![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
:
|
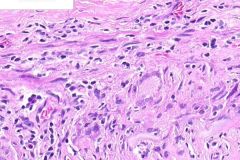
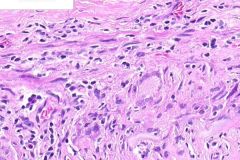
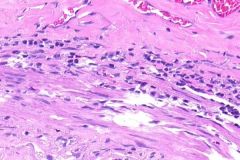
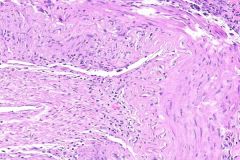
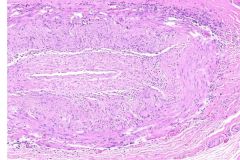
GIANT CELL or TAKAYASU'S ARTERITIS:
This thickening of the temporal arterial wall is associated with chronic inflammatory infiltrate centered in the media, and made of lymphocytes and occasional giant cells. Note the moderate fibrosis of the vessel wall in both areas of acute inflammation and in uninvolved areas, indicative of both a chronic and sporadic disease process. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
:
|
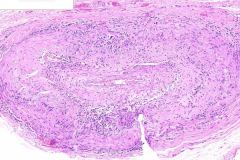
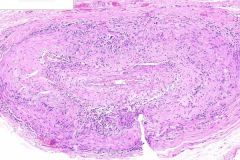
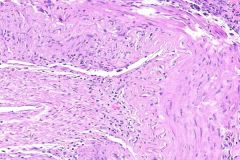
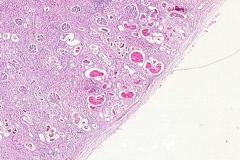
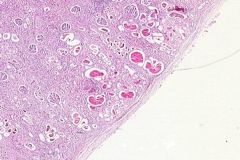
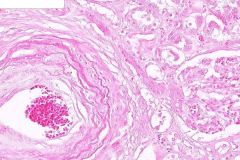
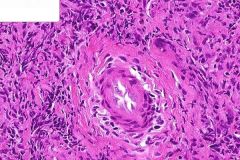
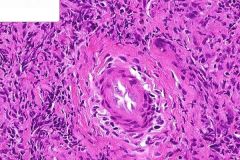
GIANT CELL ARTERITIS:
One of several cross-sections from a temportal artery (do several because even correctly-done biopsies can give false negative results due to the segmental nature of the disease). Note the narrowed vascular lumen, with thickening of the vessel wall. Elastin staining would show multiple areas of disruption of the internal elastic lamina, which is secondary to the inflammation. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
:
|
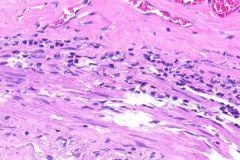
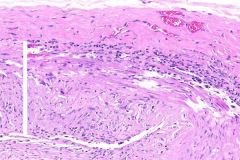
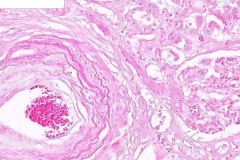
GIANT CELL ARTERITIS:
This thickening of the temporal arterial wall is associated with chronic inflammatory infiltrate centered in the media, and made of lymphocytes and occasional giant cells. Note the moderate fibrosis of the vessel wall in both areas of acute inflammation and in uninvolved areas, indicative of both a chronic and sporadic disease process. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
:
|
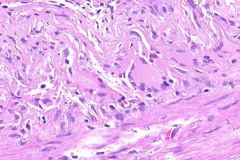
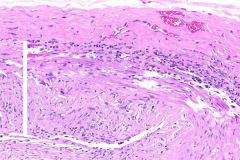
GIANT CELL ARTERITIS:
This thickening of the temporal arterial wall is associated with chronic inflammatory infiltrate centered in the media, and made of lymphocytes and occasional giant cells. Note the moderate fibrosis of the vessel wall in both areas of acute inflammation and in uninvolved areas, indicative of both a chronic and sporadic disease process. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
:
|
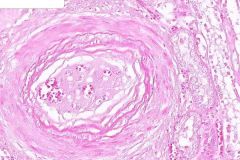
GIANT CELL ARTERITIS:
One of several cross-sections from a temportal artery (do several because even correctly-done biopsies can give false negative results due to the segmental nature of the disease). Note the narrowed vascular lumen, with thickening of the vessel wall. Elastin staining would show multiple areas of disruption of the internal elastic lamina, which is secondary to the inflammation. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
:
|
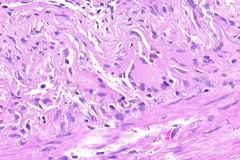
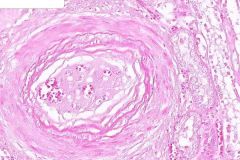
GIANT CELL or TAKAYASU's ARTERITIS:
This thickening of the temporal arterial wall is associated with chronic inflammatory infiltrate centered in the media, and made of lymphocytes and occasional giant cells. Note the moderate fibrosis of the vessel wall in both areas of acute inflammation and in uninvolved areas, indicative of both a chronic and sporadic disease process. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
ID
|
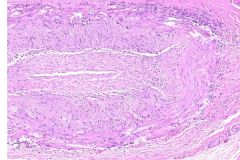
GIANT CELL ARTERITIS:
One of several cross-sections from a temportal artery (do several because even correctly-done biopsies can give false negative results due to the segmental nature of the disease). Note the narrowed vascular lumen, with thickening of the vessel wall. Elastin staining would show multiple areas of disruption of the internal elastic lamina, which is secondary to the inflammation. These histological findings are characteristic of both Giant Cell and Takayasu's arteritis, but clinical features (patient age, vessels involved) would distinguish the two. |
|
ID
|
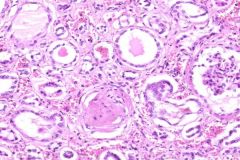
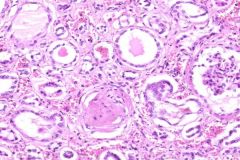
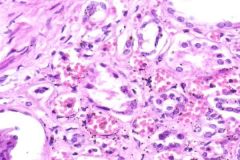
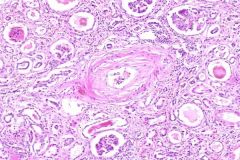
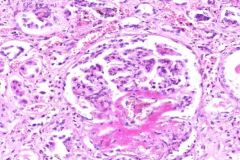
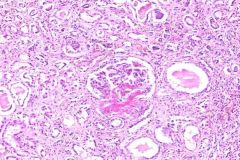
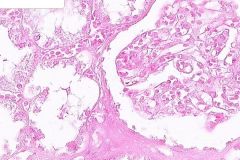
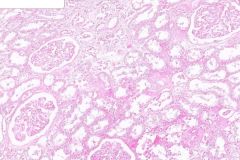
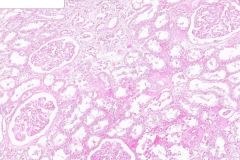
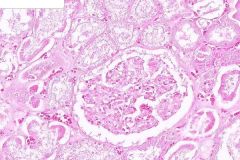
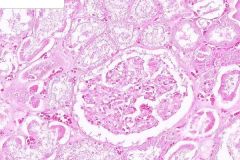
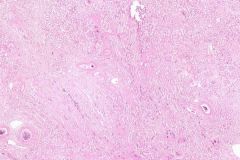
MALIGNANT NEPHROSCLEROSIS:
Note the "smudging" of the walls of the afferent arterioles with walls staining deep pink. Glomeruli often contain patchy, eosinophilic fibrinoid necrosis of the tuft. Some show adhesion between the glomerular capillary and Bowman's Capsule. Some hyalinized glomeruli are also seen. Dilated tubules are found within the cortex and contain eosinophilic (proteinaceous) material, as well as some PMNLs. A small artery show concentric hyperplastic arteriolitis that narrows its lumen. |
|
ID
|
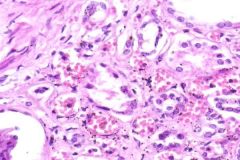
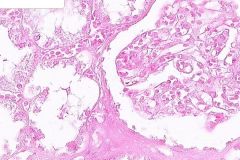
MALIGNANT NEPHROSCLEROSIS:
Dilated tubules containing eosinophilic material. Increased interstitial fibrous tissue with lymphocyte infiltration |
|
ID
|
MALIGNANT NEPHROSCLEROSIS:
ote the "smudging" of the walls of the afferent arterioles with walls staining deep pink. Glomeruli often contain patchy, eosinophilic fibrinoid necrosis of the tuft. Some show adhesion between the glomerular capillary and Bowman's Capsule. Some hyalinized glomeruli are also seen. Dilated tubules are found within the cortex and contain eosinophilic (proteinaceous) material, as well as some PMNLs. A small artery show concentric hyperplastic arteriolitis that narrows its lumen. |
|
ID
|
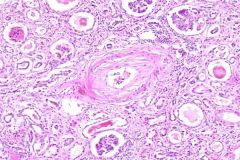
MALIGNANT NEPHROSCLEROSIS:
ote the "smudging" of the walls of the afferent arterioles with walls staining deep pink. Glomeruli often contain patchy, eosinophilic fibrinoid necrosis of the tuft. Some show adhesion between the glomerular capillary and Bowman's Capsule. Some hyalinized glomeruli are also seen. Dilated tubules are found within the cortex and contain eosinophilic (proteinaceous) material, as well as some PMNLs. A small artery show concentric hyperplastic arteriolitis that narrows its lumen. High pressure causes medial hyperplasia, which causes concentric thickening "onion skinning". This further reduces renal blood flow and increased renin results, further increasing blood pressure. Eventually, vascular necrosis leads to interruption in blood flow and infarction. (fatal within a year) |
|
ID
|
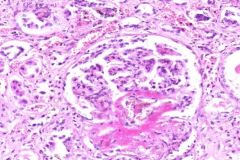
MALIGNANT NEPHROSCLEROSIS:
Glomeruli often contain patchy, eosinophilic fibrinoid necrosis of the tuft. Some show adhesion between the glomerular capillary and Bowman's Capsule. Some hyalinized glomeruli are also seen. Dilated tubules are found within the cortex and contain eosinophilic (proteinaceous) material, as well as some PMNLs. There is an increase in interstitial fibrosis with some lymphocyte infiltration. |
|
ID
|
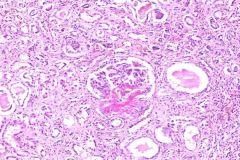
MALIGNANT NEPHROSCLEROSIS:
Note the "smudging" of the walls of the afferent arterioles with walls staining deep pink. Glomeruli often contain patchy, eosinophilic fibrinoid necrosis of the tuft. Some show adhesion between the glomerular capillary and Bowman's Capsule. Some hyalinized glomeruli are also seen. Dilated tubules are found within the cortex and contain eosinophilic (proteinaceous) material, as well as some PMNLs. Some small arteries show concentric hyperplastic arteriolitis that narrows their lumen. There is an increase in interstitial fibrosis with some lymphocyte infiltration. |
|
ID
|
MALIGNANT NEPHROSCLEROSIS:
There is an increase in interstitial fibrous tissue and a slight infiltration of lymphocytes. These are responding to necrotic changes within arterioles and glomeruli and should not be confused with pyelonephritis. |
|
ID
|
MALIGNANT NEPHROSCLEROSIS:
Capsule of the kidney is slightly thickened and infiltrated with lyphocytes. Just beneath it, there are multiple small hemorrhages. There is an increase in interstitial fibrous tissue and a slight infiltration of lymphocytes. These are responding to necrotic changes within arterioles and glomeruli and should not be confused with pyelonephritis. |
|
ID
|
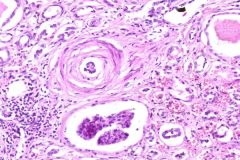
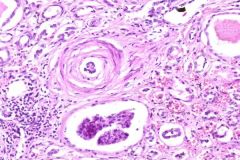
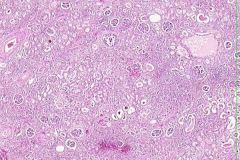
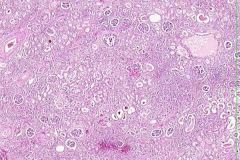
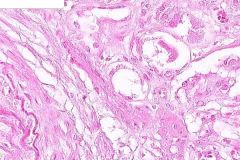
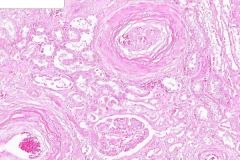
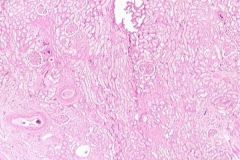
RENAL ARTERIOSCLEROSIS:
The characteristic lesion here is hyaline thickening (deep eosinophilic material in intima or entire wall) of the afferent arteriole entering the glomeruli (arteriosclerosis). Be sure to look in the periphery for this too - recall that glomeruli are spherical, and the afferent arteriole may not have made it into the plane of section. The hyaline thickening of the wall leads to narrowing or obliteration of the lumen. Some glomeruli are totally hyalinized due to ischemia following obliteration of their afferent arteriole. In some cases, eosinophilic material is found in Bowman's Space around the glomerular tuft. |
|
ID
|
RENAL ARTERIOSCLEROSIS:
Note the increase in cortical interstitial fibrosis. In the area of the cortex just beneath the capsule are numerous, dilated tubules containing eosinophilic material (proteinatious casts). A few granular and cellular casts are also found. These tubules are draining the remaining, functioning glomeruli. May or may not see: (In some of the tubules beneath the capsule there are numerous bacteria in colonies. Lack of cellular response to these suggests that they are a postmortem growth.) |
|
ID
|
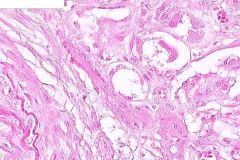
RENAL ARTERIOSCLEROSIS:
The characteristic lesion here is hyaline thickening (deep eosinophilic material in intima or entire wall) of the afferent arteriole entering the glomeruli (arteriosclerosis). Be sure to look in the periphery for this too - recall that glomeruli are spherical, and the afferent arteriole may not have made it into the plane of section. The hyaline thickening of the wall leads to narrowing or obliteration of the lumen. Interstitial fibrosis is also seen. |
|
ID
|
RENAL ARTERIOSCLEROSIS:
The characteristic lesion here is hyaline thickening (deep eosinophilic material in intima or entire wall) of the afferent arteriole entering the glomeruli (arteriosclerosis). Be sure to look in the periphery for this too - recall that glomeruli are spherical, and the afferent arteriole may not have made it into the plane of section. The hyaline thickening of the wall leads to narrowing or obliteration of the lumen. Some glomeruli are totally hyalinized due to ischemia following obliteration of their afferent arteriole. In some cases, eosinophilic material is found in Bowman's Space around the glomerular tuft. Hyalinization of the neighboring small artery as well. |
|
ID
|
RENAL ARTERIOSCLEROSIS:
Hyaline thickening of a small renal artery with surrounding interstitial fibrosis. |
|
ID
|
RENAL ARTERIOSCLEROSIS:
MALIGNANT NEPHROSCLEROSIS: The characteristic lesion here is hyaline thickening (deep eosinophilic material in intima or entire wall) of the afferent arteriole entering the glomeruli (arteriosclerosis). Be sure to look in the periphery for this too - recall that glomeruli are spherical, and the afferent arteriole may not have made it into the plane of section. The hyaline thickening of the wall leads to narrowing or obliteration of the lumen. Some glomeruli are totally hyalinized due to ischemia following obliteration of their afferent arteriole. In some cases, eosinophilic material is found in Bowman's Space around the glomerular tuft. |
|
ID
|
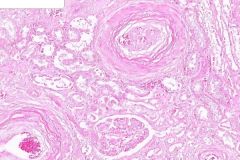
RENAL ARTERIOSCLEROSIS:
he characteristic lesion here is hyaline thickening (deep eosinophilic material in intima or entire wall) of the afferent arteriole entering the glomeruli (arteriosclerosis). Be sure to look in the periphery for this too - recall that glomeruli are spherical, and the afferent arteriole may not have made it into the plane of section. The hyaline thickening of the wall leads to narrowing or obliteration of the lumen. Some glomeruli are totally hyalinized due to ischemia following obliteration of their afferent arteriole. In some cases, eosinophilic material is found in Bowman's Space around the glomerular tuft. Hyalinization of the neighboring small artery as well with interstitial fibrosis surrounding. |
|
ID
|
WEGENER'S GRANULOMATOUS:
Acute and chronic inflammatory cells are present. Vasculitis of medium and small vessels is seen by both acute and chronic inflammatory infiltrate in vessel walls. Note that there is NO fibrinoid necrosis, but chronic changes like intimal and medial fibrosis ARE present. |
|
ID
|
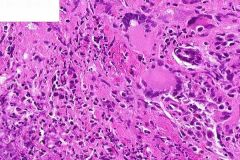
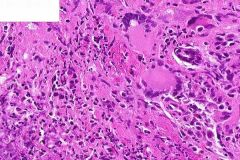
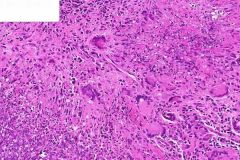
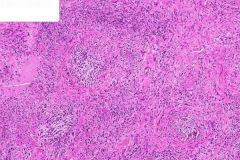
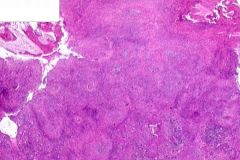
WEGENER'S GRANULOMATOUS:
Don't know the tissue "Classic" example where you can see: 1) giant cells, 2) vasculitis, 3) geographic necrosis. Deep blue is due to inflammatory infiltrate within the CT stroma. Areas of granular, basophilic material represent necrosis (necrobiosis) with no viable cells and degeneration of collagen. The "granulomas" seen are a misnomer. These are not classic granulomas like in TB, but rather collections of histiocytes and fibroblasts with some Giant Cells. Vasculitis of medium and small vessels is seen by both acute and chronic inflammatory infiltrate in vessel walls. Note that there is NO fibrinoid necrosis, but chronic changes like intimal and medial fibrosis ARE present. |
|
ID
|
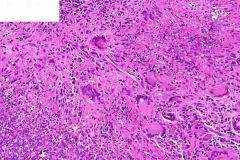
WEGENER'S GRANULOMATOUS:
"Classic" example where you can see: 1) giant cells, 2) vasculitis, 3) geographic necrosis. Admittedly difficult to ID the origin of this tissue: from mucosa or bone. Deep blue is due to inflammatory infiltrate within the CT stroma. Areas of granular, basophilic material represent necrosis (necrobiosis) with no viable cells and degeneration of collagen. The "granulomas" seen are a misnomer. These are not classic granulomas like in TB, but rather collections of histiocytes and fibroblasts with some Giant Cells. Vasculitis of medium and small vessels is seen by both acute and chronic inflammatory infiltrate in vessel walls. |
|
ID
|
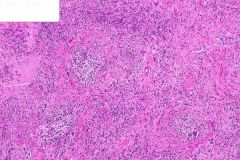
WEGENER'S GRANULOMATOUS:
"Classic" example where you can see: 1) giant cells, 2) vasculitis, 3) geographic necrosis. Admittedly difficult to ID the origin of this tissue: from mucosa or bone. Deep blue is due to inflammatory infiltrate within the CT stroma. Areas of granular, basophilic material represent necrosis (necrobiosis) with no viable cells and degeneration of collagen. The "granulomas" seen are a misnomer. These are not classic granulomas like in TB, but rather collections of histiocytes and fibroblasts with some Giant Cells. Vasculitis of medium and small vessels is seen by both acute and chronic inflammatory infiltrate in vessel walls. |
|
ID
|
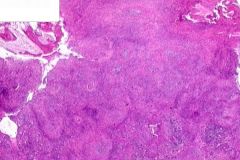
WEGENER'S GRANULOMATOUS:
"Classic" example where you can see: 1) giant cells, 2) vasculitis, 3) geographic necrosis. Admittedly difficult to ID the origin of this tissue: from mucosa or bone. Deep blue is due to inflammatory infiltrate within the CT stroma. Areas of granular, basophilic material represent necrosis (necrobiosis) with no viable cells and degeneration of collagen. The "granulomas" seen are a misnomer. These are not classic granulomas like in TB, but rather collections of histiocytes and fibroblasts with some Giant Cells. Vasculitis of medium and small vessels is seen by both acute and chronic inflammatory infiltrate in vessel walls. |
|
:
|
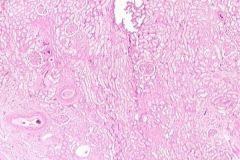
RENAL ARTERIOSCLEROSIS:
The marked narrowing of the cortex is apparent with a thickened and hyalinized renal capsule. The capsule appears adherent to the cortex and stripping it away would tear away fragments of cortical tissue. Just beneath the capsule are numerous dilated tubules containing eosinophilic (proteinatious) casts and some granular and cellular casts. Some of the tubules just beneath the capule contain bacteria in colonies with NO inflammatory response suggesting that this was a postmortem growth. |
|
:
|
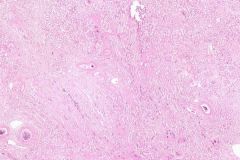
RENAL ARTERIOSCLEROSIS:
The marked narrowing of the cortex is apparent with a thickened and hyalinized renal capsule. The capsule appears adherent to the cortex and stripping it away would tear away fragments of cortical tissue. Just beneath the capsule are numerous dilated tubules containing eosinophilic (proteinatious) casts and some granular and cellular casts. Some of the tubules just beneath the capule contain bacteria in colonies with NO inflammatory response suggesting that this was a postmortem growth. |

