• Developmental Dysplasia of the Hip
• L hip 3x more common • Females more often affected |
|
|
What are the risk factors for developmental dysplasia?
|
• Breech delivery
• Oligohydraminos • Twins • (+) FH • First born |
|
|
What are the two signs used to dx a developmental dysplasia of the hip? What are there interpretations?
|
• Ortolani sign: (+) if gentle Anterior lifting with ABduction produces a palpable click or clunk
• Barlow sign: (+) if gentle Posterior pressure w/ Adduction produces click/clunk mne: Ortolani: O is a vowel, (anterior) • Barlow: b ≈ p, (posterior pressure) double pp, and double dd in adduction |
|
|
What are two signs of developmentaly dysplasia of the hip? What tests can be used?
|
• Limited Abductio nof the hip
• Waddling gait • Tests: Ultrasound (most accurate b/w 4wk-3mos), Hip X-ray > 6mos |
|
|
In a newborn exam for Developmental Dysplasia of the Hip, if there is a (+) Ortolani or Barlow tests what do you do? If there is just a click and/or some questionable findings what do you do?
At 1-2 weeks if exam is questionable what do you do? What is the key to Dx? |
• Clunk --> refer to pediatric ortho
• Questionable findings/click --> reexamine at 1-2 wks • At 1-2 weeks if exam is questionable ---> do US and refer to pediatric ortho Key to diagnosis is EARLY dx (< 4mos) |
|
|
What are the Txs available for Developmental dysplasia o the hip?
|
• Pavlik harness (holds hips Flexed & ABducted)
• Spica cast, diagnosis @ ≥ 6mos (for 3-5 mos) • Surgery(delayed diagnosis) |
|
|
What is the most common cause of limp w/ pain in a child < 10 yo? What is the peak age? Who is it most common in?
|
• Transient Synovitis
• Peak age: 3-8 yo • Most common in ♂ |
|
|
Presentation: 5yo boy with a painful limp. (-) Fever. (+) history of URI. PE: unable to medially rotate the hip or Abduct. Antalgic gait. What is the dx? What is the Tx?
|
• Dx: Transient Synovitis
• Tx: bed rest, NSAIDs, recheck in 1-2 wks. Consider Perthes |
|
|
What pediatric disorder of the hip is a pediatric emergency?
|
• Septic arthritis of the hip
|
|
|
What are the labs that are associated with Septic arthritis of the hip? X--rays? Tx?
|
• ↑ WBC & ↑ ESR
• Normal x-ray, HOT bone scan • Tx: surgical drainage |
|
|
Avascular necrosis of the femoral epiphysis. Most common in ____? What is the presentation? Tx?
|
• Legg-Perthes disease
• Most common in 4-8 yo ♂ • Presentation: painless limp • Tx: Ortho referral. mne: Think Ryan!! Legg-Perthes sounds like a white name (uncommon in blacks) |
|
|
What hip disorder most commonly presents in adolescent, obses, black ♂s ?
|
Slipped Capital Femoral Epiphysis
mne: lots of Blacks in DC (the capital) |
|
|
What is the presentation of Slipped Capital Femoral Epiphysis? What is the Tx?
|
• Chronic hip/knee pain w/ limp. Obese, hypogonadal, adolescent black ♂
• Tx: Ortho referral ASAP for internal in-situ screw fixation |
|
|
Posterior-medial, painless, non-pulsatile soft mass, prominent w/ extension
|
Popliteal cyst (Baker cyst)
|
|
|
• Very common. Increase in athletic, 8-12 yo ♂
• Overuse syndrome/traction apophysitis • Patellar ligament insertion into the tibial tuberosity • Presents w/ chronic knee pain Tx? |
Osgood-Schlatter's disease
Tx: symptomatic |
|
|
Wrist synovial fluid dilled cyst
• Most common in the radiocarpal joint. What is the Tx? |
Ganglion cyst
• Observation or surgery |
|
|
Subluxation of the annular ligament
• Presents w/ elbow flexed, palm-down position • What must you always check? |
• Dislocation of the Radial head
• ALWAYS check clavicle |
|
|
What is the most vulnerable joint in throwing injuries?
|
Elbow
|
|
|
What is the most common cause of scoliosis? Who does it present in most often? When is there the greatest risk?
|
• Idiopathic
• ♀s. Adolescent form most common. • Greatest risk during pds of rapid growth |
|
|
What is the Cobb angle used for? What is the procedure for <20º, > 20º, 30º-45º and > 45º?
|
• Cobb andle is used for the dx of scoliosis
• < 20º observe • > 20º refer • 30º-45º orthotic therapy (braces) • > 45º surgery |
|
|
What are the complications sene w/ congenital scoliosis?
|
• Congenital is very uncommon (Idiopathic is MOST common)
• GU anomalies, CHD, Spinal dysraphism, Extravertebral anomalies, VATER syndrome (Vertebra, Anal atresioa, Tracheal-Esophageal fistula, Renal agenesis) |
|
|
What test can be conducted for scoliosis? What else should you check for?
|
• Adam's forward bend test
• Check for café-au-lait spots, midline hair tufts |
|
|
What are red-flags associated with Scoliosis?
|
• Pain
• Abnormal neuro exam • Midline cutaneous abnormalities • High arches (congenital) |
|
|
When does the neural plate develop? What does it give rise to? When does the neural tube develop?
|
• Neural plate: 18 days gestation
• Gives rise to neural tube & neural crest cels • Neural tube: 22 days mne: pl8 and 22 2be (tube) |
|
|
Spinal dysraphism is?
|
Neural tube defects
|
|
|
Defects of the L5 or S1 vertebral arches:
1. Sac filled w/ CSF due to protrusion is called ___ 2. defects of the underlying bone or canal (tugts of hair, sacral dimple) 3. spinal canal & meninges are exposed |
Spinal dysraphism
• 1: Meningocele 2: Spina bifida occulta 3. Myelomeningocele |
|
|
What is Cushing triad? What does it mean?
|
• ↑ BP, ↓ Pulse, Irregular respirations
• Signifies critically ↑ ICP (shown by abnormal pupils) |
|
|
What are some of the signs & symptoms of ↑ ICP?
|
• HA (morning), vomiting (morning), CN VI palsy, papilledema, hulging fontanel, sunsetting of the eyes.
• Critically ↑ ICP is shown by Cushing triad. |
|
|
What can distension of the 3rd venticle in hydrocephalus caues?
|
• Endocrine disfxn (compession of hypothalamic regions)
• Visual dysfxn (compression of optic nerves/chiasm/tracts) |
|
|
Benign process, usually in obese ♀ of childbearing age
• Not critically ill Sx: HA, diplopia, CN VI palsy, PAPILLEDEMA • Brain imaging normal |
Psuedotumor Cerebri
|
|
|
What is the Tx of psuedotumor cerebri?
|
• Acetazolamide, repeated LPs, corticosteroids, surgery
|
|
|
What is the Tx for ↑ ICP?
|
• Elevate head of the bed
• Mannitol • Corticosteroids • Acetazolamide & furosemide • Hyperventilateion • Ventricular catheter • Phenobarbital induced coma |
|
|
• Frequent Autosomal recessive disease
• Progressive degeneraltion of anterior horn cells • Progressive proximal muscle weakness • Flaccid quadriplegia, respiratory failure & death |
• Werdnig-Hoffman or Spinal Muscular Atrophy
|
|
|
Idiopathic periopheral neuropathy • Often occurs after a respiratory or GI infxn • Areflexia, flaccidity, symmetric ascneding weakness What is the Tx? |
• Guillain-Barre Syndrome
• Often resolves spontaneously |
|
|
• Sex linked recessive trait
• Calf-psuedo-hypertrophy • Proximal musce weakness • Gower sign • Hyperlorgotic & waddling gait |
Duchenne's Musculodystrophy
|
|
|
What are the lab findings in Duchenne's Musclodystrophy? What is the underlying pathology? What is the difference b/w Duchenne's & Beckers?
|
• Labs: ↑ serum creatine phophokinase
• Pathology due to absence of dystrophin • Becker's has ABNORMAL dystrophy (Duchenne's has none) |
|
|
• AD disease
• Due to a triplet CTG repeat (shows anticipation) • At birth ther eis severe generalized weakness • Expressionless face |
Myotonic Dystrophy
|
|
|
• AD disease
• Harmartomas on organs: brain, eye, skin, kidney, & heart • Facial angiofibromas, mental retardation, severe epilepsy • Shagreen patches, ash-leaf spots (hypopigmented macule) |
• Tuberous Sclerosis
|
|
|
• AD disease
• Mutation in the tumor suppressor gene ______ • Tumors of peripheral nerves Comon sx: • Café au-lait spots • freckling in the area of the armpit • Lisch nodules |
• Neurofibramatosis Type-1
• Mutation of the NF-1 gene (chromosome 17q) |
|
|
What is required for the Dx of Neurofibramatosis Type I?
|
≥ 2 of:
• ≥ 6 café-au-lait spots • ≥ neurofibromas ≥ Freckling in the area of the armpit or groin ≥ 2 Lisch nodules or iris harmartomas • Optic nerve glioma • Scoliosis, abnormal sphenoid or tibia • FH+ for NF1 |
|
|
• AD
Loss of tumor suppressor gene on chromosome 22 • multiple intracranial & spinal tumors • Bilateral vestibular schwannomas by age 30 yo Cataracts |
• Neurofibramatosis Type II
|
|
|
What is required for the Dx of Neurofibramatosis Type II?
|
• Bilateral vestibular schwannomas
• FH of NF2 • Any two of the following: • Glioma • Meningioma • Schwannoma • Juvenile posterior subcapsular/lenticular opacity (or juvenile coritcal cataracts) |
|
|
• Sporadic disease
• Angiomas of the letomeninges • Ipsilateral port-wine nevus • possible glaucoma **Seizures due to ischemic injury to the brain underlying the meningeal angiomas** • Ca++ in gyri of brain |
Sturge-Weber syndrome
|
|
|
What is the Tx for Sturge-Weber syndrome?
|
• Anticonvulsants (to prevent seizure due to ischemic injury to the brain underlying the meningeal angiomas)
• hemispherectomy • Laser surgery (for facial nevus) |
|
|
What causes "tram track" on brain imaging in Sturge Weber syndrome?
|
• Calcium deteceted in the gyri of the brain underlying angioma
|
|
|
What causes seizures in Sturge Weber syndrome?
|
Due to ischemic inury to the brain underlying meningeal angiomas
|
|
|
• Joint disease that occurs in children16 yo
• More comon in♀ • RF is usually absent |
Juvenile rheumatoid arthritis
|
|
|
• Arthritis in children < 16 yo
• limited to a few joints • Uveitis w/ potential for blindness |
• Pauciarticular Juvenile Rheumatoid arthritis
|
|
|
• Disabling juvenile arthritis that affects many joints
|
• Polyarticular Juvenile Rheumatoid arthritis
|
|
|
• Necrotizing medium-sized vessel vasculitis involing the coronary arteries (thrombosis, aneurysm)
|
Kawasaki disease
|
|
|
What are the demographics of Kawasaki disease?
|
• ♂ < 5 yo
• Children of asian decenst higher incidence |
|
|
Disease presents as: fever, erythema, edema of hands/feet, desquamatated rash, cervical adenopathy, oral erythema & cracking of lips, Abnormal ECG
|
Kawasaki disease
|
|
|
What is the biggest risk associated with Kawasaki disease? What is the Tx?
|
• Risk of coronary complications (aneurysms)
• Tx: IV IgG and Aspirin |
|

What disease is being shown? What process?
|
Kawasaki disease
Desquamation of the skin of the toes |
|
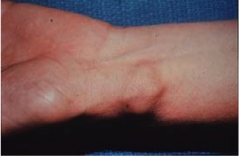
What disease is pictured?
|
Ganglion cyst
|

