![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
Defence mechanisms |
Mechanical - ciliated epithelium, mucus, cough Immunological - IgA and antimicrobials in mucus, resident alveolar macrophages and dendritic cells, innate/adaptive immune responses |
|
|
What is the parenchyma? |
The parts of lungs involved in gas transfer including alveoli, interstitium, blood vessels, bronchi and bronchioles |
|
|
Name some categories of pneumonia? |
Community acquired Hospital acquired Health care associated Aspiration associated Immunocompromised host Necrotising/abscess formation |
|
|
Name some community acquired pneumonia pathogens? |
Streptococcal pneumoniae Haemophilus influenzae Moraxella catarrhalis Staphylococcus aureus Klebsiella pneumoniae / Pseudomonas aeurginosa Mycoplasma pneumoniae |
|
|
Hospital acquired / health care associated pneumonia pathogens? |
Gram-negative rods Enterobacteriaceae and pseudomonas Staphylococcus aureus (usually methicillin-resistant) |
|
|
Pneumonia in the immunocompromised host pathogens? |
Cytomegalovirus Pneumocystic jiroveci (PCP) Mycobacterium avium-intracellulare Invasive aspergillosis Invasive candidiasis |
|
|
Necrotising/ abscess formation pathogens |
anaerobes, s. aureus, Klebsiella, S.pyogenes |
|
|
Neutrophil response to infection |
Chemotaxis Degranulation Reactive oxygen species Extracellular traps Phagocytosis |
|
|
Macrophage response to infection |
Cytokine and chemokines Phagocytosis (bacteria and dead cells) Antimicrobial peptides Resolution - also involves T cells, dendritic cells and epithelial cells |
|
|
Clinical presentation |
Cough Sputum Pyrexia Pleuritic chest pain Haemoptysis Dyspnoea Hypoxia |
|
|
General risk factors for inflammation |
Chronic diseases Immunologic deficiency Immunosuppressive agents Leukopaenia |
|
|
Local risk factors for inflammation |
Loss or suppression of cough reflex - drugs injury to mucociliary apparatus - viruses, gases accumulation of secretions - cf, obstruction (tumour) Impaired alveolar macrophages function - alcohol, tobacco Pulmonary congestiion and oedema |
|
|
What is bronchopneumonia? |
Most common pattern Patchy consolidated areas of actue |
|
|
What is lobar pneumonia? |
Rust coloured sputum S.pneumoniae consolidation of a large portion of lobe or entire lobe |
|
|
Local complications of inflammation |
Abscess formation Parapneumonic effusion
|
|
|
Systemic complications of inflammaion |
Sepsis ARDS multi-organ failure |
|
|
What is ARDS? |
Acute respiratory distress syndrome Clinical diagnosis - hypoxia (PaO2/FiO2 < 300mmHg) and non-cardiogenic pulmonary oedema Causes Direct - pneumonia, aspiration, hyperoxia, ventilation Indirect - sepsis, trauma, pancreatitis, acute hepatic failure |
|
|
What is bronchiectasis? |
Permanent dilatation of one or more large bronchi Typically affects 2nd to 8th order of segmental bronchi - largest central airways more robust |
|
|
Pathogenesis of bronchiectasis |
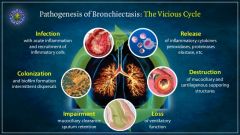
|
|
|
What is traction bronchiectasis? |
Dilatation of airways due to parenchymal fibrosis Inflammation --> new collagen formatiion --> collagen contracts --> loss of lung volume --> pulling open of airways --> airway dilatation |
|
|
What are the four forms of bronchial dilatation? |
They are based on imaging appearances Cyllindrical Saculalr Varicose Cystic |
|
|
Classifying bronchiectasis? |
More useful to think in terms of anatomical distribution of disease Closer linkage w/ aetiologies Types = localised bronchiectasis , diffuse/multifocal bronchiectasis |
|
|
What is localised bronchiectasis?? |
Bronchial obstruction due to neoplasm, foreign body, external compression (middle lobe syndrome), allergic bronchopulmonary aspergillosis Infection - TB or necrotising bacterial/viral infection Gastric acid aspiration Traction bronchiectasis Idiopathic |
|
|
Diffuse or Multifocal bronchiectasis |
Infection Idiopathic Cystic fibrosis - multi system disorder affecting lungs, GI tract loss of function in CTFR altered ion transportation viscous mucoid secretions due to H20 resorption |
|
|
Local complications of bronchiectasis |
Distal airway damage/loss and lung fibrosis pneumonia pulmonary abscess formation haemoptysis airway colonisation by aspergillus aspergilloma tumourlet formation |
|
|
Physiological complications of Bronchiectasis |
Respiratory failure Cor pulmonale |
|
|
Systemic complications of bronciectasis |
Metastatic abscess Amyloid deposition |
|
|
Infection in bronchiectasis |
Impaired bacterial clearance - altered anatomy, thickened mucus, impaired immune cell function Colonisatiion and infection - pseudomonas aeruginosa, Klebsiella, Moraxella, S/pneumoniae, H.influenzae |
|
|
Predisposing factors to Tuberculosis |
Alcoholism Diabetes mellitus HIV/AIDS Some ethnic groups |
|
|
Treatment of tuberculosis |
socio-economic conditions drugs - triple antibiotic therapy prevention - bcg vaccination |
|
|
Primary tuberculosis |
3-4 weeks - M.tuberculosis multiplies wn alveolar macrophages, bacterium resides in phagosomes and carried to regional lymph nodes, from there to circulation 3- weeks - onset of cellular immunity and delayed hypersensitivy Activated lymphocytes further activate macrophages to kill Primary infection arrested in most immunocompetent ppl few bacilli may survive dormant |
|
|
Progressive Primary TB |
Infection not arrested in kids, elderly and immunocompromised tuberculosis bronchopneumonia - infection spreads via bronchi, results in diffuse bronchopneumonia, well developed granulomas do not form Miliary tuberculosis - infection spreads via blood stream, organisms scathy, mulltiple organs - lungs, liver, spleen, kidneys,, meninges, brain |
|
|
Secondary Tuberculosis |
Reactivation of old often subclinical infection 5-10% of primary infection cases More damage due to hypersenstivity apical region of lung tubercles develop locally,, enlarge and merge erode into bronchus and cavities develop may progress to tuberculous bronchopneumonia |
|
|
What is UIP? |
Under interstitial pneumonitis |
|
|
Morphology of UIP |
Subpleural accentuation spatial and temporal hetereogeneity fibroblastic foci mixed inflammatory infiltrate excess alveolar macrophages |
|
|
Lung diseases associated w/ asbestos |
Occupational lung disease Several diseases pleural plaques asbestosis mesothelioma adenocarcinoma |
|
|
What is hypersensitivity pneumonitis
|
Type III hypersensitivity - Ab/Ag complex w/n lung Various causative agents Farmer's lung Pigeon fancier's lung Mushroom picker's lung Hot tub lung Most resolve when agent of exposure removed but can be chronic |

