![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
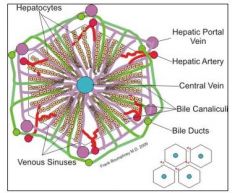
describe the liver structure of the hepatic lobule
|
|
|
|
what percentage of the blood supply enters the liver through the portal vein and hepatic artery
|
- 30-40% via hepatic artery |
|
|
describe how blood passes through the liver
|
2. passes through acinar zone / periportal (closest to afferent blood supply) 3. passes through acinar zone 2/ midzonal 4. passes through zone 3/centrilobular 5. leaves via the terminal hepatic vein to the caudal vena cava |
|
|
what defences does the liver have
|
- rib cage - Kupffer cells |
|
|
what are Kupffer cells
|
- important in endotoxin removal from portal blood |
|
|
what defences does the biliary tree have
|
- terminal sphincter in front of common bile duct that stops parasites/bacteria passing down into liver |
|
|
what problems can affect the portals of entry to the liver
|
2. haematogenous entry of parasites/bacteria which ends up in the sinusoid and causes Kupffer cell localisation 3. retrograde biliary transport (going backwards) which creates ascending parasitic or bacterial infectious gain access |
|
|
give an example of liver damage in bovines
|
bovine traumatic reticuloperitonitis with abscessation due to liver damge by eg small wires or nails causing direct extension from GIT
|
|
|
how do poisonous plants like ragwort cause liver damage
|
they contain alkaloids which are converted to pyrrolic esters by cytochrome P450 enzymes |
|
|
which species are mmost susceptible to ragwort toxicity
|
pigs>cattle/horses> sheep |
|
|
what would a cell with ragwort toxicity look like histologically
|
|
|
|
describe how liver abscesses are formed in cattle
|
leads to lactic acidosis leads to ruminitis -bacteria accumulate and pass to the portal vein this causes hepatocellular necrosis, hepatic abscesses and hepatitis |
|
|
how is the liver damaged in navel ill in calves
|
1. bacterial contamination of navel at birth 2. infection tracks up umbilical cord 3. causes multiple hepatic abscesses |
|
|
what are the mechanisms of liver injury
|
- stimulation of autoimmunity - stimulation of apoptosis - disruption of calcium homeostasis due to cell surface blebbing and lysis - canalicular injury (bile travels in caniculae) - mitochondrial injury
|
|
|
what are the main targets of liver injury
|
|
|
|
what cellular changes occur with sub-lethal/reversible injury
|
- cell atrophy (cell shrinkage) |
|
|
what cellular changes occur with lethal?irreversible injury
|
- apoptosis - doesnt stimulate any cell response |
|
|
what are the three patterns of hepatocellular degeneration and necrosis
|
2. zonal 3. massive |
|
|
what cellular changes are seen with random neccrosis
|
- single cell/small number of affected cells - viruses, bacteria, protozoa
|
|
|
what are the characteristics of zonal necrosis
|
- specific zones degenerate - mainly in centrilobular zone |
|
|
what are the characteristics of massive necrosis
|
- effects entire lobule of liver (but not whole liver) or contiguous lobules (lobules next to each other) |
|
|
where are random hepatocellular necrosis like herpesvirus most common
|
neonates/foetuses since the cant thermoregulate |
|
|
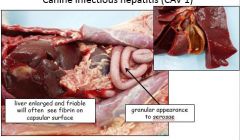
how would a liver with canine infectious hepatitis (CAV1) appear
|
|
|
|
why does zonal necrosis most often occur in the centrilobular zone
|
this area recieves the least oxygenated blood so is susceptible to hypoxia and has the greatest enzymatic activity which activate compounds to toxic forms |
|
|
what are possible causes of zonal necrosis
|
severe anaemia, right siided heart failure, passive congestion of liver which causes hypoxia due to blood stasis |
|
|
what do hepatic circulatory disturbances cause
|
passive venous congestion due to increased pressure in the hepatic veins and venules relative to the portal venules |
|
|
what are the possible causes of hepatic circulatory disturbances
|
- partial obstruction of larger hepatic veins or caudal vena cava |
|
|
hepatic circulatory disturbances can cause acute passive congestion what are the features of this
|
sudden engorgement with blood which can then cause anaphylaxis, shock or euthanasia |
|
|
hepatic circulatory disturbances can cause chronic passive congestion, what are the features of this |

- pale swollen periportal hepatocytes with fatty degeneration |
|
|
what is massive necrosis
|
necrosis of an entire lobule or neighbouring lobules |
|
|
what would a liver with massive necrosis look like
|
- histologically - areas of haemorrhage and connective tissue late - liver small with wrinkled capsule - histologically - collapsed lobule with stroma and collagen replacing hepatocytes |
|
|
give an example of massive necrosis
|
leptospirosis |
|
|
disturbances to bile flow and icterus can cause hepatic injury, how would the liver normally appear
|
yellow/brown, green/brown |
|
|
what are the 5 stages of the normal metabolism and elimination of bilirubin
|
2. extrahepatic bilirubin is bound to serum forming a bilirubin-albumin complex which is delivered to the liver 3. hepatocellular uptake 4. glucuronidation in the ER - products are water soluble and readily excreted in bile 5. gut bacteria deconjugate bilirubin and degrade it to the colourless urobilinogens whichh are excreted in urine and faeces |
|
|
how can the portals of entry to the biliary system be damaged
|
by haematogenous entry of parasites from blood by retrograde biliary transport which gives access to bacterial or parasitic infections |
|
|
what is cholangiohepatitis
|
a disease starting in the biliary system and spreading to the liver parenchyma |
|
|
what can liver fluke cause
|
ectasis (dilation of a hollow organ) stenosis (abnormal narrowing of a passage in the body) |
|
|
how does the liver respond to injury
|
- fibrosis - biliary hyperplasia |
|
|
how can the pattern of fibrosis suggest the underlying cause of the liver damage
|
- periportal fibrosis = chronic inflammatory changes |
|
|
what is cirrhosis |
scarring/fibrosis of the liver due to long term liver damage with hyperplastic nodule formation |
|
|
what are the causes of cirrhosis
|
- inflammation - bile duct obstruction - right sided heart failure - inherited metabolism disorders - idiopathic |
|
|
how does cirrhosis lead to oedema
|
1. causes decreased albumin production 2. leads to hypoproteinaemia 3.leads to decreased oncotic pressure 4. oedema |

