![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
126 Cards in this Set
- Front
- Back
|
1. Arterial supply to the cerebral hemispheres
|
The arterial supply to the cerebral hemispheres is derived from the anterior circulation provided by the bilaterally paired internal carotid arteries, as well as by the posterior circulation provided by the bilateral vertebral arteries.
|
|
|
2. Circle of Willis
|
The anterior and posterior circulations meet in an anastomotic ring called the circle of Willis, from which all major cerebral vessels arise. The circle of Willis provides abundant opportunities for collateral flow; however, a complete ring in present in only approx 25% of individuals.
|
|
|
3. What are the terminal branches of the internal carotid arteries?
|
The anterior cerebral arteries and middle cerebral arteries are the terminal branches of the internal carotid arteries.
|
|
|
4. Where does the posterior cerebral arteries arise from?
|
The PCAs arise from the top of the basilar artery, which in turn is formed by the convergence of the two vertebral arteries.
|
|
|
5. What are the segments of the internal carotid artery?
|
1. Cervical segment in the neck
2. Petrous segment where it enters the temporal bone 3. Cavernous segment as the artery begins an S-shaped turn, AKA the carotid siphon, within the cavernous sinus 4. Intracranial segment, or supraclinoid, where it pierces the dura to enter the subarachnoid space. |
|
|
6. What are the main branches of the supraclinoid internal carotid artery?
|
Remember the mnemonic OPAAM
This stands for: Ophthalmic, Posterior communicating, Anterior choroidal, Anterior cerebral, and Middle cerebral arteries. |
|
|
7. Ophthalmic artery
|
The opthalmic artery ususally arises from the bend in the internal carotid just after it enters the dura.
It enters the optic foramen with the optic nerve and provides the main blood supply to the retina. |
|
|
8. Anterior cerebral artery
|
The ACA passes forward to travel in the interhemispheric fissure as it sweeps back and over the corpus callosum. Two major branches commonly seen are the pericallosal and callosomarginal arteries.
The ACA thus supplies most of the cortex on the anterior medial surface of the brain, from the frontal to the anterior parietal lobes, usually including the medial sensorimotor cortex. |
|
|
9. Middle cerebral artery
|
The MCA turrns laterally to enter the depths of the Sylvian fissue. Within the Sylvian fissue it usually bifurcates into the superior division and the inferior dividsion.
The branchs of the MCA form loops as they pass over the insula and then around and over the operculum to exit the Sylvian fissure onto the alteral convexity. The MCA thus supplies most of the cortex on the dorsolateral convexity of the brain. |
|
|
10. Superior division of the MCA
|
The superior division of the MCA supplies the cortex above the Sylvian fissure, including the alteral frontal lobe and usually including the peri-Rolandic cortex.
|
|
|
11. Inferior division fo the MCA
|
The inferior division of the MCA supplies the cortex below the Sylvian fissure, including the lateral temporal lobe and a variable portion of the parietal lobe.
|
|
|
12. Posterior cerebral artery
|
The PCA curves back after raising from the top of the basilar and sends branches over the inferior and medial temporal lobes and over the medial occipital cortex.
The PCA territory therefore includes the inferior and medial temporal and occipital cortex. |
|
|
13. What is the name of the most important penetrating vessels at the base of the brain?
|
The lenticulostriate arteries.
These small vessels arise from the initial portions of the MCA, before it enters the Sylvian fissue, and they penetrate the anterior perforated substance to supply large regions of the basal ganglia and internal capsule. In hypertension, the lenticulostriate arteries and other similar small vessels are particularly prone to narrowing, which can lead to lacunar infarction, as well as to rupture, causing intracerebral hemorrhage. |
|
|
14. Anterior choroidal artery
|
The anterior choroidal artery arises from the internal carotid artery.
Its territory includes portions of the globus pallidus, putamen, thalamus, and the posterior limb of the internal capsule extending up to the lateral ventricle. |
|
|
15. Recurrent artery of Heubner
|
The recurrent artery of Heubner comes off the initial portion of the anterior cerebral artery to supply portions of the head of the caudate, anterior putamen, globus pallidus, and internal capsule.
|
|
|
16. Thalamoperforator arteries
|
Small pentrating arteries that arise from the proximal posterior cerebral arteries near the top of the basilar artery include the thalamoperforator arteries, which supply the thalamus and sometimes extend to a portion of the posterior limb of the internal capsule.
|
|
|
17. Infarcts and ischemic events are most common in which arteries supplying the brain?
|
Infarcts and ischemic events are more common in the MCA that in the anterior or posterior cerebral arteries, at least in part, b/c of the relatively large territory supplied by the MCA.
|
|
|
18. In what three general regions do MCA infarcts occur?
|
1. Superior division
2. Inferior division 3. Deep territory |
|
|
19. MCA stem infarcts
|
Proximal MCA occlusions affecting all three of these regions are called MCA stem infarcts.
|
|
|
20. Large MCA territory infarcts
|
Large MCA territory infarcts often have a gaze preference towards the side of the lesion, especially in the acute period, shortly after onset.
|
|
|
21. Lacunes
|
Small deep infarcts involving penetrating branches of the MCA or other vessels are called lacunes. Certain characteristic lacunar syndromes can often be distinguished on clinical grounds from infarcts involving large blood vessel territories.
|
|
|
22. ACA infarcts
|
ACA infarcts typically produce contralateral lower extremity cortical type sensory loss and weakness of the upper motor neuron type.
There may also be a variable degree of frontal lobe dysfunction depending, in part, on the size of the infarct. Such dysfunction may include a grasp reflex, impaired judgment, flat affect, apraxia, abulia, and incontinence. |
|
|
23. Alien hand syndrome
|
Sometimes damage to the supplementary motor area and other regions in the frontal lobe leads to an unusal "alient hand syndrome" characterized by semiautomatic movements of the contralateral arm that are not under voluntary control.
|
|
|
24. PCA infarcts
|
PCA infarcts typically cause a contralateral homonymous hemianopia. Smaller infarcts that do not involve the whole PCA territory may cause smaller homonymous visual field defects. Sometimes the small penetrating vessels that come off the proximal PCA are involved, leading to infarcts int he thalamus or posterior limb of the internal capsule.
The result can be a contralateral sensory loss, contralateral hemiparesis, or even thalamic aphasia, if the infarct is in the dominant hemisphere thereby mimicking features of MCA infarcts. |
|
|
25. What type of infarction can produce alexia without agraphia?
|
PCA infarcts that involve the left occipital cortex and the splenium of the corpus callosum can produce alexia without agraphia.
|
|
|
26. Watershed zones
|
When a cerebral artery is occluded, ischemia or infarction occurs in the territory supplied by that vessel, with regions near other vessel relatively spared.
In contrast, when the blood supply to two adjacent cerebral arteries is compromised, the regions between the two vessels are most susceptible to ischemia and infarction. These regions between cerebral arteries are called watershed zones. |
|
|
27. Bilateral watershed infarcts
|
Bilateral watershed infarcts in both the ACA-MCA and MCA-PCA watershed zones can occur with severe drops in systemic BP.
A sudden occlusion of an internal carotid artery or a drop in BP in a patient with carotid stenosis can cause an ACA-MCA watershed infarct, since these vessels are both fed by the carotid. |
|
|
28. Deficits caused by a watershed infarct
|
Watershed infarcts can produce proximal arm and leg weakness ("Man in the barrel" syndrome) b/c the regions of homunculus involved often include the trunk and proximal limbs.
In the dominant hemisphere, watershed infarcts can cause transcortical aphasia syndromes. MCA-PCA watershed infarcts can cause disturbances of higher-order visual processing. In addition to watershed infarcts between the superficial territories of different cerebral vessels, watershed infarcts can also occasionally occur between the superficial and deep territories of the MCA. |
|
|
29. What are the most common causes of transient neurologic episodes?
|
The most common causes of transient neurologic episodes are transient ischemic attack, migraine, seizure, and other non-neurologic conditions such as cardiac arrhythmia or hypoglycemia.
|
|
|
30. Transient ischemic attack (TIA)
|
A TIA is classically defined as a neurologic deficit lasting less than 24 hours, caused by temporary brain ischemia. The more typical duration for a TIA is about 10 minutes.
Ischemic deficits lasting more than about 10 minutes probably produce at least some permanent cell death in the involved region of the brain. TIAs lasting more than an hour, in fact, are usually small infarcts. On the other hand, despite the appearance of a small infarct on an MRI scan, complete functional recovery can sometimes occur within one day. |
|
|
31. Mechanisms for transient ischemic attack
|
One possibility is that an embolus temporarily occludes the blood vessel but then dissolves, allowing return of blood flow before permanent damage occurs.
Other possibilities include in situ thrombus formation on the blood vessel wall and/or vasospasm leading to temporary narrowing of the blood vessel lumen. |
|
|
32. What are some other diagnoses that can commonly mimic TIAs?
|
Focal seizures and migraines; also - episodes of hypoglycemia can sometimes produce transient focal neurologic deficits, especially in the elderly.
|
|
|
33. What can cause a transient loss of consciousness without other focal features?
|
This is a special case of transient neurologic dysfunction. The most common cause by far is cardiogenic syncope including vasovagal transient episodes of hypotension ("fainting"), arrhthmias, and other non-neurologic causes.
Neurological causes are responsible for less than 5-10% of cases of syncope, and include seizures, and rarely, TIA of the posterior circulation affecting the brainstem reticular activating systems. |
|
|
34. Stroke
|
Stroke is the third leading cause of death in the US and a major cause of permanent disability.
Stroke refers to both hemorrhagic events, such as intracerebral or subarachnoid hemorrhage, and to ischemic infarction of the brain. |
|
|
35. Hemorrhagic conversion
|
Sometimes ischemic strokes can cause blood vessels to become fragile and rupture, leading to secondary hemorrhagic conversion.
|
|
|
36. Mechanisms of ischemic stroke
|
Ischemic stroke occurs when there is inadequate blood supply to a region of the brain for enough time to cause infarction (death) of brain tissue.
In clinical practice, a distinction is often made between embolic and thrombotic infarcts. |
|
|
37. Embolic infarcts
|
A piece of material (usually a blood clot) is formed in one place and then travels through the bloodstream to suddenly lodge in and occlude a blood vessel supplying the brain.
|
|
|
38. Thrombotic infarct
|
In thrombotic infarcts, a blood clot is formed locally on the blood vessel wall, ususally at the site of an underlying atherosclerotic plaque, causing the vessel to occlude.
Embolic infarcts are considered to occur suddenly with maximal deficits at onset, while thrombotic infarcts may have a more stuttering course. |
|
|
49. Large-vessel infarcts
|
Large-vessel infarcts involve the major blood vessels on the surface of the brain, such as the MCA and its main branches.
Large-vessel infarcts are most often caused by emboli, although thrombosis can also occasionally occur, esp in large proximal vessels such as the vertebral, basilar, and carotid arteries. |
|
|
40. Small-vessel infarcts
|
Small vessel infarcts involve the small penetrating vessels that supply deep structures.
In the cerebral hemispheres these include the basal ganglia, thalamus, and internal capsule, while in the brainstem these include the medial portions of the midbrain, pons, and medulla. Small-vessel infarcts are sometimes also called lacunar infarcts b/c they resemble small lakes or cavities when the brain is examined on pathologic section. |
|
|
41. Dissection of the carotid or vertebral arteries
|
Often results in thrombus formation, which can embolize to the brain.
|
|
|
42. Patent foramen ovale and embolus
|
Sometimes, a patent foramen ovale can allow a thromboembolus formed in the venous system to bypass the lungs and pass directly from the right to the left side of the heart, reaching the brain.
|
|
|
43. Lypohalinosis
|
In hypertension, small penetrating vessels become occluded by a pathologic process known as lipohyalinosis.
|
|
|
44. Ataxic hemiparesis
|
In ataxic hemiparesis, the ataxia is caused by damage to proprioceptive or cerebellar circuitry rather than by damage to the cerebellum itself.
|
|
|
45. Thalamic lacunes vs. basal ganglia lacunes
|
Thalamic lacunes can cause contralateral somatosensory deficits, sometimes followed by a thalamic pain syndrome.
Basal ganglia lacunes can occasionally cause movement disorders such as hemibalismus. |
|
|
46. Cortical lesions
|
Corical lesions can be differentiated from subcortical lesions by the presence of cortical signs.
These signs include aphasia, neglect, homonymous visual field defects, and cortical sensory loss. |
|
|
47. Headaches in ischemic strokes
|
Headache occurs in 25-30% of ischemic strokes. When the headache is unilateral, it is more commonly on the side of the infarct, although exceptions do occur.
Headache may be more common for posterior than for anterior circulation infarcts, and is often seen in dissection of the carotid or vertebral arteries. |
|
|
48. Summary of emboli, lacunes, and thrombosis...
|
1. Emboli usually cause large-vessel infarcts involving cerebral or (less commonly) cerebellar cortex, with sudden onset of maximal deficits.
2. Lacunes are small-vessel infarcts usually seen in chronic hypertension, commonly affecting the deep white matter and nuclei of the cerebral hemispheres and brainstem. 3. Thrombosis occasionally occurs in large proximal vessels such as vertebral, basilar, and carotid arteries and may also contribute to lacunar infarction. |
|
|
49. Common stroke risk factors
|
1. Hypertension
2. Diabetes 3. Hypercholesterolemia 4. Cigarette smoking 5. Positive family history 6. Cardiac disease (valvular disease, atrial fibrillation, patent foramen ovale, low ejection fraction) 7. Prior history of stroke or other vascular disease |
|
|
50. Hypercoagulation and strokes
|
Less commonly, several other systemic medical conditions may affect the coagulation pathways or work through other mechanisms to increase both thrombotic and embolic infarcts.
These hypercoagulate states also increase the risk for venous thrombosis. |
|
|
51. Ischemic strokes in young patients
|
Ischemic stroke is relatively uncommon in young individuals b/c the cumulative effects of the major stroke risk factors tend to worsen with age.
When stroke does occur in a young patient, conditions such as arterial dissection, patent foramen ovale, or the hypercoagulable states should be considered. |
|
|
52. Diagnostic workup of ischemic stroke and TIA
|
Prompt medical attention allows early therapeutic interventions that improve outcome.
When the history and exam suggest a possible ischemic event, an imaging study of the brain should be done immediately to rule out hemorrhage. Remember that an infarct will often not be visible on the CT scan, especially if it is done within a few hours of symptoms onset; however, a hemorrhage will almost always be visible. Meanwhile, routine blood chemistries, cell counts, and coagulation studies should be sent. |
|
|
53. Treatment of ischemic stroke
|
Once a hemorrhage has been ruled out by CT, many physicians treat patients with thrombolytic agents, such as t-PA in acute ischemic stroke.
This treatment has been demonstrated to be effective and it improves the chances of a good functional outcome if given within 3 hours of stroke onset; however, it does carry increased risk of intracranial hemorrhage. |
|
|
54. What do you give patients that are not eligible for t-PA treatment, or those patients who have had a TIA?
|
Heparin anticoagulation is often used while further diagnostic studies are being performed.
As with t-PA, it is essential to rule out the presence of intracranial hemorrhage before administering this treatment. |
|
|
55. Intra-arterial thrombolysis
|
This is performed by catheterization of the occluded vessel, which allows direct administration of the thrombolytic agent to the thrombus.
|
|
|
56. Hyperglycemia in acute stroke
|
Hyperglycemia should be corrected in acute stroke b/c it can worsen infarctions, possibly by increasing local tissue acidosis and blood-brain barrier permeability.
|
|
|
57. How does one assess blood flow in the major cranial and neck vessels?
|
Blood flow in the major cranial and neck vessels should be assessed with Doppler ultrasound and/or magnetic resonance angiography.
This is aprticularly important in suspected internal carotid artery stenosis, since carotid enarterectomy may be required. Conventional angiography may be needed in cases where the degree of stenosis is uncertain based on these invasive tests. |
|
|
58. Patients with atrial fibrillation and stroke
|
Patients with atrial fibrillation are at increased risk of embolic stroke, and that this risk is significantly reduced when they are treated with Coumadin oral anticoagulation.
|
|
|
59. Hemicraniectomy
|
In patients with large MCA infarcts, there may be substantial edema and mass effect, which can sometimes lead to herniation and death.
One therapeutic measure that is being investigated for such patients in hemicraniectomy, in which a portion of skull is temporarily removed over the region of swelling and is later replaced after the danger of herniation has passed. |
|
|
60. What is the most common cause of stenosis in the internal carotid artery just beyond the carotid bifurcation?
|
Atherosclerotic disease commonly leads to stenosis of the internal carotid artery just beyond the carotid bifurcation.
Thrombi formed on a stenotic internal carotid artery can embolize distally, giving rise to TIAs or infarcts of various carotid branches, esp the MCA, ACA, and ophthalmic artery. |
|
|
61. Carotid stenosis symptoms
|
Carotid stenosis is associated with MCA territory symptoms such as contralateral face-arm or face-arm-leg weakness, contralateral sensory changes, contralateral visual field defects, aphasia, or neglect.
In addition, there may be ophthalmic artery symptoms such as ipsilateral monocular visual loss, and ACA territory symptoms such as contralateral leg weakness. |
|
|
62. How can one assess the severity of a carotid stenosis?
|
Can be estimated noninvasively with Doppler ultrasound and MRA, although conventional angiography remains the gold standard.
|
|
|
63. Carotid endarterectomy
|
Treatment for symptomatic carotid stenosis. In this procedure the carotid artery is exposed surgically and temporarily clamped.
A longitudinal incision is made in the artery, and atheromatous material is shelled out from the internal carotid lumen, eliminating the stenosis. |
|
|
64. Carotid occlusion
|
Sometimes an internal carotid artery can gradually or suddenly become 100% occluded, causing infarcts in the MCA, ACA, or ACA-MCA watershed territories.
Carotid occlusion may be completely asymptomatic if there is sufficient collateral flow via the anterior or posterior communicating arteries. |
|
|
65. Common location of carotid occlusions
|
The occlusion usually occurs just beyond the carotid bifurcation, and the vessel then becomes filled with thrombus up to the level of the ophthalmic artery, which is perfused by collateral flow.
Emboli may become dislodged from the top of the thrombus and cause TIAs or strokes. |
|
|
66. Treatment for carotid occlusions
|
In contrast to carotid stenosis, endarterectomy is not usually performed in cases of 100% carotid occlusion b/c of the risk of dislodging more emboli, and b/c the procedure has no proven benefit.
|
|
|
67. Random cause for infarction with carotid stenosis
|
A sudden drop in systemic BP - leads to infarction in the ACA-MCA watershed territory.
|
|
|
68. Carotid dissection
|
Head or neck trauam, and sometimes even minor events can cause a small tear to form on the intimal surface of the carotid or vertebrate arteries.
This may allow blood to burrow into the vessel wall, producing a dissection. A flap then protrudes into the vessel lumen, under which thrombus forms that can embolize distally. |
|
|
69. Symptoms of a carotid dissection
|
Patients with a carotid dissection may describe feeling or hearing a pop at the onset.
They may hear a turbulent sound with each heartbeat and have an ipsilateral Horner's syndrome and pain over the eye. |
|
|
70. Vertebral dissection
|
In a vertebral dissection, there is often posterior neck and occipital pain.
Sometimes dissection, particularly of the vertebral artery, leads to formation of a pseudoaneurysm that may rarely rupture, causing subarachnoid hemorrhage. |
|
|
71. Vertebral vs. carotid dissection infarct locations
|
TIAs or infarcts occur in the anterior circulation with carotid dissection.
They occur in the posterior circulation with vertebral dissection. |
|
|
72. Treatment of dissections
|
Dissection is usually treated with IV heparin followed by oral Coumadin to prevent thromboembolic events.
|
|
|
73. Sagittal sinus thrombosis
|
Sagittal sinus thrombosis is often associated with one of the hypercoagulable states. It occurs with increased frequency in pregnant women and within the first few weeks post partum.
Obstruction of the venous drainage usually causes elevated ICP. In addition, the increased venous pressure can decrease cerebral perfusion, leading to infarcts. Seizures are common. Patients often have headaches and papilledema, and they may have depressed level of consciousness. Treatment is usually with anticoagulation therapy, although this is controversial when hemorrhage has occurred. |
|
|
74. Where do the superficial veins of the brain drain?
|
The superficial veins drain mainly into the superior sagittal sinus and the cavernous sinus.
|
|
|
75. Where do the deep veins of the brain drain?
|
The deep veins of the brain drain into the great vein of Galen.
Ultimately, nearly all venous drainage for the brain reaches the internal jugular veins. |
|
|
76. Cavernous sinus
|
The cavernous sinus is a plexus of veins located on either side of the sella turcica that surrounds portions of the internal carotid artery and CN III, IV, V, and VI.
The cavernous sinus drains via the superior petrosal sinus into the transverse sinus, and via the inferior petrosal sinus into the internal jugular vein. |
|
|
77. The confluence of the sinuses (AKA torcular Herophili)
|
The confluence of sinuses occurs where the superior sagittal, straight, and occipital sinuses join together and are drained by the transverse sinuses.
The torcula is often shaped in such a manner that most blood from the superior sagittal sinus enters the right transverse sinus, while most blood from the straight sinus enters the left transverse sinus. |
|
|
78. What are the five major cortical veins?
|
1. Inferior anastomotic vein of Labbe, which drains into the transverse sinus
2. Superior anastomotic vein of Trolard, which drains into the superior sagittal sinus 3. Superficial middle cerebral vein, which drains into the cavernous sinus 4. Anterior cerebral veins* 5. Deep middle cerebral veins* *Drains into the basal veins of Rosenthal, which then join the internal cerebral veins to form the great vein of Galen |
|
|
79. Left MCA superior division infarct
|
Left MCA superior division infarct
1. Right face and arm weakness of the upper motor neuron type 2. Nonfluent, or Broca's, aphasia 3. In some cases there may also be some right face and arm cortical type sensory loss. |
|
|
80. Left MCA inferior division infarct
|
Left MCA inferior division infarct
1. Fluent, or Wernicke's aphasia 2. Right visual field deficit 3. There may also be some right face and arm cortical type sensory loss. 4. Motor findings are usually absent, and patients may initially seem confused or crazy, but otherwise intact, unless carefully examined. 5. Some mild right sided weakness may be present, especially at the onset of symptoms. |
|
|
81. Left MCA deep territory infarct
|
Left MCA deep territory infarct
1. Right pure motor hemiparesis of the upper motor neuron type. 2. Larger infarcts may produce cortical deficits as well, i.e. aphasia. |
|
|
82. Left MCA stem infarct
|
Left MCA stem infarct
Combo of above with: 1. Right hemiplegia 2. Right hemianesthesia 3. Right homonymous hemianopia 4. Global aphasia 5. There is often a left gaze preference, especially at the onset, caused by damage to the left hemisphere cortical areas important for driving the eyes to the right. |
|
|
83. Right MCA superior division infarct
|
Right MCA superior division infarct
1. Left face and arm weakness of the upper motor neuron type 2. Left hemineglect is present to a variable extent. 3. In some cases there may also be come left face and arm cortical type sensory loss |
|
|
84. Right MCA inferior division infarct
|
Right MCA inferior division infarct
1. Profound left hemineglect 2. Left visual field and somatosensory deficits are often present, however, these may be difficult to test convincingly b/c of the neglect. 3. Motor neglect w/decreased voluntary or spontaneous initiation of movements on the left side can also occur. However, even patients with left motor neglect usually have normal strength on their left side, as evidenced by occasional spontaneous movements or purposeful withdrawal from pain. 4. Some mild right-sided weakness may be present. 5. There is often a right gaze preference, especially at onset. |
|
|
85. Right MCA deep territory infarct
|
Right MCA deep territory infarct
1. Left pure motor hemiparesis of the upper motor neuron type. 2. Larger infarcts may produce "cortical" deficits as well, such as left hemineglect. |
|
|
86. Right MCA stem infarct
|
Right MCA stem infarct
Combo of the above with: 1. Left hemiplegia 2. Left hemianesthesia 3. Left homonymous hemianopia 4. Profound left hemineglect 5. There is usually a right gaze preference, especially at the onset, caused by damage to right hemisphere cortical areas important for driving the eyes to the left. |
|
|
87. Left ACA infarct
|
Left ACA infarct
1. Right leg weakness of the upper motor neuron type 2. Right leg cortical type sensory loss 3. Grasp reflex, frontal lobe behavioral abnormalities, and transcortical aphasia can also be seen. 4. Larger infarcts may cause right hemiplegia |
|
|
88. Right ACA infarct
|
Right ACA infarct
1. Left leg weakness of the upper motor neuron type 2. Left leg cortical type sensory loss 3. Grasp reflex, frontal lobe behavioral abnormalities, and left hemineglect can also be seen. 4. Larger infarcts may cause left hemiplegia |
|
|
89. Left PCA infarct
|
Left PCA infarct
1. Right homonymous hemianopia 2. Extension to the splenium of the corpus callosum can cause alexia without agraphia 3. Larger infarcts including the thalamus and internal capsule may cause aphasia, right hemisensory loss, and right hemiparesis |
|
|
90. Right PCA infarct
|
Right PCA infarct
1. Left homonymous hemianopia 2. Larger infarcts including the thalamus and internal capsule may cause left hemisensory loss and left hemiparesis. |
|
|
91. Pure motor hemiparesis or dysarthia hemiparesis
|
Pure motor hemiparesis or dysarthia hemiparesis
Clinical features: Unilateral face, arm, and leg upper motor neuron type weakenss, with dysarthria. Locations: Posterior limb of internal capsule*, ventral pons*, conona radiata, cerebral peduncle *Most common |
|
|
92. Ataxic hemiparesis
|
Ataxic hemiparesis
Clinical features: Same as pure motor hemiparesis, but with ataxia on same side as weakness Location: Same as pure motor hemiparesis |
|
|
93. Pure sensory stroke (thalamic lacune)
|
Pure sensory stroke (thalamic lacune)
Clinical features: Sensory loss to all primary modalities in the contralateral face and body Location: VPL nucleus of the thalamus |
|
|
94. Sensorimotor stroke (thalamocapsular lacune)
|
Sensorimotor stroke (thalamocapsular lacune)
Clinical features: Combination of thalamic lacune and pure motor hemiparesis Locations: Posterior limb of the internal capsule, and either thalamic VPL or thalamic somatosensory radiation |
|
|
95. Basal ganglia lacune
|
Basal ganglia lacune
Clinical features: Usually asymptomatic, but may cause hemiballismus (involuntary flinging motions of the extremities) Locations: Caudate, putamen, globus pallidus, or subthalamic nucleus |
|
|
96. 1. Profound weakness of the left leg, with mild weakness of the left arm and face, mild dysarthria, left leg hyperreflexia, and Babinski's sign
2. Left grasp reflex and motor impersistence 3. Left arm "out of control" 4. Unawareness of left sided weakness and abrasions, decreased response to pinprick on the left, tactile extinction on the left. |
Dx: Embolic stroke causing an infarct in the right medial frontal lobe including foot motor cortex and supplementary motor area would be caused by occlusion of the right anterior cerebral artery.
In sum, right ACA infarct |
|
|
97. Right homonymous hemianopia and left retro-orbital headache
|
PCA infarct which caused a left primary visual cortex infarct
|
|
|
98. 1. Right handed weakness and speech difficult "mixing up words"
2. Dim blurry vision in the left eye 3. Right leg suddenly gave out 4. High-pitched bruit audible over the left carotid artery |
Very tight stenosis of the left internal carotid artery.
|
|
|
99. Decreased movements of right face (sparing forehead), profound right arm weakness, and mild right leg weakness
Also has nonfluent (Broca's) aphasia |
Left MCA superior division infarct causing infarcts in the left primary motor face and arm areas, Broca's area, and adjacent left frontal cortex.
|
|
|
100. 1. Fluent aphasia with impaired comprehension and repetition
2. Blink to threat present only on the left 3. Greater grimace in response to pinprick on the left side than the right 4. Slightly increased tone in the right arm, with right Babinski's sign |
Left MCA inferior division infarct causing lesions int he left temporal and parietal lobes, including Wernicke's area, optic radiations and somatosensory cortex.
|
|
|
101. Dysarthria and right face, arm, and leg paralysis with a right Babinski's sign
|
This is pure motor hemiplegia.
Most likely resulted from an ischemic infarct of the internal capsule. Internal capsule infarcts are most commonly caused by occlusion of the lenticulostriate arteries, which take their origin from the proximal MCA and supply the deep MCA territories. |
|
|
102. 1. Right face, arm, and leg paralysis, w/right hyperreflexia and Babinski's sign
2. No response to pain on the right side except for weak flexion of the right leg 3. Global aphasia 4. No blink to threat on the right 5. Left gaze preference 6. Decreased right corneal reflex |
Left MCA stem infarct
|
|
|
103. 1. Left facial weakness sparing the forehead, left arm weakness, and hyperreflexia
2. Mild dysarthria 3. Occasional extinction on the left side to double simultaneous visual or tactile stimulation |
Right MCA superior division infarct
|
|
|
104. 1. Anosognosia
2. Left visual neglect 3. Extinction on the left to double simultaneous tactile stimulation 4. Moving the hand to the right of the page 5. Decreased spontaneous movements on the left side 6. Right gaze preference 7. No blink to threat on the left 8. Decreased spontaneous movements on the left side, with mildly decreased left nasolabial fold, and slightly brisker reflexes on the left |
TIA followed by ischemic infarct of the right temporoparietal lobe which is supplied by the right MCA inferior division.
|
|
|
105. 1. Anasognosia, hemiasomatognosia
2. Left face, arm, and leg plegia with left Babinski's sign 3. No blink to threat on the left 4. No voluntary gaze to the left past the midline 5. No response to pinprick on the left side |
Right MCA stem infarct
|
|
|
106. 1. Weakness of the proximal left arm and leg, with left hyperreflexia and Babinski's sign
2. Unsteady gait, veering to the left 3. Decreased leftward fast phases of optokinetic nystagmus 4. Right carotid bruit |
Acute infarct in the right ACA-MCA watershed territory
|
|
|
107. 1. Right frontal headache
2. Weakness of the left face and arm more than the left, with left Babinski's sign 3. Mildly decreased light touch, pinprick, temp, vibration and joint position sense on the left side, with decreased left stereognosis and graphesthesia 4. Left visual and tactile extinction |
Hemorrhage in the parietal lobe extending to the face and arm regions of the precentral gyrus.
|
|
|
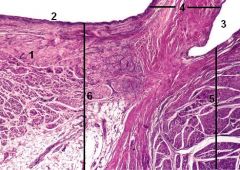
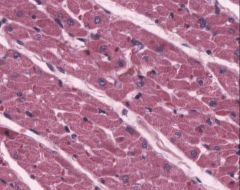
Heart, atrioventricular septum
1. Purkinje fibers 2. Squamous epithelium of endocardium 3. Squamous epithelium of endocardium 4. Mitral valve 5. Ventricular wall 6. Atrial wall |
|
|
Heart, atrioventricular septum
1. Purkinje fibers 2. Intercalated disks 3. Subendocardial DCT 4. Smooth muscle fibers 5. Endocardial DCT |
|
|
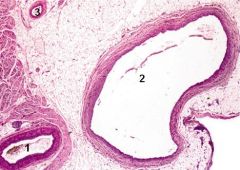
Heart, atrioventricular septum
1. Coronary artery 2. Coronary vein 3. Smaller arterial vessel |
|

|
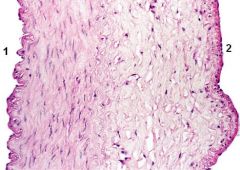
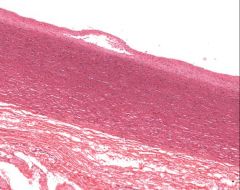
Aorta - longitudinal section
Elastic artery; The three layers can usually be recognized |
|

|
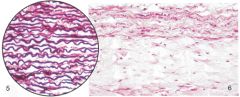
Aorta stained in resorcin-fuchsin on the left
Aorta showing higher magnification of tunica media on the right. Note that the tunica media contains an abundance of smooth muscle; and a lot of elastic material. |
|
|
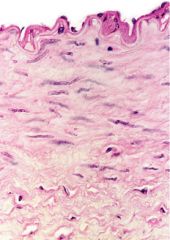
Left shows closer examination of the tunica media of the aorta
Right shows the outermost layer of the aorta; the tunica adventitia. The tunica adventitia (on bottom part of right pic) contains mostly collagenous fibers that course in longitudinal spirals |
|
|
Muscular (medium) artery and vein
1. Arterial endothelium 2. Venous endothelium |
|
|
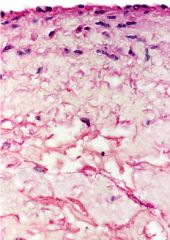
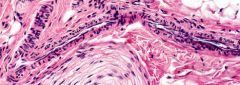
Muscular artery
|
|
|
Medium vein
|
|
|
1. Venule
2. Arterioles 3. Small peripheral nerve |
|
|
Arteriole
|
|

|
Lymphatic vessel
1. Valve 2. Lymph 3. Dense irregular CT |
|
|
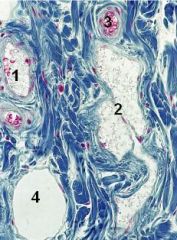
Lymphatic vessel stained with Mallory blue
1. Venule 2. Lymphatic valve 3. Arteriole 4. Adipocyte |
|
|
Vasa vasorum in the tunica adventitia of large arteries (contains a system of vessels)
|
|
|
Vena cava
|
|
|
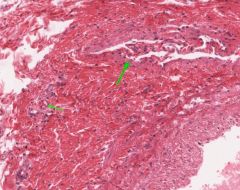
Ventricle stained with Mallory stain.
|
|
|
Aorta - elastic artery
|
|

|
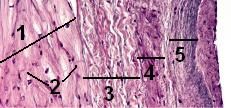
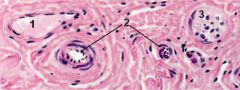
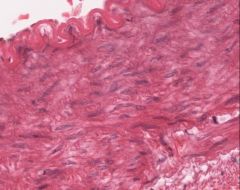
Mitral valve
1. Atrial side 2. Ventricular side 3. Ventrcularis 4. Fibrosa 5. Spongiosa |
|
|
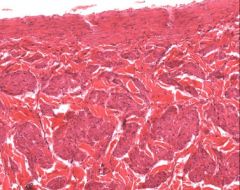
Muscular - medium artery
|

