![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What is a cataract
|
An opacifaction of the lens
|
|
|
|
Name 6 substances that are known to cause cataracts
|
Corticosteroids
Phenothiazines Ergot Naphthalene 2,4-dinitrophenol Phospholine iodide (topical) |
None
|
|
|
What 4 physical agents may cause cataracts
|
Ultraviolet light, Trauma, Intraocular surgery, Ultrasound
|
|
|
|
Name 9 systemic diseases associated with cataracts
|
Congenital rubella virus, Diabetes mellitus, Down syndrome, Atopic dermatitis, Scleroderma, Alport syndrome, Cretinism, Fabry disease, Galactosemia
|
|
|
|
What is the most common type of cataract in the US
|
Senile cataract
|
|
|
|
What is presbyopia
|
Often referred to as old age vision, it is a refractive condition associated with aging in which there is diminished power of accommodation resulting from loss of elasticity of the lens
|
|
|
|
At what age does presbyopia usually occur
|
Occurs in most persons after 40-50 years of age
|
|
|
|
What is the ultimate result of presbyopia
|
People begin to have difficulty reading and require spectacles for near vision
|
|
|
|
What is keratitis
|
Inflammation of the cornea secondary to an infectious or mechanical etiology
|
|
|
|
Name 5 infectious agents frequently involved in keratitis
|
Staphylococcus, Streptococcus, Pseudomonas, Herpes virus, Chlamydia
|
|
|
|
What predisposes the cornea to infection
|
Exposure or trauma
|
|
|
|
What is the treatment for corneal opacities secondary to scarring
|
Corneal transplant
|
|
|
|
What is the most common complaint of a patient suffering from a corneal abrasion
|
Pain
|
|
|
|
What is used to diagnose a corneal abrasion
|
Fluorescein test
|
|
|
|
What is band keratopathy
|
Calcium phosphate depositions in a horizontal band across the superficial central cornea
|
|
|
|
With what condition is band keratopathy usually seen
|
Hypercalcemia
|
|
|
|
What is the pathognomonic ocular finding in Wilson disease
|
Kayser-Fleishcer rings—golden rings of copper deposits in Descemet membrane of the cornea
|
|
|
|
What percent of untreated Wilson disease patients with neurologic symptoms have Kayser-Fleischer rings
|
100%, eventually
|
|
|
|
What ophthalmologic procedure helps visualize Kayser-Fleischer rings
|
A slit-lamp examination
|
|
|
|
What is retinal detachment
|
A separation of the neurosensory retina from the pigment epithelium and its supportive choroid, resulting in retinal infarction
|
|
|
|
What is the pathophysiology of retinal detachment
|
Damage to the retina allows fluid to collect in the subretinal space
|
|
|
|
Name 4 causes of retinal detachment
|
Age, Trauma, Ocular surgery, Diabetes
|
|
|
|
What are common complaints of a patient with a detached retina
|
Floaters, blind spots, and flashing lights
|
|
|
|
What is the treatment of choice for retinal detachment
|
Surgery, either sclera bucking therapy or vitrectomy
|
|
|
|
What is retinitis pigmentosa
|
Hereditary, progressive retinal degeneration in both eyes
|
|
|
|
Name 3 symptoms of retinitis pigmentosa
|
Night blindness (usually in childhood)
Loss of peripheral vision, progressing over many years to tunnel vision Eventual night blindness |
None
|
|
|
What is retinoblastoma
|
Hereditary, malignant intraocular tumor of retinal cells
|
|
|
|
What is the most common childhood ocular malignancy and what is its incidence
|
Retinoblastoma, affecting 1:20,000 to 1:34,000 children
|
|
|
|
Name 5 presenting signs of retinoblastoma
|
White pupil (leukocoria)
Squint (strabismus) Poor vision Spontaneous hyphema (blood in the anterior chamber of the eye) Red, painful eye |
None
|
|
|
What is diabetic retinopathy
|
A progressive microangiopathy of the blood vessels of the retina in diabetic patients
|
|
|
|
Name and describe the 2 types of diabetic retinopathy
|
Non-proliferative (background): retinoscopic hemorrhages without neovascularization
Proliferative: advanced retinoscopic vascular changes with neovascularization |
None
|
|
|
What is the most common complaint with diabetic retinopathy
|
Decreased visual acuity
|
None
|
|
|
What are 2 modalities used for diagnosis of diabetic retinopathy
|
Retinoscopy; Fluorescein angiogram
|
|
|
|
In severe cases of diabetic retinopathy, what is the treatment of choice
|
Photocoagulation with argon laser to peripheral retina
|
|
|
|
What is hypertensive retinopathy
|
Retinal changes caused by high blood pressure
|
|
|
|
Name 6 features of hypertensive retinopathy
|
Arteriolar narrowing
Copper wiring: dull light reflections from blood vessel surfaces Flame-shaped hemorrhages: hemorrhages in the retinal nerve fiber layer Exudates: often radiating from the center of the macula (macular star) Cotton-wool spots: fluffy white bodies (infarctions) in the superficial retina Microaneurysms |
None
|
|
|
What is a cherry-red spot
|
An apparent color change in the retinal area of sharpest vision (fovea) that results from the opacification of the retinal layers around it
|
|
|
|
Name two conditions in which cherry-red spots are seen
|
Central retinal artery occlusion; Tay-Sachs disease
|
|
|
|
What is glaucoma
|
An ocular disease complex characterized by increased intraocular pressure
|
|
|
|
What are 3 classifications of glaucoma
|
Chronic open angle glaucoma; Narrow angle glaucoma; Congential glaucoma
|
|
|
|
Name the 3 types of chronic open angle glaucoma and identify the most common type
|
Bilateral; Insidious; Slowly progressive. Slowly progressive is the most common type and accounts for 90% of the cases of chronic open angle glaucoma
|
|
|
|
What is the pathophysiology of glaucoma
|
Increased intraocular pressure (caused by either increased intraocular aqueous humor production or decreased outflow of aqueous humor) leads to optic nerve degeneration
|
|
|
|
Glaucoma is diagnosed by what 3 modalities
|
Increased intraocular pressure; Retinoscopy (optic disc cupping); Peripheral vision field testing
|
|
|
|
How is glaucoma treated
|
Intraocular pressure is decreased through topical eye drops, surgery, or both
|
|
|
|
What is papilledema
|
Optic nerve head swelling with engorged blood vessels
|
|
|
|
When is papilledema seen
|
With elevated pressure within the skull
|
|
|
|
What is pseudotumor cerebri
|
Intracranial inflammation that resembles a brain tumor
|
|
|
|
Name 4 symptoms associated with pseudotumor cerebri
|
Optic nerve head swelling (papilledema); Headaches; Protrusion of the eyeball (proptosis); Transient loss or reduction in vision
|
|
|
|
Who gets pseudotumor cerebri most frequently
|
Obese women in their 30s
|
|
|
|
What are the 8 signs of serious ocular pathology in a red eye
|
Visual loss; Pain; Opacities; Pupil irregularities; Perilimbal erythema; Increased pressure; History of eye disease; Refractory to treatment
|
|
|
|
What are the clinical signs for bacterial conjunctivitis
|
Conjunctival redness with purulent discharge
|
|
|
|
What are the clinical signs for viral conjunctivitis
|
Conjunctival redness with serous discharge
|
|
|
|
What are the clinical signs for allergic conjunctivitis
|
Conjunctival redness with clear discharge
|
|
|
|
What are the clinical signs for acute narrow angle glaucoma
|
Acute pain, cloudy cornea, perilimbar redness, blurred vision
|
None
|
|
|
What are the clinical signs for iritis
|
Perilimbal redness, irregular pupil, pain, decreased vision
|
|
|
|
What are the clinical signs for corneal ulcer
|
Epithelial defect with infiltrate, pain
|
|
|
|
What are the clinical signs for orbital cellulits
|
Periocular swelling, erythematous ocular surface, decreased vision
|
|
|
|
What is strabismus
|
Misalignment of the eyes
|
|
|
|
Why is it important to correct strabismus
|
To allow proper development of visual acuity and binocular vision
|
|
|
|
What condition develops if strabismus is not corrected
|
Amblyopia
|
|
|
|
Define amblyopia
|
Decreased vision in one or both eyes without detectable anatomic damage in the eye or visual pathways
|
|
|
|
What is optic neuritis
|
Inflammatory demyelination of the optic nerve. It is the most common ocular finding in multiple sclerosis
|
|
|
|
Name 2 symptoms of optic neuritis
|
Blurred vision; Pain on eye movement
|
|
|
|
Characterize the visual acuity in optic neuritis
|
Reduced
|
|
|
|
Will refraction help acuity in optic neuritis
|
No
|
|
|
|
What papillary abnormality occurs in optic neuritis
|
An afferent papillary defect
|
|
|
|
What is an afferent papillary defect
|
Reduced pupilloconstriction on ipsilateral eye illumination with persistence on contralateral illumination
|
|
|
|
What visual field defect is common in optic neuritis
|
A central scotoma
|
|
|
|
What is the name for optic neuritis behind the optic nerve head
|
Retrobulbar neuritis
|
|
|
|
What is the appearance of the optic disc in optic neuritis
|
Pink and swollen with indistinct margin if optic nerve head is involved. In retrobulbar neuritis, the disc is normal
|
|
|
|
What 3 things characterize Horner syndrome
|
Ptosis of the upper eyelid; Miosis: constriction of the pupil; Anhidrosis: absence of sweating on the affected side
|
|
|
|
What causes a Horner syndrome
|
A destructive lesion of the superior cervical ganglion
|
|
|
|
What is xanthomas (xanthelasma)
|
Small yellowish lipid deposits on the eyelids
|
|
|
|
In what 3 conditions are xanthomas commonly seen
|
Familial hypercholesterolemia; Primary biliary cirrhosis; High blood fat levels
|
|
|
|
In what population are xanthomas most common
|
The elderly
|
|
|
|
What is amaurosis fugax
|
Sudden, transient decrease in vision in one eye, varying from visual field constriction to total blindness
|
|
|
|
What causes amaurosis fugax
|
Reduced cerebral circulation resulting in insufficient blood flow to the ophthalmic artery
|
|
|
|
What is keratoconjunctivits sicca
|
Often called dry eye syndrome, it is corneal and conjunctival dryness due to deficient tear secretion
|
|
|
|
What condition is associated with keratoconjunctivitis sicca
|
Sjogren syndrome
|
|
|
|
Define esotropia
|
Eyes turned inward
|
|
|
|
Define exotropia
|
Eyes turned outward
|
|
|
|
Define hypertropia
|
Eyes turned upward
|
|
|
|
Define hypotropia
|
Eyes turned downward
|
|
|
|
Define diplopia
|
Double vision
|
|
|
|
Define blepharitis
|
Inflammation of the eyelids
|
|
|
|
Define hordeolum
|
A suppurative inflammation of a gland of the eyelid
|
|
|
|
Define sty
|
An external hordeolum of the oil glands of Zeis (in the follicles of eyelashes)
|
|
|
|
Define chalazion
|
An internal hordeolum that causes an inflammatory lump in a meibomian gland resulting in a painless swelling in the eyelid
|
|
|
|
Define pinguecula
|
Yellowish, benign conjunctival lump
|
|
|
|
Define pterygium
|
A triangular fold of vascularized conjunctiva that grows horizontally onto the cornea in the shape of an insect wing
|
|
|
|
Define arcus senilis
|
A white ring due to lipid deposition in the peripheral cornea that occurs with aging
|
|
|
|
Define proptosis
|
Abnormal protrusion of bulging forward of the eye
|
|
|
|
Define sympathetic ophthalmia
|
Autoimmune destruction of the contralateral good eye after penetrating injury causes blindness to ipsilateral eye
|
|
|
|
What is the most common ocular finding in multiple sclerosis
|
Optic neuritis
|
|
|
|
What are the clinical features of uveal melanoma
|
Most frequently occuring intraocular tumor in adults
Risk factors UV light History of cutaneous melanoma or multiple nevi Family history of ocular melanoma Light color of the iris Protective features: Black skin, brown iris, glasses |
|
|
|
What is the uveal tract
|
The pigmented vascular coat of the eye consisting of the iris, ciliary body and choroid
|
|
|
|
How does uveal melanoma presents
|
Patient with decreased vision or blindness with an enlarged liver
IF the melanoma occurs in the iris, it may change the color of the iris Late manifestations: Glaucoma, Cataracts, Retinal detachment No pain unless there is associated glaucoma or inflammation |
|
|
|
What location of uveal melanoma is associated with a better prognosis
|
The iris, at this site they are usually detected earlier and may even be resected (not enucleated)
|
|
|
What does this picture demonstrate
|
Uveal melanoma
Fundus photograph of a choroidal tumor. The tumor is out of focus due to the elevation of the mass. This tumor would be classified as large clinically and medium-sized pathologically. Elevation of the retina by the bulging tumor mass may lead to retinal detachment and the absence of transillumination of the lesion. Tumors vary in size and pigmentation. Some melanomas are amelanotic. |
|
|
|
What are the treatment options for uveal melanoma
|
Resection for a few (iris), radiation, enucleation, and chemotherapy (extraocular)
|
|
|
|
What is the most common cause of death from uveal melanoma
|
Liver metastases
Conjuctival melanoma is localized |
|
|

What does this picture demonstrate
|

Uveal melanoma
Fundus photograph of a small tumor with orange pigment on the surface. A dark mass is present beneath the retinal blood vessels. |
|
|

What does this picture demonstrate
|

Uveal melanoma
Malignant melanoma arising from a preexisting nevus in the posterior portion of the choroid. The retina is elevated as the tumor bulges into the vitreous cavity. Malignant melanoma is the most common malignant intraocular tumors. The tumor arises from melanocytes or nevi in the uveal tract. |
|
|
What does this picture demonstrate
|
Uveal melanoma
Malignant melanoma arising from a preexisting nevus in the posterior portion of the choroid. The retina is elevated as the tumor bulges into the vitreous cavity. Malignant melanoma is the most common malignant intraocular tumors. The tumor arises from melanocytes or nevi in the uveal tract. |
|
|
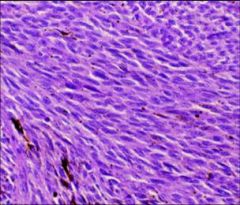
What does this picture demonstrate
|
Uvela melanoma
Histologic types: A (no visible nucleoli) B (prominent nucleoli readily visible) |
|
|
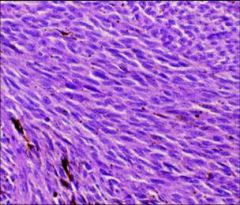
What does this picture demonstrate
|
Uveal melanoma
Histologic types: Epitheliod (polygonal cells with identifiable borders and nucleoli) |
|
|
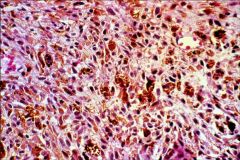
What does this picture demonstrate
|
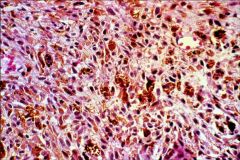
Uveal melanoma
Most tumors are a mixture of the three different types with some necrosis |
|
|
|
With uveal melanoma, what features indicate an adverse prognosis
|
Epitheliod cells
Large size Involvement of the ciliary body Extrasceleral extension Older patient Increased mitotic activity |
|
|
|
What are some infections and inflammatory conditions that affect the uvea
|
Bacterial, Viral, Fungal
Sarcoidosis: uveal involvement is common involving about one-third of patients Sympathetic ophthalmia: autoimmune bilateral granulomatous inflammation secondary to a traumatic injury in one eye. This condition, although rare, arises within a few weeks of the injury. Once the autoimmune response begins, bilateral blindness is usually the final result. The ophthalmologist must decide in a few weeks whether to remove the injured eye to prevent the response. |
|
|
|
With uveal melanoma, what is the pattern of spread and how does it differ from melanoma of the skin
|
Direct extension through the scleral canal
Local metastases through intravascular spread General metastases: hepatic metastases predominate, 95% of uveal melanomas with metastases have liver involvement While melanoma of the skin spreads through the lymphatic channels, uveal melanoma spreads hematogenously because there are no lymphatic channels in the eye |
|
|

What does this picture demonstrate
|

Conjunctival melanoma
Accounts for 5% of ocular melanomas Behaves like typical melanoma of the skin Has propensity for local recurrence |
|
|

What does this picture demonstrate
|

Retinoblastoma
The most frequently occuring intraocular tumor in children On physical exam, leukocoria is present Median age of diagnosis is 2 years in boys and 1 year in girls, if unilateral. Less than 1 year bilateral 70-75% unilateral, of these 10-15% have germline mutation 95% are cured |
|
|

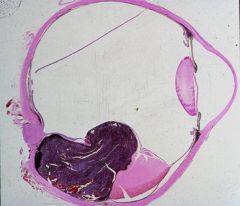
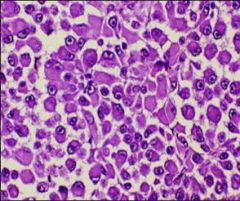
What does this picture demonstrate
|

Retinoblastoma
Note small round blue cells with rosettes Results from defect in RB gene, a tumor suppressor gene at 13q14 Hereditary and nonhereditary forms. Bilateral tumors in hereditary retinoblastoma Believed to arise form neuroepithelial cell in retina Increased risk of osteosarcoma |
|
|
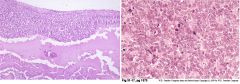
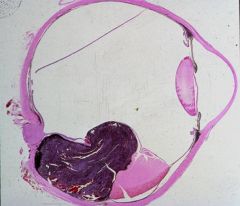
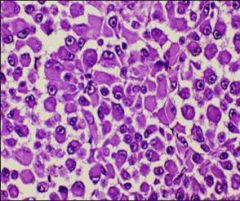
What do these pictures demonstrate
|

Retinoblastoma
Left: Small round blue cells with hyperchromatic nuclei and minimal cytoplasm Right: Flexner Wintersteiner rosettes and numerous mitotic figures |
|

