![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
|
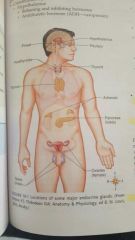
major endocrine glands |
|
|
functions of endocrine glands |
secrete hormones directly to blood |
|
|
function of exocrine glands |
secrete into a duct, such as mucus, serous gland or pancreatic digestive enzymes |
|
|
hormones are |
chemical messengers that are classified by action, source or chemical structures |
|
|
hormones that affect blood glucose levels |
insulin, glucagon, epinephrine, cortisol and growth hormone |
|
|
hypothalamus, oxytocin, pituitary, thymus, thyroid, parathyroid, adrenal cortex, adrenal medulla, pancreas, pineal gland, ovaries and testis are... |
how hormones are classified by source |
|
|
steroid and nonsteroid are... |
how hormones are classified by chemical structures |
|
|
lipids that enter cell and nucleus and act directly in nucleus to engage in transcription (messenger RNA) |
steroids |
|
|
need second messenger system to finally activate formation of mRNA |
nonsteroid |
|
|
the release of hormones from glands is most frequently controlled by |
negative feedback |
|

|
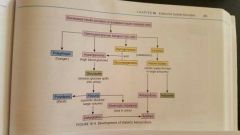
negative feedback mechanism with glucose, insulin and glucagon |
|
|
hypothalamic-releasing hormones |
source= hypothalamus primary effects = stimuli to anterior pituitary to release specific hormone |
|
|
hypothalamic-inhibiting hormones |
source= hypothalamus primary effects = decrease release of specific hormone by anterior pituitary |
|
|
growth hormone (GH, somatotropin) |
source= pituitary anterior lobe (adenohypophysis) primary effects = stimulates protein synthesis |
|
|
adrenocorticotropic hormone (ACTH) |
source= adenohypophysis primary effects = stimulates adrenal cortex to secrete primary cortisol |
|
|
thyroid stimulating hormone (TSH) |
source = adenohypophysis primary effects = stimulates thyroid glad |
|
|
follicle stimulating hormone |
source= adenohypophysis primary effects = (women) stimulates growth of ovarian follicles and estrogen secretion (men) stimulates sperm production |
|
|
luteinizing hormone (LH) |
source= adenohypophysis primary effects = (women) stimulates maturation of ovum and ovulation (men) stimulates secretion of testosterone |
|
|
prolactin (PRL) |
source = adenohypophysis primary effects = stimulates breast milk production during lactation |
|
|
antidiuretic hormone (ADH or vasopression) |
source= post pituitary (neurohypophysis) primary effects = increases reabsorption of H2O by kidneys |
|
|
oxytocin (OT) |
source= neurohypophysis primary effects = stimulates contraction of uterus after delivery and stimulates breast milk ejection during lactation |
|
|
insulin |
source = pancreas (beta cells of islets of Langerhans ) primary effects = transport of glucose and other substances into cells lowers blood glucose levels |
|
|
glucagon |
source = pancreas (alpha cells) primary effects = glycogenolysis in liver. increases blood glucose levels |
|
|
parathyroid hormone (PTH) |
source = parathyroid gland primary effects = increases blood calcium levels by stimulating bone demineralization and increasing absorption of calcium in digestive tract and kidneys |
|
|
calcitonin |
source = thyroid glad primary effects = decrease release of calcium from bone to lower blood calcium levels |
|
|
thyroxine (T4) and triiodothyronine (T3) |
source = thyroid gland primary effects= increases metabolic rate in all cells |
|
|
aldosterone |
source= adrenal cortex primary effects = increases sodium and water reabsorption in kidneys |
|
|
cortisol |
source= adrenal cortex primary effects= anti inflammatory and decreases immune response catabolic effect on tissue; stress response |
|
|
norepinephrine |
source = adrenal medulla primary effects = general vasoconstriction |
|
|
epinephrine |
source = adrenal medulla primary effects = stress response. visceral and cutaneous vasoconstriction. vasodilation of skeletal muscle. increase rate and force of heart contractions. bronchodilation |
|
|
those hormones of anterior pituitary gland that affect growth, nutrition, or function of other endocrine glands. (ex: TRH, ACTH) |
Tropic hormones |
|
|
hormones formed by tissues outside normal endocrine site of production. (ex: adrenocorticotropic hormone produced by bronchogenic carcinoma) |
ectopic hormone |
|
|
insulin is what kind of hormone |
anabolic hormone |
|
|
building up or synthesis of complex substances from simple molecules |
anabolic |
|
|
insulin defect results in |
abnormal carbohydrate, protein, and fat metabolism because the transport of glucose and amino acids into cells is impaired, as well as the synthesis of protein and glycogen |
|
|
more severe form of diabetes |
type 1 |
|
|
type 1 diabetes |
absolute deficit of insulin |
|
|
acute complications most likely to occur with type 1 diabetes |
hypoglycemia or ketoacidosis |
|
|
type 1 diabetes is major factor predisposing... |
strokes (cerebrovascular accident), myocardial infarction, peripheral vascular disease, amputation, kidney failure and blindness |
|
|
diabetes based on decreased effectiveness of insulin or relative deficit of insulin |
type 2 |
|
|
decreased pancreatic beta cell production of insulin, increased resistance by body cells to insulin, increased production of glucose by liver |
types of abnormalities involved with type 2 diabetes |
|
|
how is type 2 diabetes controlled? |
regulating dietary intake increase use of glucose, such as with exercise reduce insulin resistance stimulating beta cells of pancreas to produce more insulin |
|
|
early manifestation of type 2 |
diabetes prediabetes |
|
|
slow onset type 1 autoimmune diabetes |
latent autoimmune diabetes in adults |
|
|
rare form of diabetes caused by mutation in an autosomal dominant gene |
maturity onset diabetes of the young |
|
|
diabetes not related to blood sugar levels, but an insensitivity of kidneys to ADH |
diabetes insipidus |
|

|
general comparison of type 1 and type 2 diabetes |
|
|
sequence of events for an insulin defect |
1. initial stage 2. progressive effects |
|
|
initial stage of insulin defect |
1. results in decreased transportation and use of glucose in many cells 2. hyperglycemia 3. glucosuria 4. polyuria due to glucose in urine exerting osmotic pressure in filtrate, resulting in large volume of urine to be excreted with loss of Na and K 5. fluid loss through urine and high blood glucose levels draw water from cells, resulting in dehydration 6. dehydration causes polydipsia 7. polyphagia due to lack of nutrients in cells |
|
|
progressive effects of insulin defect |
1. diabetic ketoacidosis (more common in type 1) 2. ketonuria 3. as dehydration develops, glomerular filtration rate in kidneys is decreased, and excretion of acids is more limited, resulting in decompensated metabolic acidosis 4. diabetic coma |
|
|
lack of glucose in cells results in |
catabolism of fats and proteins |
|
|
catabolism of fats and proteins leads to |
excessive amounts of fatty acids and their metabolites, known as ketones or ketoacids in blood |
|
|
treatment for diabetes |
1. diet and exercise 2. oral medication to increase insulin secretion or reduce insulin resistance 3. insulin replacement |
|
|
risk of exercising too much with diabetes |
hypoglycemia |
|
|
diabetes complications may result from |
variations of diet and exercise, presence of infection or alcohol use. |
|
|
acute complications |
1. hypoglycemia (insulin shock) causes defect of glucose in blood (usually occurs in type 1) 2. hypoglycemia affects nervous system, because neurons can't use fats or proteins as energy source |
|
|
1 group of signs related to impaired neurologic functions resulting from hypoglycemia |
poor coordination, slurred speech, poor concentration, staggering gait |
|
|
second group of signs related to hypoglycemia stimulating sympathetic nervous system |
increased pulse rate, pale moist skin, anxiety and tremors |
|
|
if hypoglycemia is left untreated can lead to |
loss of consciousness, seizures and death |
|

|
hypoglycemic shock |
|
|
development of ketoacidosis |
|
|
S&S of DKA are related to |
dehydration, metabolic acidosis and electrolyte imbalance |
|
|
ketoacidosis leads to |
kussmaul respiration, acetone breath (sweet fruity smell) , lethargy, decreased responsiveness, depression of CNS, and decreased blood flow |
|
|
hyperosmolar hyperglycemic nonketotic coma develops frequently in patients with |
type 2 diabetes |
|
|
chronic complications |
vascular problems infections cataracts |
|
|
capillary basement membranes become thick and hard, causing obstruction or rupture of capillaries and small arteries, resulting in tissue necrosis and loss of function |
microangiopathy |
|
|
leading cause of blindness for diabetic patient |
retinopathy |
|
|
diabetic nephropathy, or vascular degeneration in kidney glomeruli eventually leads to |
chronic renal failure |
|
|
affects large arteries, leading to high incidences of heart attack, strokes, and peripheral vascular disease in diabetics |
macroangiopathy |
|
|
obstruction of arteries in legs frequently results in |
ulcers on feet and legs that are slow to heal |
|
|
peripheral neuropathy leads to |
impaired sensation, numbness, tingling, weakness and muscle wasting |
|
|
neuropathy results from |
ischemia and altered metabolic processes |
|

|
diabetic retinopathy in eye |
|

|
retina from a case of advanced diabetic microangiopathy showing several aneurysms |
|

|
diabetic nephrosclerosis in bisected kidney |
|

|
neuropathic diabetic foot ulcer |
|
|
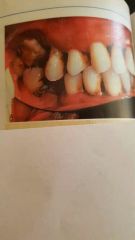
periodontal disease in diabetic |
|

|
candidiasis in right axilla with satellite pustules |
|

|
potential complications of diabetes mellitus |
|
|
hypoparathyroidism leads to |
hypocalcemia |
|
|
hypocalcemia affects |
nerve and muscle functions |
|
|
hypocalcemia results in |
weak cardiac muscle contractions and increased excitability of nerves, leading to skeletal muscle twitch |
|
|
hyperparathyroidism may be caused by |
adenoma, hyperplasia or secondary renal failure |
|
|
hyperparathyroidism causes |
hypercalcemia |
|
|
hypercalcemia leads to |
forceful cardiac contractions and predisposition to kidney stones |
|
|
increased parathyroid hormone (PTH) causes calcium to |
leave bone, leading to osteoporosis, weakening bone so it fractures easily |
|
|
most common cause of pituitary disorders |
benign adenomas |
|
|
diabetes insipidus results from |
deficit of ADH |
|
|
inappropriate antidiuretic hormone syndrome is due to |
excess ADH |
|
|
thyroid disorders may result from |
pituitary or thyroid gland dysfunction |
|
|
enlargement of thyroid gland, visible on anterior neck |
goiter |
|
|
goiters are caused by |
various hypothyroid and hyperthyroid conditions |
|
|
low iodine levels is related to |
hypothyroid condition, and leads to low T3 and T4 production and increase in TSH from pituitary, producing hyperplasia and hypertrophy in thyroid gland |
|
|
hyperthyroid condition resulting from hyperactivity of thyroid gland, perhaps due to excessive stipulation by TSH, which produces large nodular gland |
toxic goiter |
|
|
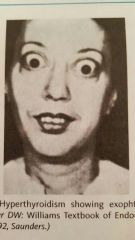
graves' disease is form of |
hyperthyroidism, with increased T3 and T4 secretions |
|

|
hypothalamus-pituitary-thyroid gland feedback mechanism with thyroid hormone |
|
|
acute situation in a patient with uncontrolled hyperthyroidism, usually precipitated by infection or surgery |
thyroid storm or thyrotoxic crisis |
|
|
why is thyroid storm life threatening? |
because results in hyperthermia, tachycardia, heart failure and delirium |
|

|
general comparison of hypothyroidism and hyperthyroidism |
|
|
hyperthyroidism showing exophtalmos |
|
|
type of hypothyroidism that is a destructive autoimmune disorder |
hashimoto's thyroiditis |
|
|
severe hypothyroidism in adults, nonpitting edema |
myxedema |
|
|
acute hypothyroidism resulting in hypotension, hypoglycemia, hypothermia, loss of consciousness, life threatening complication |
myxedema coma |
|
|
benign tumor of adrenal medulla that secretes epinephrine, norepinephrine, and sometimes other substances |
pheochromocytoma |
|
|
disease caused by excessive amount of glucocorticoids (e.g. hydrocortisone or cortisol) |
cushings syndrome |
|
|
excess glucocorticoids may result from |
*adrenal adenoma *pituitary adenoma (cushings disease) *etopic carcinoma that causes paraneoplastic syndrome *iatrogenic conditions, such as administration of large amount of glucocorticoids for many chronic inflammatory conditions |
|
|
essential for stress response and essential for life |
glucocorticoids |
|
|
characteristic physical changes with cushings syndrome |
1. moon face 2. buffalo hump 3. fragile skin 4. osteoporosis 5. increased gluconeogenesis and insulin resistance (leads to glucose intolerance and then diabetes) 6. retention of sodium and water (leading to hypertension, edema, and possibly hyperkalemia) 7. suppressed immune response and inflammatory response 8. stimulating erythrocyte production 9. emotional lability and euphoria |
|
|
disease caused by deficiency of adrenocortical secretions, the glucocorticoids, mineralcorticoids, and androgens |
Addisons disease |
|
|
major effects of hormonal defects of Addisons disease |
decreased blood glucose levels, poor stress response, fatigue, weight loss, and frequent infections |
|
|
what results from mineralcorticoid (aldosterone) defect, which could lead to cardiac arrhythmia and failure? |
low serum sodium concentration, decreased blood volume, and hypotension, accompanied by high potassium levels |
|
|
other manifestations of Addisons disease |
decreased body hair due to lack of androgens and hyperpigmentation in extremities, skin creases, buccal mucosa, and tongue, because of increased ACTH resulting from low cortisol secretion |
|

|
cushings syndrome, adrenal cortical adenoma |
|

|
cushings syndrome causes and feedback effects |
|

|
typical appearance of person with cushings syndrome |
|

|
early signs of insulin defect |
|

|
progressive signs of insulin defect |
|

|
vascular problems with diabetes |

