![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
What immune cells (and subsets) are infected by HIV?
|
CD4+ T-cells (Th1, Th2)
Macrophages / Dendritic cells |
|
|
What cells are directly destroyed (through the lytic cycle) by HIV?
|
CD4+ T-Cells
(Indirectly destroyed through cytotoxic immune system) |
|
|
Which cells acts as a "reservoir" for viral replication?
|
Macrophages
|
|
|
Which cell transports HIV to lymphoid tissue?
|
Macrophages
Dendritic cells |
|
|
What are the three main transmission routes of HIV?
Which two have the highest "act risk" for acquisition of HIV? What is advocated in reducing the risk of spreading HIV through sexual transmission? |
1. Sexual Route
2. Blood or Blood Product Route (includes needle Sharing (IDU) 3. Mother-to-Child Transmission 2 Highest Risk: Mother-to-Child Transmission, and Blood or Blood Product route Teaching Safe Sex!!!! |
|
|
What is the risk of transmitting AIDS though saliva, tears, and urine? Why?
|
No documented account of transmitting AIDS through saliva, tears, or urine unless there is a significant amount of blood and direct contact of this.
|
|
|
What roles do the following play in the "binding, fusion, and infection" steps in the life cycle of HIV:
GP120, GP41, co-receptors CCR5, CXCR4, and CD4? |
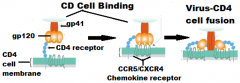
Binding:
HIV gp120 "docks" to CD4 cell (CCR5) or macrophage (CXCR4) Fusion: -gp120 pulled away -underlying gp41 "sticks" into cell membrane Infection: -HIV RNA, Reverse Transcriptase, Protease, Integrase enters the cell |
|
|
What specific roles do the following enzymes play in the HIV life cycle:
reverse transcriptase |
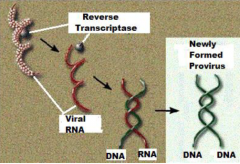
single strands viral RNA --->> double stranded DNA
|
|
|
What specific roles do the following enzymes play in the HIV life cycle:
Integrase |
Integrase: insert viral DNA into host cell genome
|
|
|
What specific roles do the following enzymes play in the HIV life cycle:
Protease |
AFTER transcription/translation of viral DNA
Protease: "slices and dices" the long HIV protein |
|
|
From the original infection, what is the usual period time before the clinical manifestations of aids occurs?
Can this time period be shorter? |
Left untreated: 8 to 10 yrs, but can be 2 yrs or less
~10% succumb to AIDS, 2 to 3 yrs. |
|
|
What are the three factors that can effect the period of time until onset of AIDs ?
|
1. Nature of the exposure
(route, size of microbial inoculum) 2. "Virulence" of the microbe 3. Host immune status |
|
|
In what two phases of the course of AIDs is an infected person the most contagious? Why?
|
Phase 1 and 3
b/c of the HIV levels are the HIGHEST |
|
|
How do fusion inhibitors differ from reverse transcriptase inhibitors and anti proteases in terms "before/after" infection?
|
Before:
Fusion inhibitors blocked HIV to hook up to CD4 chemokine receptor After: Reverse transcriptase inhibitors and anit-protease prevents the process once the virus gets into the cells by preventing it from killing the CD4 cells. |
|
|
What 4 surface proteins do fusion inhibitors attach to?
|
gp120/gp41
CCR5/CXCR4 |
|
|
Why will the treatment of one RT inhibitor not continue to work over time?
|
generations of HIV
result in mutated strains Resistance develops after 6mo -1yr of drug use |
|
|
Explain how protease inhibitors work.
|
Protease inhibitors block the action of protease and prevents the "Slicing and dicing" of long proteins into HIV functional proteins. Used with a combination with reverse transcriptase inhibitors.
|
|
|
Explain how integrase inhibitors work.
|
Integrase inhibitors block the action of integrase and prevents the incorporation of the viral genome into the target cell genome.
|
|
|
Explain HAART
|
Highly Active Anti-Retroviral Therapy (HAART): combo. of several antiretroviral drugs (3 or 4, with combo of 2-3 types of RTs and protease)
|
|
|
During HAART therapy, what happens to the levels of HIV?
Are these persons still infectious? |
The use of HAART regimen of drugs can lead to undetectable levels of HIV in the bloodstream.
There is still is HIV in genital secretions so these people are still infectious. |
|
|
What are the three phases on the graph included in the graph?
|
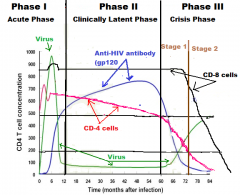
Phase 1: Acute
Phase 2: Clinically Latent Phase 3: Crisis |
|
|
For phase 1: changes that are occurring and why for
CD4+ T Cell |
1. Initial rise in CD4 Cells (activiation of specific Th1 and Th2 against HIV, thus mounting both humoral and cytotoxic immune response)
2. Fall (destruction of CD4 by HIV though the lytic cycle) 3. Then a rise back to almost normal #'s (bone marrow activated to replace CD4 cells killed by HIV) |
|
|
For phase 1: changes that are occurring and why for
CD8 T cell |
1. Acutely rise due to activation of specific CD8 cells by Th1 against HIV
2. This "spike" will return to normal as the serum HIV declines |
|
|
For phase 1: changes that are occurring and why for
Anit-HIV CP120 antibodies |
1.It takes 3-4 months following initial infection for these antibodies to appear in the blood at high enough concentrations to be measured.
2. Begins to rise as humoral immune response is activated |
|
|
For phase 1: changes that are occurring and why for
HIV Blood/body fluid levels |
1. Immediately after infection, virus titer rises and 6 months into this phase, virus titers are very high
2. Strong cell-mediated and humoral mounted against HIV, the virus largely disappears from the circulation by the end of the first phase |
|
|
For phase 2: changes that are occurring and why for
CD4+ T Cell |
1. 5% or more are being killed, which about 1 trillion, A DAY!!
2. (bone marrow) is being severely stressed and over time, the immune system is slowly being annihilated |
|
|
For phase 2: changes that are occurring and why for
CD8 T Cell |
1. As long as there are sufficient amount of viable CD4 Th1 cells to activate the CD8 t cell, the levels of these will remain at the normal levels
|
|
|
For phase 2: changes that are occurring and why for
Anti-HIV GP120 |
1. if there are sufficient amount of viable CD4 Th2 cells to activate the B, these antibodies will remain high
|
|
|
For phase 2: changes that are occurring and why for
HIV blood/fluid levels |
HIV blood levels stay constant, at a low level
|
|
|
For phase 3 (Stage 1): changes that are occurring and why for
CD4+ T Cell |
1. CD4 cells fall below 500 per cu mm and cont. to fall towards 200 per cu mm
|
|
|
For phase 3 (Stage 1): changes that are occurring and why for
CD8 T Cell |
1. CD8 expansions persist, and absolute #'s of CD8 cells stay relatively normal
|
|
|
For phase 3 (Stage 1): changes that are occurring and why for
Anti-HIV GP120 Antibodies |
1. As Th2 CD4 cells drop, the levels of anti-HIV gp 120 antibody dramatically drop
2. Humoral arm of the immune system is becoming non-functional |
|
|
For phase 3 (Stage 1): changes that are occurring and why for
HIV blood/body fluid levels |
1. As CD4+ drops, significant rise in of HIV viral components in the blood and body fluid
|
|
|
For phase 3 (Stage 2): changes that are occurring and why for
CD4+ T Cell |
CD4 cells fall below 200 mm^3 and the immune system, for all the extent and purposes ceases to function
|
|
|
For phase 3 (Stage 2): changes that are occurring and why for
CD8 T Cell |
All CD8+ T Cell #'s begin to fall, which includes memory CD8+ T cells to other pathogens besides HIV
|
|
|
For phase 3 (Stage 2): changes that are occurring and why for
Anti-HIV GP120 Antibodies |
When Th2 CD4 cells drop below 200 mm^3, the levels of anti-HIV gp 120 antibody in the patient's is low to almost non-existent
|
|
|
For phase 3 (Stage 2):changes that are occurring and why for
HIV blood/body fluid levels |
As the T4 cells fall below 200 per cu mm, virus titers rise rapidly and immune activity drops precipitously
|
|
|
For phase 1, explain the symptoms!!
|
1. Mild "flu like" condition that is self-limiting
2. Half remain asymptomatic during the initial period of infection 3. Symptoms are "not specific" enough to be identified with HIV infection |
|
|
For phase 2, explain the symptoms!!!
|
1. Presence of mild to moderate lymphandenopathy or asymptomatic
|
|
|
For phase 3, Stage 1 explain the symptoms!!
|
1. Weight loss approx. 10% of body weight
2. Chronic diarrhea 3. Recurrent upper respiratory tract infections (bacterial sinusitis, bacterial pneumonia) 4. Oral candidiasis (thrush) 5. Oral hairy leukoplakia |
|
|
For phase 3, Stage 2 explain the symptoms!!!
|
1. Pneumocystis carinii pneumonia
2. Cytomogalovirus disease of liver, spleen, and lymph nodes 3. Candidiasis of esophagus, trachea, bronchi 4. Pulmonary and extrapulmonary tuberculosis 5. Kaposi's Sarcoma |
|
|
Which may be among the first cells to encounter HIV at mucosal surfaces?
|
Epidermal dendritic cells (Langerhans cells)
|
|
|
What exposure route has a 90% chance of infection?
|
Blood or Blood product route
|
|
|
What exposure route has a 25% chance of infection?
|
Mother to Child
|

