![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
508 Cards in this Set
- Front
- Back
|
dilation of the ventricles in the brain caused by obstruction within the ventricular system
|
hydrocephalus
|
|
|
what are three etiologies of hydrocephalus?
|
all are obstruction of CSF flow
1. congenital 2. inflammation 3. neoplasia (primary or secondary) |
|
|
why do the ventricles dilate in hydrocephalus?
|
pressure atrophy of the brain
|
|
|
formation of a fluid-filled cavity in the cerebrum caused by necrosis and loss of the nervous tissue
|
porencephaly
|
|
|
a severe form of porencephaly in which most of the white matter is lost and the lateral ventricles expand to fill the space
|
hydranencephaly
|
|
|
what is the most common cause of hydranencephaly/porencephaly?
|
viral infection in utero such as blue tongue virus, border disease, and BVD.
|
|
|
failure of the cerebellum to develop to normal size
|
cerebellar hypoplasia
|
|
|
what is the most common cause of cerebellar hypoplasia in
bovines? cats? |
- bovines: BVD
- cats: panleukopenia virus |
|
|
a calf or kitten with a hypermetric gait, tremors, and loss of balance may have what neurological defect?
|
cerebellar hypoplasia
|
|
|
atrophy of the cerebellum after the organ has developed to normal size. in what animal is this most frequently seen?
|
cerebellar abiotrophy. dogs.
|
|
|
what are two diseases of lambs is caused by copper malnutrition in pregnant sheep?
|
1. swayback (hydranencephaly)
2. enzootic ataxia |
|
|
what is the difference between enzootic ataxia and swayback (both are diseases of lambs caused by copper insufficiency during gestation)?
|
- swayback (hydranencephaly) is necrosis and degeneration of white matter
- enzootic ataxia is axonal degeneration (gray matter) |
|
|
a congenital condition where myelin fails to generate. in what three species is this most common?
|
hypomyelinogenesis
- pigs - dogs - sheep (Border disease) |
|
|
what is border disease? species? clinical signs?
|
- congenital hypomyelinogenesis
- sheep - "hairy shakers." animals that tremor and whose wool looks like hair |
|
|
failure of the spine to close during fetal development
|
spina bifida
|
|
|
what are the two most common lesions caused by spina bifida?
|
1. meningocele - meninges protruding out of the spine
2. meningomyelocele - spinal cord protrudes out of the spine |
|
|
dilation of the central canal of the spinal cord
|
hydromyelia
|
|
|
formation of a fluid-filled cavity in the parenchyma of the spinal cord
|
syringomyelia
|
|
|
what are the two general pathogenic processes of edema in the nervous system?
|
1. intracellular (vasogenic)
2. extracellular (cytotoxic) |
|
|
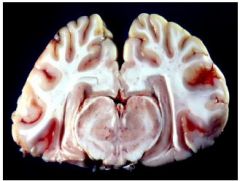
how does the brain look with severe edema?
|
swelling of the brain with flattening of the gyri. the cerebellum is forced into the foramen magnum and becomes narrowed into a cone shape.
|
|
|
what are three etiologies of vasogenic (intracellular) edema of the brain?
|
1. neoplasia
2. inflammation 3. trauma |
|
|
neurologic disease occurring secondarily to liver disease
|
hepatoencephalopathy
|
|
|
what are three etiologies of cytotoxic (extravascular) edema of the brain?
|
1. lead toxicity
2. salt toxicity 3. hepatoencephalopathy |
|
|
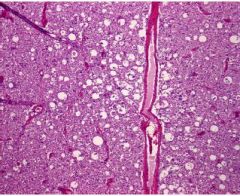
histologically, how does cerebellar hypoplasia compare to a normal cerebellum (H&E stain)?
|
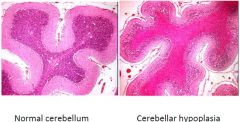
- normal cerebellar gray matter has basophilic axonal bodies and appears blue
- with hypoplasia, the axonal bodies are destroyed and the gray matter stains an eosinophilic pink. |
|
|
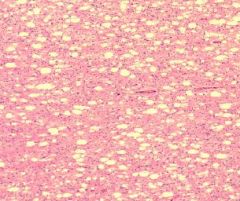
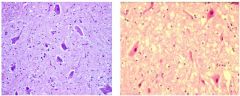
how does hypomyelinogenesis appear histologically (H&E stain)?
|
the normal brain has homogeneously dispersed neurons with clear zones where myelin was before slide preparation. Hypomyelinogenesis appears as distorted clear zones, often with axonal bodies with no myelin.
|
|

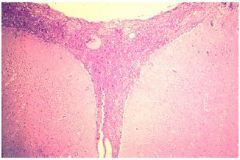
This section of spinal cord has what defect?
|
hydromyelia
|
|

this section of spinal cord has what defect?
|
syringomyelia
|
|
This section of brain has what defect?
|
edema
|
|
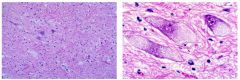
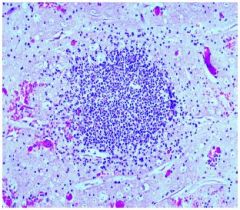
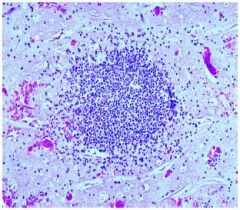
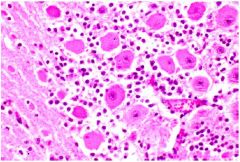
These are two different magnifications of the same brain section. What disease is present?
|
lysosomal storage disease
|
|
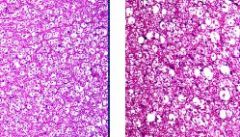
The section of brain on the left is normal. That is wrong with the section on the right?
|
axonal degeneration
|
|
What is wrong with this spinal cord? What is the main etiology of this lesion?
|
Wallerian degeneration (lost axons and demyelination). Usually caused by spinal cord compression.
|
|
what is the difference between the spinal cord section on the left from the section on the right?
|
the left is normal (basophilic), the right is necrotic neurons (eosinophilic)
|
|
the presence of yellow discoloration in the white matter is indicative of what disease?
|
polioencephalomalacia
|
|
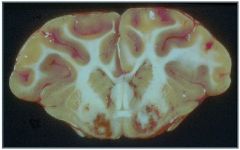
describe the lesions in this brain section. What infectious agent could cause this?
|
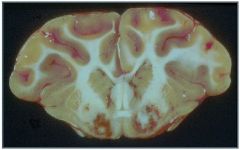
- severe edema and hemorrhage
- swollen gyri - Clostridium perfringens type D |
|
this section of cerebrum is showing what disease?
|
meningitis
|
|

a bacterial infection is causing what lesions in this brain?
|
choroiditis and ependymitis
|
|
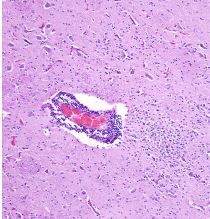
the circle pattern of basophilic dots in this brain section is which type of lesion? what is one infectious agent that can cause this?
|
abscess caused by Listeria monocytogenes
|
|
What lesions are present in this cerebral section? What is the disease and a common causative agent?
|
- thrombosis of the blood vessels
- multiple small abscesses - this is thrombotic meningoencephalitis caused by Histophilus somni |
|
what is the lesion in this brain section? what is it caused by?
|
- lymphocytic and plasma cell perivascular cuffs
- caused by a viral infection |
|
In this brain section, what are the large, eosinophilic lesions called? What causes them?
|
- Negri bodies
- Rabies |
|
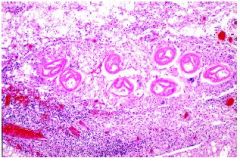
In this section of spinal cord, what are the circular pink lesions?
|
they are a single worm (cut in multiple planes). Paralaphostrongylus tenuis
|
|
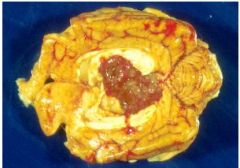
this dorsal section of a brain has what lesion?
|
choroid plexus tumor
|
|
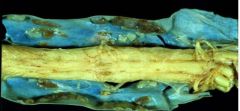
In this sagittal section of the spinal cord, what lesions are present (note that the blue color is an artifact of photography)
|
dura ossification
|
|
|
a sharply delineated pale, tan, or yellow lesion in the brain could be what?
|
infarction
|
|
|
disease of cats of unknown cause that produce areas of infarction and necrosis in the cerebrum
|
feline ischemic encephalopathy
|
|
|
what causes focal infarction in the brain and spinal cord? what are two common causes
|
- emboli
1. bacterial (e.g. Histophilus somni) 2. fibrocartilagenous from rupture of intervertebral disc material |
|
|
an embolus of intervertebral disc material in the spinal cord is called what? what is a clinical sign in animals with this lesion?
|
- fibrocartilagenous embolism
- animals would show posterior paralysis due to infarction of the spinal cord |
|
|
what is the usual cause of hemorrhage in the CNS?
|
trauma
|
|
|
what are two non-traumatic causes of hemorrhage in the CNS?
|
1. leukoencephalomalacia in horses
2. Clostridium perfringens type D in sheep |
|
|
a group of inherited diseases each caused by absence or deficiency of a single enzyme in a pathway that breaks down cellular organelles in lysosomes
|
lysosomal storage diseases
|
|
|
what are the four types of lysosomal storage disease?
|
1. lipidosis
2. mucopolysaccharidosis 3. glycoproteinosis 4. ceroid-lipofuscinosis |
|
|
comment on the Mendelian genetics of lysosomal storage disease
|
it is an autosomal homozygous recessive disease.
|
|
|
besides genetics, what is another common etiology of lysosomal storage disease?
|
ingestion of poisonous plants such as Astragalus (locoweed) or swainsoma.
|
|
|
what are clinical signs associated with lysosomal storage disease?
|
- clinical signs appear shortly after birth
- ataxia, incoordination, tremors - death after many months |
|
|
how do neurons with lysosomal storage disease appear microscopically?
|
neurons are filled with substrate that is often foamy or granular in appearance
|
|
|
what general group of diseases are caused by prions?
|
transmissible spongiform encephalopathy
|
|
|
what is neuropil?
|
a type of glial cell located in the brain. they are the "pink background" in an H&E stain of brain tissue.
|
|
|
what lesions are seen macroscopically and microscopically in transmissible spongiform encephalopathy?
|
- no gross lesions are present
- vacuoles are present in the neuropil |
|
|
what is Nissl substance?
|
ribosomes within neurons
|
|
|
the dispersion of Nissl substance in a neuron, giving the cytoplasm a glassy appearance, caused by axonal degeneration
|
chromatolysis
|
|
|
compressive necrosis and degeneration of myelin and axons of the spinal cord
|
Wallerian degeneration
|
|
|
in which two species is Wallerian degeneration most common?
|
dogs and horses
|
|
|
what is seen microscopically in Wallerian degeneration?
|
- lost axons
- fragmented and swollen myelin sheaths, leaving vacuoles in the white matter - macrophages in the empty axon sheaths - reactive astrocytes |
|
|
what are two common etiologies of Wallerian degeneration caused by compression of the spinal cord?
|
1. herniation of an intervertebral disc
2. cervical vertebral stenotic myelopathy |
|
|
what is Wobbler Syndrome? What microscopic lesion is present?
|
- cervical vertebral stenotic myelopathy of the horse
- malformation of the cervical vertebra, causing stenosis of the spinal canal and pressure necrosis of the spinal cord - lesions will appear as Wallerian degeneration |
|
|
what is the most important class of toxin that causes axonal degeneration?
|
organophosphates
|
|
|
a disease of most commonly horses, but also dogs, with an unknown cause, characterized by diffuse Wallerian degeneration of the spinal cord
|
degenerative myelopathy
|
|
|
how do necrotic neurons appear on an H&E stain compared to normal neurons?
|
- normal are blue
- necrotic are red |
|
|
A disease of the brain, characterized by associated edema and softening of the gray matter and necrosis.
|
polioencephalomalacia
|
|
|
what is the most common cause of polioencephalomalacia in ruminants? what are clinical signs in these animals?
|
- thiamine deficiency
- blind, paresis → recumbency, grinding of teeth, opisthotonus (back muscle spasm) and extensor rigidity |
|
|
besides thiamine deficiency, what are three causes of polioencephalomalacia in ruminants (and pigs)?
|
1. salt poisoning
2. dehydration → salt poisoning 3. lead toxicity |
|
|
what is the usual result of ischemia or hypoxia to neural tissue?
|
necrosis
|
|
|
neuronal necrosis in the foal caused by hypoxia and ischemia during dystocia
|
neonatal maladjustment syndrome
|
|
|
unique to the horse, a necrosis of the white matter of the brain with softening, caused by corn spoiled with Fusarium mold.
|
leukoencephalomalacia
|
|
|
what is the gross appearance of leukoencephalomalacia? what species are affected? clinical signs?
|
- cerebral cortical white matter is edematous and thickened with hemorrhage and yellowing
- this disease is unique to horses - sudden onset of staggering, weakness, circling, depression, and head pressing - seizures and hyperexcitability → death |
|
|
what lesions are observed in a neurological infection of Clostridium perfringens type D in sheep?
|
- secondary neuronal necrosis with hemorrhage in the basal ganglia, cerebellar peduncles, and internal capsule
- bilaterally symmetrical - focal symmetrical encephalomalacia |
|
|
a disease of unknown cause in the horse characterized by chromatolysis and necrosis of the neurons of the ventral horns of the spinal cord.
|
equine motor neuron disease
|
|
|
in pigs, caused by selenium toxicity, posterior paralysis and quadriplegia due to necrosis of the ventral horn of the cervical and lumbar spinal cord
|
poliomyelomalacia
|
|
|
inflammatory cells and lymphocytes surrounding a blood vessel in the CNS as a response to necrosis, ischemia, and inflammatory diseases
|
perivascular cuffing
|
|
|
inflammation of the leptomeninges, pia and arachnoid
|
meningitis
|
|
|
meningitis that has extended into the neuropil
|
meningoencephalitis
|
|
|
how do the meninges appear grossly with severe inflammatory meningitis?
|
opaque white, yellow, or green
|
|
|
what are the two major types of tooth germ tumors?
|
1. ameloblastoma
2. odontoma |
|
|
comment on the malignancy of tooth germ tumors
|
they are generally benign, but very proliferative.
|
|
|
in which species do tooth germ tumors commonly occur?
|
dog, cat, bovine
|
|
|
failure to form enamel of the teeth
|
enamel hypoplasia
|
|
|
what causes enamel dysplasia in young dogs?
|
distemper virus
|
|
|
what non-infectious agent can cause destruction of the enamel? Pathogenesis?
|
- fluorine
- calcuim fluoride makes the enamel more brittle, exposing the dentin (looks yellow) |
|
|
what is the most common cause of periodontal disease?
|
tartar buildup on the teeth
|
|
|
a cyst that forms when a salivary duct ruptures and saliva accumulates in the adjacent soft tissue
|
mucocele
|
|
|
a mucocele of the sublingual salivary gland that forms a cyst at the base of the tongue
|
ranula
|
|
|
inflammation of the salivary gland. Where is this most commonly found?
|
-sialoadenitis
- corona virus in rats - (mumps in people) |
|
|
what is the most common tumor of the salivary gland? Appearance?
|
salivary gland adenocarcinoma
singular nodular node in the submandibular region |
|
|
comment on the malignancy of salivary gland adenocarcinomas
|
highly metastatic, especially to the lungs
|
|
|
what is the most common lesion of the esophagus?
|
ulcers
|
|
|
what is a major causative agent of ulcers in the bovine esophagus?
|
- BVD
|
|
|
how to ulcers appear in the esophagus?
|
they are linear
|
|
|
what is "choke"?
|
annular ulcers of the equine esophagus caused by dry food getting stuck and causing pressure necrosis. Can perforate
|
|
|
what are four etiologies of proliferative, caseous lesions of the esophagus?
|
1. avian pox
2. hypovitaminosis A 3. candida (thrush) 4. trichomonas |
|
|
what causes thrush? Where is the lesion?
|
- candida
- usually lesions on the tongue, but anywhere in the oral cavity |
|
|
what are four etiologies for respiratory squamous metaplasia in birds?
|
Candida, Trichomonas, Pox Virus, Hypovitaminosis A
|
|
|
why does hypovitaminosis A cause proliferation of the avian esophagus?
|
it causes squamous metaplasia, which proliferates and keratinizes
|
|
|
dilation of the esophagus, commonly associated with a persistent right aortic arch
|
megaesophagus
|
|
|
what causes Edema disease of swine? Where is the edema?
|
- E. coli
- stomach, subcutis, mesentery, and other sites |
|
|
what dietary deficiency can cause edema of the stomach wall and/or intestinal wall
|
hypoproteinemia
|
|
|
what are four common causes of gastric ulcers?
|
1. idiopathic
2. Gastrophilus larvae in horses 3. stress 4. steroids or NSAIDs |
|
|
what are three causes of megaesophagus?
|
1. myasthenia gravis
2. persistent right aortic arch 3. dermatomyositis |
|
|
what are two common causes of gastric hemorrhage
|
1. heavy metals
2. uremia |
|
|
in which species do bloat most commonly occur?
|
horses and captive primates
|
|
|
what is the most common site of ulcers in horses? Etiology? Severity of disease?
|
- the margo plicatus
- Gastrophilus larvae - incidental finding |
|
|
what to bots look like in the horse stomach?
|
yellow bumps at the margo plicatus
|
|
|
at necropsy, how do you differentiate whether a stomach has hemorrhage or if it has congestion?
|
- congestion is light and diffuse
- hemorrhage is usually bright red and sharply demarcated |
|
|
what is melena?
|
a black colored blood in the GI tract (usually in the stools), caused by digestion of the blood
|
|
|
how can renal failure lead to melena?
|
renal failure → uremia → gastric ulcers → hemorrhage into stomach → melena
|
|
|
what is volvulus?
|
twisting of the stomach or intestine around the axis of the mesentery
|
|
|
what is a fancy name for bloat?
|
gastric distention
|
|
|
how is bloat commonly caused in horses?
|
grain overload causes excessive fermentation and bloat. Can lead to rupture
|
|
|
what is a common sequela to gastric distention in dogs?
|
volvulus
|
|
|
what is a lesion resulting from gastric torsion that involves a place other than the stomach?
|
splenic ischemia
|
|
|
swallowing of air
|
aerophagia
|
|
|
what are two common causes of a displaced abomasum in cattle?
|
1. bloat
2. parturition |
|
|
what is the most common species and pathogenesis of a stomach rupture?
|
horses from intestinal obstruction or gastric distention
|
|
|
plant foreign body in the stomach
|
phytobezoar
|
|
|
fancy name for a hairball
|
trichobezoar
|
|
|
how can a tricho- or phytobezoar be a problem?
|
if they obstruct the pylorus, they can cause gastric distention
|
|
|
what is a common cause of gastric mucosal hyperplasia in
- cattle? - horses? |
- cattle: Ostertagia
- horses: Trichostrongylus |
|
|
what does an abomasum infected with Ostertagia look like?
|
bumps on the mucosa
|
|
|
what are three common neoplasias of the stomach (species)
|
1. Gastric carcinoma (dogs)
2. Squamous cell carcinoma (horse) 3. Lymphoma (dog, cat, cattle) |
|
|
what does a gastric carcinoma look like? Malignancy?
|
very fibrous and proliferative. Very malignant and poor prognosis
|
|
|
why can horses get squamous cell carcinoma of the stomach, but not usually dogs? Comment on malignancy
|
because horses have a non-glandular portion of their stomach. These are very malignant because they commonly spread to the intestines and colic
|
|
|
comment on the gross appearance of gastric lymphoma
|
homogeneous, tan, soft tissue. Can fill the stomach and outline the shape and cause obstruction
|
|
|
tumor of smooth muscle
|
leiomyoma
|
|
|
what does a leiomyoma of the GI tract look like. Prognosis
|
a coarse, single-nodular tumor that bulges into the lumen. Can be surgically removed.
|
|
|
inflammation of the choroid plexus
|
choroiditis
|
|
|
inflammation of the epithelioid tissue lining the ventricles of the brain and spinal cord
|
ependymitis
|
|
|
what is the most common pathogenic source of bacterial infection in the CNS?
|
hematogenous
|
|
|
Neural Listeriosis in ruminants
- how does it get into the CNS - lesions - clinical signs |
- enters the brainstem through the mouth via the cranial nerves secondary to trauma to the oral cavity
- purulent encephalitis with microabscesses - circling, head pressing, paralysis of CN-VII causing unilateral drooping of the ear, lip, or eyelid |
|
|
thrombotic encephalitis in cattle is caused by what?
|
Histophilus somni
|
|
|
Histophilus somni in cattle (neurologic infection)
- disease name - lesions - clinical signs |
- thrombotic meningoencephalitis
- localization in the brain, producing a vasculitis with thrombosis of cerebral vessels. Grossly, multifocal hemorrhages which are infarcts - arthritis, pneumonia; death is usually rapid |
|
|
microscopically, what are three lesions associated with CNS viral infection?
|
- lymphocytic and plasma cell perivascular cuffing
- chromatolysis and necrosis of neurons - glial nodules - proliferation and aggregation of microglia |
|
|
what are Negri bodies?
|
eosinophilic intracytoplasmic accumulations of Rabies virus
|
|
|
how is Rabies definitively diagnosed?
|
microscopically, by the presence of Negri bodies in the brain
|
|
|
a highly contagious and zoonotic infection of pigs that can lead to fatal neurologic disease
|
pseudorabies
|
|
|
pseudorabies:
- causative agent - host species - clinical signs |
- a herpes virus
- pigs - some pigs are asymptomatic; young pigs develop severe neurologic disease; older pigs develop mild respiratory disease |
|
|
neurological disease of the horse transmitted through mosquito bites
|
equine viral encephalitis
|
|
|
equine viral encephalitis
- what is the infectious agent? - how is it acquired? - clinical signs |
- an arbovirus
- acquired by mosquito bites - drowsiness, blindness, circling, and death |
|
|
describe the microscopic lesions of retroviral neurologic infection in goats and sheep.
|
- perivascular cuffs
- demyelination |
|
|
a brain section of a goat shows demyelination and perivascular cuffs. what could this indicate?
|
retroviral infection such as caprine arthritis encephalitis
|
|
|
caprine arthritis encephalitis
- causative agent - clinical signs - microscopic lesions |
- a retrovirus
- in goat kids, encephalomyelitis; in adult goats, arthritis and interstitial pneumonia - in a brain section, demyelination and perivascular cuffs |
|
|
a retroviral disease of sheep similar to caprine arthritis encephalitis
|
visna
|
|
|
canine distemper
- causative agent - lesions in the CNS - characteristic clinical sign |
- a morbillivirus
- neuronal necrosis in the gray matter and demyelination in the white matter; basophilic intranuclear and intracytoplasmic viral inclusion bodies in the neurons and astrocytes. - (variable clinical signs but) one common clinical sign is myoclonus (repetitive contraction) of the masticatory muscles. |
|
|
a dog presents with spasms of the masticatory muscles and severe neurologic disorders. After euthanasia, a brain section shows neuronal necrosis in the gray matter and demyelination in the white matter. Also, intranuclear and intracytoplasmic inclusion bodies were found in the neurons and astrocytes. What disease did this dog have?
|
canine distemper
|
|
|
a viral infection of the horse that is most well-known for causing abortion, but also can cause vasculitis and hemorrhage in the spinal cord and brain
|
equine herpesvirus 1
|
|
|
a poliomyelitis and encephalitis affecting horses is caused by which infective agent?
|
west nile virus
|
|
|
what is the typical lesion of a fungal infection in the nervous system?
|
granulomatous or pyogranulomatous inflammation
|
|
|
what is the most important fungal disease in animals affecting the nervous system? In which species does this occur? describe pathogenesis and diseases
|
- Cryptococcus (a yeast)
- cats - infection of the nasal mucosa extends into the brain, producing meningitis or meningoencephalitis |
|
|
name three parasites that infect nervous system and their hosts?
|
1. Sarcocystis neurona - horses
2. Paralaphostrongylus tenuis - sheep and llamas 3. Halicephalobus gingivalis - horses |
|
|
describe the lesions observed with parasitic infection of the nervous system
|
- multifocal inflammation and necrosis of white and gray matter
- eosinophils |
|
|
what type of infection is associated with eosinophils?
|
parasites such as protozoa and helminthes
|
|
|
equine protozoal myelitis
- causative agent - microscopic lesions - clinical signs |
- Sarcocystis neurona
- multifocal inflammation and necrosis of white and gray matter; eosinophils - paralysis, paresis, ataxia |
|
|
Paralaphostrongylus tenuis
- animals affected - carrier - clinical signs |
- sheep and llamas
- white-tailed deer are asymptomatic carriers - infection of the spinal cord, leading to paresis, paralysis, and ataxia |
|
|
Halicephalobus gingivalis
- host species - what does it do? |
- horses
- infects the kidney and nasal cavity. It can penetrate the skin and migrate hematogenously to the brain |
|
|
an idiopathic disease of dogs characterized by lesions (often discolored) of the white matter and consists of lymphocytes, plasma cells, and macrophages
|
granulomatous meningoencephalitis
|
|
|
what neurologic disease of horses is characterized by incontinence, perineal anesthesia, and tail paralysis?
|
cauda equina neuritis
|
|
|
name two types of glial cell tumors and their prevalence
|
- astrocytoma - most common
- oligodendroglioma - very rare |
|
|
astrocytomas
- which animals are most commonly affected? - location of tumors - describe the lesions - what is the main reason they cause clinical signs? |
- brachycephalic breeds of dogs
- cerebral cortex - tan, gray, or white, and can range from well to poorly delineated - they cause compression of surrounding tissue, which causes clinical signs |
|
|
tumors of the choroid plexus
- types of tumors - appearance - where are they usually located? |
- adenoma or adenocarcinoma
- very vascular and red grossly - in the 4th ventricle |
|
|
a neoplasm on the surface of the brain
|
meningioma
|
|
|
what is the most common tumor of the CNS in the dog and cat? describe the lesion and location of the lesion.
|
- meningioma
- white to gray fibrous mass on the surface of the brain - ventral in dogs; dorsal in cats |
|
|
a tumor of the cells lining the ventricles of the CNS
|
ependymoma
|
|
|
what is the difference in appearance of a choroid plexus tumor and an ependymoma?
|

a choroid plexus tumor is red and vascular; an ependymoma is gray, white, or tan
|
|
|
name three tumors of the nervous system that originate from primitive neurons
|
1. neuroblastoma
2. medulloblastoma 3. ganglioneuroma |
|
|
peripheral nerve sheath tumor
- what type of cells are neoplastic? - species - location of tumors |
- Schwann cells (note this is also called a Schwannoma)
- mainly dogs, more rarely cattle - in dogs: skin and brachial plexus; cattle: intrathoracic nerves |
|
|
a dog presents with unilateral thoracic limb paralysis and firm masses under the skin near the axilla. What is it?
|
peripheral nerve sheath tumor (Schwannoma)
|
|
|
a horse at necropsy presents with hydrocephalus and large nodules obstructing the ventricles. What could these nodules be?
|
cholesterol granuloma
|
|
|
what is dural ossification?
|
mineralized plaques in the dura of older dogs
|
|
|
inflammation of the mouth
|
stomatitis
|
|
|
inflammation of the tongue
|
glossitis
|
|
|
inflammation of the gums
|
gingivitis
|
|
|
what usually occurs secondarily to a cleft palate in a neonate?
|
aspiration pneumonia from colostrum/milk entering the nasopharynx. sucking may also be difficult
|
|
|
what is the fancy name for a blister
|
vesicle
|
|
|
name four vesicular disturbances of the mouth, caused by reportable, contagious viral infections and the species in which they are found
|
1. foot and mouth disease - pigs, cattle, sheep
2. vesicular stomatitis - horses, cattle, pigs 3. vesicular exanthema - pigs 4. swine vesicular disease - pigs |
|
|
a cat with ulcers in the mouth and an upper-respiratory infection probably has what?
|
feline calici virus
|
|
|
what causes cold sores in rhesus monkeys, but kills other monkeys like humans?
|
Herpes B virus
|
|
|
what are two autoimmune diseases of the dog and cat that produce a vesicular stomatitis?
|
1. pemphigus vulgaris
2. bullous pemphigoid |
|
|
what are two rule-outs for ulcerations of the esophagus, small intestine, and mouth of cattle?
|
1. BVD
2. malignant catarrhal fever |
|
|
what is bluetongue?
|
an insect-transmitted orbivirus infection of sheep causing ulcers in the mouth and hemorrhages in the forestomach, coronet, and pulmonary artery
|
|
|
what causes ulcers on the tongue and stomach secondary to renal failure?
|
uremia
|
|
|
ulcers in the mouth of dogs and cats caused by a hypersensitivity to parasitic infection
|
eosinophilic granuloma complex
|
|
|
gram-negative infection of fish and reptiles causing septicemia, and necrosis and hemorrhage of the mouth and other organs
|
Aeromonas
|
|
|
a pox virus infection of sheep and goats producing crusty lesions on the lips, face, and feet
|
contagious ecthyma
|
|
|
what is contagious ecthyma?
|
a pox virus infection of sheep and goats producing crusty lesions on the lips, face, and feet
|
|
|
in cattle, a parapox virus infection producing discrete circular, slightly raised lesions in the mouth and esophagus, usually an incidental finding.
|
bovine papular stomatitis
|
|
|
a gram-negative bacterial infection of young cattle, producing ulcerative and caseous proliferative lesions in the mouth and larynx. The organism is a secondary invader following trauma to the mucosa.
|
Fusobacterium necrophorum
|
|
|
bovine papular stomatitis
- etiology - lesions - malignancy |
in cattle, a parapox virus infection producing discrete circular, slightly raised lesions in the mouth and esophagus, usually an incidental finding.
|
|
|
Fusobacterium necrophorum
- species infected - lesions - etiology |
a gram-negative bacterial infection of young cattle, producing ulcerative and caseous proliferative lesions in the mouth and larynx. The organism is a secondary invader following trauma to the mucosa
|
|
|
what diseases in the mouth of cattle are produced by
- Actinobacillus - Actinomyces |
- Actinobacillus: wooden tongue
- Actinomyces: lumpy jaw |
|
|
proliferation of the gums, usually in response to chronic periodontal disease in dogs
|
gingival hyperplasia
|
|
|
what is the most common cause of gingival hyperplasia?
|
periodontal disease
|
|
|
what are four types of neoplasias of the small intestine
|
1. lymphosarcoma
2. leiomyoma/leiomyosarcoma 3. adenocarcinoma 4. gastrointestinal stromal tumor |
|
|
what is the appearance of small intestinal lymphoma
|
- usually not constrictive
- tan and firm |
|
|
what the appearance of adenocarcinoma in the small intestine
|
annular band
|
|
|
what is a gastrointestinal stromal tumor in the SI?
|
tumor of the interstitial cells of Cajal, which are part of the autonomic nervous system and located in the myenteric plexuses of the intestinal wall
|
|
|
tumor of the interstitial cells of Cajal, which are part of the autonomic nervous system and located in the myenteric plexuses of the intestinal wall
|
gastrointestinal stromal tumor
|
|
|
what is the appearance of a leiomyoma of the SI
|
distinct tan nodule beneath the mucosa.
|
|
|
in what species is volvulus of the SI most common?
|
horse
|
|
|
what lesions are caused by volvulus of the SI? Why can animals die?
|
no venous drainage; so congestion, edema, necrosis, endotoxic shock, death
|
|
|
a telescoping of the intestine into itself
|
intussusception
|
|
|
what is the most common cause of intussusception?
|
secondary to hypermotility
|
|
|
what lesions are associated with intussusception? Clinical signs
|
it is a local lesion, so it can be removed. Pain, colic.
|
|
|
condition where the intestine is trapped by a band of connective tissue
|
strangulation/incarceration
|
|
|
what is the usual cause of SI strangulation/incarceration in horses?
|
most commonly with lipomas in the mesentery
|
|
|
entrapment of the intestine in constricted openings such as enlarged inguinal rings, an open umbilicus or a ruptured diaphragm
|
hernia
|
|
|
what are four non-infectious rule-outs for small intestine that have diffuse congestion, hemorrhage, and edema of the affected bowel?
|
1. hernia
2. strangulation/incarceration 3. volvulus 4. torsion |
|
|
a tumor that looks like an annular band in the SI is probably what?
|
adenocarcinoma
|
|
|
what is the difference between a torsion and a volvulus?
|
torsion is twisting on itself; volvulus is a rotation on its mesenteric axis
|
|
|
what are two bacterial causes of excess fluid within a normal intestine?
|
E. coli, Clostridium perfringens type D
|
|
|
what are three viral causes of excess fluid within a normal intestine?
|
rotavirus, coronavirus, panleukopenia
|
|
|
what is a protozoal cause of excess fluid within a normal intestine?
|
cryptosporidia
|
|
|
what are two non-infectious diseases of the small intestine characterized by excess fluid, but not usually hemorrhage?
|
1. lymphangiectasia
2. inflammatory bowel disease |
|
|
in which species is E. coli an important infection of the intestines of neonates?
|
pigs, ruminants, foals
|
|
|
how do coronaviruses and rotaviruses lead to excess fluid in the otherwise normal intestine of a neonate?
|
the virus destroys the epithelial cells on the villi, leading to malabsorption and diarrhea
|
|
|
what is the "classic lesion" of a rotavirus or a coronavirus infection of the small intestine?
|
villous atrophy
|
|
|
how does cryptosporidia cause excess fluid in the otherwise normal small intestine?
|
attaches to the microvillus border of the intestinal epithelial cells
|
|
|
what is a common cause of Clostridium perfringens type D enterotoxemia in sheep?
|
a change in feed from poor quality to good quality, which leads to bacterial overgrowth
|
|
|
dilation of the lacteals in the intestinal wall of the dog resulting in malabsorption
|
lymphangiectasia
|
|
|
what is inflammatory bowel disease?
|
an allergic enteritis of the dog and cat of unknown cause, probably from dietary antigens, that causes excess fluid of the normal SI and diarrhea
|
|
|
a parvovirus infection of the cat, causing hypoplasia of all cell lines in the bone marrow and necrosis of the intestinal crypts
|
panleukopenia
|
|
|
in inflammatory bowel disease, what is the scientific term for the most common form for the disease?
|
lymphoplasmacytic enteritis
|
|
|
macrophages in the mucosa of the large intestine along with ulcers
|
ulcerative colitis/histiocytic ulcerative colitis
|
|
|
what is the lesion associated with ulcerative colitis?
|
macrophages in the mucosa
|
|
|
a bacterial infection of primates producing an ulcerative and sometimes hemorrhagic colitis
|
Shigella
|
|
|
what infection causes ulcerative colitis in the horse?
|
Salmonella
|
|
|
what breed of dogs is predisposed to ulcerative colitis?
|
Boxers
|
|
|
what lesions are observed with salmonellosis of the large intestine?
|
ulcerative and/or hemorrhagic or fibrinous or fibrinonecrotic
|
|
|
name three bacteria involved in fibrinous/necrotic/fibrinonecrotic lesions of the large intestine and their associated hosts
|
1. Salmonella - horses, pigs (SI in cattle)
2. Brachyspira hyodysenteriae (swine dysentery) - pigs 3. Yersinia pseudotuberculosis - primates, rodents, occasionally cattle |
|
|
name three parasites involved in fibrinous/necrotic/fibrinonecrotic lesions of the large intestine and their associated hosts
|
1. Histomonas meleagridis - turkeys
2. Trichuris (whipworms) - pig and dog 3. heavy infections with small strongyles - horses |
|
|
name two non-infectious causes of fibrinous/necrotic/fibrinonecrotic lesions of the large intestine in horses
|
1. certain oral antibiotics
2. NSAIDs |
|
|
what is the lesion associated with Histomonas infection of the lower GI tract in birds?
|
caseous necrosis of the cecum
|
|
|
what common parasite causes fibrinous colitis in pigs and dogs?
|
whipworms
|
|
|
what is "Colitis X"?
|
a disease in the horse, probably caused by an overgrowth of Clostridia bacteria. It produces hemorrhage and edema in the wall of the colon but no blood in the feces.
|
|
|
a disease in the horse, probably caused by an overgrowth of Clostridia bacteria, producing hemorrhage and edema in the wall of the colon but no blood in the feces.
|
Colitis X
|
|
|
what are three etiologies of hemorrhage of the large intestine?
|
1. Colitis X - horse
2. DIC 3. Anticoagulant toxicosis |
|
|
in ruminants, a disease caused by Mycobacterium avium ss paratuberculosis, which causes thickening of the mucosa due to granulomatous inflammation.
|
Johne's disease
|
|
|
what is Johne's disease
|
in ruminants, a disease caused by Mycobacterium avium ss paratuberculosis, which causes thickening of the mucosa due to granulomatous inflammation.
|
|
|
what type of neoplasias can cause proliferative disorders in the colon?
|
1. lymphoma
2. adenocarcinoma 3. leiomyoma 4. gastrointestinal stromal tumor |
|
|
what are the two main proliferative lesions of the large intestine?
|
1. Johne's disease
2. neoplasia |
|
|
obstruction of the colon
|
impaction
|
|
|
what things usually cause impaction of the large intestine?
|
feces, coarse feed, foreign bodies, (enteroliths and sand in horses)
|
|
|
mineralized concretions in the bowel lumen that build in size over time, which can cause bowel impaction in horses
|
enteroliths
|
|
|
no anus
|
atresia ani
|
|
|
atresia ani
|
no anus
|
|
|
a congenital defect in cattle where the colon ends in a blind sac somewhere other than the anus
|
atresia coli
|
|
|
abnormal dilation of the colon
|
megacolon
|
|
|
what is thought to cause megacolon?
|
spinal disc disease → loss of innervation
|
|
|
what is a melanoma? Where are they found in the body? Comment on malignancy.
|
- tumor of melanocytes
- found in the oral cavity of the dog and skin of many species - 90% are malignant and survival time is 6 months |
|
|
name six neoplasias of the upper GI tract and the species in which they are commonly found
|
1. melanoma - dogs
2. squamous cell carcinoma - cats (tongue) and dogs (tonsil) 3. fibrosarcoma - dogs and cats 4. Epulis - dog 5. papilloma - dog (oral), cattle (rumen) 6. tooth germ cell tumor - dog, cat, cattle |
|
|
squamous cell carcinoma of the upper GI tract:
where are they found in the cat? Dog? Comment on malignancy |
- usually on the tongue of the cat
- tonsils of the dog - invasive, but slow to metastasize. More malignant in the dog tonsil than in the oral cavity |
|
|
what is an epulis? Where does it originate?
|
a benign tumor of the gingiva in the dog that resembles gingival hyperplasia. It aries from the periodontal ligament.
|
|
|
a benign tumor of the gingiva in the dog arising from the periodontal ligament
|
epulis
|
|
|
In the dog, proliferation of the gums: what are two rule-outs?
|
- gingival hyperplasia
- epulis (a neoplasm of the periodontal ligament) |
|
|
what is the fancy name for a wart? What causes it? Where they can be found in the GI system (species)?
|
- papilloma
- papilloma virus infection - oral cavity of the dog and rumen of cattle |
|
|
a rare disease of the dog that is similar to carcinoma grossly in which the stomach wall is infiltrated with eosinophils and fibrosis
|
eosinophilic gastroenteritis
|
|
|
eosinophilic gastroenteritis
- species - lesions |
a rare disease of the dog that is similar to carcinoma grossly in which the stomach wall is infiltrated with eosinophils and fibrosis
|
|
|
a nematode parasite of the horse that burrows into the glandular stomach producing nodules with a central pore
|
Draschia megastoma
|
|
|
Draschia megastoma
- what is it? - species affected - gross lesions observed |
- a nematode
- horse - nodules with a central pore in the glandular stomach |
|
|
what is a common sequela to grain overload in ruminants?
|
bloat
|
|
|
what two basic nutrients can cause bloat in the rumen?
|
- CHO
- proteins (from legumes) |
|
|
why can grain overload lead to ulcers in the rumen
|
because lactic acid buildup damages the rumen mucosa
|
|
|
what is a bloat line?
|
a line of demarcation in the esophageal mucosa at the thoracic inlet, with the cranial esophagus being congested and the caudal esophagus being blanched and pale
|
|
|
a line of demarcation in the esophageal mucosa at the thoracic inlet, with the cranial esophagus being congested and the caudal esophagus being blanched and pale
|
bloat line
|
|
|
in ruminants, what two infectious agents can be associated with lesions secondary to bloat?
|
1. Fungi
2. Fusobacterium |
|
|
what do the gross lesions of a fungal infection of the rumen look like?
|
circular lesions with a red rim
|
|
|
what important bacterial infection of large animals is known to produce ulcers, hemorrhage, or fibrinous lesions of the intestines?
|
Salmonella
|
|
|
what produces ulcers in the Peyer's patches of cattle?
|
BVD
|
|
|
an important cause of ulcers in reptiles
|
amoeba, especially entamoeba
|
|
|
an important disease of young poultry and game birds caused by Clostridium colinum.
|
ulcerative enteritis
|
|
|
ulcerative enteritis in birds
- causative agent - lesions |
- Clostridium colinum
- GI ulcers and multifocal yellow foci in the liver |
|
|
fibrinous enteritis of the mammalian GI tract is almost always what?
|
Salmonellosis
|
|
|
an important disease of chickens caused by Clostridium perfringens type A that produces diffuse necrosis of the GI tract with a fibrinonecrotic pseudomembrane
|
necrotic enteritis
|
|
|
necrotic enteritis in birds
- causative agent - species affected - lesion |
- Clostridium perfringens type A
- chickens - diffuse necrosis of the GI tract with a fibrinonecrotic pseudomembrane |
|
|
what does DIC stand for?
|
disseminated intravascular coagulation
|
|
|
how does heavy metal toxicosis affect the small intestine?
|
causes hemorrhage
|
|
|
an important virus of dogs and cats that causes hemorrhagic enteritis in dogs and panleukopenia and a non-hemorrhagic enteritis in cats?
|
parvovirus
|
|
|
how does parvovirus infection cause disease in dogs?
|
it destroys intestinal crypt cells leading to villous collapse and ulceration. this produces an hemorrhagic enteritis.
|
|
|
how does parvovirus infection cause disease in the GI tract of cats? what does it do to the bone marrow?
|
- it causes necrosis of the intestinal crypt cells and causes a non-hemorrhagic enteritis
- destroys bone marrow, causing a panleukopenia |
|
|
nematode parasite of the large intestine of dogs that causes hemorrhagic enteritis
|
hookworms
|
|
|
what are three bacteria that infect the large intestine of neonates and cause hemorrhagic enteritis (other than E. coli)
|
1. Clostridium perfringens type A - large animals
2. Clostridium perfringens type C - large animals 3. Clostridium difficile - foals |
|
|
name eight bacterial genera that are involved in severe lower GI infections and the diseases they cause
|
1. Brachyspira - swine dysentery
2. Clostridium - neonatal enteritis, Colitis X, ulcerative enteritis of birds, enterotoxemia of sheep, 3. Escherichia (E. coli) - enteritis of all kinds 4. Fusobacterium - ruminal ulcers 5. Mycobacterium - Johne's, proliferative enteritis of birds 6. Salmonella - hemorrhagic enteritis 7. Yersinia - fibrinonecrotic colitis in primates and rodents 8. Lawsonia - proliferative enteritis in pigs |
|
|
what is hemorrhagic bowel syndrome?
|
thought to be caused by Clostridium perfringens type A, a disease of adult dairy cows which produces hemorrhage and blood clots in the duodenum and jejunum, often leading to fatality.
|
|
|
thought to be caused by Clostridium perfringens type A, a disease of adult dairy cows which produces hemorrhage and blood clots in the duodenum and jejunum, often leading to fatality.
|
Hemorrhagic bowel syndrome
|
|
|
an idiopathic hemorrhagic disease in the duodenum of horses
|
proximal enteritis
|
|
|
what common class of protozoan causes hemorrhagic enteritis in a variety of animals?
|
coccidia
|
|
|
bacterial infection of pigs marked by thickening of the intestinal mucosa with necrosis and hemorrhage.
|
Lawsonia intracellularis
|
|
|
Lawsonia intracellularis
- species affected - disease - lesions and gross appearance |
- pigs, hamsters (also horses and dogs)
- proliferative enteritis - marked thickening of the SI mucosa with necrosis and hemorrhage - mucosa has a corrugated appearance and may also have a fibrinonecrotic pseudomembrane |
|
|
an idiopathic disease in horses where the SI mucosa is infiltrated with macrophages
|
granulomatous enteritis
|
|
|
bacterial infection of birds and occasionally mammals that results in diffuse thickening of the mucosa caused by granulomatous inflammation with acid-fast bacteria and macrophages
|
Mycobacterium avium
|
|
|
what does chronic coccidiosis look like in sheep?
|
focal 1-2 mm, raised plaques or nodules in the intestines
|
|
|
what are two non-infectious, non-neoplastic pathologic conditions of muscle of the GI tract?
|
1. idiopathic muscular hypertrophy of the distal ileum in horses
2. hypertrophy of the tunica muscularis externa and tunica muscularis mucosa secondary to chronic obstruction |
|
|
an incidental finding in horses in which there are single or multiple red to brown plaques on the serosa, usually near the ileum.
|
Hemomelasma ilei
|
|
|
what is hemomelasma ilei
|
an incidental finding in horses in which there are single or multiple red to brown plaques on the serosa, usually near the ileum.
|
|
|
a rickettsia infection of horses transmitted by insect vectors. The colon is filled with watery content and the mucosa has patchy congestion with no ulcers, fibrin or hemorrhage.
|
Potomac horse fever
|
|
|
Potomac horse fever
|
a rickettsia infection of horses transmitted by insect vectors. The colon is filled with watery content and the mucosa has patchy congestion with no ulcers, fibrin or hemorrhage.
|
|
|
accumulation of clear, yellow fluid in the abdomen
|
ascites
|
|
|
ascites
|
accumulation of clear, yellow fluid in the abdomen
|
|
|
extensive fibrosis in the liver producing portal hypertension and ascites
|
chronic liver disease
|
|
|
how does chronic liver disease manifest in the abdomen?
|
extensive fibrosis in the liver producing portal hypertension and ascites
|
|
|
an E. coli infection of pigs, where the bacteria produces a toxin which causes edema of the subcutis, stomach, and mesentery
|
edema disease of swine
|
|
|
edema disease of swine
- causative agent - where is the edema? |
an E. coli infection of pigs, where the bacteria produces a toxin which causes edema of the subcutis, stomach, and mesentery
|
|
|
blood in the abdomen
|
hemoperitoneum
|
|
|
in cattle, when a metallic object perforates the reticulum, diaphragm, and pericardial sac
|
traumatic reticulopericarditis
|
|
|
what inflammatory process is associated with traumatic reticulopericarditis
|
fibrinous pericarditis
|
|
|
in which two animals is ruptured urinary bladder most common (pathogenesis)
|
castrated male cats and steer secondary to blockage with mineral deposits
|
|
|
what inflammatory process does urine in the abdomen produce?
|
fibrinous peritonitis
|
|
|
a corona virus infection of cats causing high-protein fluid to form in the body cavities along with fibrin. Small, white plaques on the mesentery and granulomas may be seen in various organs
|
feline infectious peritonitis
|
|
|
feline infectious peritonitis
|
a corona virus infection of cats causing high-protein fluid to form in the body cavities along with fibrin. Small, white plaques on the mesentery and granulomas may be seen in various organs
|
|
|
how does fat necrosis appear in the GI tract?
|
firm, chalky, yellow to brown plaques or nodules
|
|
|
what are two common non-infectious causes of fat necrosis in the cat?
|
Vitamin E deficiency, high dietary polyunsaturated fats
|
|
|
necrosis of the mesenteric fat around the pancreas of the dog or cat is probably what?
|
pancreatitis
|
|
|
in which animals does idiopathic fat necrosis occur?
|
Jersey and Guernsey cows
|
|
|
what plant causes fat necrosis in cattle
|
Fescue toxicosis
|
|
|
how do lipomas often appear in the horse?
|
in the mesentery, they often hang by a fibrous stalk which causes occlusion of blood supply to the lipoma. The fat becomes necrotic and mineralized. "strangulated lipoma"
|
|
|
how does chronic peritonitis appear?
|
fibrous tags on the peritoneum, which makes the peritoneum appear shaggy. Adhesions of the intestine.
|
|
|
what species and where in the body is mesothelioma most commonly found? What do they look like?
|
- congenital in calves, or in the adult dog
- abdomen, thorax, or pericardial space - multiple white nodules and plaques in the abdomen |
|
|
in the cat, an infectious disease characterized by small white plaques on the mesentery and/or nodules in the abdominal region
|
feline infectious peritonitis
|
|
|
in which breed of dogs is hypoplasia of the pancreas most common?
|
German Shepherds
|
|
|
a dog with a voracious appetite and large, voluminous, foul-smelling feces may have what?
|
hypoplasia of the pancreas
|
|
|
necrosis, hemorrhage, and edema of the pancreas, often with fibrin deposition
|
acute pancreatitis
|
|
|
how does chronic pancreatitis appear in the dog?
|
pale, tan, firm, and nodular
|
|
|
what are the two most common neoplasms of the pancreas?
|
adenoma or adenocarcinoma
|
|
|
how does hyperplasia of exocrine pancreatic tissue appear?
|
(incidental), 1-3mm tan to white nodules in the pancreas
|
|
|
what produces a pale tan or brown color change in the liver
|
it can be modest amounts of fat or glycogen within the liver cells
|
|
|
comment on the pathology of a tan or brown color change in the liver that is diffuse versus focal.
|
- diffuse change is pathologic (nutritional or metabolic disease such as diabetes or Cushings)
- focal change is physiologic and not pathologic |
|
|
what causes a yellow color change in the liver?
|
fat
|
|
|
what are two patterns of fat change in the liver?
|
diffuse or lobular
|
|
|
why would a liver have green color change
|
excess bile accumulation, resulting in icterus. The liver appears yellow-green or olive green
|
|
|
why would a liver have a red or red-brown color change?
|
congestion. This is seen in most livers at necropsy
|
|
|
a disease process that affects a specific lobule of the liver will have what histologic pattern?
|
lobular/reticular
|
|
|
what are five disease processes that cause a lobular/reticular pattern in the liver
|
1. passive congestion
2. anemia 3. lipidosis 4. hepatotoxin 5. cholangitis |
|
|
what is the most common cause of a lobular pattern of liver change?
|
passive congestion
|
|
|
what is the most common cause of passive congestion of the liver?
|
heart failure
|
|
|
why does anemia cause a lobular pattern in the liver?
|
it is due to hypoxia to the centrilobular cells
|
|
|
why does lipid accumulation cause a lobular pattern in the liver?
|
accumulation of lipid in the centrilobular area
|
|
|
what is cholangitis?
|
an uncommon bacterial infection of the liver bile ducts, causing a lobular pattern
|
|
|
a pattern of liver change similar to the lobular pattern, but more severe, with larger lesions
|
mosaic pattern
|
|
|
what is a general cause of a mosaic pattern in the liver?
|
massive necrosis
|
|
|
what is a major cause of massive necrosis in the liver of the
- pig? - dog? |
- pig: Vitamin E/selenium deficiency
- dog: halothane, anticonvulsants, and other drugs/toxins |
|
|
what is the most common change associated with damage to the liver?
|
fatty change
|
|
|
what are two basic causes of focal or multifocal change to the liver?
|
1. infectious disease
2. neoplasia |
|
|
what are four neoplasias of the liver?
|
1. hepatocellular carcinoma
2. biliary adenoma and carcinoma 3. metastatic carcinomas and sarcomas 4. nodular hyperplasia |
|
|
a rare tumor of the liver, mostly in the dog, usually single masses, but can be multilobulated, which present as focal areas of brown, red hemorrhage, and yellow (fat)
|
hepatocellular carcinoma
|
|
|
hepatocellular carcinoma
- what is it? - species affected - gross lesions |
a rare tumor of the liver, mostly in the dog, usually single masses, but can be multilobulated, which present as focal areas of brown, red hemorrhage, and yellow (fat)
|
|
|
a single, discrete nodule in the liver that often cystic and contains green or clear fluid, occurring in the cat. In the dog it is seen rarely as multiple firm, white nodules with depressed centers
|
biliary adenoma/carcinoma
|
|
|
describe biliary adenoma/carcinoma in the cat and dog
|
a single, discrete nodule in the liver that often cystic and contains green or clear fluid, occurring in the cat. In the dog it is seen rarely as multiple firm, white nodules with depressed centers
|
|
|
what does a primary hemangiosarcoma of the liver look like?
|
multiple red nodules and blood-filled cysts
|
|
|
how do metastatic carcinomas or sarcomas in the liver typically appear?
|
multifocal tumors in the liver that appear as multiple, firm white nodules
|
|
|
an incidental finding in the liver of an aged dog, a solitary discrete nodule that is soft and tan due to fat accumulation. Some consider these to be hepatocellular carcinoma.
|
nodular hyperplasia of the liver
|
|
|
what is nodular hyperplasia of the liver?
|
an incidental finding in the liver of an aged dog, a solitary discrete nodule that is soft and tan due to fat accumulation. Some consider these to be hepatocellular carcinoma.
|
|
|
how much liver can be removed for complete regeneration?
|
up to two-thirds
|
|
|
what microanatomical aspect of the liver is necessary for regeneration
|
in intact architectural framework and basement membrane is necessary
|
|
|
what are two major rule-outs for a lobular pattern in the liver?
|
1. toxins
2. hypoxia |
|
|
what is the term applied to regenerating hepatocytes?
|
regenerative nodules
|
|
|
what is the usual lesion seen in chronic liver disease? What patterns of this lesion are seen?
|
fibrosis: lobular (portal or central) or multifocal
|
|
|
inflammation of the biliary system
|
cholangitis
|
|
|
an important, common liver disease in dogs that is of unknown cause. The liver is misshapen and has many nodules (cirrhosis)
|
chronic hepatitis
|
|
|
nodular regeneration of the liver with fibrosis
|
cirrhosis
|
|
|
what is cirrhosis of the liver?
|
nodular regeneration of the liver with fibrosis
|
|
|
why are patches of red seen in a mosaic pattern in the liver? Why is there yellow?
|
when blood enters the liver, blood tends to dump into the necrotic regions, making it red. The yellow is from lipid accumulation in the necrotic tissue
|
|
|
what causes a "nutmeg liver"
|
massive necrosis. It is like a mosaic liver, but in a microscopic lobular pattern.
|
|
|
the healing phase of massive necrosis of the liver is called what? What does it look like?
|
post necrotic scarring. The necrotic lobules collapse, forming bands of fibrous tissue
|
|
|
what is the pathogenesis of liver injury secondary to chronic heart failure?
|
chronic passive congestion and fibrosis in the centrilobular areas. The liver retains its shape pretty well, but is congested with a nodular pattern.
|
|
|
a rare disease of the liver caused by a bacterial infection in the biliary tract. The liver is firm and has a lobular pattern.
|
chronic cholangitis
|
|
|
describe chronic cholangitis
|
a rare disease of the liver caused by a bacterial infection in the biliary tract. The liver is firm and has a lobular pattern.
|
|
|
why are lesions so commonly seen in the centrilobular areas of the liver when exposed to toxins?
|
because these cells try to detoxify the substance, damaging themselves in the process
|
|
|
what type of lesions are produced by bacteria in the liver
|
multifocal
|
|
|
what lesions to the liver are commonly observed with portosystemic shunts?
|
since the portal vein is the main blood supply to the liver, shunting of blood leads to atrophy of the liver cells and a small liver
|
|
|
what two types of processes most commonly cause multifocal lesions in the liver?
|
bacterial infection (not toxins, etc.) and neoplasia
|
|
|
why can acquired portosystemic shunts develop? Pathogenesis? What are lesions outside the liver commonly seen?
|
- chronic liver disease such as cirrhosis
- scarring in the liver ↑pressure in the portal veins, causing pressure buildup in the portal system - tortuous, distended veins often appear in the mesentery |
|
|
comment on hepatocellular carcinoma in the woodchuck versus other species
|
associated with viral infection
|
|
|
distended, firm bile ducts:
- common etiology and species affected - lesions |
- associated with liver flukes in sheep and cattle
- they are visible on the liver surface as white, thick, tortuous channels are often raised above the liver surface. |
|
|
white, thick, tortuous channels raised above the liver surface in a sheep or cow is indicative of what type of infection? What is this lesion?
|
- liver flukes
- distended, firm bile ducts |
|
|
what is the most common cause of hemorrhage of the gall bladder?
|
bleeding disorders such as DIC or anticoagulant toxicosis
|
|
|
a disease of the gall bladder that can occur by Salmonella infection in cattle
|
fibrinous cholecystitis
|
|
|
what causes fibrinous cholecystitis in cattle?
|
Salmonella infection
|
|
|
what is the usual cause of thick, viscous, opaque bile?
|
anorexia
|
|
|
how does nodular hyperplasia of the dog liver look?
|
well-delineated, single or multiple discrete masses.
|
|
|
an uncommon, incidental finding of unknown cause in dogs, where the mucosa of the gall bladder contains numerous small cysts, or larger, papillary, or nodular growths.
|
cystic hyperplasia
|
|
|
a collection of mucus in the gall bladder, forming a solid gel that obstructs the gall bladder and can lead to rupture.
|
gall bladder mucocele
|
|
|
what lesions and diseases are seen with a gall bladder mucocele?
|
- cystic hyperplasia
- icterus - gall bladder rupture |
|
|
aggregates of neutrophils and sometimes eosinophils in the epidermis
|
pustules
|
|
|
inflammation of the skin that is predominantly neutrophils
|
pyoderma
|
|
|
a dried-up accumulation of keratin, inflammatory cells, serum, and bacteria on the skin
|
crust (a scab)
|
|
|
what are two requirements for a liver to be called cirrhotic?
|
nodules and scarring
|
|
|
scarring of the liver without nodules is called what?
|
fibrosis
|
|
|
what is the a major cause of pustular dermatitis?
|
bacterial or fungal infection
|
|
|
inflammation of the hair follicle caused by infection with bacteria, fungi, or Demodex mites
|
folliculitis
|
|
|
an autoimmune pustular dermatitis caused by an autoantibody against keratinocytes
|
pemphigus foliaceus
|
|
|
detached keratinocytes that are found histologically floating in a pustule is called what? What disease is this indicative of?
|
- acanthocytes or acantholytic cells
- diagnostic histologic feature of pemphigus foliaceus |
|
|
fluid-filled cavities within or beneath the epidermis less than 5 mm in diameter
|
vesicle
|
|
|
a vesicle greater than 5 mm in diameter
|
bulla
|
|
|
edema between the keratinocytes of the skin
|
spongiosis
|
|
|
edema within the keratinocytes of the skin
|
intracellular edema
|
|
|
what is the usual resolution of a bulla on the skin?
|
rupture and crust formation
|
|
|
why do vesicles form in spongiosis or intracellular edema of the skin?
|
from the loss or displacement of keratinocytes
|
|
|
intracellular edema within the basal epidermal cells
|
hydropic degeneration
|
|
|
what lesion is associated with hydropic degeneration in the skin?
|
intracellular edema within the basal epidermal cells
|
|
|
what are three etiologies of hydropic degeneration of the skin?
|
1. lupus
2. dermatomyositis 3. drug reactions |
|
|
intracellular edema within the superficial keratinocytes of the epidermis
|
ballooning degeneration
|
|
|
what causes ballooning degeneration of the skin
|
viral infection, such as pox virus
|
|
|
what is the histopathological difference between hydropic degeneration and ballooning degeneration of the skin?
|
- hydropic degeneration is intracellular edema within the basal epidermal cells
- ballooning degeneration is intracellular degeneration within the superficial keratinocytes of the epidermis. |
|
|
what are two autoimmune diseases that cause vesicular dermatitis?
|
1. pemphigus vulgaris
2. bullous pemphigoid |
|
|
describe the histopathological appearance of pemphigus vulgaris.
|
suprabasilar vesicle containing acantholytic cells
|
|
|
describe the histopathological appearance of bullous pemphigoid.
|
it is a subepidermal vesicle
|
|
|
what are the causes of pemphigus vulgaris and bullous pemphigoid?
|
an antibody directed against the keratinocyte (pemphigus vulgaris) or the basement membrane (bullous pemphigoid)
|
|
|
a group of inherited congenital diseases producing bullae and vesicles at the dermal-epidermal junction that progress to ulcers.
|
epidermolysis bullosa
|
|
|
what is epidermolysis bullosa?
|
a group of inherited congenital diseases producing bulla and vesicles at the dermal-epidermal junction that progress to ulcers.
|
|
|
what is the usual end-stage of necrosis of the skin?
|
ulceration
|
|
|
a flat, discolored area of the skin, usually less than 1 cm in diameter that can lead to crust formation and ulceration
|
macule
|
|
|
a slightly raised area within the skin which is usually red
|
papule
|
|
|
what are six etiologies of necrotizing dermatitis?
|
1. erythema multiforme
2. toxic epidermal necrolysis 3. burns 4. photosensitization 5. systemic bacterial infections 6. foot rot |
|
|
necrosis of single keratinocytes throughout the epidermis
|
erythema multiforme
|
|
|
a severe form of erythema multiforme characterized by full-thickness epidermal necrosis
|
toxic epidermal necrolysis
|
|
|
what is the main cause of erythema multiforme and toxic epidermal necrolysis?
|
adverse drug reaction in association with systemic inflammation and neoplasia
|
|
|
what two factors, extrinsic to the skin, can predispose an animal to photosensitization?
|
1. a photodynamic agent in the feed
2. secondary to chronic liver disease |
|
|
how can systemic bacterial infection lead to necrosis of the skin?
|
bacteria localize, producing a vasculitis and thrombosis that leads to necrosis
|
|
|
a necrotizing dermatitis of the interdigital skin of cattle in sheep caused by a Fusobacterium and/or a mixed infection
|
foot rot
|
|
|
what is the most common cause of exudative dermatitis?
|
allergic skin disease
|
|
|
allergic skin disease caused by inhalation of an allergen or food allergy
|
atopy
|
|
|
for allergic skin disease, comment on the species differences in the role of eosinophils in dogs, cats, and horses
|
eosinophils play a role in cats and horses, but not dogs.
|
|
|
a group of three histologically different diseases of the skin caused by hypersensitivity or allergy, and may produce nodules, papules, or ulcers.
|
eosinophilic granuloma complex
|
|
|
describe eosinophilic granuloma complex
|
a group of three histologically different diseases of the skin caused by hypersensitivity or allergy, and may produce nodules, papules, or ulcers.
|
|
|
inflammation of the epidermis
|
dermatitis (not "epidermitis")
|
|
|
inflammation of the skin
|
dermatitis
|
|
|
an allergic skin disease caused by contact of the skin with an allergic substance
|
allergic contact dermatitis
|
|
|
allergic contact dermatitis:
- what usually causes this condition? - describe the lesions |
- chemicals and plastics
- lesions may very from papules to crusts |
|
|
direct contact of the skin with irritating substances
|
irritant contact dermatitis
|
|
|
irritant contact dermatitis:
- what can cause this condition? - describe the lesions |
- drugs, soaps, acids, detergents, and others
- depending on the severity of the irritant: erythematous papules or ulcers and crusts of exudative dermatitis |
|
|
what is the scientific name for a "hot spot?"
|
pyotraumatic dermatitis
|
|
|
a severe exudative dermatitis of the dog caused by self-inflicted trauma of biting and scratching because of the pruritis and pain from allergic skin disease
|
pyotraumatic dermatitis ("hot spots")
|
|
|
where on the body does contact dermatitis usually occur?
|
places with sparse or no hair
|
|
|
excess keratin on the surface of the skin and grossly produces flakes or scales on the skin.
|
hyperkeratosis/seborrhea
|
|
|
what are the two histologic patterns of hyperkeratosis?
|
1. orthokeratotic (called "hyperkeratosis")
2. parakeratotic (called "parakeratosis") |
|
|
what is the major histological difference between hyperkeratosis and parakeratosis?
|
in hyperkeratosis, the cells lack nuclei; in parakeratosis the cells have nuclei
|
|
|
what are two causes of seborrhea in the dog?
|
1. an inherited defect in keratinization
2. occurring secondary to primary skin diseases such as allergy, parasites, infection, and endocrine diseases |
|
|
what parasites commonly cause perivascular dermatitis with hyperkeratosis?
|
mites such as Sacroptes and Choioptes
|
|
|
a group of disorders of cornification characterized by hyperkeratosis and the accumulation of scales that look like fish scales. It is a congenital inherited disease
|
ichthyosis
|
|
|
what is ichthyosis?
|
a group of disorders of cornification characterized by hyperkeratosis and the accumulation of scales that looks like fish scales. It is a congenital inherited disease
|
|
|
a disease of small animals causing parakeratosis and associated with chronic liver disease. Associated with defective glucose and amino acid metabolism
|
superficial necrolytic dermatitis
|
|
|
what is superficial necrolytic dermatitis?
|
a disease of small animals causing parakeratosis and associated with chronic liver disease. Associated with defective glucose and amino acid metabolism
|
|
|
hyperplasia of the epidermis
|
acanthosis
|
|
|
a hyperplastic condition of the skin that may appear thickened grossly and have a leathery texture
|
lichenification
|
|
|
increased melanin pigment in the epidermis that makes the skin look dark or black
|
hyperpigmentation
|
|
|
what is the most common cause of hyperpigmentation of the skin?
|
chronic hyperplastic dermatitis
|
|
|
hypopigmentation due to a generalized absence of melanocytes
|
piebaldism
|
|
|
hypopigmentation due to a localized absence of melanocytes
|
vitiligo
|
|
|
hypopigmentation of the skin due to lack of melanin production by melanocytes
|
albinism
|
|
|
what are three general etiologies of skin hypopigmentation?
|
1. absence of melanocytes - piebaldism (generalized) and vitiligo (localized)
2. albinism (lack of melanin production) 3. acquired - inflammation, trauma, irritants, nutritional |
|
|
what is the general pathogenesis of inflammation of the skin?
|
All inflammation must come from the blood vessels. It usually starts as perivascular dermatitis and may spread to become diffuse or nodular.
|
|
|
parasitic infection of the skin
- which inflammatory cells predominate? - what lesions are present? |
- eosinophils
- maculopapular eruptions, crusts, and a perivascular dermatitis |
|
|
what are two major rule-outs for eosinophils in skin inflammation?
|
1. parasite infection (e.g. mites, fleas, flies)
2. allergic skin disease |
|
|
inflammation of the superficial dermis at the dermal/epidermal junction, which obscures the distinction between the dermis and epidermis
|
interface dermatitis
|
|
|
what is interface dermatitis?
|
inflammation of the superficial dermis at the dermal/epidermal junction, which obscures the distinction between the dermis and epidermis
|
|
|
a dense band of inflammation on the superficial dermis which is distinct and sharply demarcated from the adjacent tissue
|
lichenoid dermatitis
|
|
|
what is the difference between interface dermatitis and lichenoid dermatis?
|
- interface dermatitis: dermal/epidermal junction is not well-defined
- lichenoid dermatitis: dermal/epidermal junction is sharply demarcated |
|
|
what is lichenoid dermatitis?
|
a dense band of inflammation on the superficial dermis which is distinct and sharply demarcated from the adjacent tissue
|
|
|
firm swellings in the dermis and/or subcutis and palpate as a mass
|
nodules
|
|
|
what are five causes of nodular dermatitis?
|
1. infection
2. sterile granulomatous/pyogranulomatous nodular dermatitis (dogs only) 3. furunculosis 4. panniculitis 5. neoplasia |
|
|
infection of the dermis usually produces what type of lesion?
|
nodular dermatitis
|
|
|
in the dog, a non-infectious inflammation of the dermis, centered on the adnexa, which produces a nodular dermatitis
|
sterile granulomatous/pyogranulomatous nodular dermatitis
|
|
|
a nodular dermatitis produced by the rupture of hair follicles
|
furunculosis
|
|
|
what is furunculosis? pathogenesis?
|
- a nodular dermatitis caused by rupture of hair follicles
- occurring secondary to folliculitis or trauma (licking, biting), a release of hair and keratin into the dermis, which elicits a severe inflammation. |
|
|
inflammation of the subcutis in cats and dogs that may or may not involve the dermis or epidermis. produces a nodular dermatitis.
|
panniculitis
|
|
|
what is panniculitis?
|
inflammation of the subcutis in cats and dogs that may or may not involve the dermis or epidermis. produces a nodular dermatitis.
|
|
|
what are four etiologies for panniculitis?
|
- secondary to dermatitis
- physical injury or infection - vitamin E deficiency in the cat - idiopathic |
|
|
loss of hair
|
alopecia
|
|
|
what is the most important cause of primary alopecia?
|
endocrine skin disease
|
|
|
what is the usual pattern of alopecia associated with endocrine skin disease?
|
bilaterally symmetrical alopecia over the perineum, back, and flanks.
|
|
|
what is the most common endocrine disorder that causes endocrine skin disease? what are two other less-common causes?
|
- most common: hypothyroidism
- also: hyperestrogenism and hyperadrenocorticism |
|
|
what is the main lesion seen with endocrine skin disease?
|
alopecia due to hair follicle atrophy
|
|
|
a group of inherited diseases characterized by alopecia and an absence of hair follicles
|
hypotrichosis
|
|
|
a group of hereditary diseases in which collagen is defective. The skin is hyper-extensible, loose, and tears easily
|
collagen dysplasia (dermatosparaxis, cutaneous asthenia)
|
|
|
abnormal development of hair follicles
|
follicular dysplasia
|
|
|
where on/in the body does cutaneous squamous cell neoplasia occur in the
- dog? - horse? - cow? - cat? |
- dog: skin and oral cavity
- horse: penis, eye, stomach - cow: eye - cat: nose, pinna |
|
|
where does melanoma occur in the following animals (comment on malignancy)?
- dogs - horses |
- dogs: skin (usually benign); oral cavity (usually malignant)
- perineum of old gray horses (benign, but multiple masses present) |
|
|
cutaneous warts
- scientific name - cause - species most commonly affected - age factor |
- papilloma
- epithelial tumor caused by a papilloma virus - most often in cattle, but also horse and dog - affects young animals and usually spontaneously regresses |
|
|
a rare benign tumor of the skin of the dog with a predisposition in the Norwegian Elkhound
|
Intracutaneous cornifying epithelioma (keratoacanthoma)
|
|
|
what breed of dog is most predisposed to Intracutaneous cornifying epithelioma (keratoacanthoma)?
|
Norwegian Elkhound
|
|
|
what is the most primitive of the skin adnexal tumors? in which species are these most common?
|
- basal cell tumor
- dogs and cats |
|
|
a common benign adnexal tumor of the dog arising from the hair follicle that makes hair follicle and hair
|
trichoepithelioma
|
|
|
what is a trichoepithelioma?
|
a common benign adnexal tumor of the dog arising from the hair follicle that makes hair follicle and hair
|
|
|
a rare benign tumor of the dog arising from the hair matrix, where only hair is made.
|
pilomatricoma
|
|
|
what is a pilomatricoma
|
a rare benign tumor of the dog arising from the hair matrix, where only hair is made.
|
|
|
what are three general tumors of the glands of the skin?
|
1. sebaceous gland tumors
2. apocrine gland tumors 3. perianal gland tumors |
|
|
what are the three most common locations of apocrine gland tumors in the dog and cat?
|
1. sweat glands
2. ceruminous glands of the external ear 3. apocrine glands of the anal sac |
|
|
which tumors of the glands of the skin in the dog have a predisposition to
- females? - males? |
- female: apocrine gland tumor of the anal sac
- male: perianal gland tumors |
|
|
what often occurs secondarily to apocrine gland tumors of the anal sac?
|
hypercalcemia
|
|
|
a very common benign tumor of dogs less than 2 years of age that arises from the Langerhans (dendritic) cells of the epidermis
|
histiocytoma
|
|
|
histiocytoma in the epidermis
- species - age - what cells are affected? - malignancy |
- dog
- < 2 years of age - Langerhans (dendritic) cells - benign |
|
|
mast cell tumors
- species - malignancy |
- most common in dog, but also seen in cat and horse
- can be benign or malignant |
|
|
a rare benign tumor of the dog and cat arising from fibroblasts
|
fibroma
|
|
|
what type of tumor can occur in the skin of cats secondarily to vaccination?
|
fibrosarcoma
|
|
|
malignant tumor of fibroblasts
|
fibrosarcoma
|
|
|
a fibroblast tumor of the horse which is benign and does not metastasize, but has a high rate of local recurrence
|
sarcoid
|
|
|
what is a sarcoid?
|
a fibroblast tumor of the horse which is benign and does not metastasize, but has a high rate of local recurrence
|
|
|
a very common benign tumor of the dog that arises from fat or adipocytes
|
lipoma
|
|
|
plasma cell tumor
- species - where in/on the body does it occur? |
- dog
- skin and oral cavity |
|
|
tumor arising from vascular endothelium
|
hemangioma
|
|
|
a common tumor of unknown cellular origin that occurs in the dermis and subcutis of dogs.
|
hemangiopericytoma
|

