![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
753 Cards in this Set
- Front
- Back
|
Normal Mammalian Sexual Development
|
1. Establishment of chromosomal sex
2. Development of Gonadal sex 3. Development of Phenotypic sex |
|
|
Abnormalities of Phenotypic Sex
|
-Pseudohermaphrodites
-persistent mullerian duct syndrome -androgen insensitivity -steroid 5-a-reductase deficiency -Adrenogenital syndrome |
|
|
Pseudohermaphrodites
|
-Chromosomal constitution and gonadal sex match but Internal or external genitalia are ambiguous
-Gonads of one gender and ducts of opposite gender -Male pseudohermaphrodites are more common than female pseudohermaphrodites -Most mechanisms are not understood |
|
|
Persistent Paramesonephric Duct Syndrome
Mullerian Remnant Syndrome |
-Abnormality of Phenotypic sex
-XY genotype, SRY+ -Testes are present with female internal tubular genitalia -Receptor abnormality, lack of Mullerian Inhibiting Substance or Anti-mullerian hormone receptor -Inherited autosomal recessive trait -Homozygous dogs with descended tests are usually fertile and will transmit trait to all offspring --produces carriers or affected dogs -Occurs in miniature schnauzers -Dx is confirmed by presence of 78,XY chromosome constitution, bilateral testes, and present of all mullerian duct derivatives |
|
|
Persistent Paramesonephric Duct Syndrome
Clinical Abnormalities |
-Undescended testes attached to uterine horns
-Vas deferens are located in the wall of the uterus -Bilateral oviducts, complete uterus with cervix, and cranial portion of a vagina -Bilateral scrotal testes, unilateral or bilateral cryptorchidism may be present also -Dogs may present with pyometra, UTI, prostate infection, or Sertoli cell tumor |
|
|
Androgen Insensitivity
|
-Testicular feminization or Male feminization
-Reported in dogs, mice, rats, cats, cattle, horses -Mutation in the X-linked androgen receptor gene -Deficiency or abnormality of the cytosol receptors for androgen -Testosterone production is normal, conversion to dihydrotestosterone is normal, but target organs are unable to respond to hormones --complete or partial failure of androgen-dependent masculinization --Degree of Dysfunction depends on whether the androgen receptor is non-functional or partially functional -Paramesonephric/Wolffian system does not develop or does not fully develop -No male external genetalia, internal male genetalia -Uterus, cervix, and vagina regress, normal response to mullerian inhibitory ssubstance |
|
|
Non-functional androgen receptor
|
-Androgen-dependent masculinization is absent
-Complete diagnosis for androgen insensitivity and testicular feminization -Affected males present as females that are sterile and do not cycle -Mullerian duct derivatives are absent (like normal male) --regression is not dependent on androgens -Occurs in DSH cats |
|
|
Steroid 5-alpha reductase deficiency
|
-Abnormality of phenotypic sex
-Absence of changes that occur under influence of dihydrotestosterone -No closure of the urethra and scrotum -Will have development of the |
|
|
Genital Abnormalities
|
-Sex abnormalities
--phenotypic, gonadal, chromosomal -Ovarian Abnormalities --developmental, inflammatory, neoplastic -Uterine Tube Abnormalities -Uterus Abnormalities --non-inflammatory or inflammatory |
|
|
Phenotypic Abnormalities of Sex organs
|
-Pseudohermaphrodites
-True hermaphrodites -Chimeras -Have to do histologic assessment to determine if male or female gonadal tissue is present |
|
|
Clinical Indicators of DSD
|
-Lack of estrus
-Enlarged or masculinized clitoris -increased anus-vulva distance |
|
|
Examples of Pseudohermaphroditism
|
-Mullerian remnant Syndrome
--XY chromosomes, SRY+ -Androgen insensitivity --XY chromosomes, SRY+ --receptor issue -XY, SRY- --gonadal dysgenesis --results in hypoplastic or undifferentiated gonads --Female genotype |
|
|
Androgen Insensitivity in Horses
|
-Vagina is a blind sac
-No tubular internal genitalia -Seminiferous tubules are lined by inactive sertoli cells -No male accessory sex glands -Normal appearing mammary glands |
|
|
XX disorders of Sexual Development
|
-Most are SRY negative
-Often have ovotestes (true hermaphrodites) -Ambiguous or female phenotype -Autosomal recessive in American cocker spaniels -Associated with the polled gene in goats |
|
|
True Hermaphrodites
|
-Both male and female gonadal tissue is present
-Chromosomal make-up is a chimera --mosaic --XX with or without SRY gene -Often penis is not fully masculinized -One or both testes may palpable, or not, but are undescended -Dx confirmed via karyotype and histopathology |
|
|
Unilateral Hermaphrodite
|
-Ovotestis on one side
|
|
|
Bilateral hermaphrodite
|
-Ovotestis on both sides
|
|
|
lateral hermaphrodite
|
-Ovary on one side and testis on other side
-Ducts are abnormal |
|
|
Causes of True Hermaphroditism
|
-Congenital adrenal gland hyperplasia
-Fetal exposure to sex hormones -Testicular feminization syndrome -XY gonadal dysgenesis -XY gonadal agenesis -Chromosomal abnormalities |
|
|
True Hermaphrodite affected breeds
|
-American and English cocker spaniel dogs
-Polled goats -German shorthaired pointer -Weimaraner -Beagle -Kerry Blue terrier -Chinese pug -West Highland white terrier -Basset hound -Doberman pinscher -Pomerania -Viszla -Walker |
|
|
XX/XY Chimeras
|
-Two or more types of cells, each with different chromosomal constitution
-Different cells arise from a different source -Product is a hermaphrodite -Free martin |
|
|
XX-XY Mosaics
|
-2 or more types of cells
-Cells arise from the same individual -Non-disjunction at mitosis in a single zygote |
|
|
XO, XXX, XXY
|
-Chromosomal abnormalities
-Cause gonadal hypoplasia without phenotypic ambiguity |
|
|
DAX1 gene
|
-Member of the nuclear hormone receptor
-Superfamily whose expression is mainly restricted to steroidogenic tissues -Expressed in adrenal glands, ovaries, testes, hypothalamus, and pituitary gland -Interruption of expression may be cause of hypogonadotropic hypogonadism (HH) |
|
|
SOX9 gene
|
-Regulates SRY expression
-Encodes a transcription factor involved in chondrogenesis and testis development |
|
|
Bovine Freemartin
|
-Chimeras
-Affects female in a set of male/female twins -Anastomosis of vasculature allows male hematopoietic cells to colonize the female fetus --venous anastomoses between umbilical cords --anastomosis is normal -Both are chimeras, but male is minimally affected -Mullerian inhibiting substance is produced by the male testes, affects female development |
|
|
Female Bovine Freemartin
|
-Small gonads with no germ cells or partially converted to testes
-Externally appears female --vestibule and vulva are hypoplastic --clitoris is enlarged -May be comprised of seminiferous-like tubules -Mullerian duct will be normal or cord-like structure that does not communicate with the vagina -Seminiferous vesicles are present -Other wolffian structures are present |
|
|
Freemartin Pathogenesis
|
-Normal Vascular anastomosis in twin fetuses leads to exchange of blood between fetuses
-Female is exposed to cells and hormones produced by the male testes -Female is masculinized -Male produces testis-determining factor (SRY product) --ovarian inhibition |
|
|
Features of Freemartin Calves
|
-Hypoplastic uterine horns
-Paired hypoplastic vesicular glands -Short, non-patent vagina -Ovotestes are partially surrounded by epidodymal tissue -Clitoris is enlarged -Hypoplastic vulva and vestibule -Prominent tuft of hair ventral to vulva -Male twin is minimally affected -Both twins are chimeras in hematopoietic cells |
|
|
Ovarian Developmental Abnomalies
|
-Agenesis: complete absence of the ovary and its associated primordium
-Hypoplasia: incomplete development or underdevelopment of the ovary --will have decreased number of cells --may or may not have abnormal chromonsomes (XO, XXX) --follicles are usually absent |
|
|
Cystic Graafian Follicle
|
-Prolonged interval between parturition and 1st post-partum estrus
-Occurs in cows and pigs -Larger than normal follicles that persist for more than 10 days without CL formation -Failure of egg release from follicle -AKA cystic ovarian degeneration in cows -Suspected due to deficient LH |
|
|
Anovulatory Luteinized cysts
|
-Develop from follicular cysts with delayed or insufficient release of LH
-Can be considered part of Cystic Ovarian Degeneration -Can be associated with nymphomania |
|
|
Cystic Corpus Luteum
|
-Center of cyst fails to fully luteinize, get cystic center
-Usually incidental finding -No interference with length of estrus cycle |
|
|
Oophoritis
|
-Inflammation of the ovary
-Rare -Can be viral cuase or bacterial cause -Systemic diseases that affect the reproductive tract |
|
|
Turner Syndrome
|
-Partial or complete absence of 1 X chromosome (XO)
-Hypogonadism, small fibrotic ovary -Individual will be short with a broad-based neck, narrow aorta -Not an inherited problem |
|
|
Follicular Atresia
|
-Excessive atresia can result in infertility
-Selective loss of ovarian follicles via atresia occurs through apoptosis -Most obvious in granulosa cell layer |
|
|
Dysgerminoma
|
-Rare germ cell neoplasm
-Analogous to seminoma in males -Relatively benign -Pale brown appearance of parenchyma with a central collagenous scar |
|
|
Teratoma
|
-Rare, benign tumor
-Usually well-differentiated -occurs in 2 of the 3 embryonic germ layers --epithelium --fibrous tissue --endothelial tissue -Composed of non-proliferating somatic tissues, jumble of well-differentiated cells |
|
|
Granulosa Cell Tumor
|
-Most common ovarian neoplasm in large animals
-Solid, cystic, polycystic morphologies -Can produce testosterone in mares --results in stallion-like behavior -Anestrous, continuous estrous, or intermittent estrous are all possible -Will have atrophy of the contralateral ovary due to inhibin production and decreased FSH -Can occur in pregnant mares -Can have thecal differentiation, results in granulosa-theca cell tunor |
|
|
Ovarian Epithelium
|
-Can resemble endometrium
-Contiguous with mesothelium |
|
|
Cystadenoma
|
-Ovarian epithelial tumor
-Common in dogs, rare with spaying -May be lined by epithelium that is serous or mucinous -Mucinous tumors are filled with sticky mucin, tend to be multiloculated -Can be bilateral |
|
|
Hydrosalpinx
|
-Distention of the uterine tube by clear fluid
-Can be due to blockage of outflow of normal tissues -Will lead to salpingitis, inflammation of the uterine tube |
|
|
Salpingitis
|
-Inflammation of the uterine tube and oviducts
-Due to bacterial and viral infections |
|
|
Pyosalpinx
|
-Accumulation of purulent fluid in the lumen of the oviduct
-Pus in the fallopian tubes -Can be accompanied by an obstruction |
|
|
Non-inflammatory conditions of the uterus
|
1. Developmental abnormalities
2. Endometrial hyperplasia 3. Positional abnormalities 4. Subinvolution 5. Endometrial atrophy 6. Adenomyosis 7. Endometriosis |
|
|
Segmental Aplasia of the Uterus
|
-Failure of the Mullerian ducts to reach the urogenital sinus
-Normal on one side and missing on the other side -Prostaglandin produced in the blind uterine horn can cause CL lysis in the contralateral ovary during pregnancy -Long-term distension can cause inability to produce endometrial prostaglandin --no regression of CL --Compression Atrophy leads to damage |
|
|
Endometrial Hyperplasia
|
-Increase in the size and number of endometrial glands with no increase in stroma
-Due to increase in estrogen (large animals) or progesterone (dogs and cats) -Simple endometrial hyperplasia can lead to cystic endometrial hyperplasia, which can cause endometritis and pyometra |
|
|
Endometrial Hyperplasia in Cattle
|
-Due to excessive and prolonged estrogen stimulation
-May have granulosa cell tumor or ovarian follicular cysts -May be due to ingestion of estrogenic cpds |
|
|
Endometrial Hyperplasia in Dogs
|
-Receptors for estrogen on endometrial cells are stimulated, results in synthesis of intracellular receptors for progesterone
-Progesterone converts endometrium to secretory mode -Associated with long-acting progestational cpds used to delay estrus |
|
|
Uterine Torsion
|
-Positional abnormality
-Results in compression of venous outflow -Causes hypoxia, infarction, and shock -Predisposing factors include pyometra, mucometra, and pregnancy -Just because calf is alive does not mean cow is OK |
|
|
Uterine Prolapse
|
-Uterine horn with pregnancy and uterine body
-Urinary bladder and intestines may be involved -Results in hypoxia, infarction, and shock in cow -Occurs in cows, ewes, sows -May result in uterine artery rupture --bleeds into broad ligament and can bleed out -Usually occurs after birth or late in pregnancy -Predisposing factors include dystocia, hypocalcemia, and estrogenic plant ingestion |
|
|
Uterine Subinvolution
|
-Delayed and abnormal involution of the zonal placental sites
-Mostly in dogs -Can have reproductive consequences -Placental sites are thicker than normal, rough, brown, and composed of hematoma and cell debris -Collagen deposition occurs deeper, along with dilated glands -Trophoblast can invade myometrium wither perforation -Hyperplastic endometrium with congestion |
|
|
Endometrial Atrophy
|
-Due to Loss of Ovarian function
-Occurs in seasonal anestrus animals -Older animals that are no longer cycling can also have endometrial atrophy |
|
|
Hematuria
|
-Occurs in rabbits due to uterine issue
-Endometrial venous aneurisms -Uterine adenocarcinoma -Uterine polyps -Urinary bladder polyp -Pyelonephritis -renal infarcts |
|
|
Endometriosis
|
-Heterotrophic endometrial gland with neoplasia-like behavior
-Occurs mostly in primates |
|
|
Endometritis
|
-Inflammation of the endometrium
-related to introduction of semen, pregnancy, parturition, and post-partum involution -most infections start in the endometrium -Progesterone makes the uterus susceptible to infection -Estrogens increase WBC phagocytosis and induice cervix opening --Protects against infection and allows drainage (also exposure) -Prostaglandins facor uterine motility -Can destroy epithelium and decrease reproduction -Truperella pyrogenes |
|
|
Endometritis Pathogenesis
|
Chronic endometritis → decrease in capability to produce prostaglandin → CL persists and progesterone production persists
|
|
|
Pyometra
|
-Acute or chronic suppurative inflammation of the uterus
-Pus accumulates within the uterine lumen -Endometrial hyperplasia can lead to pyometra -Bone marry atrophy and immuno-complex glomerulonephritis in dogs can cause also |
|
|
Twin Placenta
|
-Non-infectious lesion
-Twinnig in the mare and cow are pathological, NOT normal! -Chorion not in contact with the endometrium does not develop villi -Splits available blood flow -Decreased area for nutrient exchange |
|
|
Adventitial Placentation
|
-Non-infectious lesion
-Compensatory measure in the ruminant -Response to inadequate number of placentomes |
|
|
Hydroallantois
|
-Non-infectious lesion
-Excessive acccumulation of fetal urine within the allantoic cavity -Can cause abortion, uterine paresis, or retention of the placenta |
|
|
Hydranmnios
|
-Non-infectious lesion of placenta
-Increased fluid in the amnion -Associated with fetal abnormalities, especially facial abnormalities |
|
|
Umbilical cord abnormalities
|
-Excessive length leads to torsion
-Frequent finding in aborted equine fetuses -Hemorrhage and edema must be present to confirm -Thromobosis and mineralization of placental blood vessels secondary to ischemia are histologically detectable --important for diagnosis |
|
|
Congenital Goiter
|
-Occurs in sheep and goats
-Can cause dystocia -Due to deficiency in diet of the dam |
|
|
Placentitis
|
-Chorionitis
-Amnionitis -Allantoitis -Allantochorionitis |
|
|
Descending placentitis
|
-Hematogenic
-From somewhere else, systemic infection -Ex: Leptospira -Usually bacterial or viral infections |
|
|
Ascending placentitis
|
-Infection ascending from the cervix
--Can be due to chorionic cervical star -Most commonly bacteria and fungi (especially in mares) |
|
|
Large animal abortion
|
-Abortion → release of prostaglandins → regression of corpus luteum → decreased progesterone
-No progesterone, pregnancy is not maintained -Dead fetus is expelled |
|
|
Carnivore and swine abortion
Multiparous abortion |
-DEath of the fetus is NOT followed by CL regression
-Dead fetus is retained until normal time of parturition |
|
|
Pathology of Infectious Abortion Mechanisms
|
1. Fetal hypoxia and stress → fetal corticosteroid release, prostaglandin release → CL regression
2. Uterine contractions → fetal expulsion 3. Microorganism infection of fetus → fetal septicemia/parasitemia→ fetal death in-utero Can have expulsion of fetus with no sequelae, or can have endometritis -retention of fetus with mummification can lead to severe endometritis |
|
|
Mummification
|
-Possible outcome of fetal death
-Fetus will be small, dessicated, and diffusely red -Conceptus is retained in the uterus and progressively dehydrates -Enzyme producing bacteria have to be absent and uterus has to be closed -Sometimes associated with viral infections |
|
|
Maceration
|
-Bacterial contamination of the fetus
-Endometritis and pyometra are likely to occur -Fetus rots -Introduction of bacteria leads to lytic enzymes and decomposition |
|
|
Abortion with fetus and placenta not involved
|
-Different/external cause for abortion
-Damage limited to the uterus can trigger abortion -May occur with equine arteritis virus --causes vasculitis and necrosis of the endometrium and myometrium --fetal hypoxia results -fetus can be viable at the time of expulsion |
|
|
Stillbirth
|
-Delivery of a dead fetus at a stage when it should have been viable
|
|
|
Pathogenesis of Infectious Abortion
|
1. Descending or ascending infection of the chorionic trophoblast
2. Cell necrosis is induced by direct or indirect cytopathic effect 3. Cellular release of inflammatory mediators, prostaglandin included -causes edema and inflammation 4. Hypoxia is triggered by thickening and effacement of trophoblast, endothelial cell necrosis and thrombosis 5. Fetal hypoxia and stress causes corticosteroid release and prostaglandin release 6. uterine contraction and fetal expulsion 7.If organisms are able to infect the fetus, fetal septicemia occurs |
|
|
Herpesvirus
|
-Causes necrosis
-have intranuclear inclusion bodies -Cause mid to late term abortions -Can cause neonatal death |
|
|
Equine Herpesvirus 1 and 4
|
-Respiratory disease, vasculitis, encephalomyelopathy
-Causes necrosis of the lung, liver, and lymphoid organs -All have intranuclear inclusion bodies -Losses for equine industry -EHV-1 causes respiratory disease, fatal vasculitis, and myelopathy secondary to vasculitis --can affect camelids -Fetal liver will have faint white spots and multifocal areas of necrosis -Will see inclusion bodies on histology |
|
|
Bovine HerpesVirus
|
-Infectious Bovine Rhinotracheitis
-Infectious bovine pustular vulvovaginits -causes inflammation of the penis, sheath, vulva, and vagina -Pathogenesis and lesions are similar to EHV-1 --multifocal necrosis -Fetus is autolysed, usually 5-8 months gestation |
|
|
Bacterial abortion vs. Viral abortion
|
-Bacterial: rotten fetus
-Viral: increases birth defects and early embryonic loss -Gestational age at time of infection is important for pestiviruses |
|
|
Suid Herpesvirus 1
|
-Pseudorabies, Aujesky disease
-SMEDI -Distribution and lesions are similar to EHV-1 -Abortion, neonatal mortality -Multifocal white spots on liver -Encephalitis can occur, especially in species eating raw pork |
|
|
Canine Herpesvirus 1
|
-Multifocal visceral necrosis with renal hemorrhages
-Cause of neonatal mortality and presumptive cause of abortion -Direct viral cytopathic effect on parenchymal cells and endothelium |
|
|
Pestiviruses
|
-Bovine Viral Diarrhea
-Border disease -Hog Cholera |
|
|
Bovine Viral Diarrhea
|
-Bovine Pestivirus
-Causes early embryonic death/abortion -Fetuses will be small for gestational age, will have defects -May cause mummification, stillbirth -Weak calves -Able to infect ant cell type |
|
|
Bovine Viral Diarrhea effects on Pregnancy by gestation date
|
1. BVD infection 0-60 days: death of conceptus, embryo is usually resorbed
2. 60-120 days: fetal growth retardation, ocular and nervous system malformations, abortion 3. after 6th month: possible abortion 4. non-cytopathic BVD in 2nd-4th month: immunological tolerance for disease may occur --results in persistently infected animal and constant shedder |
|
|
Hog Cholera
|
-Pestivirus
-Foreign animal disease -Similar to BVD -Tonsils best for diagnosis -Causes abortions -Big meaty spleen with necrosis |
|
|
Hairy Shaker Syndrome
|
-Ovine Pestivirus/Border Disease
-Similar to BVD |
|
|
Arterivirus
|
-Equine Viral Arteritis
-Causes vasculitis of the endometrium --can lead to fetal hypoxia and stress, cortisol release -Fetus rarely has lesions, dies due to secondary lack of O2 from endometrium -Stallions act as carriers |
|
|
Porcine reproductive and Respiratory Syndrome Arterivirus
PRRS |
-Similar to Equine arterivirus
-Causes secondary bacterial infections -Hypofertility, abortion, pneumonia, and infant death -Lesions: chorionitis, vasculitis, pneumonia -Virus replicates within macrophages and endothelium |
|
|
Streptococci, E.coli, and Pseudomonas as cause of equine abortion
|
-Cause ascending placentitis, leading to thickened chorionic cervical star
-Aborted tissues are filled with agents and are INFECTIOUS! |
|
|
Fungi and equine abortion
|
-Cause ascending placentitis, leading to thickened chorionic cervical star
|
|
|
Leptospira interrogans and abortions
|
-Multifocal chorionitis
-Fetal nephritis and pneumonia -Placenta is thickened, edematous, necrotic, or can be totally normal -Have to run PCR for diagnosis |
|
|
Mare Reproductive Loss Syndrome
|
-Eastern tent caterpillar
|
|
|
Ascending infection in uterus
|
-Causes cervical star lesions
|
|
|
Hematogenous infection in uterus
|
-Multifocal chorionic lesions
|
|
|
Herpesvirus and Abortions
|
-Multifocal necrosis in numerous organs
|
|
|
Bluetongue and abortions
|
-Orbivirus
-Causes erosions and ulcers in upper GI -Results in stillbirth, mummification, early embryonic death, infertility -Causes defects and growth retardation -Microvascular injury --before day 70: abortion of absorbtion --70-130: hydranencephaly and death --after day 200: Ab production and fetus is virus-free at birth -Has been migrating northwards -DO NOT export!!! |
|
|
Truperella Pyrogenes and Bovine Abortion
|
-Causes endometritis, placentitis, and fetal pneumonia
-Intraleisional coccobacilli -Often fatal for adults and young -Usually not an outbreak situation -Will have huge colonies of bacteria in the lung -Hemorrhagic tracheal casts in the lung |
|
|
Brucella, Campylobacter, and Chlamydophila and Bovine Abortion
|
-Yellow/brown to gray exudate
-fetal lymphadenitis, vasculitis, abomasitis, bronchopneumonia -Intercotyledonary -Bacteria are morphologically different, but outcome is similar |
|
|
Coxiella burnetti
|
-Q-fever
-Resistant bacterial agent -Causes chorionitis and fetal septicemia -Cotyledons and intercotyledonar chorionic areas are covered by whitish, chalky, exudate -Thickened and leathery placenta -Suppurative placentitis -Occurs in US and Europe -Can also occur in Humans! |
|
|
Bovine Mycotic Abortion
|
-Aspergillus
-Zygomycetes -Cotyledons are eroded away, covered in fibrin-like material --fungal plaques |
|
|
Bacterial Abortion in Bovine
|
-Rotten fetus
-Cotyledons with or without intercotyledonary spaces -Lungs and abomasal contents are important for culture |
|
|
Viral Abortion in Bovine
|
-INcreased birth defects and early embryonic loss
-gestational age at the time of infection is important for pestiviruses |
|
|
Bluetongue in Sheep and Goats
|
-before day 50: absorption and abortion
-Day 50-80: necrotizing encephalopathy -Last trimester: immunocompetence |
|
|
Porcine Parvovirus
|
-Causes stillbirth, mummification, early embryonic death, infertility, reduced litter size
-Infects rapidly dividing cells |
|
|
Causes of Porcine Abortion
|
-Pestivirus
--hog cholera -African Swine Fever Virus -Porcine circovirus 2 |
|
|
Canine herpesvirus 1 and abortions
|
-Multifocal visceral necrosis with renal hemorrhages
-causes neonatal mortality in dogs |
|
|
Feline Herpesvirus and abortion
|
-Rare cause of neonatal mortality
-presumptive cause of abortion -Multifocal visceral necrosis -Often causes conjunctivitis, rhinitis, and tracheitis |
|
|
Brucella canis
|
-Causes abortions after day 50
-Can be a source of brucellosis for other species -Will have gray/green vaginal discharge -Epididymis or testicular degeneration |
|
|
Bacteria, Fungi, and Protozoa affecting multiple species
|
-Chlamydophila:
--ruminants, pigs -Listeria Monocytogenes: --sheep, cattle, primates -Leptospira interrogans: all species -Brucella: --ruminants, dogs -Salmonella: --horses, cows, sheep -E. coli: --all |
|
|
Listeria Monocytogenes
|
-Affects ruminants and primates
-Associated with rotting vegetation -Multifocal necrotizing and suppurative chorionitis and fetal septicemia -Coccobacilli are visible with histochemical and immunohistochemical stains -Causes abortions, neonatal deaths, encephalitis -Only affects the brainstem in sheep and cattle |
|
|
Cysts in the Vulva and Vagina
|
-Arise from Gartner ducts (Wolffian remnants) or from vestibular glands of Bartolinus
-Hyperestrogenism or inflammation can predispose formation -Need to remove the entire cyst for it not to come back |
|
|
Vulvo-vaginitis
|
-Viral, bacterial, mycotic, traumatic, or chemical damage
-infectious pustular vulvovaginitis due to BHV1 or BHV4 -Can be due to multi-systemic illness --Taylorella equigenitalis |
|
|
Vulvular Edema
|
-In pigs
-Zearalenone toxicity -Estrogenic -Can cause reproductive issues |
|
|
Neoplasia of the Vulva and Vagina
|
-Leiomyoma
--most common in dogs -Squamous cell carcinoma --due to UV radiation and papillomavirus -Fibropapilloma --most common tumor in cow vulva -Transmissible Venereal Tumor --not common in US |
|
|
Scrotal dermatitis
|
-Trauma predisposed to increase in size due to testicular neoplasms
-Skin diseases |
|
|
Developmental Abnormalities of the Testes
|
1. Cryptorchidism
2. Hypoplasia 3. Degeneration |
|
|
Cryptorchidism
|
-Incomplete descent of the testis
-Often genetic condition, sex-limited autosomal recessive -Most common genital disorder in male cat and horse -Can be unilateral of bilateral, unilateral is more common -May be due gubernaculum testis lack of development, improper position, excessive growth, failure to regress -After puberty retained testis becomes small and fibrotic -Histologically testicle is hypoplastic and degenerate |
|
|
Cryptorchidism predisposing factors
|
-testicular hypoplasia
-Estrogen exposure during pregnancy -Breech labor, interfering with blood supply to the testes -Delayed closing of the umbilicus, causes delayed ability to increase abdominal pressire |
|
|
Cryptorchidism sequelae
|
-Reduced fertility
-predisposition to developing tumors, remove undescended testicle! |
|
|
Causes of testicular hypoplasia
|
-Cryptorchidism
-Intersex development -Poor nutrition -Gonadotropin deficiency -Specific genes -Endocrine or cytogenetic abnormality -Ketoconazole, ethanol, acetaldehyde, cannabinoids |
|
|
Testicular degeneration
|
-Testicle was normal and shrank
-Common -Multiple causes and mechanisms -Targets are sertoli cells, germ cells, or interstitial cells --usually all 3 are affected -More mature stages of spermatogenesis are preferentially affected |
|
|
Orchitis
|
-Inflammation of the testicle
-Intratubular -Necrotizing -Granulomatous -Can have ectopic germplasms after rupture of tubules --act like foreign bodies --Immune privileged sites, germ cells can cause foreign body rxn -Process can spread to epididymis and tunnica vaginalis -Fistula rarely develops through scrotum |
|
|
Testicular Neoplasia
|
-Germ cell tumors:
--seminoma --teratoma -Gonadal stromal tumors --Sertoli cell tumor --interstitial cell tumor/leydig cell tumor |
|
|
Seminoma
|
-Germ cell tumor
-From primitive seminiferous epithelium -Does not produce significant levels of hormones -Multicentric origin within the testes -Locally invasive without metastasis --Metastasis is possible in horse and humans -Soft and bulging when cut, has fine fibrous trabeculae |
|
|
Sertoli Cell Tumor
|
-gonadal stromal tumor
-Firm, white mass with fibrous tissue dividing it into lobules -Locally invasive and may metastasize -Spindle cells organized in tubules and/or sheets -BIG tumor, occludes normal tissue -Usually local, but can metastasize -Produce estrogen, have feminizing effect --also causes bone marrow toxicity and other effects |
|
|
Sertoli Cell Tumor and Estrogen
|
-1/3 of all sertoli cell tumors produce estrogen
-Bone marrow toxicity --non-regenerative anemia --granulocytopenia --thrombocytopeina -Liver damage can occur -Hypothyroidism and alopecia -Hyperplasia or squamous metaplasia of prostate acini -Will have atrophy of testicles/penis -Reduced libido |
|
|
Interstitial Cell Tumor
Leydig Cell Tumor |
-Tan/orange
-Most common testicular tumor in dogs -Non-invasive, finely encapsulated -Generally not hormonally active --if androgens are produced, usually does not cause hyperandrogenism -Histologically looks like round/polyhedral/spindle shaped cells --have vacuolated cytoplasm |
|
|
Spermatic granuloma
|
-Sperm escapes from normal containment
--acts as foreign body -Can be due to trauma or influx of urine along the vas deferens -Can occur due to infections (Brucella) |
|
|
Prostatitis
|
-Inflammation of the prostate
-Usually ascending, organisms invade via prostatic urethra -Most often gram- bacteria -Can be due to trauma |
|
|
Porstate Hyperplasia
|
-Common in old dogs and old humans
-Hypertrophy with enlargement -Altered androgen:estrogen ratio -Castration is preventative and therapeutic -Acinar hyperplasia can be due to androgenic effects or other steroids -Fibromuscular hyperoplasia may be caused by estrogen excess |
|
|
Prostate Squamous Metaplasia
|
-Squamous metaplasia of the acinar prostatic epithelium
-Adds to estrogen-induced hypertrophy of the prostate -Often due to presence of sertoli cell tumor |
|
|
Prostatic adenocarcinoma
|
-most common prostatic neoplasm
-Most common in old dogs -Derived from prostatic glandular epithelium of alveoli and ducts -Very aggressive neoplasm --70-80% of cases metastasize at time of diagnosis |
|
|
Transmissible Venereal Tumor
TVT |
-Transmissible neoplasm
-On the genitalia of both sexes of dogs -Mesenchymal, round/oval cells -May spontaneously regress -Transmissible neoplasm! -Genetically distinct from host |
|
|
Squamous cell carcinoma on Penis
|
-Mostly in dogs and horses
-Proliferative and ulcerative lesion -Exophytic, ulcerative mass -Can be locally invasive and hard to excise -Can look like sarcoids on horses, Biopsy!! |
|
|
Embryology of the mammary Glands
|
-Appear as 2 linear thickenings or ridges
--"milk lines" -Detectable on the ventrolateral ectoderm of the dog embryo at day 25 of gestation -Supported by specialized mesoderm -Extend from axillary to inguinal region -Overlying epithelial cells and underlying mesenchymal cells -Development occurs due to communication between ectodermal/epithelial cells and mesenchymal cells |
|
|
Development of the mammary gland
|
-Ectodermal cells migrate along the mammary lines, coalesce into placodes
-Each placode gives rise to a single gland -Ectodermal cells of the placode proliferate to form solid cords (mammary buds) -Mammary buds sprout into the underlying mesoderm as a branching structure -Number of sprouts determines the number of papillary duct orifices that will develop on each nipple sheath |
|
|
Nipple Sheath
|
-Area of specialized epithelium
-Forms the raised teat in adults -Evagination -Each teat usually has several duct orifices -Each duct branches into a lobe of the adult gland --acts as an individual functional unit -Number of teats depends of species, number of teat orifices depends on species |
|
|
Duct orifices per teat
|
Dog: 7-16, can get up to 22
Cat: 4-7 Ruminant: 1 |
|
|
Mammary glands per species
|
-Goat and sheep: 2 teats
-Mare: 4 glands, 2 teats -Cow: 4 glands, 4 teats -Sow: 8-18 glands and teats -Primates: 2 glands, 2 teats More teats allows for more developing embryos |
|
|
Dog mammary glands
|
-Usually develop 5 pairs of glands
-2 thoracic -2 abdominal -1 inguinal Different glands will metastasize to different regional lymph nodes |
|
|
Cat mammary glands
|
-4 pairs of glands
-Axillary pair -Thoracic pair -Abdominal pair -Inguinal pair -At birth, only large ducts have developed (teat is not fully developed) --only extend a short distance into the underlying mesenchymal tissue from the teat -With puberty, release of estrogens from ovary induces cell proliferation at the terminal ends of the ducts -Release of estrogen stimulates formation of ductal system |
|
|
Terminal End Buds
|
-Terminal ends of the large ducts in a cat
-Induced by estrogen at puberty to develop and grow -Site of stem cell proliferation -Form alveolar system and secretory gland |
|
|
Estrogen and mammary duct proliferation
|
-Stimualtes proliferation of the ducts at the onset of puberty
|
|
|
Progesterone and mammary ducts
|
-Increased progesterone induces formation of lobules and alveoli
-Levels increase in diestrus and pregnancy -Allows for formation of milk secretory unit (alveoli) |
|
|
Prolactin and mammary ducts
|
-Pre-secretory alveolar cells differentiate into secretory alveolar cells
-Increase in the size and number of secretory alveolar cells |
|
|
Mammary gland at parturition
|
-Secretory ductal-lobular-alveolar structure
|
|
|
Duct development "clock"
|
1. Pre-pubertal or 1st pro-estrus: small duct
2. Pro-estrus: early ductules, early lobules 3. Oestrus: some intralobular loose stroma 4. Early diestrus: more intralobular loose stroma 5. Late diestrus: Ductal branching, alveolus formation 6. Early anestrus: alveolar regression, regressive features present in alveoli 7. Late anestrus: all inactive lobules and regressive features |
|
|
Normal Histology of the mammary gland
|
-Multiple papillary ducts open to teat surface
-Teat ducts are lined by stratified squamous epithelium --surrounded by a highly protective circular smooth muscle sphincter -Longitudinal and transverse smooth muscle fibers and elastin within the dermis of the teat and along larger ductal system --Smooth muscle constricts when milk is present, release when milk needs to be let down -Sebaceous glands empty onto the skin NOT into hair follicle -Gradual transition of cells |
|
|
Mammary tree of life
|
Secretory unit → ductal units → reservoir → environment
|
|
|
Histology of Teats
|
-Each teat duct opens into the teat sinus
--teat sinus is lined by bilayered cublidal to columnar epithelium --flattened myoepithelial cells on outside -Interlobular ducts empty into the teat sinus --have bilayered cublidal epithelium with peripheral myoepithelial cells -Smaller interlobular ducts are lined by monolayer of cublidal epithelial cells --fewer peripheral fusiform myoepithelial cells --allows for "peristalsis" of the duct |
|
|
Ductal growth
|
-Elongation and branching occur due to epithelial cell proliferation
-Penetrate through the gaps between myoepithelial cells -Occurs with estrogen and progesterone stimulation |
|
|
Mammary alveoli
|
-Functional unit of the Mammary gland
-Lined by a single layer of epithelial cells and externally star-shaped myoepithelial cells -Seretory phase epithelium is cuboidal to columnar with intracytoplasmic lipid droplets --fat in milk -Epithelial and myoepithelial cells reside on and produce basement membrane --mostly collagen IV, laminins, and heparin sulfate proteoglycans |
|
|
Myoepithelial cells in normal mammary tissue
|
-Stellate, NOT fusiform
|
|
|
Mammary stroma
|
-Supports epithelial structures
-Derived from specialized mesoderm -Subdivided into intralobular stroma and interlobular stroma -INTRAlobular stroma: loosely arranged and finer collagen bundles -INTERlobular stroma: Separates lobules, formed by thicker and more tightly organized collagen bundles |
|
|
Mastitis
|
-Infection of the mammary gland
-Economically important disease --Causes severe economic loss, esp. in cows -Less common in ovine and caprine -Rare in other species -Most cases are caused by bacteria |
|
|
Bacteria causing mastitis
|
1. Staphylococcus agalactia, staphylococcus aureus, mycoplasma
-Mammary gland serves as the reservoir -Persistent infection 2. E. coli -Environmental reservoir, infection from environment -SEVERE inflammatory response 3. Streptococcus uberis, streptococcus dysgalactia -Mammary gland or environment is the reserovir -Organisms can persist in mammary gland OR environment |
|
|
Mastitis infection
|
-Usual route of entry is via the teat duct
--lined by stratified squamous epithelium -Bacteria colonize and multiply on the surface, cause intramammary infections -Acute inflammatory response occurs, inflitration with chronic inflammatory cells -Healing via fibrosis can occur -Granulomatous mastitis caused by mycobacterium bovis can spread to humans in raw milk |
|
|
Viral Mastitis
|
-Ovine progressive pneumonia virus
--lentivirus --mastitis in sheep -Caprine arthritis-encephalitis virus --lentivirus --causes mastitis in goats |
|
|
Acute mastitis Histology
|
-Basal lamina is gone
-Neutrophilic and macrophage infiltration -No more cuboidal/columnar cells lining ducts -Will get fibrosis with chronicity |
|
|
Basics of Canine Mammary Tumors
|
-Classical presentation
-Older female dog -Wide range of breeds -Sexually intact or spayed later in life -One of more palpable tumors in the mammary chain --usually more than one gland is affected |
|
|
Risk factors for mammary tumor development
|
-Age
-Hormonal exposure, endogenous or exogenous -Breed --smaller breeds live longer and are more likely to develop tumors -Diet -Obesity has unknown associated risk |
|
|
Age and Canine Mammary tumors
|
-Older dogs around age 8 and older
-Peak incidence of mammary tumor between 9-11 years old -Age of onset can vary depending on natural lifespan of breed -Rare in dogs under 5 unless given exogenous hormones (progestins) -Lipid-rich secretory carcinomas can be seen in younger dogs |
|
|
Hormones and canine mammary carcinoma
|
-Endogenous ovarian hormones early in life is the most important source and cause of mammary tumor development
-Spay before 1st estrus has 0.05% risk of mammary neoplasm --no ductal development, no tissue to become cancerous -Spay before 2nd estrus has 8% risk -Spay after 2nd estrus has 26% risk -Spay after 4 years old no protection -Estrus irregularity, pseudo-pregnancy, and pregnancy have not been found to influence mammary tumor risk |
|
|
Progestins and Mammary tumor risk
|
-Progestin-treated dogs have a significantly increased risk of cancer
|
|
|
Diet and Obesity contributing to Mammary tumors
|
-Thinner dogs have decreased risk of mammary tumors
-Obese dogs or dogs fed a high fat diet later in life are not more likely to develop mammary tumors -Dogs fed a diet high in red meat and dogs obsese at 1 year old are more likely to develop mammary tumors |
|
|
Common clinical presentation of Canine Mammary carcinoma
|
-Commonly have more than 1 tumor
--Close to 70% -Caudal 2 pairs of glands are most commonly affected --more mammary and adipose tissue -Tumors can be large or small, fixed or freely moveable, ulcerated or not -Best if removed when less than 1 cm -Lymph nodes may or may not be clinically enlarged |
|
|
Gynecomastia
|
-Enlargement of the mammary gland in the male dog
-Common with sertoli cell tumors |
|
|
Mammary hyperplasia/dysplasia
|
-Duct ectasia, dilated duct that can enlarge and become a cyst
-Lobular hyperplasia (adenosis) --increase in number of minor ducts or intralobular ducts -Epitheliosis: intraductal proliferation -Papillomatosis: proliferation of epithelium without supporting stroma -Fibroadenomatous change |
|
|
Mammary Duct ectasia vs. ductal cyst
|
Duct ectasia: dilated duct
-less than 5mm Ductal cyst: -more than 5mm |
|
|
Mammary gland Lobular hyperplasia
Adenosis |
-Increase in the number of minor ducts/intralobular ducts
-Can be regular -Can have secretory activity (lactational) Can have fibrosis- interlobular fibrous connective tissue -Can be atypical, nuclei and cells do not look normal |
|
|
Mammary Epitheliosis
|
-Intraductal proliferation
-Affects intralobular ducts -Proliferation of epithelial cells within the lumen of the intralobular ducts -Epithelial cells can fill the lumen -Nuclei are regular, hyperchromatic with little pleomorphism -Pre-neoplastic change |
|
|
Papillomatosis
|
-Multifocal papilliferous proliferation of the interlobular ducts
-Affects inter lobular ducts -Papillae are not supported by fibrous stroma |
|
|
Benign mammary neoplasms
|
-Adenoma: simple
-Intraductal papillary adenoma (duct papilloma) -Ductal adenoma (basaloid adenoma) --with squamous differentiation -Fibroadenoma -Myoepithelioma -Complex adenoma (adenomyoepithelioma) -Mixed tumor |
|
|
Mammary Mixed tumor
|
-benign
-Ductal epithelium and myoepithelial cells are neoplastic -Common in dogs, uncommon in all other animals -Will have all sorts of tissues developing |
|
|
Intraductal papillary adenoma
|
-Duct papilloma
-Can block duct |
|
|
Tubular carcinoma
|
-When the neoplastic cells infiltrate into the surrounding mammary tissue and illicit a stromal response
-Variations on formation of tubular structure in mammary gland -Desmoplasia is bad news! |
|
|
Anaplastic Mammary carcinoma
|
-Worst neoplasm in the mammary gland of a dog
-Short prognosis -Readily metastasize to lymph nodes and lungs -Infiltrate the lung interstitium --looks like interstitial pneumonitis |
|
|
Inflammatory Mammary Carcinoma
|
-Clinical term, not pathological
-Looks like it should be mastitis but it is not -Sudden presentation with edema, erythema, firm and warm mammary gland -Can occur with or without mammary nodules -May have erosions and exudates -Histologically looks like invasion of dermal lymphatic vessels by neoplastic emboli --blockage of lymphatics -Metastatic disease! |
|
|
Mammary Osteosarcoma
|
-Malignant transformation of a benign mixed turmor
-Will metastasize by blood to the lungs -Remove mixed adenomas early so they do not develop into mammary osteosarcoma --take off when small! |
|
|
Malignant mixed mammary tumor
|
-Carcinosarcomas
|
|
|
Fibroadenomatous change in the mammary gland
|
-Proliferation of interlobular ducts and periductal stromal cells
-Stroma is often edematous or myxomatous -Nuclei exhibit some pleomorphism, mitoses present -Cells are hyperplastic and dysplastic, not cancerous -Progestins/Progesterone administration can cause formation --used for behavior issues in males --birth control in females |
|
|
Mamamry tumors in Cats
|
-95% are malignant!!
-Assume malignant until proven benign -Usually are of suubstantial size -teats do not enlarge |
|
|
Grading of Mammary carcinoma
Tubule formation |
1. more than 75% of whole carcinoma forms tubules
2. 10-75% of carcinoma forms tubules 3. less than 10% of the carcinoma forms tubules |
|
|
Grading of mammary carcinoma
Nuclear Atypia/pleomorphism |
1. Nuclei are only slighly larger than normal epithelium
2. Nuclei are distinctly larger, often vesicular, nucleoli are visible -May have variable size and shape, but not always 3. Markedly enlarged nuclei, often vesicular, prominent nucleoli, marked variation in size and shape |
|
|
Grading of Mammary Carcinoma
Mitotic counts |
-Count definite mitoses in 10 consecutive high-power fields
1. less than 10 mitoses 2. 10-19 mitoses 3. more than 20 mitoses -Mitotic frequency score will vary considerably depending on the field diameter of your microscope |
|
|
Final grading of Mammary carcinomas
|
-Add together Tubule formation score, Nuclear atypia/pleomorphism score, and mitotic count score
1. score 3, 4, 5: metastasis is low 2. score 6, 7: gray area 3. score 8 or 9: metastasis is high |
|
|
Features of the Endocrine System
|
-Widely Distributed
-Highly Integrated -Involved with endocrine signaling -Under feedback inhibition |
|
|
Feedback Inhibition
|
-Increasing activity at the target tissue decreases the activity of the gland that secretes stimulating hormone
|
|
|
Types of Hormones
|
1. Interact with cell surface receptors
2. Diffuse across cell membrane to interact with nuclear or cytosolic receptors |
|
|
Hormones interacting with Cell Surface receptors
|
-Short half-life
-Water soluble -Polypeptides (insulin) -Small molecules (epi, norepi) -Binding to receptor stimulates intracellular signaling molecules --2nd messengers -Leads to production of mediators and shifts intracellular Ca -Influences cell proliferation, differentiation, function, and survival |
|
|
Hormones diffusing across the cell membrane
|
-Interact with nuclear or cytosolic receptors in cell
-Bind to recognition eelements in the DNA -Steroid hormones: progesterone, glucocorticoids, estrogen --lipid in cytoplasm, allows diffusion across cell membrane --long half-life -Tyrosine derivatives (thyroid hormones) |
|
|
Organs in the endocrine system
|
-Pituitary gland
-Thyroid gland -Parathyroid glands -Adrenal glands -Pancreatic islets -Paraganglia -Renal JG apparatus -Ovary/testis -Neuroendocrine cells Always look at both organs when there is a pair! |
|
|
Mechanisms of Endocrine Disease
|
1. Too little hormone
2. Too much hormone 3. Body is unable to utilize the hormone |
|
|
Causes of Too Little Hormone
|
1. Primary hypofunction: sub-normal hormone secretion
2. Secondary Hypofunction: destructive process interferes with secretion of hromone |
|
|
Primary Hypofunction of an Endocrine gland
|
-Sub-normal hormone secretion
-Destruction by a disease process: --immune-related injury causes hypofunction --thyroiditis, adrenalitis --primary inflammation in the gland interferes with function -Failure of organ to develop --issue with pituitary decreases GH, leads to dwarfism -Biochemical defect in the hormone |
|
|
Secondary hypofunction of an Endocrine Gland
|
-Destructive process interferes with secretion of trophic hormone
-Destructive lesion in one organ will result in failure to secrete hormone → hypofunction in target organ -Pituitary tumor, no releasing hormones, no hormones released |
|
|
Primary Hyperfunction of an Endocrine Gland
|
-Leads to too much hormone produced, increased hormone levels
-Functional tumor in an endocrine gland --parathyroid adenoma --islet cell tumor --sertoli cell tumor --thyroid adenoma or adenomatous hyperplasia -Neoplasms secrete hormone in excess of body's ability to degrade the hormone -Very important mechanism in domestic animals |
|
|
Examples of primary hyperfunction of an endocrine gland
|
1. Parathyroid chief cell adenoma → parathyroid hormone production → fibrous osteodystrophy
2. Beta cell adenoma of pancreatic islet → insulin producion → hypoglycemia 3. Sertoli cell tumor → estrogen production → feminization 4. Thyroid follicular cell adenoma → T4/T3 production → increased BMR |
|
|
Secondary hyperfunction of an endocrine gland
|
-Lesion (usually a functional tumor) in one organ secretes excessive tropic hormone
-Target organ is stimulated → hypersecretion by target organ -Ex: pituitary gland tumor → ACTH → adrenal cortex stimulation → excessive cortisol |
|
|
Anal sac apocrine gland carcinoma
|
-Functional tumor of non-endocrine tissues
-Mimics natural hormone, stimulates same activity that hormone would -Causes paraneoplastic syndrome |
|
|
Endocrine Dysfunction secondary to failure of target cell response
|
-Hormone is produced at normal levels but target cell cannot respond
-Defective target -May be due to lack of adenylate cyclase in cytoplasm or lack of hormone receptors -Cells of 1st gland will become hypertrophic, no negative feedback and no response from cells |
|
|
Endocrine Dysfunction due to abnormal degradation of hormone
|
-Secretion is normal but blood levels of the hormone are elevated
-Decreased rate of degradation stimulates hyposecretion in endocrine organ --constant negative feedback |
|
|
Endocrine hyperactivity secondary to diseases of other organs
|
-Hyperparathyroidism that develops secondary to chronic renal failure or nutritional imbalances
-Retention of P and decrease in Ca (Increase in P:Ca ration) -Leads to parathyroid stimulation -Decreased kidney fxn leads to decreased vitamin D activation, less Ca absorbed from intestine →Progressive hypocalcemia -Causes chronic parathyroid hyperplasia and generalized demineralization of the skeleton --body wants Ca from skeleton |
|
|
Iatrogenic syndromes of Hormone excess
|
-Administration of exogenous hormone causing functional disturbances
-Prolonged Administration of glucocorticoids → disturbances associated with hypersecretion of cortisol, hyperadrenocorticism → atrophy of adrenal cortex -Excessive T4/Thyroxine → hyperthyroidism -Excessive insulin → hypoglycemia |
|
|
Glucocorticoid administration
|
-Iatrogenic cause of hormone excess
-Given to suppress immune system -Can lead to disturbances associated with hypersecretion of cortisol --atrophy of the adrenal cortex -Prednisone, dexmethasome |
|
|
Endocrine Dysfunction due to failure of fetal endocrine function
|
-Leads to prolonged gestation
-Abnormalities in fetal pituitary development can result in prolonged gestation |
|
|
Pituitary gland
|
-Small bean-shaped organ
-Sits in the sella turcica below the brain -Attached to the hypothalamus by pituitary stalk -Anterior lobe (adenohypophysis) -Posterior lobe (Neurohypophysis) |
|
|
Adenohypophysis
Anterior pituitary |
-Comprises most of the pituitary gland (80%)
-Derived from Rathke's pouch -Portal vascular system allows transport of hypothalamic releasing hormones from hypothalamus to the pituitary -Pars distalis: largest, secretes trophic hormones -Pars tuberalis: wraps around the neural stalk --capillary network of hypophyseal portal system from median eminence to pars distalis -Pars intermedia: junction between pars distalis and pars nervosa |
|
|
Pars Distalis
|
-in Adenohypophysis
-Synthesizes and secretes pituitary trophic hormones -Acidophils: --Somatotrophs secrete growth hormone --Luteotrophs secrete luteotropic hormone (Prolactin) -Basophils: --Thyrotrophs secrete TSH --gonadotrophs secrete LH and FSH -Chromophobes: --Secrete ACTH and MSH |
|
|
Neurohypophysis
Posterior pituitary |
-Modified glial cells and axonal processes
-Extend from the nerve cell bodies in the supraoptic and paravenricular nuclei through the pituitary stalk to the posterior lobe -Secretes ADH and Ocytocin -Supplied by an artery and drains into a vein, hormones are released directly into systemic circulation |
|
|
Hypothalamic control of the pituitary
|
-All cell populations in the pituitary are controlled by releasing hormones produced in the hypothalamus
-Negative feedback occurs via hormone produced by endocrine gland or specific inhibitory hormones -Primary center for regulation of body temp, appetite, and seasonal shedding |
|
|
Antidiuretic hormone
ADH Vasopressin |
-Produced in supraoptic nucleus
-Released in response to various stimuli --plasma osmotic pressure --left atrial distention --exercise --emotional states -Acts on renal collecting ducts and distal nephron -Increases water resorption from the glomerular filtration -Counteracts dehydration |
|
|
Oxytocin
|
-Stimulates contraction of smooth muscle in the uterus and myoepithelial cells surrounding the mammary gland ducts
|
|
|
Hyperfunction of the Pituitary gland
|
-Neoplasm is the most likely cause
--functional corticotroph adenoma -Pars distalis adenoma is most common in dogs -Pars intermedia adenoma is most common in horses -Different clinical presentations with neoplasms in different areas |
|
|
Functional Corticotroph Adenoma
|
-Causes hyperfunction of the pituitary gland
-Produces excessive ACTH -Acts on adrenal gland cortex -Glyconeogenic -Results in protein catabolism --atrophy of temporal muscles |
|
|
Clinical findings with Functional corticotroph adenoma
|
-Signs associated with too much cortisol
-Pituitary will be enlarged --may expand and compress thalamus or hypothalamus → hemorrhage, necrosis, mineralization → CNS signs, blindness, behavioral change, seizures -Adrenal glands will have cortical hyperplasia, affects zona fasciculata much more than zona reticularis |
|
|
Equine Pituitary Pars Intermedia Dysfunction
|
-Adenoma of pars intermedia
-Associated with Equine Cushing's syndrome --NOT the same as cushing's syndrome in other animals -Autonomous production of POMC peptides -Loss of normal inhibitory control |
|
|
Equine Cushing's Syndrome
Pituitary Pars Intermedia Dysfunction PPID |
-Due to pituitary tumor in the pars intermedia
--Autonomously functional chromophobe adenoma -Associated with autonomous production of pituitary POMC peptides --loss of normal inhibitory control -Decrease in dopamine in pars intermedia --normally inhibits cells (melanotrophs) -Loss of inhibition of melanotrophs → increased synthesis of peptides → hyperthrphy and hyperplasia → adenoma formation -Plasma cortisol inhibits ACTH secretion by the pars distalis, but does not affect pars intermedia -Increased ACTH and other peptides that potentiate ACTH → adrenocortical hyperplasia → cushing's like disease |
|
|
Clinical signs due to deranged hypothalamic function
|
-Excessive POMC derived peptides
-Compression tumor on hypothalamus -Weight loss, muscle weakness and atrophy --catabolic effects of cortisol -Increased susceptibility to infection and poor wound healing --anti-inflammatory and immunosuppressive effects of cortisol -PU/PD -Laminitis -Hypertrichosis, no seasonal shedding -Intermittent fever -Behavioral changes -Generalized swelling |
|
|
Functional Acidophilic adenoma
|
-Acidophils produce growth hormone
-Occasionally seen in middle-aged to older male cats -Clinical signs related to increased production of GH -Leads to Acromegaly |
|
|
Feline Acromegaly
|
-Syndrome of bone and soft-tissue overgrowth
-Insulin resistance due to excessive GH secretion -New bone deposition → broadening of the face -Increased weight due to increased muscle/bone/organ mass -Respiratory stridor due to thickening of airway mucus membranes -Severe insulin-resistant diabetes mellitus --due to GH induced insulin resistance -Death is typically due to renal or congestive heart failure, progressive CNS disease due to tumor enlargement |
|
|
Acromegaly and Diabetes mellitus
|
-Due to GH-induced insulin resistance
-Decrease in target cell insulin receptors -Decreased receptor affinity -Undefined post receptor insulin defect |
|
|
Hypofunction of the Pituitary gland
|
1. Compressive Disease
2. Lack of target organ receptors 3. Congenital malformations 4. Prolonged gestation due to dysfunction of fetal pituitary |
|
|
Compressive disease of the Pituitary
|
-Major cause of hypofunction
-Usually Pituitary neoplasia -Can be functional or non functional --non-functional: signs due to compression, lack of secretion of trophic hormones -Can expand and destroy remaining pituitary and hypothalamus -Pituitary carcinomas are usually non-functional but may result in secondary disturbances --destruction of anterior and posterior pituitary --compressive and inflitrative |
|
|
Diabetes Insipidus
|
-Hypofunction of the Pituitary gland
-Caused by inadequate production of ADH or failure of target cells in the kidney to respond to ADH -Inadequate ADH → drinking and excretion of large volumes of water -Compression/destruction of neurohypophysis → inadequate ADH production → Diabetes insipidus |
|
|
Nephrogenic Diabetes insipidus
|
-Target cells in kidney cannot respond to ADH
-Congenital lack of adenylate cyclase in cytoplasm -Secondary Diabetes indipidus can develop in animals with pyometra -Cells lack target organ receptors |
|
|
Juvenile Panhypopituitarism
Pituitary dwarfism |
-Congenital malformation of pituitary
-Pharyngeal ectoderm fails to differentiate into hormone-secreting cell populations -Undifferentiated cells produce fluid, causes large cysts in the sella turcica -Abscence of adenohypophysis -Autosomal recessive trait in German Shepherd dogs --occasionally seen in other dog breeds -Clinical signs due to growth hormone deficiency -TSH and ACTH stimulation tests are often normal --hypothyroidism and hypoadrenocorticism do occur in some cases -Individual will be normal at birth, then will not grow or grow slowly |
|
|
Clinical signs of Juvenile Panhypopituitarism
|
-Small stature
-Failure to grow, or slow growth -Failure to gain adult hair coat -Delayed eruption of permanent teeth -Delayed epiphyseal closure -External genitalia will be infantile |
|
|
Pituitary cysts
|
-Can either be due to Juvenile panhypopituitarism (genetic) OR incidental
-Not all cysts are associated with developmental disorders -Pit cysts are relatively common in dogs but dwarfism is rare |
|
|
Prolonged gestation due to dysfunction of fetal pituitary
|
-Causes hypofunction of the pituitary
-In ruminants is secondary to ingestion of plat toxin -Veratrum californicum ingestion in early gestation will cause severe cranial malformations |
|
|
Thyroid gland Physiology
|
-Thyroid follicle is the functional unit of the thyroid gland
--Single layer of epithelial cells surrounding protein-rich colloid -If active, cells are cublidal to columnar with less colloid inside -If inactive, cells are flattened and more cuboidal with more colloid inside -C-cells (parafolicular cells) secrete calcitonin to act opposite PTH |
|
|
Thyroid Physiology
|
-Thyroid follicular cells uptake dietary iodine
-Binds thryroglobulin in the lumen, forms Thyroxine (T4) and thriiodothyronine (T3) --thyroid peroxidase= enzyme that does the binding -re-uptake of thyroglobulin by thyroid epithelial cells leads to release of T3 and T4 into the bloodstream -99% of T3 and T4 are bound to plasma proteins in the blood --Free T3 and T4 are physiologically active --almost all is bound to proteins --Anything that changes plasma protein levels will also affect T3 and T4 |
|
|
Thyroid peroxidase
|
-Enzyme that binds iodine to thyroglobulin in the thyroid gland
-Allows formation of Thyroxine (T4) and triiodothyronine (T3) -Can be inhibited |
|
|
T3 vs T4
|
-Triiodothyronine= T3
-Thyroxine= T4 -Both are bound to plasma proteins in blood -T3 is more physiologically active than T4 -T3 is formed from deiodination of T4 --T4 is converted to T3 in cells |
|
|
Measuring Thyroid Hormone
|
-measure FREE T4
-T3 is unreliable -Need to know total T4 and free T4 to get an idea as to TSH activity |
|
|
Common Thyroid Diseases
|
1. Hyperfunction: too much thyroid hormone
-More common in cats 2. Hypofunction: too little thyroid hormone -more common in dogs |
|
|
Feline Hyperthyroidism
|
-Common in older cats
-Multifocal, firm, brown nodules composed of well-differentiated thyroid tissue -Adenomatous hyperplasia -Nodules produce thyroxine and negatively inhibit TSH -Will have increased T4 and T3, decreased TSH -Leads to thyroid gland atrophy, nodules are producing what the body uses -Often bilateral -Will have elevated T4 and T3 levels |
|
|
Feline Hyperthyroidism Clinical Signs
|
-Weight loss with ravenous appetite
-Nervousness, tachycardia -heat intolerance, HOT animal -Weakness -Cardiomegaly, hypertrophy of cardiac muscle -Arrythmias -Saddle thromboemboli and death |
|
|
Canine Hypothyroidism Causes
|
1. Lymphocytic thyroiditis
2. Idiopathic atrophy |
|
|
Lymphocytic thyroiditis
|
-Inflammation of the thyroid gland
-Results in canine hypothyroidism -Immune-mediated -Thyroid gland is infiltrated by lymphocytes, plasma cells, and macrophages -Clinical signs start to appear when 75% of the gland is destroyed -beagles have a genetic component -Thyroid gland damage leads to release of antigens into circulation --will see antibodies to thyroglobulin in the blood |
|
|
Idiopathic Atrophy of the Thyroid Gland
|
Leads to hypothyroidism
-Gland can be 1/10 of normal size -Replaced by adipose tissue and fibrous connective tissue -May be end-stage of lymphocytic thyroiditis -Histologically will see adipose tissue and blue areas of blue lymphocytes in the thyroid parenchyma |
|
|
Clinical signs of Canine Hypothyroidism
|
-Slowing of metabolism
-lethargy -Exercise intolerance -Heat-seeking animals, always cold -Mental dullness -Weight gain -Bradycardia, slow pulse -Neuromuscular and reproductive problems --facial nerve paralysis -Mild non-regenerative anemia -Hypercholesterolemia (rare) --atherosclerosis in dogs usually indicates hypothyroidism -"Tragic face" because skin is filled with mucin |
|
|
Dermatologic lesions associated with Canine Hypothyroidism
|
-Controversial
-Scaling, bilateral alopecia that may be subtle --excessive stratum corneum, scales on coat, NOT a crust --rat tail -Myxedema if severe --tragic face, mucin build up in skin -Secondary infections --otitis, ptoderma |
|
|
Iodine Deficiency
|
-Most common preventable cause of mental retardation worldwide
-No adequate maternal iodine, fetus and mother are hypothyroid -no supplemental iodine, fetus may develop cretinism --mental retardation, deaf-utism, spasticity |
|
|
Goiter
|
-Bilateral enlargement of the thyroid glands due to non-neoplastic and non-inflammatory causes
-Indicates impaired synthesis of thyroid hormone -Results in euthyroid or hypothyroid state --thyroid levels can look normal or high |
|
|
Dietary causes of Goiter
|
1. Iodine deficiency
2. Ingestion of goitrogenic substances --substances that interfere with thyroid hormone synthesis --Brassica 3. Excessive iodine (rare) |
|
|
Thyroid Carcinoma
|
-Dog issue
-Usually malignant neoplasm -Can be unilateral of bilateral -Neoplastic cells break capsule, invade venous vasculature and get to heart and lungs quickly -Most likely dog is hypothyroid |
|
|
Thyroid adenomas
|
-Incidental findings on post-mortem exam of horses and cats
|
|
|
Parathyroid Glands
|
-Internal and external glands
-Embedded in thyroid glands or just crainal to the thyroid glands -Made of of Chief cells, one cell type |
|
|
Chief cells and Calcium homeostasis
|
-Chief cells produce PTH
-Ca retention, puts Ca into blood -Increases bone resorption for Ca mobilization -Dumps P in the kidney, reabsorbs Ca -Increases active vitamin D in the kidney -Increases intestinal absorption of Ca |
|
|
Calcitonin
|
-Produced by C-cells in thyroid
-Secreted in response to increased Ca in blood -Counters action of PTH -Acts on bone and kidney -Inhibits bone resorption |
|
|
Cholecalciferol
Vitamin D |
-Acquired from diet and epidermis
--precursor molecules from UV light -Epidermis converts provitamin D3 into Vitamin D3 -Vitamin D3 is hydroxylated in the liver then in kidneys to form 1,25 vitamin D3 -Increases absorption of Ca and P form intestines -Required for mineralization of bone matrix and endochondral ossification in young animals |
|
|
Hyperparathyroidism
|
-Too much Parathyroid hormone
-Primary cause: functional parathyroid adenoma -Increases blood Ca -Does not respond to negative feedback, Ca levels in blood stay high -Signs: anorexia, weakness, PU/PD, stiff gait, pathologic fractures, thickened mandible, loose teeth -Elevated serum PTH and Ca -Looks a lot like Anal sac carcinoma or lymphoma |
|
|
Secondary hyperparathyroidism
|
-Caused by chronic renal disease
-Decrease P secretion in the kidney → hyperphosphatemia, increase in P:Ca ratio -Decreased vitamin D3 → decreased Ca absorbed from intestine -high P → PTH secretion → parathyroid hyperplasia → release of Ca from bone -Signs: chronic renal disease --vomiting, PU/PD, dehydration --Fibrous Osteodystrophy |
|
|
Pseudohyperparathyroidism
|
-Hypercalcemia of Malignancy
-Anal sac apocrine adenosarcoma -Lymphosarcoma (most common neoplasm associated with hypercalcemia) -Parathyroid hormone related protein (PTHrP) is secreted by a tumor --Malignant tumor of non-parathyroid origin -PTH will be low, parathyroid glands atrophied |
|
|
Causes of Hypercalcemia
|
-Lymphosarcoma (PTHrP)
-Anal sac apocrine adenosarcoma (PTHrP) -Malignant tumors growing within bone due to bone resorption -Malignant neoplasms that metastasize to bone |
|
|
Hypoparathyroidism
|
-Very rare
-Can be iatrogenic with inadvertent removal of parathyroid glands --can't remove thyroid glands, may take away parathyroid glands also -Idiopathic: rare in dogs |
|
|
Adrenal gland Removal
|
-Leads to death within just a few days
-K in extracellular fluid becomes elevated -Urinary excretion of Na is high -Concentration of Na in extracellular fluid decreases significantly -Volume of extracellular fluid and blood decrease -Heart begins to function poorly --cardiac output declines, shock ensues -Due to direct loss of mineralocorticoid activity -Can be prevented by replacement of salts and mineralocorticoids from zona glomerulosa |
|
|
Adrenal Gland Anatomy
|
-Cortex and Medulla
-Cortex has 3 regions --Glomerulosa: mineralocorticoids --Fasciculata: glucocorticoids, stimulated by ACTH to make cortisol --Reticularis: sex hormones -medulla makes catecholamines (epi and norepi) -Normal cortex:medulla ratio is about 1:1 |
|
|
Gross lesions of the Adrenal Gland
|
-Lesions can be functional and produce cortisol, or non-functional
-Nodular cortical hyperplasia (usually incidental lesion) -Diffuse cortical hyperplasia (look for primary neoplasm in pituitary) -Cortical adenomas -Cortical carcinomas |
|
|
Cortisol
|
-Produced in the Zona Fasciculata of the Adrenal Cortex under ACTH stimulation
-Negatively inhibit ACTH from pituitary and hypothalamus |
|
|
Pheochromocytoma
|
-Neoplasm in the adrenal medulla
-Causes hyperfunction of the adrenal medulla |
|
|
Bilateral adrenocortical hyperplasia
|
-Hyperplastic adrenal cortex, atrophied adrenal medulla
-Due to increased ACTH stumilation -Results in increased cortisol levels in the blood -Due to functional tumor in the pituitary --cranks out ACTH regardless of negative feedback |
|
|
Exogenous cortisol effects on adrenal
|
-Atrophy of adrenal cortex, medulla will be normal
-Exogenous corticosteroids in blood are providing negative feedback to receptors in hypothalamus and pituitary --less ACTH released --Less stimulation for cortisol production in adrenal cortex -Cortisol just isn't needed |
|
|
Primary Adrenal Carcinoma
|
-Opposite adrenal gland will have an atrophied cortex
-Functional tumor is producing unregulated cortisol --cortisol is inhibiting ACTH release from hypothalamus and pituitary --no additional cortisol needed -Atrophy from consistently decreased ACTH levels |
|
|
Non-functional primary adrenal carcinoma
|
-Has no effect on adrenal gland
|
|
|
Adrenal medullary tumor
|
-Does not have an effect on the adrenal cortex
-Will increase HR (produces more epi and norepi) -Does not communicate with the pituitary/adrenal cortex axis |
|
|
Adrenal gland Hyperfuction
|
-Cushing's disease
-Main cause is functional adrenocortical adenoma/carcinoma -Secondary hyperfunction due to corticotroph adenoma in pituitary |
|
|
Zona glomerulosa
|
-Outer zone of adrenal cortex
-Produces mineralocorticoids --Aldosterone -Secretion of mineralocorticoids depends on renin/angiotensin system from kidneys and potassium -Activation results in increased Na and water resorption → increased renal perfusion -Not under control of the Hypothalamic-pituitary axis |
|
|
Aldosterone
|
-Produced in zona glomerulosa of the adrenal cortex
-Responds to angiotensin II in the blood --decrease in renal perfusion -Stimulates retention of Na and water from the kidneys, results in increased renal perfusion -Not under the control of the Hypohalamic-pituitary axis |
|
|
Zona Fasciculata
|
-Middle zone of the adrenal cortex
-Produces glucocorticoids in response to increased ACTH release from pituitary --High levels of corticosteroids will inhibit ACTH release from hypothalamus and pituitary |
|
|
Glucocorticoids
|
-Produced in zona fasciculata of the adrenal glands
-Increase glucose production -Catabolic effects on fat, muscle, lymphoid and connective tissue -Suppress immune system, inflammation, and collagen synthesis --leads to impaired wound healing -Under control of Hypothalamic-pituitary axis |
|
|
Zona reticularis
|
-Inner zone of the adrenal cortex
-Produces sex steroids and small amounts of glucocorticoids -Under control of the Hypothalamic-pituitary axis |
|
|
Adrenal Medulla
|
-Made up of chromaffin cells and a few ganglion cells
-Under controol of the sympathetic/parasympathetic nervous system -Chromaffin cells produce epi and norepi |
|
|
Cushing's Syndrome
|
-Hyperfunction of the adrenal cortex
-Pituitary cushing's syndrome: functional tumor in the anterior pituitary (secondary cushing's) -Adrenal Cushing's syndrome: functional tumor in the adrenal cortex (Primary cushing's) -Iatrogenic cushing's syndrome: exogenous corticosteroid use |
|
|
Clinical signs of Cushing's disease
|
-Middle-aged/older animal
-Elevated alkaline phosphatase -Pot belly, pendulous abdomen due to lack of tone in the abdominal muscles -PU/PD -Increased appetite -hepatomegaly -Muscle atrophy -Alopecia and thin skin -Calcinosis cutis -increased susceptibility to pathogens -Diabetes mellitus |
|
|
Feline hyperadrenocorticism
|
-Similar to dogs
-Cats are not usually PU/PD and no steroid hepatopathy -Often associated with diabetes mellitus due to cortisol-induced peripheral insulin resistance -May develop severe dermal atrophy and fragile skin -Can have functional adrenal or pituitary tumors |
|
|
Ferret hyperadrenocorticism
|
-Very common in middle-aged ferrets
-Signs are due to hyperestrogenism -Due to primary adrenal cortical tumor secreting estrogens -Serum cortisol is normally low |
|
|
Cushing's disease Classic presentation
|
-Pituitary: Middle aged or older animal
-Adrenal tumor: older female dog -Increased alkaline phosphatase liver enzyme -Pot belly -PU/PD -Increased appetite -Hepatomegaly -Panting |
|
|
Calcinosis cutis
|
-Mineralization of collagen in the skin
-Occurs in dogs only -Due to long-term exogenous steroids -Can become osseous plaques over time -Will get secondary folliculitis as body tries to get rid og Ca |
|
|
Adrenal medullary Hyperfunction
|
-Tumor of medullary chromaffin cells
--Pheochromocytoma -May cause tachycardia, hypertension, hyperglycemia, vasoconstriction, diffuse sweating -Clinical signs are hard to document in animals -Often ends up as an incidental finding -Benign tumors are more common than malignant -Malignant tumors metastasize widely, can infiltrate the vena cava |
|
|
Addison's disease
|
-Hypofunction of the adrenal cortex
-Affects all 3 zones -Adrenal gland will be small and atrophied --few cells in the capsule -Most often occurs in female dogs |
|
|
Adrenocortical insufficiency
Hypoadrenocorticism |
-Idiopathic loss/atrophy of all 3 cortical zones
-Addison's disease -Thought to be autoimmune disease -Loss or necrosis of cortical cells and lymphoplasmacytic inflammation leads to cortical atrophy -Gradual process that waxes and wanes --exacerbated by stress, no steroids are present to maintain homeostasis -Clinical signs appear with destruction of 90% of cortices --have to destroy A LOT of the cortex to get signs |
|
|
Addison's disease clinical signs
|
-Weakness, lethargy
-Collapse -Weak femoral pulse -Dehydration -Bradycardia -HYpothermia -Abdominal pain and GI signs (diarrhea) -Hypontremia and hyperkalemia with unconcentrated urine -Can present with sudden death -Zona glomerulosa is KEY for electrolyte balance, no aldosterone no electrolyte balance |
|
|
Clinical signs related to a decrease in aldosterone
|
-Hypovolemia
-Hypotension -Reduced CO -Hyperkalemia leading to decreased myocardial excitability -Increased refractory period, slowing of conduction -K is so high it is cardio-toxic -All due to destruction of the zona glomerulosa |
|
|
Clinical signs related to a decrease in Cortisol
|
-GI signs: anorexia, vomiting, abdominal pain
-Weight loss -Diminished energy metabolism -Impaired tolerance of stress |
|
|
Secondary Hypoadrenocorticism
|
-Loss of 2 adrenal cortical regions
-Due to long-term exogenous corticosteroids --Negative feedback to HPA, decreases ACTH, causes atrophy of fasciculata and reticularis -Lysodren treatment leading to selective destruction of fasciculata and reticularis -Renin-angiotensin loop is preserved -Clinical signs are due to decreased glucocorticoids |
|
|
Endocrine Pancreas Anatomy
|
-Islets of Langerhans cell types:
--Beta cells: produce insulin --Alpha cells: produce glucagon (counters insulin) --Delta cells: somatostatin --F cells: pancreatic polypeptide |
|
|
Insulin
|
-Produced by beta-cells in the exocrine pancreas islets of langerhans
-Increases cell uptake and storage of glucose, AA, fatty acids -Allows sugar to get into the cells -Secreted in response to hyperglycemia -Promotes storage of adipose tissue and prevents fat breakdown -Promotes anabolic effects of protein synthesis on muscles -Increases glycogen synthesis, decreases gluconeogenesis -Functional tumor will cause hypoglycemia |
|
|
Glucagon
|
-Produced in alpha cells in the endocrine pancreas islets of langerhans
-Maintains serum glucose levels, keeps glucose in the blood -Catabolic -Balances insulin -Increases glycogenolysis -increases lipolysis -Increases gluconeogenesis -Functional tumor will cause hyperglycemia |
|
|
Somatostatin
|
-General inhibitory function
|
|
|
Diabetes Mellitus
|
-relative or absolute insulin deficiency
--relative deficiency due to target cell receptor issue, insulin is present it just can't get into cells -Prevents target cell utilization of glucose, no glucose can get into the cells -May be due to lack of beta cells in the pancreas (no insulin production at all) |
|
|
Hyperfunction of the endocrine pancreas
|
-Most common cause is iatrogenic insulin overdose
--too much insulin leads to hypoglycemia -Can also be due to a functional tumor of islet cells |
|
|
Beta cell tumors
|
-Insulinoma, islet cell tumor
-Uncommon in dogs, rare in the cat -Common in ferrets -Usually small tumors and difficult to find --blends in with pancreatic parenchyma -In dogs are usually malignant, metastasize to regional lymph nodes and liver -In ferrets are usually benign -Does not occur in horses or cattle |
|
|
Beta cell tumor clinical signs
|
-Incoordination
-Ataxia -Weakness -Syncope -Muscle twitching -Blindness -Seizures -Polyphagia |
|
|
Diabetes mellitus
|
-Need Hyperglycemia and glucosuria for diagnosis
-Insulin is not produced by the beta cells OR cannot get into the target cells --issue with insulin production --issue with insulin receptor |
|
|
Type I Diabetes mellitus
|
-Genetic susceptibility
-Immunologic destruction of beta cells leading to insulin insufficiency --no insulin produced because cells are destroyed -Circulating antibodies against islet cell components come before hyperglycemia |
|
|
Type II Diabetes mellitus
|
-Insulin resistance and dysfunctional beta cells
--exhausted b-cells, lost target for insulin on cells -Genetic susceptibility with long lag phase before hyperglycemia -Exacerbated by environmental factors and obesity -In humans insulin is not usually used to control disease --diet, exercise, other glucose lowering drugs |
|
|
Diabetes mellitus in Animals
|
-Characterized as:
--Insulin-Dependent DM: requires insulin --Non-insulin dependent: does not require insulin -Familial history is rarely available for animals -Autoantibodies are not available -Clinical presentation is often not heloful -ALL DOGS and 50-75% of cats have insulin-dependent diabetes mellitus |
|
|
Clinical signs of Diabetes Mellitus
|
-Hyperglycemia and glycosureia
--tubular threshold for glucose resorption is exceeded -Osmotic diuresis, leads to PU/PD --can also lead to bacterial infections and cystitis -Polyphagia -Weight loss, cells are starving, causes fat and muscle catabolism -Increased lipolysis leading to ketoacidosis -Cataracts: glucose enters lens of the eye -Glomerulonephropathy and sclerosis -Fatty liver due to lack of insulin leading to breakdown of lipids and protein --increases lipids in hepatocytes |
|
|
Histologic changes occurring with Diabetes Mellitus
|
-Typically no histological changes in islets
-May see loss or decreases size of islets -Hydropic change of basal cells -Islet amyloidosis in cats --can also be incidental |
|
|
Tumors of the Paraganglia
|
-Tumors of chemoreceptors or baroreceptors
-Organs are sensitive to changes in pH, CO2, O2 --aid in regulation of circulation and respiration -Aortic body tumors: rare -Carotid body tumors |
|
|
Aortic body tumors
Chemodectoma |
-Heart Base tumor
-Rare -Most frequently occur in boxers and boston terriers --brachycephalic dogs -Has a space-occupying effect leading to compression of the atria, vena cava --results in dyspnea, ascites, hydrothorax, and hydropericardium (cardiac tympani) |
|
|
Carotid Body tumors
|
-Arise near the bifurcation of the common carotid artery in cervical area
-Rare tumors -Not functional but space-occupying |
|
|
Grave's disease
|
-Autoimmune disease
-Anti-Thyroid stimulating hormone antibody binds to TSH receptors on thyroid follicular cells -Stimulates secretion of thyroid hormone -Causes diffuse thyroid follicular hyperplasia |
|
|
Anopthalmos
|
-Developmental defect
-defective organogenesis -Complete absence of the eye or eyes -Very very rare |
|
|
Buphthalmos
|
-Enlargement and distention of the fibrous coats of the eye
|
|
|
Coloboma
|
-Apparent absence or defect of some ocular tissue
-Usually results from a failure of part of the fetal fissure to close -Most often seen as a notch-like defect of the caudal pole at the optic disc -Outpouching -Something did not fuse that should have -Can see the separation histologically |
|
|
Endophthalmitis
|
-Inflammation involving the ocular cavities and adjacent structures
--uvea, retina |
|
|
Exophalmos
|
-Abnormal protrusion of the eyeball
|
|
|
Glaucoma
|
-Group of diseases characterized by an increase in intraocular pressure
-Causes pathological changes in the eye |
|
|
Microphthalmos
|
-Congenitally small eye
-May be associated with other ocular defects |
|
|
Panophthalmitis
|
-Inflammation of all of the structures or tissues of the eye
--including the sclera |
|
|
Phthisis
|
-Shrinking, wastage, and hypotony of the eyeball
|
|
|
Synophthalmos
|
-Fused eye, 2 eyes are fused into 1
-Occurs with hellabore ingestion on day 14 of gestation |
|
|
Cystic eye
|
-Optic vesicle remains
|
|
|
Tissues in the eye derived from mesenchymal tissue
|
-Corneal stroma
-Corneal endothelium -Uveal stroma -Hyaloid artery system -Choroid -Orbital cartilage and bone -Sclera Tissues undergo a series of migrations, differentiations and atrophies during development of the mature eye |
|
|
Tissues in the eye derived from surface ectoderm
|
-Lens
-Corneal epithelium -Lacrimal apparatus -Epithelial portions of the eyelids and adnexae |
|
|
Tissues in the eye derived from Neuroectoderm
|
-Retina
-Optic nerve -Ciliary body -Posterior iris |
|
|
Mesenchymal defective differentiation in the Eye
|
-Issue with migration:
--choroidal hypoplasia --Iris hypoplasia -Incomplete atrophy of anterior or posterior chamber mesenchyme --Persistent pupillary membrane --anterior segment dysgenesis --Goniodysgenesys --Persistent hyaloid artery |
|
|
Persistent pupillary membrane
|
-Defect in mesenchymal differentiation of the eye
-Iris tissue/vascular tissue does not go away -membrane is attached to the cornea --turns blue and affects water flow across the lens -May block vision -Can lead to corneal or lens opacity |
|
|
Goniodysgenesis
|
-Defective mesenchymal development of the eye
-Maldevelopment of the filtration angle -No trabecular meshwork exists in filtration angle -Acts as a functional barrier to flow of aqueous humor in the eye -Can lead to glaucoma |
|
|
Choroid hypoplasia
|
-Defective mesenchymal differentiation
-Induction failure by defective retinal pigment epithelium -Key defect that results in Collie Eye --also includes colobomas and retinal separation |
|
|
Iris Hypoplasia
|
-Defective mesenchymal differentiation
-Rare defect -May occur alone or in conjunction with multiple defects -Most frequent in horses -May be inherited -Associated with cataract and conjunctival dermoids |
|
|
Anterior Segment dysgenesis of the Eye
|
-Mesenchymal defective differentiation
-Multiple anomalies of the cornea, lens, and anterior uvea |
|
|
Persistent hyaloid artery
|
-Mesenchymal defective differentiation in the eye
-May lead to focal cataracts |
|
|
Eyelid defective differentiation
|
-Surface ectoderm defective differentiation
-Abnormal palpebral opening -Entropion -Ectropion -Abnormal cilia -Imperforate puncta leading to excessive tearing -Coloboma |
|
|
Corneal defective differentiation
|
-May be ectodermal or mesenchymal defective differentiation
-Microcornea in an otherwise normal globe -Dermoid -Corneal opacities |
|
|
Dermoid
|
-Choristoma
-Ectodermal defective differentiation in the eye -Skin-like differentiation with epidermis and irregular dermis and adnexa -Haired skin on the eye -On the corneal or bulbar conjunctival surface |
|
|
Congenital Corneal opacities
|
-Usually caused by congenital anterior synechiae and persistent pupillary membranes
-Also caused by edema and non-cellular deposits |
|
|
Lens defective differentiation
|
-Ectodermal defective differentiation
-Aphakia -Microphakia -Lenticonus (misshapen lens) -ectopic lens (misplaced lens) -cataract |
|
|
Congenital Cataract
|
-Ectodermal defective differentiation
-Associated with other abnormalities or can be alone -Often due to persistence of mesoderm -Seen in horses and dogs -Sometimes hereditary, sometimes not -Unknown pathogenesis |
|
|
Defective differentiation of the neuroectoderm
|
-Retinal dysplasia
--usually occurs alone -Optic nerve hypoplasia --usually occurs with other diseases |
|
|
Retinal dysplasia
|
-Neuroectoderm defective differentiation
-Characterized by retinal folds, rosettes, blending/jumbling of retinal layers, loss of cells, glial proliferation -Seen most commonly in dogs and cattle -Caused by: --failure of proper apposition of the 2 layers of the optic cup --Failure of induction by RPE --necrosis or dysplasia of developing retina by viruses (BVDV, Bluetongue, CHV1, panleukopenia, FeLV) |
|
|
Signs of retinal dysplasia
|
-Neuroectoderm defective differentiation
-Retinal folds -Rosettes -Blending/jumbling of retinal layers -Loss of cells -Glial proliferation |
|
|
Optic Nerve hypoplasia
|
-Neuroectoderm defective differentiation
-Most common anomaly of the optic nerve -More likely to be atrophy due to destruction of ganglion cells -Toy dog breeds are most common |
|
|
Inflammatory and degenerative lesions of the eye
|
-Adnexa
-Conjunctiva -Cornea -Uvea -Lens -Retina -Optic nerve/sclera/orbit |
|
|
Adnexa
|
-Eyelids and associated glands
|
|
|
Inflammation of the eyelids
|
-Anything that affects the skin can affect the eyelids
-Skin diseases -Blepharitis (inflammation of the eyelid) -Hordeolum (suppurative adenitis/Stye) -Chalazion (Meibomian secretion) |
|
|
Hordeolum
|
-Stye
-Localized purulent inflammation of one or more Meibomian glands of the eyelids -External: occurs on cutaneous surface at the edge of the eyelid -internal: occurs on the conjunctival surface of the lid |
|
|
Blepharitis
|
-Inflammation of the eyelids
|
|
|
Chalazion
|
-Chronic granulomatous inflammation of an eyelid gland
-Meibomian gland inflammation -Meibomian gland can rupture and release sebum into the surrounding tissue -Will see macrophages in tissue |
|
|
Dacryoadenitis
|
-inflammation of the lacrimal glands
-Viral-related diseases --FIP, Canine Distemper, SDAV -Can be due to malignant catarrhal fever |
|
|
Prolapsed gland of the 3rd eyelid
Cherry eye |
-gland can be see protruding
-Often is excised, but not recommended --can contribute to keratoconjunctivitis sicca |
|
|
Cheomosis
|
-Edema of the eye conjunctiva
-Can be severe |
|
|
Distichiases
|
-Presence of a double row of eyelashes on an eyelid
-One or both of the eyelashes are turned against the eyeball -Can cause corneal irritation |
|
|
Ectropion
|
-Eversion of an edge or margin of the eyelid
-Results in exposure of palpebral conjunctiva --can predispose to infections |
|
|
Entropion
|
-Turning inward/inversion of an edge or margin of the eyelid
-Piece of the eyelid is turned in towards the eyeball -Can result in corneal irritation |
|
|
Conjunctivitis
|
-Inflammation of the conjunctiva
-Can be acute or chronic --Acute: may be due to any noxious stimulus (physical, chemical, allergy, microbial) -infectious causes --Chronic: usually due to persistent noxious stimulus --upper respiratory infections --herpesvirus --oncocerca parasite -Immune-mediated causes --allergies |
|
|
Immune-mediated Conjunctivitis
|
-Allergy: affects all species and most often dogs
-Eosinophilic conjunctivits -Ligneous conjunctivitis (linked to plasminogen deficiency) -Feline lipogranulomatous conjunctivitis |
|
|
Descemetocele
|
-Herniation of Descemet's membrane
-Usually herinates outward through the corneal stroma and epithelium -May have melanosis --inundates chronically afected eye |
|
|
Keratitis
|
-inflammation of the cornea
-Inflammatory cells and other components of inflammation arrive through tears or aqueous --no blood vessels, have to come in with tears -Specific types of keratitis for each species |
|
|
Keratoconjunctivitis
|
-Inflammation of the cornea and conjunctiva
|
|
|
Keratoconjunctivitis sicca
|
-inflammation of the cornea and conjunctiva
-Associated with or due to drying of the conjunctiva -Usually there is decreased tear production or tears are unable to reach important structures |
|
|
Pannus
|
-Superficial vascularization of the cornea
-Will have infiltration of granulation tissue |
|
|
Cornea Anatomy
|
-Intact cornea is necessary to transmit light and protect deeper eye structures in the globe
-Injury may lead to corneal opacity and loss of clarity -Epithelium: non-keratinized and non-pigmented --orderly differentiation -Stroma: orderly with few cells --periodicity of stromal collagen is similar to the wavelength of visible light --No vessels -Descemet's membrane: thick basement membrane -Endothelium: pumps out fluids, keeps cornea dehydrated --Na/K dependent ATPase pump keeps dehydrated |
|
|
Abnormal corneal epithelium
|
-Keratinized and pigmented
-Thickened -Disorganized -Opaque |
|
|
Abonrmal stromal collagen
|
-Disorganized
-Thickened -May be scarred -May have vascularized keratinocytes -Increased inflammation -Melanin, iron, and Ca pigments |
|
|
What can go wrong with the Cornea
|
-Edema: fluid in stroma will increase thickness
-Erosion: erodes epithelium -Ulcer: damage beyond the epithelium --will have neovascularization and granulation tissue formation --Cornea will become keratinized and pigmented |
|
|
Pathology of Corneal Rupture
|
-Stimulus → erosion or loss of epithelium → edema → inflammation → ulcer (scar) → neovascularization (scar) , granulation tissue, fibroplasia → deep corneal stromal ulcer (scar) → desmetocele that extends to decemet's membrane, causes outward pressure → corneal rupture
|
|
|
Causes of Corneal Injury and Opacity
|
-Chemicals: caustics, NH3, medications
-Physical: cold, heat, penetrating objects -Microbial: bacteria, viruses, fungi -Immunologic: type III hypersensitivity -Glaucoma: increased intraocular pressure -Lysosomal storage diseases |
|
|
Corneal edema
|
-Reaction to cornea injury
-Cornea becomes thickened and opaque due to increased stromal fluid -Fluid is from damaged endothelium or from tears that go through damaged epithelium |
|
|
Corneal erosions and ulcers
|
-Loss of epithelium
-Ulcers can result in secondary bacterial infections --pseudomonas, strep |
|
|
Corneal Endothelial Dystrophy
|
-Common in boston terriers, Chihuahuas, Dachshunds, and others
-Causes progressive bilateral corneal edema -Lack of normal vasularization leads to edema -Feline sequestrum -Canine persistent ulcer syndrome |
|
|
Corneal Deposits
|
-Can be congenital or acquired
-Pigment: melanin, iron, Ca --usually occurs secondary to injury -Lipidosis: cholesterol, lipid, macrophages --primary or secondary to hypercholesterolemia or corneal injury |
|
|
Corneal Degeneration
|
-Corneal lesions characterized by non-inflammatory loss of epithelial or stromal cells
|
|
|
Feline Corneal sequestrum
|
-Discrete orange brown discoloration of the central cornea
-Common in persian or himalayan cats -Necrosis of stromal cells -Sequestrum will eventually slough and heal by granulation tissue -May be an uncommon result of corneal ulceration in cats |
|
|
Canine persistent ulcer syndrome
|
-Recurring ulcers
-Shallow central corneal erosion -Lesion does not heal, repeatedly re-ulcerates -Epithelial cells are unable to anchor |
|
|
German Shepard Keratitis
|
-Pannus keratitis
-Idiopathic lesions -Stromal mononuclear infiltrate |
|
|
Canine Keratitis
|
-Keratoconjunctivitis sicca
-Consequence of inadequate tear film -Chronic, progressive inflammation -Idiopathic |
|
|
Feline Herpes Keratitis
|
-Herpes keratitis due to FHV1
-Causes latent infection in adults -Often unilateral -May not have associated respiratory signs -Ulcers and stromal keratitis |
|
|
Feline Eosinophilic Keratitis
|
-Proliferative, "fluffy" white lesion
-Mix of macrophages, fibroblasts, and eosinophils |
|
|
Equine keratitis
|
-Mycotic keratitis
-Destructive, suppurative, deep stromal inflammation -Aspegillus is the most common pathogen |
|
|
Cattle Keratitis
|
-infectious bovine keratoconjunctivitis
-"Pink eye" -Caused by Moraxella bovis -May have concurrent infections -Shallow central ulcer -Abscess and malacia also present |
|
|
Sheep and goat keratitis
|
-Infectious keratoconjunctivits
-Contagious opthalmia -Mycoplasms and Chlamydophila psittaci may be important agents |
|
|
Corneal injury pathogenesis
|
-Noxious stimulus → Erosion/loss of epithelium or endothelium
-Can be repaired and return to normal -Can also lead to edema, which then repairs and returns to normal -Edema → inflammation → Ulcer → Neovascularization → Scar and vascular "ghosts" → desmetocele, phthisis bulbi → corneal rupture -Repair can occur at any stage -End result of injury depends on severity and chronicity of injury AND ability of the cornea to respond -Some stages of repair can still end up with scarring |
|
|
Aphakia
|
-Absence of the lens
-Can be congenital or acquired -Lens is just missing! |
|
|
Cataract
|
-Opacity of the crystalline lens
-Can be due to age -Can be secondary to intraocular disease --uveitis, tumors, glaucoma, retinal degeneration, trauma, metabolic disease -Occurs in diabetic dogs -May be hereditary in dogs and horses |
|
|
Lenticonus
|
-Conical protrusion of the substance of the crystalline lens
|
|
|
Microphakia
|
-Abnormally small crystalline lens
|
|
|
Nuclear Sclerosis
|
-Age related compression o the lens fibers
-Causes central lens opacity or tranlucency |
|
|
Chorioretinitis
|
-Inflammation of the choroid and retina
|
|
|
Severe chronic keratitis
|
-Dry eye
-Diffuse uptake of fluorescein stain |
|
|
Ulcerative keratitis Histology
|
-Epithelial layer is destroyed, complete perforation of the cornea
-Will have fibroblast proliferation -Infiltration of inflammatory cells |
|
|
Uveitis
|
-Common in most domestic animals
-Anterior uveitis: iris, ciliary body, usually anterior and posterior chambers are involved -Posterior uveitis: ciliary body, choroid, and usually retina are involved -Panuveitis: alll structures inside the sclera are involved --diffuse uveitis |
|
|
Classifications of Uveitis
|
-Serous: protein-rich fluid produces "aqueous flare" (mild)
-Suppurative: usually bacterial, hypopyon -Granulomatous: fungal, algae, helminths, mycobacteria, lens rupture, idiopathic, lymphoplasmacytic --most common form of uveitis in cats --can be due to FIP |
|
|
Canine "Blue Eye"
|
-Caused by Canine Adenovirus
-Can be due to a modified live vaccine -Diffuse corneal edema -Convalescent phase or post-cavvine -Animal develops uveitis and corneal edema (blue eue) |
|
|
Choroiditis
|
-Inflammation of the choroid
|
|
|
Hypopyon
|
-Accumulation of neutrophils (pus) in the anterior chamber
|
|
|
Iritis
|
Inflammation of the iris
|
|
|
Iridocyclitis
|
-Inflammation of the iris and ciliary body
|
|
|
Synechia
|
-Adhesion of parts
-Adhesion of the iris to other structures -Anterior synechia: adhesion of the iris to the cornea -Posterior synechia: adhesion of the iris to the capusle of the lens --rarely adhesion of the iris to the vitreous body |
|
|
Infectious Causes of Uveitis
|
-Bacterial infection:
--Bartonella in cats --can be heatogenous or from penetrating wounds -Fungal infection: Secondary to mycotic keratitis or part of systemic disease -Protozoal infection: Toxoplasma gondii -Parasitic larval migrans: toxocara canis, Dirofilariasis, onchocerca |
|
|
Idiopathic causes of Uveitis
|
-Feline lymphoplasmacytic uveitis
-Unknown etiology -Possibly due to toxoplasma and bartonella? |
|
|
Immune-mediated uveitis
|
-Lens induced uveitis
--Phacolytic: lymphocytic uveitis associate with cataracts --Phacoclastic: occurs 10-14 days after lens rupture -Canine Adenovirus -Equine recurrent uveitis |
|
|
Equine recurrent uveitis
|
-Periodic ophthalmia
-result of hypersensitivity to exogenous antigen -Leptospir -Onchocerca |
|
|
Canine Uveodermatologic Syndrome
|
-AKA Vogt-Koyanagi-Harada (VKH) syndrome
-Akitas are predisposed -Autoimmune disease -targets melanin or component protein expressed in melanocytes -Bilateral granulomatous uveitis |
|
|
Sequelae of Uveitis
|
-Depends on location, severity, and duration of inflammation
-Corneal opacities due to edema, keratosis/fibrosis, inflammation -Anterior and posterio synechia (adhesions) -Glaucoma -Retinal separation or degeneration -Cataracts -Pre-iridal fibrovascular membranes --Formation of granulation tissue --leads to intraocular hemorrhage --Can also be caused by retinal separation and ciliary body tumors -Phthisis bulbi |
|
|
Phthisis bulbi
|
-"End stage eye"
-Hypotonic, shrunken, disorganized eye -Eye is shriveled up and fibrotic |
|
|
Iris atrophy
|
-Degenerative lesions of the uvea
-Age-related change -Occurs in several species -Progressive thinning of the iris stroma that creates "holes" in the iris -Looks like congenital iris hypoplaisa and colobomas |
|
|
Irido-ciliary cysts
|
-Degenerative lesion of the uvea
-Occur commonly in dogs -May or may not be clinically significant |
|
|
Lens
|
-Avascular crystalline structure with no nuclei present
-Composed of a capsule, epithelium, and lens fibers -Changes in lens position can lead to secondary issues -Most common lesion is opacity (Cataracts) |
|
|
Diseases of the Lens
|
-Cataract
-Nuclear sclerosis -Positional change -Phakitis |
|
|
lens Clarity
|
-Determined by the anatomy and physiology of the lens
-Lens is avascular, gets nutrition from aqueous -35% of the lens is soluble crystalline protein -Very few (if any) nuclei -Very few mitochondria --undergoes anaerobic glycolysis |
|
|
Histologic Changes associated with Cataracts
|
-Morgagnian globules
--denatured lens proteins -Bladder cells: large cells, result of aborted efforts at new fiber formation -Fiber degeneration and fragmentation -Lens epithelial hyperplasia or metaplasia -Posterior migration of the lens epithelium -Mineralization of the lens |
|
|
Diabetic Cataract
|
-90% of spontaneously diabetic dogs develop cataracts
-Bilateral condition -Begins in the cortex at the equator of the lens -Progresses rapidly over a few weeks |
|
|
Pathogenesis of Diabetic Cataracts
|
-Glucose is major energy source for lens fibers
--via Embden-Meyerhof pathway of anaerobic glycolysis --Hexokinase is rate limiting enzyme -With hyperglycemia, hexokinase is saturated and glucose is shunted to other pathways -Primary alternative is Sorbitol pathway --occurs when glucose is higher than 90mg/dl -Sorbitol accumulates and osmotically attracts water -Leads to hydropic degeneration and rupture of lens fibers --opacification of lens |
|
|
Nuclear Sclerosis of the Lens
|
-Age-related compression of the lens fibers
-New fiber formation leads to compression -Does not affect vision |
|
|
Positional changes of the Lens
|
-Ectopic lens
-Subluxation/luxation --anterior or posterior movement --Due to zonule rupture -Configuration: usually congenital |
|
|
Phakitis
|
-Inflammation of the lens
-Can accompany endophthalmitis/panophthalmitis -Lens proteins are antigenic |
|
|
Papilledema
|
-Hydropic swelling of the optic disc
-Caused by increased CSF pressure, inflammation, decreased intraocular pressure |
|
|
retinitis
|
-Inflammation of the retina
-Usually involves choroid also -Rare on own, usually occurs with other lesions -May occur with neurotropic viral infections -Can occur with RMSF and Ehrlichia canis |
|
|
Scleral Extasia
|
-Bulging of the sclera, usually through a defect (coloboma)
|
|
|
Staphyloma
|
-Protrusion of the sclera (posterior) or cornea (anterior)
-Protrusion is lined with uveal tissue -Results from inflammation |
|
|
Retinal Separation
|
-Separates between photoreceptors and pigmented epithelium
-Ora ciliaris and optic disc remain attached -Can be artifactual with processing or fixation -True separation will have hypertrophy of the RPE and protein accumulation in the subretinal space --can see on histology -Causes: --trauma --inflammatory exudates and transudates --Neoplastic cells --Parasites --Contraction of cyclitis membrane |
|
|
Retinal Degeneration
|
-Atrophy
-Loss of layers of retina, decreased thickness of layers -All except glaucoma begin in the outer layer and progress inwards -Starts with photoreceptors → outer nucelar layer → inner nuclear layer → ganglion cell -Older lesions look similar to each other --end result is a glial scar that is poorly cellular -Can be inheritied condition |
|
|
Progressive Retinal Atrophy
|
-Inherited retinal degeneration
-Large group of bilateral retinal diseases in dogs -Affects more than 100 breeds -Most are autosomal recessive -Progresses to blindness unassociated with inflammation -Ultrastructural and biochemical changes vary between breeds -Age of onset and speed of progression differ between breeds -Common in Irish setters, Norwegian Elkhounds, Collies, and mini poodles |
|
|
Nutritional cause of Retinal degeneration
|
-Vitamin C
-Vitamin A -Vitamin E -Taurine in cats |
|
|
Causes of retinal degeneration
|
-Inherited disorders
-Senile changes, old age -Nutritional deficiencies -Toxic retinopathies -INjury/trauma -Diabetes mellitus -Hypersensitive retinopathy -Storage diseases |
|
|
Optic Neuritis
|
-inflammation of the optic nerve
-Caused by: --spread of meningitis or meningoencephalitis --Spread of endophthalmitis --Primary viral cause (FIP, Canine distemper) --Chorionic gliosis, astrocytosis, or axonal degeneration |
|
|
Issues with the Sclera and Orbit
|
-Nodular Granulomaatous scleritis (dogs)
--nodular proloferative inflammatory lesions of the sclera --behaves like a locally infiltrative neoplasm -Orbital cellulitis: extension of inflammation from adjacent non-ocular tissues and foreign bodies -Retrobulbar abscesses: tooth root abscesses, foreign bodies -Orbital myositis: Occurs in dogs, Ab against type IIM Muscle fibers |
|
|
Glaucoma
|
-Diverse group of pressure-dependant neurodegenerative disorders
-All result in loss of normal function of retinal ganglion cells and axons in the optic nerve -Ultimately degeneration leads to loss of vision -Most consistently recognized feature is elevation in intraoular pressure -Occurs in dogs more often than cats, more often than horses, least often in ruminants |
|
|
Key mechanism for Increase in intraocular pressure
|
-Reduction in capacity for aqueous outflow
-increase in episcleral venous pressure --from orbital space-occupying lesions |
|
|
Primary Glaucoma
|
-No other ocular disease
-Goniodysgenesis -Maturity or middle age -Malformation or malfunction of the filtration angle apparatus --can be isolated event or part of mesenchymal dysgenesis |
|
|
Secondary Glaucoma
|
-Increase in Intra-ocular pressure due to other ocular disease
-Uveitis -Synechiae -Pre-iridal fibrovascular membrane -Lens luxation -Intraocular hemorrhage |
|
|
Sequelae of Glaucoma
|
-Depends on duration and severity
-Buphthalmia -Scleral thinning -Corneal edema -Corneal striae, breaks id Descemet's membrane -Exposure keratitis secondary to buphthalmos -Lens luxation or subluxation due to zonule damage -Cataract -Atrophy of iris and ciliary body -Retinal Atrophy -Retinal separation -Optic disc cupping |
|
|
Squamous cell Carcinoma of the Eyelid
|
-Occurs in cows most often → horses → feline → dogs
-Occurs most often in limbus, then 3rd eyelid, then eyelid -UV light causes epidermal plaque formation → papilloma → carcinoma in-situ -Carcinoma can be invasive and metastasize |
|
|
Neoplasia of the Eyelid and Conjunctiva
|
-Squamous cell carcinoma
-Meibomian gland neoplasms -Melanocytoma -Hemangioma/Hemangiosarcoma -Mast cell tumors -Adenocarcionma of the 3rd eyelid -Lymphoma -Papillomas |
|
|
Meibomian gland Neoplasms
|
-Adenomas are very common in dogs
--70% of eyelid tumors -Carcinomas are rare |
|
|
Eyelid/Conjunctival Melanocytoma
|
-Common in dogs
|
|
|
Eyelid/Conjunctival Hemangioma/Hemangiosarcoma
|
-Occurs in dogs, cats, and horses
-May also be related to UV light |
|
|
Melanocytoma/ Malignant melanoma Intraocular neoplasms in the Dog
|
-prognosis based on histological criteria
--Anaplasia, mitoses, invasion -Occurs on the iris --90% are benign -Choroid: rare and usually benign |
|
|
Melanocytoma/Malignant Melanoma Intraocular neoplasm in the Cat
|
-Diffuse iris melanoma is more common than solitary masses
-May obstruct filtration angle and cause glaucoma -Long-term neoplasms have greater risk for distant metastasis |
|
|
Iridociliary adenomas and carcinomas
|
-Most common primary tumors of the eye after melanomas
|
|
|
Feline post-traumatic sarcomas
|
-Arise from metaplasia of lens epithelium after injury
-Very aggressive neoplasia -REMOVE NEOPLASTIC EYE! --any sarcoma will go right back to the brain if it metastasizes |
|
|
Metastatic Neoplasia to the Eye
|
-Lymphoma (most common)
-Pulmonary carcinomas (rare in cats) -Almost all other neoplasms are possible to metastasize to the eye |
|
|
Medulloepitheliomas
|
-Very rare
|
|
|
Orbital Neoplasms
|
-Optic nerve meningioma
-Sarcomas -Carcinomas (lacrimal adenocarcinoma) |
|
|
REasons for bringing a pet to the vet
|
1. Ear infection
2. Skin allergy 3. Upset stomach 4. Benign tumors 5. Bladder infection 6. Skin infection LOTS of skin reasons! |
|
|
Skin function
|
1. Barrier function (enclosing, microbial, thermal, chemical, photoprotection, immunoregulation)
2. Sensory perception (touch, heat, pain, cold) 3. Storage (electrolytes, fat, protein) 4. Temperature regulation 5. Vitamin D synthesis 6. Indicator of general health and internal disease |
|
|
Vitamin D synthesis in the Skin
|
Sunlight hits the epidermis, converts provitamin D3 (7-dehydrocholesterol) to Vitamin D3 (Cholecalciferol)
-Vitamin D3 is hydroxylated in liver → 25-hydroxy D3 and in kidneys to active form of 1,25- Vitamin D3 -Redulates epidermal differentiation and proliferation -Important for Ca absorption from the gut |
|
|
Structural components of the Skin
|
-Epidermis
-basement Membrane -Dermis -Adnexal structures --Hair follicles, apocrine glands, exocrine glands, sebaceous glands, errector pili muscles -Subcutis/hypodermis --does not exist in all areas |
|
|
Skin as an enclosing barrier
|
-TIGHTLY regulates water within the body
-Keeps water in and pathogens out -Number one goal is to prevent water loss -Prevents loss of elecctrolytes -Prevent loss of cells -Protect the animal from environmental insults --microbial --thermal -chemical |
|
|
Epidermis Composition
|
-Keratinized stratified squamous epithelium
-85% keratinocytes -3-8% Langerhan's cells -5% melanocytes (always in basal layer -2% Merkel cells |
|
|
Epidermal thickness
|
-Depends on species
-Thickness depends on contact with the environment --thin epidermis on abdomen --thick epidermis on footpads |
|
|
Skin Adnexal Structures
|
-Hair follicles
-Apocrine glands --epitrichial, near the hair follicle -Eccrine glands --atrichial, on foot pads) -Sebaceous glands -Arrector pili msucles |
|
|
Species differences in Epidermis
|
1. Dog: melanin in basal layer
-thin skin 2. Pig: pegs anchor dermis into the epidermis 3. Young human: thick skin 4. Old human: thin skin |
|
|
Keratinocyte function
|
-Structural support
-Contribute to skin immune system --produce cytokines --can produce inflammatory mediators with stimulation --Amplify contact hypersensitivity reactions -Undergoes differentiation and cornification to allow for barrier function |
|
|
Cornification
|
-Formation of stratum corneum
-Modified form of programmed cell death, modified apoptosis -Keratinocytes undergo dramatic change in shape, size, and function --Lose all cytoplasmic organelles -Move from basal layer to the stratum corneum -Results in development of a thick cornified envelope, replacement of cell plasma membrane |
|
|
Stratum basale
|
-basal cell layer in the epidermis
-Progenitor cell layer -Slow-cycling stem cells -Transiently amplifying cells -terminally differentiated cells -Hemidesmosomes anchor basal keratinocytes to the dermis --Essential function! -Contains melanocytes |
|
|
Stratum Spinosum
|
-"Sponge" or "Prickle cell layer"
-Keratinocytes become larger, flatten out horizontally -Desmosomes are prominent and attach cells to each other -May contain Langerhans cells -If edematous, can visualize desmosomes |
|
|
Stratum Granulosum
|
-Granular Cell lyaer
-Layer of flattened keratinocytes -Keratohyalin granules present in the cytoplasm of keratinocytes (basophilic) -Profilaggrin undergoes proteolysis to form filaggrin --"Filament aggregating Protein" --Aggregates keratin filaments -Layer is present in some domestic animals and not others |
|
|
Stratum Corneum
|
-Horny or cornified layer
-Fully keratinized, anucleate, dead cells -More than 20 layers thick --85% protein, 15% lipid --Keratin acts as "bricks" and lipid acts as "mortar" -Restricts water movement, reduces water loss -Prevents pathogen and allergen entry -decreases exposure to topical drugs and irritants -Absorbs UV light to protect from free radical oxidation -Continuously shed |
|
|
Structural support of the Epidermis
|
-Keratin intermediate filaments
--10-25 um --Provide structural integrity -Intermediate filaments can be used for diagnostic purposes |
|
|
Process of Cornification
|
1. Lipid Formation
2. Dissolution of the Nucleus and Organelles -release of proteases, DNAse, RNAse 3. Formation of the Protein Core -Aggregation of keratin filaments 4. Formation of the cornified envelope -replace plasma membrane with a protein barrier 5. Desquamation Dramatic change in size, shape, and function of cells -70% of water islost |
|
|
Keratinocytes and Inflammation
|
-Keratinocytes produce cytokines
--constitutive production --can be activated by microbial toxins, trauma, or hypoxia --can cause systemic effects -Produce other inflammatory mediators --neuropeptides, free radicals, prostaglandins, growth factors -Imoportant for drug metabolism |
|
|
Abnormalities in Cornification process
|
-Leads to hyperkeratisis, clinical scaling, and decreased barrier function
|
|
|
Cornification Process
Lipid Formation |
-Lamellar bodies are formed in stratum spinosum
--Fuse with cell membrane and expel lipid contents into the intracellular space --at junction of SG and SC layer -Enzymes modify lipid, make it more hydrophobic -Lipid acts like glue, adheres corneocytes to each other --Provide moisture and act as hydrophobic barrier -"Juice packets" burst at the junction into intracellular space |
|
|
Enzymes in skin that change lipids
|
-In granular cell layer:
--Glycosphingolipids --Phospholipids --Hydrolases -In cornified layer: --ceramides --Cholesterol --fatty acids |
|
|
Cornification Process
Release of Nucleus and Organelles |
-Proteases, DNAse and RNAse
-Orthokeratisis: normal dissolution, nuclei are cleaved -Parakeratosis: abnormal dissolution, nuclei are retained --occurs with increased turnover of the stratum corneum from minor trauma |
|
|
Parakeratosis
|
-Abnormal dissolution of cell organelles and nucleus during cornification process
-Occurs due to increased turnover of the stratum corneum -Will have retained nuclei --histologically can see blue nuclei in pink stratum corneum |
|
|
Cornification Process
Formation of the Protein Core |
-Aggregation of Intermediate filaments
--Keratin fibrils -Profilaggrin → filaggrin → Packing of keratin fibers to form a thick protein core --Cross linking keratin filaments --Can also break down keratin to form AA |
|
|
Cornification Process
Formation of the cornified envelope |
-Surrounds protein core
-Transglutaminases cross-link small proteins --involucrin, loricrin -Small proteins form tough protein shell that replaces cell membrane |
|
|
Cornification Process
Desquamination |
-Enzymes cleave desmosomes
-pH dependent -Layers of corneocytes are sandwiched between layers of lipid -Desmosomes are actively broken down and keratin squames are shed into the environment |
|
|
Hyperkeratosis
|
-Abnormality of the cornification process
-Primary= mutation in one of the enzymes involved in cornification --Can be lamellar bodies, transglutaminase, or keratin intermediate filaments -Secondary: occurs due to any insult --allergic disease, endocrine disorder, parasitic and bacterial infections |
|
|
Ichthyoses
|
-Heterogenous group of diseases that are all characterized by faulty cornification that results in scaling
-Usually congenital and heritable disorders -Harlequin ichthyosis: defective lamellar bodies, no lipid in stratum corneum -Lamellar Ichthyosis: mutation in transglutaminase gene -keratin 10 mutation: keratin proteins are not made appropriately -Ichthyosis vulgaris: Abnormal filaggrin expression |
|
|
Langerhans Cells
|
-Skin Immune system function
-Potent antigen processing cells, dendritic cells -Bone-marrow derived -Sense environment between cells -When activated leave epidermis and enter lymphatic vessels --travel to local lymph nodes to interact with T-cells -May be increased with some hypersensitivity disorders --cause contact hypersensitivity -May be decreased after UV exposure |
|
|
Histiocytoma
|
-Neoplasia derived from langerhan's cells
-Benign tumors, regress on own |
|
|
Melanocytes
|
-In basal cell layer of the epidermis and hair follicles
-Produce melanin -Transfer pigment via melanosomes to keratinocytes --Transfer pigment to other cells -One melanocyte per 10-20 keratinocytes -Provide hyperpigmentation after injury --Re-pigmentation is slower than keratinocyte epithelialization, scars are usually hypopigmented |
|
|
Melanin
|
-Produced by melanocytes in the skin and distributed to keratinocytes
-Provides cosmetic pigmentation -Acts as UV radiation barrier --absorb UVR and scavenge free radicals from UV light -Scavenge free radicals |
|
|
Skin disorders due to abnormal melanization
|
-Post-inflammatory hyperpigmentation
-Color dilution alopecia --black hair follicular dysplasia --melanocytes do not transfer melanin properly to hair -Vitiligo -Melanoma |
|
|
Merkel Cells
|
-Mechanoreceptors in the skin
-have features of epithelial and neuroendocrine cells -Located in the basal layer of tylotrich pads and hair follicles |
|
|
Basement membrane Zone
|
-Anchors epidermis to the dermis
-Provides protective barrier -Complex system that keeps epidermis bound to the dermis -Important in wound healing, nutritional transport, maintaining a functional epidermis -Site of many pathological processes -Ulcerative wounds that penetrate below the basement membrane are more likely to heal with scarring |
|
|
Components of the Basement Membrane
|
-Hemidesmosomes: intermediate filaments connect to nuclear membrane of cels
--provide structural rigidity --have inner and outer plaques -Lamina lucida: clear zone -Lamina densa: type IV collagen -Sublamina densa: anchoring fibrils, type VII collagen |
|
|
Desmosome vs. Hemidesmosome
|
-Desmosomes attach cells to each other
-Hemidesmosomes attach cells to basement membrane |
|
|
Autoantibodies to basement membrane components
|
-Prevent epidermis from being anchored
-Congenital and acquired blistering disorders -Hair can act as an anchor in some areas |
|
|
Epidermolysis Bullosa Acquista
|
-Acquired antibody to component of collagen in basement membrane
|
|
|
Dermis
|
-Provides elasticity and tensile strength to protect skin against injury
-Acts as a scaffold for vessels and nerves -Composed of collagen, elastin, proteoglycans (glucosaminoglycans) --collagen and elastin produced by fibroblasts -Divided into superficial and deep layers -Also has mast cells, dermal dendritic cells, and lymphocytes |
|
|
Abnormal Collagen in Dermis
|
-Defects in formation can lead to collagen that lacks tensile strength and leads to tearing of skin
-Dietary deficiency in Vitamin C (ascorbic Acid) results in Scurvy --also get hemorrhages, collagen lines blood vessels |
|
|
Abnormal Elastin in dermis
|
-Prolonged solar exposure causes permanent damage to elastin fibers
--"Solar elastosis" |
|
|
Ehlers-Danlos Syndrome
|
-VERY stretchy skin due to deficient collagen in dermis
-Occurs in Labs -Skin can tear, and suture will not really fix it |
|
|
Abnormal Ground Substance in Dermis
|
-Mucin deposition/hyaluronic acid in the dermis leads to wrinkles
--"tragic face" with hypothyroidism -When too much mucin is deposited, can have cutaneous mucinosis |
|
|
Hair follicles
|
-Act as physical and photoprotective barrier
-Provide visual stimulus for sexual attraction -Aid with thermoregulation -Role in sensory perception -Important for wound healing, hair follicle supplies germ cells to heal wound |
|
|
Structure of hair
|
-"Tube in a tube"
-Outer root sheath is continuous with the epidermis -Outer root sheath surrounds inner root sheath -Combined, root sheaths surround the hair shaft -Hair bulb at the base of the follicle contains papilla that is part of the dermis |
|
|
Simple Hair Follicle
|
-Found in humans, horses, cattle, rats, mice
|
|
|
Compound hair follicle
|
-Found in dogs, cats
-Composed of few large hairs --primary/guard hairs -Large hairs are surrounded by many smaller hairs --secondary undercoat hairs -In sheep secondary follicles have secondary follicles, compound compound follicles |
|
|
Anatomical regions of the Hair follicle
|
1. Infundibulum: extends from the opening of the follicle to the insertion of the sebaceous gland duct
2. isthmus: area between the sebaceous gland duct and insertion of the arrector pili muscle 3. Inferior portion: below the arrector pili muscle, contains the bulb of the actively growing hair -Inflammatory conditions may target specific regions |
|
|
Hair Cycle
|
-Hair grows in cycles, not continuously
-Affected by photoperiod, temperature, hormones, nutrition, genetics -Hair replacement in dogs and cats occurs as a mosaic pattern --neighboring hair follicles are in different stages of the hair cycle |
|
|
Stages of the Hair cycle
|
1. Anagen: state of growing hair
2. Catagen: transitional stage 3. Telogen: resting stage, no growth |
|
|
Sinus hairs
|
-Vibrissae, whiskers
-Slow-adapting mechanoreceptors |
|
|
Tylotrich hairs
|
-Rapid adapting mechanoreceptors in normal body hair
-Scattered among normal hairs -Merkel cells in tylotrich pads |
|
|
Folliculitis
|
-Inflammation of the hair follicle
-Caused by bacteria, demodex mites, or dematophytes (ringworm fungi) -Results in patchy hair loss |
|
|
3 causes of Folliculitis
|
1. Bacteria (staph)
2. Demodex mites 3. Dermatophytes (ringworm fungi) |
|
|
Furunculosis
|
-Follicular rupture
-Hair is released into dermis -Body has foreign body reaction to released hair |
|
|
Disorders affecting hair follicles
|
-Folliculitis
-Furunculosis -Hair follicle dysplasia -Hair cycling disorders -Atrophy/miniaturization |
|
|
Hormonal influence on Hair cycle
|
-Hormones that stimulate anagen
--thyroid hormones --Androgens -Hormones that inhibit anagen --glucocorticoids --Estrogen |
|
|
Sebaceous glands
|
-Holocrine glands: open into the hair follicle
-Sebocytes degenerate to form sebum --makes skin water repellent -Give luster to haircoat -Help maintain normal flora --bacteriostatic and funcistatic -Pheremone production -Provide for markings and sexual attraction |
|
|
Sebaceous gland inflammation
|
-Sebaceous adenitis
-Hair follicles are annealed at the base -Will have silvery scales on the bridge of the nose -Hair follicles are cemented together, come out of skin together -Without sebaceous glands, animal will not have lubricant for hair, leads to hyperkeratisis -Animal is prone to secondary bacterial infections -Scaly dog with hair loss and infections |
|
|
Sweat Glands
|
1. Apocrine: epitrichial
-Empty into the hair follicle -Produce odorless milky fluid composed of proteins and lipids 2. Eccrine glands: atrichial -Present only in the footpads of carnivores -Not associated with a hair follicle -Ducts empty directly onto the surface of the skin |
|
|
Subcutis/Hypodermis
|
-Between the dermis and skeletal muscle below
-COmposed of adipose tissue and loose connective tissue --Panniculus= adipose tissue -Metabolic storage pool, protects deeper structures |
|
|
Cutaneous Vasculature
|
-No direct blood flow
-Have 3 inter-communicating plexuses --Superficial plexus --Middle plexus --Deep plexus |
|
|
Elevated Skin Lesions
|
-Papule
-Plaque -Pustule -Crust -Eschar -Scale -Vesicle -Bulla -Wheal |
|
|
Papule
|
-Elevated bump
-Less than 1.0cm -Can be follicular or non-follicular -Small, solid, red/white, and raised |
|
|
Plaque
|
-"Big papule"
-Solid, slightly raised lesion -More than 1.0cm |
|
|
Pustule
|
-Small circumscribed elevation that is filled with pus
-Has fluid in it -Rupture will lead to crust formation |
|
|
Crust
|
-Aggregate of inspissated serous debris
-May or may not have WBCs, RBCs, or bacteria -Superficial pyoderma |
|
|
Scale
|
-Flat plate of stratum corneum
|
|
|
Eschar
|
-Crust that forms in association with an ulcer
-Tightly adherent to the skin --incorporates dermal collagen --Scab sticks to underlying dermis |
|
|
Bulla
|
-Large vesicle, 1.0cm or larger
-Fluid-filled, translucent elevation -"Clear blister" |
|
|
Vesicle
|
-Fluid-filled, translucent elevation that is less than 1.0cm
-Small bulla |
|
|
Wheal
|
-Firm, circumscribed, raised elevation in the skin
-Composed of edema -Often erythematous -"Mesa," flat-topped lesions caused by edema |
|
|
Planes
|
-Lesions level with the skin surface
-Macule: less than 1.0cm --color differs from that of the surrounding normal skin -Patch: same as a macule, but more than 1.0cm -Flat, deep, bright, hemorrhage, erythema |
|
|
Erosion
|
-Depression in the skin surface
-Loss of all or part of the epidermis -Does not go past the basement membrane |
|
|
Ulcer
|
-Depression below the skin surface
-Loss of the entire epidermis and at least some of the dermis -DEEP lesion |
|
|
Comedone
|
-Keratin-filled dilated hair follicle infundibulum
-Also contains sebaceous material with or without microorganisms -"Blackhead" -Follicular plugging |
|
|
Alopecia
|
-Gross term for hair loss
|
|
|
Lichenification of Epidermis
|
-Thickening of the skin
-Associated with accentuation of the normal skin markings -Results from a chronic friction or inflammation --chronic surface trauma -Can get hyperpigmentation |
|
|
Epidermal collarette
|
-Special type of scale
-Arranged in a circular pattern, usually caused by the roof of a pustule or papule -Ruptured pustule with rim of scale left --Hyperpigmentation in the center -Usually a sign of bacterial infection |
|
|
Follicular Casts
|
-Accumulation of keratin that thightly adheres to hair shafts
-Hairs in the follicle are annealed together by keratin |
|
|
Pruritus
|
-Unpleasant sensation that provokes a desire to scratch
ITCHY SKIN |
|
|
Pathogenesis of Acute Epidermal Trauma
|
-Trauma → cytokine release by keratinocytes → dermal vasodilation, protein extravasation and inflammatory cells surround superficial dermal blood vessels
-Inflammatory cells migrate into the epidermis -Langerhans cells migrate to the lymph nodes and present antigen -Adaptive immune response occurs |
|
|
Reaction to Skin injury
|
-Involves the entire cutaneous unit
-Multiple processes/structures are involved in any pathogenic process -Have to understand the timing of lesion development to understand the lesion -Use skin biopsies |
|
|
Lifespan of skin lesions
|
-All evolve over time
-Skin biopsies can be used for Dx and direction for therapy -Thermal burn: 2-3 days will get coagulative necrosis on histology, 7-10 days get dermal fibrosis and scarring -Pyoderma: papules progress to pustules, then epidermal collarettes --pustule is short-lived |
|
|
Effects of chronic surface trauma on the skin
Gross lesions |
-Regionally extensive
-Lichenification is a focal cutaneous thickening/nodule formation --mayor may not have erosions/ulcers |
|
|
Signs of Chronic surface trauma
|
-Hair loss
-Skin thickening -Erythema -Erosions -Hyperpigmentation -Scales -May or may not see crusts |
|
|
Hair follicle chronic trauma
|
-Hyperplasia of the Outer Root sheath
-May or may not have atrophy also |
|
|
Sebaceous gland chronic trauma
|
-Sebaceous gland hyperplasia
|
|
|
Apocrine gland chronic trauma
|
-Pores blocked
-Become dilated -Periapocrine inflammation |
|
|
Dermis chronic trauma
|
-Fibroplasia in the superficial dermis that leads to fibrosis
|
|
|
Histopathology of chronic skin trauma
|
-Hyperplasia of skin with formation of rete ridges
-Skin forms a tighter bond to the dermis -Compact orthokeratotic hyperkeratosis (anuclear) -May or may not have patchy parakeratotic hyperkeratosis (nuclei retained) -Hyperpigmentation is common |
|
|
Pattern Diagnosis
|
-Pattern recognition is important for neoplastic and inflammatory disorders
--can see at low magnification -Pattern corresponds to a list of differential diagnoses -Diseases tend to produce typical reaction patterns in the dermis -Method of pattern diagnosis was developed by Ackermann -Used by pathologists to read and report findings in skin and tumor biopsies |
|
|
Patterns in Dermatopathology
|
1. Perivascular dermatitis
2. Interface dermatitis 3. intraepidermal Vesicular and pustular dermatitis 4. Subepidermal Vesicular and pustular dermatitis 5. Nodular and Diffuse Dermatitis 6. Folliclitis/perifolliculitis and furunculosis 7. Vasculitis 8. Panniculitis 9. Atrophic dermatoses 10. Fibrosing dermatitis |
|
|
Superficial Perivascular Dermatitis
|

Inflammatory cells aggregate around dermal blood vessels
-May have dermal edema and spongiosis -Generally non-specific inflammatory reaction -Eosinophilic infiltrate: allergy -Neutrophilic infiltrate: bacterial |
|
|
Interface Dermatitis
|
-Inflammatory change focused on basal cell layer
-Limited number of potential causes --Usually autoimmune or hereditary disease --Immune complex deposition, type II hypersensitivity reaction, auto-reactive cytotoxic T-cells -Characterized by lichenoid band and hydropic degeneration |
|
|
Intraepidermal Vesicular and Pustular Dermatitis
|
-Intraepidermal fluid-filled spaces due to intracellular or intercellular edema
-Pustules are filled with inflammatory cells, are more common than vesicles |
|
|
Subepidermal Vesicular and Pustular Dermatitis
|

-Vesicles form within or below the basement membrane
-Caused by immunologic or mechanical forces -Autoimmune or congenital disease |
|
|
Nodular and Diffuse Dermatitis
|
-Usually infectious agent or foreign material
-Nodular discrete clusters or diffuse dense cellular infiltrate -Neutrophils dominate: bacterial -Eosinophils dominate: parasitic or allergic-eosinophilic granuloma -Histiocytes: chronic granulomatous or pyogranulomatous lesions |
|
|
Folliculitis/Perifolliculitis and Furunculosis
|

|
|
|
Vasculitis
|
-Inflammatory cell infiltrate within/around the vessel wall
--leukocytoclasia -Evidence of vascular injury --endothelial swelling or necrosis, fibrinoid change, intravascular fibrin thrombi |
|
|
Panniculitis
|
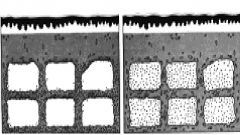
-Extension of dermal inflammation
-Damage to adipocytes results in release of lipids --lipids undergo hydrolysis into fatty acids and glycerol -Most inflammatory diseases are sterile and idiopathic -Can also be an infectious agent, foreign body, trauma, vasculitis, or nutritional cause |
|
|
Atrophic Dermatosis
|
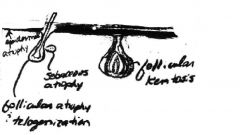
-Most often associated with endocrine disorders
-Results in bilaterally symmetrical alopecia, dull, dry hair coat, hyperpigmentation -Not pruritic |
|
|
Fibrosing Dermatitis
|

-Loss of adnexal units with dermal fibrosis
-Chronic change indicative of prior cutaneous insult |
|
|
Superficial Perivascular dermatitis
|
Inflammatory cells aggregate around dermal blood vessels
-May have dermal edema and spongiosis -Generally non-specific inflammatory reaction -Eosinophilic infiltrate: allergy -Neutrophilic infiltrate: bacterial |
|
|
Acute perivascular dermatitis
|
-Dermal edema with mild inflammatory infiltrate
-Acute inflammation produces edema -Will have dermal edema and epidermal edema -Eosinophils present: type I hypersensitivity reaction |
|
|
Chronic Perivascular dermatitis
|
-Lesions of chronic superficial trauma
-Epidermal hyperplasia, increased cell layers in the epidermis -Acanthosis: hyperplasia of the stratum spinosum ONLY -Rete ridge formation, projections of epidermis into the dermis |
|
|
Acanthosis
|
-Hyperplasia of the Stratum Spinosum only
-Can see bridging desmosomes -Indicates edema |
|
|
Hyperkeratosis types
|
-Orthokeratotic hyperkeratosis: normal process
--anuclear hyperkeratosis -Parakeratotic hyperkeratosis: Abnormal process --retained nuclei --increased keratinocyte cell turnover --Metabolic disease |
|
|
Type I hypersensitivity reaction
|
-Causes Wheal and flare response in skin
-Vascular congestion -Can be sensitivity to environmental allergens, food allergy, flea allergy, sarcoptic mange |
|
|
Sarcoptic Mange and Dermal reaction
|
-From Sarcoptes scabiei mite
-Transmissible to humans and animals -Causes severe pruritus on the abdomen, chest, legs, elbows, and pinnae -Mites burrow into the stratum corneum -Mites themselves are rarely found |
|
|
Superficial bacterial infections of the Skin
|
-Perivascular accumulation of neutrophils as inflammatory cells undergo transmigration from vasculature into the vascular space
-Causes epidermal pustules and crusts -Common to have both an allergy and pyoderma |
|
|
Allergic Dermatitis
|
-Perivascular pattern of dermatitis
-Can have secondary complicating factors --superficial trauma, bacteria, fungal infection -May have parakeratosis -Hypergranulosis -Spongiosis -Epidermal hyperplasia |
|
|
Disorders associated with perivascular dermatitis
|
-Zinc-responsive dermatosis: poor diet
-Superficial necrolytic dermatitis: liver disease or glucagonoma -Flea allergy -mite infestation |
|
|
Zinc-responsive dermatosis
|
-Common in arctic breeds
-Can occur in any breed if animal has poor diet -Zinc is not absorbed from the gut -Usually a mild dermatosis -Crusty, scaly lesions on the face and pressure points -Perivascular dermatitis with epidermal and follicular parakeratotic hyperkeratosis |
|
|
Superficial necrolytic dermatitis
|
-Skin disorder in dogs with liver disease
-Hepatocutaneous syndrome -Less likely cause can be glucagonoma -Caused by lack of nutrition to the skin -Animal will have sore feet -Will see parakeratotic hyperkeratosis, acanthosis with intracellular edema in spinous layer -Hyperplasia of the basal layer keratinocytes -"red, white, blue" appearance -Poor prognosis |
|
|
Superficial Bacterial infections in Skin
|
-Perivascular accumulation of neutrophils as inflammatory cells move from vasculature into perivascular space
-Epidermal pustules/crusts -Common to have both allergy and pyoderma |
|
|
Lethal acrodermatitis of Bull Terriers
|
-Rare
|
|
|
Parakeratotic hyperkeratosis
|
-Indicative of increased epidermal turnover
--Fast epidermal turnover -Can be due to trauma, malassezia infection, and other causes when focal -If diffuse have a limited number of DDx |
|
|
Causes of Diffuse Parakeratotic hyperkeratosis
|
-Zinc Responsive Dermatosis
-Hepatocutaneous syndrome -Lethal acrodermatitis of Bull terriers -Thallium toxicity |
|
|
Interface Dermatitis Overview
|
-Pathological events target the basal keratonocytes and dermoepitermal junction
--no clear junction present --Band of lymphocytes will be present within the dermis -Immune complex deposition -Type II hypersensitivity reaction -Autoreactive cytotoxic T-cells -Tends to be more serious |
|
|
Interface Dermatitis Injury tree
|
1. Damage of basal keratinocytes
-Causes atrophic damage that leads to dermatomyositis and vasculitis -May have multifocal keratinocyte apoptosis, leads to erythema multiforme --usually due to drug reaction -Plasma cell rich infiltrate leads to discoid lupus -Lymphohistiocytic cell infiltrate leads to cutaneous lupus |
|
|
Characteristic changes associated with Interface Dermatitis
|
1. Lichenoid band of inflammatory cells
-obscures dermo-epidermal junction -Usually lymphoplasmacityc inflammatory cells 2. Hydropic degeneration of basal epithelial cells -due to intracellular edema |
|
|
Exfoliative cutaneous lupus erythematosus of German Shorthaired Pointers
|
-Lupoid derm
-Severe autosomal recessive disorder -Generalized scaling with erosions/hair loss and depigmentation -necrosis of basal epithelial cells |
|
|
Discoid Lupus erythematosus
|
-Localized lupus
-Localized to nasal planum |
|
|
Dermatomyositis
|
-Familial skin disease of young collies, shelties, and crosses
--hereditary -Interface dermatitis -lesions seen around the face, tips of ears, and pressure points |
|
|
Erythema multiforme
|
-Acute disorder
-Associated with adverse drug reactions -less commonly associated with infections and neoplasia -Lymphocyte-mediated destruction of keratinocytes --lymphocytes attack keratinocytes at all levels -Can involve oral mucosa and foot pads -Can be idiopathic -Hydropic basal cell degeneration with individual keratinocyte necrosis/apoptosis in all epidermal layers -Can be a reaction to injectible heartworm medication |
|
|
Acantholysis
|
-Loosening of the spines Gk
-Loss of cohesion between keratinocytes -Results in formation of clefts, vesicles, and pustules -Desmosomes are destroyed -No cohesion between keratinocytes -Results in SEVERE edema -Characteristic feature of pemphigus foliaceus -Caused by type II hypersensitivity -Autoimmune disease due to autoantibody production to cell adhesion molecules --antibody-emdiated targeting of cell adhesion molecules -Can also be caused by bacterial infection with release of proteolytic enzymes and bacterial toxins -rarely due to dermatophytosis |
|
|
Acantholytic cells
|
-Keratinocytes that separate completely from neighbors
-become round -Nucleus is round, uniformly stained -Cytoplasm is eosinophilic -Small numbers can be seen in superficial bacterial infection --proteolytic enzymes cleave desmosomes -Also occur during spongiosis and dermatophytosis |
|
|
Acanthosis
|
-Hyperplasia of the epidermis and stratum spinosum
|
|
|
Bacterial cause of Acantholysis
|
-Bacterial infection with release of bproteolytic enzymes and bacterial toxins
-Mild acantholysis, not a lot of acantholytic cells -Bacteria are usually present -Small pustules form --neutrophils in the pustules are necrotic -Hard to differentiate between bacterial pemphigus and autoimmune pemphigus --both cause pustules and acantholysis |
|
|
Dermatophytosis causing Acantholysis
|
-Rarely a cause of acantholysis
-Occurs in dogs and horses |
|
|
Intercellular edema
Intracellular edema |
-INTERcellular edema: spongiosis
-INTRAcellular edema: Ballooning degeneration Both cause acantholysis |
|
|
Differential Dx for Vesicular/pustular dermatitis
|
1. Autoimmune disorders
-Pemphigus foliaceus -Pemphigus vulgaris 2. Bacterial infection -Pyoderma -Superficial pyoderma -Impetigo 3. Viral infection -Contagious pustular dermatitis |
|
|
Pemphigus foliaceus
|
-Autoimmune disorder that can result in vesicular/pustular dermatitis
-Will have healthy neurtophils and no bacteria -Vesicles appear on face, ears, groin, feet, footpads --ONLY occurs on haired skin and footpads -May progress to generalized autoantibody to desmoglein 1 -Diagnose based on pattern and histology -Large intraepithelial pustules and crusts --contain non-degenerate neutrophils and acantholytic keratinocytes without bacteria or fungi -Antibody is in desmosomes adhesion complex |
|
|
Desmoglein 1
|
-Cadherin group of adhesion molecules in desmosomes
-Attacked by autoantibodies to form pemphigus foliaceus |
|
|
Pemphigus vulgaris
|
-Autoantibody to desmoglein 3
-Acantholysis occurs above the basal cell layer -Results in vesicle formation -Basal cells remain attached to the basement membrane via hemidesmosomes -Gives "tombstone" effect histologically -Occurs in oral cavity mucocutaneous junction -Acantholysis with suprabasilar clefting -Treat with immunosuppressive drugs -Less often pustular, more often get ulcers |
|
|
Pyoderma
|
-Bacterial infection of the skin
-Can be primary or secondary -May result inIntraepidermal vesicular/pustular dermatitis -Can be due to environmental or food allergies, flea allergy |
|
|
Superficial pyoderma
|
-bacterial infections that involve the epidermis and follicular epithelium
-Pustules are usually small and contain necrotic cell debris |
|
|
Impetigo
|
-Type of superficial pyoderma
-Occurs in puppies or immunosuppressed adult dogs -Sparsely haired skin is affected -Usually caused by staphylococcus pseudointermedius -Large intrapeidermal pustules containing degenerate neutrophils, some acantholytic cells, and bacterial cocci -Causes Vesicular/pustular dermatitis |
|
|
Viral infection as a cause of Vesicular/pustular Dermatitis
|
-Contagious pustular dermatitis
-Contagious ecthyma, orf, scabby mouth -Parapox infection in sheep and goats -Vesicles are transient -Epidermal hyperplasia with edema and intracytoplasmic inclusion bodies |
|
|
Pemphigus folieceous vs. Pemphigus vulgaris
|
-Foliaceous: in haired skin
--Desmoglein 1 is present throughout entire skin layer, autoantibodies to DSG1 --Desmoglein 3 is only present at the bottom --3 can compensate for 1 when it is attacked by autoantibodies, can cover if 1 is attached by autoantibodies -Vulgaris: Mucus membranes --Desmoglein 1 only exists in upper part of skin, DSG3 throughout the skin --When Desmglein 3 is attacked, 1 cannot compensate to keep skin together --deep layers are affected |
|
|
Pemphigus Foliaceous vs. Pyoderma
|
-PF: larger pustules that span several adnexal units
--crusts also present --"Healthy" neutrophils --No bacteria present --LOTS of acantholysis -Pyoderma: bacteria is present along with necrotic cellular debris and neutrophils --usually smaller pustules --minimal acantholysis |
|
|
Blistering Disorders of the Basement Membrane Zone
|
-Auto-antibody formation (autoimmune)
--Bullous pemphigoig --Hemidesomsomal protein -Congenital defect --Epidermolysis bullosa, junctional and dystrophic |
|
|
Epidermolysis Bullosa
|
-Congenital or acquired disorder
-Causes subepidermal vesicular dermatitis -Affects structural integrity of the epidermis at the basement membrane zone -Results in oral mucosa sloughing especially in areas with increased mechanical trauma -Epidermis does not stay adhered to the dermis -Acquista: due to auto-antibody to collagen VII -Junctional: due to congenital abnormality in hemidesmosomal proteins |
|
|
Cell types in Nodular/Diffuse Dermatitis
|
-Neutrophils: bacterial cause
-Eosinophils: parasitic or allergic cause -Histiocytes: chronic granulomatous or pyogranulomatous lesions --mycoabcteria, fungal, or foreign body |
|
|
Bacterial skin diseases associated with Nodular/Diffuse Dermatitis
|
-Mycobacterial granulomas: cutaneous nodules of granulomatous inflammation
--Acid-fast organisms within epithelioid macrophages --Actinomycosis, Nocardiosis |
|
|
Systemic funcal diseases with cutaneous forms
|
-Blastomycosis (Blastomyces dermatitidis)
-Saprophytic soil organism often located near water -In young male sporting breeds will cause systemic disease --weight loss, dyspnea, ocular disease |
|
|
Protozoal disease associated with Nodular/diffuse Dermatitis
|
-Leishmaniasis
|
|
|
Non-infectious Diffuse/Nodular Dermatitis
|
-Eosinophilic granuloma
-Localized erythematous plaque -On medial inguinal area, oral cavity -Large raised lesions due to hypersensitivity reaction -Allergic phenomenon -Diffuse eosinophilic dermatitis with granulomatous response surrounding hypereosinophilic dermal collagen -Associated with allergic skin disease in cats |
|
|
Perifolliculitis
|
-Inflammation around the hair follicle
|
|
|
Folliculitis
|
-inflammation in the hair follicle
|
|
|
Mural folliculitis
|
-Inflammation targeting the wall of the hair follicle
|
|
|
Furunculosis
|
-Follicle rupture within inflammation
-Foreign body reaction to keratin in the dermis -lesions often progress from folliculitis to furunculosis -Rupture can carry bacteria with it -AKA deep pyoderma |
|
|
3 major causes of folliculitis
|
1. bacterial
2. dermatophyte (ringworm) 3. Demodex mites |
|
|
Bacterial folliculitis
|
-Staphylococcus pseudointermedius is commonly isolated
-Usually secondary to another primary disease -May result in furunculosis |
|
|
Dermatophytosis folliculitis
|
-"Ringworm"
-Fungi that utilize keratin in hair and epidermis -3 genera: microsporum, trichophyton, epidermophyton -Luminal folliculitis, mural folliculitis (cats and horses), pyogranulomatous furunculosis -Fungal hyphae and arthrospores in hair follicles and on hair shafts -Histologically cannot see distinction between the hairshaft and the medulla --filled with fungus -Zoonotic |
|
|
Demodex canis
|
-Mites reside in the hair follicle
-Normal skin flora on the face of dogs -"Cigar-shaped" mites -Proliferate under states of immunosuppression --In puppies, juvenile form --in older dogs, immunosuppressed form -Causes lymphoplasmacytic mural folliculitis -Furunculosis is common -Foreign body reaction is common -Skin will ave hair loss, hyperpigmentation |
|
|
Other non-infectious folliculopathies
|
-Pattern alopecia
-Cyclic flank alopecia -Color dilution alopecia --black hair follicular dysplasia |
|
|
Follicular changes
|
-Outer root sheath can undergo same changes as epidermis
-Folliculitis -Follicular keratosis -Follicular Atrophy- different forms --faded follicles --excessive trichilemmal keratinization --miniaturization -Follicular dysplasia/color dilution alopecia -Follicular neoplasia |
|
|
Vasculitis
|
-Inflamamtory cell infiltrate within or around the blood vessel wall
-Can have evidence of vascular injury --endothelial swelling/necrosis, fibrinoid change, intravascular fibrin thrombi -Often associated with existing disease --bacterial or viral infection -Can be due to autoimmune disease or adverse drug reaction -Commonly idiopathic cause -Will have swelling and hemoorhage, sometines infarcts -Can see necrosis of vessel, fibrin with edema in the adjacent tissue |
|
|
Post-vaccinal alopecia
|
-Associated with rabies vaccination
-Local reaction in skin -Ischemia to hair follicles -Ischematic change induces telogen in hair follicles |
|
|
Causes of Panniculitis
|
-Trauma
-Foreign body -Infectious (have to rule out) -rarely autoimmune -Often idiopathic and sterile --immune-mediated process Firm swellings in the skin with ulcers that weep fluid |
|
|
Hyperadrenocorticism and Atrophic Dermatoses
|
-Due to increased endogenous glucocorticoids or exogenous administration of glucocorticoids
-Results in atrophy of epidermis, hair follicles in telogen phase, and follicular hyperkeratosis |
|
|
Topical corticosteroids and skin
|
-Can cause atrophy of skin
|
|
|
Calcinosis Cutis
|
-Mineralization of dermal collagen
-Hallmark lesion of hyperadrenocorticism -Indicates long-standing cushing's disease -Collagen acts as foreign body, extruded out into the skin -Skin mineralizes and can become bone |
|
|
Dermal Fibroplasia
|
-Proliferation of fibroblasts and blood vessels with new collagen production
--granulation tissue production |
|
|
Dermal Fibrosis
|
-End-stage fibroplasia
-Increased collagen deposition with altered arrangement -May find a few remaining fibroblasts |
|
|
Anatomical components of the Ear
|
-Pinna
-Ear canal -Ear drum/Tympanic membrane -Ossicles -Eustachian tube -Vestibular organ with semi-circular canals and otolith organs -Cochlea -Auditory nerve |
|
|
Diseases of the External Ear
|
-Otitis externa
-Hematoma -Pinnal vasculitis/necrosis -Alopecia -Dermatological conditions Epidermis can get hyperplastic Seruminous glands get hyperplastic -Increased keratin can cause stenosis of the canal |
|
|
External ear
|
-Auricle/pinna
-Externa acoustic meatus/passageway -Auricle to the tympanic membrane |
|
|
Inner Ear
|
-Membranous labyrinth
-Utriculus of 3 semi-circular ducts --contribute to balance -Saccules --cochlear duct, hearing |
|
|
Middle Ear
|
-Tympanic membrane
-Bulla -Ossicles --malleus, incus, stapes -Auditory tube/Eustachian tube --connects tympanic cavity with the nasopharynx |
|
|
Otitis externa
|
-Common pathology in dogs
-Long pinna, hair in the ear canal, and stenotic canals are predisposing factors --ear can occlude canal -Inflammation will also decrease the diameter of the ear canal -Allergic skin disease is also predisposing factor -Ear mites in rabbits, cats, rats, goats --otodectes in kittens --psoroptes in rabbits -Foreign bodies (kids putting stuff in ears) --usually unilateral condition -Endocrine diseases (cushing's) -Neoplasia -Microorganisms are linked to situation that permits proliferation of bacteria |
|
|
Pitbull ear canals
|
-Have tiny stenotic ear canals
-Predisposes to otitis externa |
|
|
1st time otitis
|
-Usually due to yeast or bacterial cocci
-Subsequent infections can destroy the natural bacteria in the ear -Secondary organisms an grow in the wax in the ear --pseudomonas --E. coli |
|
|
Tympanic membrane rupture
|
-Can lead to infection
-Will get pus in the middle ear -Can eventually get pus into the inner ear --causes balance problems -Animal will be deaf |
|
|
Aural hematoma
|
-Will have otitis first
-Animal shakes its head so hard a hematoma forms in the ear --trauma from head shaking -Small space for blood to pool, can get very large -Hematoma develops on the concave side o the pinna -Starts out fluctuant and becomes firm with organization --leads to disfigurement |
|
|
Vasculitis on pinna
|
-Can be idiopathic or infectious
-Tick-borne lesions -Post-vaccinal vasculitis in dogs |
|
|
Gross lesions on the External Ear
|
-Severity depends on chronicity and microbial population
-Will have hyperemia, accumulation of cerumen -Ceruminous gland hyperplasia gives "cobblestone" appearance -May or may not have purulent discharge and debris -Stenosis |
|
|
Histopathology of External ear Otitis
|
-Epidermal hyperplasia
-Atrophy of hair follicles -Hyperkeratosis -Sebaceous and ceruminous gland hyperplasia -May or may not have ulcers -Inflammatory cells present -Dermal fibrosis -Ossification |
|
|
Otitis Media
|
-Inflammation of the tympanic cavity
-Usually bactieral cause --can be acute or chronic -Can enter middle ear via eustachian tube (pigs,lambs, cats) or punctured tympanum (dogs, cats) -Animal will have conduction deafness and pain -Ear looks hyperemic with edema, ulcers, exudate -Ossicles and tympanum can become lysed -May have mineralization of necrotic material within the bullae that can spread to the inner ear and mrainstem |
|
|
Guttural Pouch empyema
|
-In horses
-Suppurative inflammation of the guttural pouches -Streptococcus equi (strangles) -Want to flush out and culture the pus -May have to go in and clean out surgically |
|
|
Guttural pouch Mycosis
|
-Occurs in horses
-Fungal infection of the guttural pouch -Often due to aspergillus -Can lead to rupture of the internal carotid artery and bleeding out |
|
|
Otitis Interna
|
-Inflammation of the inner ear
--involves cochlea, vestibule, and semicircular canals -Usually secondary to otitis media -Bacterial and suppurative -May ascend the Vestibulocochlear nerve to the brain --rare --Can cause focal meningoencephalitis in the pons and medulla -Animal will have vestibular dysfunction and deafness --vertigo, nystagmus, nausea, ataxia, torticollis |
|
|
Types of deafness
|
1. Conduction deafness
2. Sensorineural deafness |
|
|
Conduction deafness
|
-Interference with the conduction of sound results in deafness
-Can be due to disease in the external or middle ear -Caused by inflamamtion, neoplasia, rupture of the tympanum, entrapment of ossicles in granulation tissue |
|
|
Senssorineural deafness
|
-Maldevelopment or degeneration of the sensory organ, 8th cranial nerve, or auditory pathways within the brain
-Usually involves the organ of corti -Most prevalent type of deafness in animals -Can be due to Hereditary cochleosaccular degeneration, Senile, or ototoxic causes |
|
|
Hereditary cochleosaccular degeneration
|
-Type of sensorineural deafness
-Complex inheritance pattern -May be associated with incomplete pigmentation of the hair coat and uvea in dogs, cats, mink, and mice -Atrophy of the sensory and supporting cells of the organ of corti, saccular macula -Collapse of the dorsal or lateral walls of the cochlear and saccular membranous labyrinth -Secondary degeneration of neurons within the spiral ganglion |
|
|
Senile deafness
Presbycusis |
-Degeneration of hair cells in the organ of corti and loss of neurons from the spiral ganglion
|
|
|
Acoustic and Chemical ototoxicity
|
-Deafness due to noise or chemicals
-Chemicals: aminoglycoside antibiotics --gentamycin, streptomycin, neomycin --cats are very susceptible --toxicity is dose-dependent -Diuretics: furosemide, bumetanide, ethacrynic acid -Acetylsalicylic acid (asprin) |
|
|
Vestibular Disease
|
-Central or peripheral disease
-Same causes as deafness --inflammation, neoplasia, trauma, toxins -Idiopathic cause is common -Can be associated with otitus or brain tumor -Clinical signs include head tilt, falling forwards to affected side, ataxia without weakness, nystagmus -more easily detected than hearing loss --mild lesions of the inner ear are more often associated with vestibular lesions instead of hearing deficits |
|
|
Neoplasia in the Ear
|
1. Skin tumors on the pinna
2. Ceruminous gland neoplasms 3. Nasopharyngeal and inflammatory polyps 4. Dentigerous cyst |
|
|
Skin tumors on the Pinna
|
-Histiocytoma and plasmocytoma are common
-Squamous cell carcinoma in white cats and sheep -Trihoblastoma -Sebaceous gland adenoma/epithelioma |
|
|
Ceruminous gland neoplasms
|
-Develop in animals with chronic otitis
-Modified apocrine sweat glands -Seen in older dogs and cats --in dogs most are benign --in cats 50% are malignant -Adenomas and carcinomas -Carcinomas may invade from auditory meatus into a region of the parotid salivary gland or into bone --usually in the ear canal |
|
|
Nasopharyngeal and Inflammatory polyps
|
-Polyps in ears
-Originate in the Eustachian tubes -Common in cats -Connective tissue, blood vessels, lymphocytes covered by stratified to columnar epithelium |
|
|
Dentigerous Cyst
|
-occurs in foals
-draining nodule on the rostral aspect of the base of the pinna |
|
|
Hematopoietic tissue
|
-Primary site of blood cell production in adults
-Hematopoiesis can occur elsewhere also, most often spleen --extramedullary hematopoiesis -Flat and long bones in animals -With age, central areas and distal extremities of bone are replaced with fat (yellow marrow) |
|
|
Bone Marrow Hematopoietic environment
|
-Hematopoiesis takes place between the venous sinuses in the marrow cavity itself
-Reticular cells are specialized fibroblasts --extend cytoplasmic processes into the hematopoietic spaces --forms scaffold to support hematopoietic cells -Osteoblasts, osteoclasts, and flat cells line endosteum -Stromal cells provide structural support and produce extracellular matrix components -Adipocytes, macrophages, lymphocytes, plasma cells |
|
|
Hematopoietic cell behavior
|
-Influenced by direct cell-cell and cell-matrix interactions
-Soluble mediators are important --cytokines and hormones -Undergo sequential divisions as they develop --progressively higher numbers of cells as hematopoietic cells mature -Cells continue to mature after they have stopped dividing |
|
|
Hematopoietic tissue
|
-Highly proliferative and self-renewing
-Gives rise to cells with committed differentiation programs -Common ancestor of all blood cells |
|
|
Products of Hematopoiesis
|
-Pluripotent stem cell → Myeloid stem cell →
--RBCs --granulocytes --Monocytes --Platelets |
|
|
Erythropoiesis
|
-Formation of RBCs
-Organized series of maturation regulated by Erythropoietin -Rubriblast → prorubricyte → rubricyte → metarubricyte → polychromatophil → RBC -Normal development time is about 1 week -Reticulocytes start maturation in bone marrow and finish in peripheral blood circulation and spleen --except horses, do not release reticulocytes into circulation |
|
|
Erythropoietin
EPO |
-Dominant regulator of erythropoiesis
-Glycoprotein -Acts on early erythroid progenitor cells with other cytokines -Synthesized in the kidney -Promotes proliferation of RBCs -Inhibits apoptosis of RBCs -Stimulus for increased production is hypoxia |
|
|
Reticulocytes vs. RBCs
|
-RBCs: no organelles
-Reticulocytes: have ribosomes and mitochondria --make reticulocyte bluish/purple |
|
|
RBCs
|
-Mature reticulocytes
-No organelles -Take about 1 week to mature -Last about 150 days in horses and cattle --100 days in dogs --70 days in cats -Production is stimulated by hypoxia and increase EPO synthesis in the kidney |
|
|
Granulocytes
|
-Neutrophils
-Eosinophils -Basophils -Monocytes Important immune functions |
|
|
Granulopoiesis and Monocytopoiesis (Myelopoiesis)
|
-Formation of granulocytes and monocytes
-Initiated by release of inflammatory mediators (IL and TNF-a) --mediators stimulate fibroblasts, macrophages, and endothelial cells to produce cytokines --G-CSF and GM-CSF) -Increase in cytokines G-CSF and GM-CSF result in increased granulopoiesis and monocytopoiesis -Progranulocyte → myelocyte → metamyelocyte → band cell → neutrophil, eosinophil, or basophil (granulocytes) -Process takes about 5 days for neutrophils |
|
|
Neutrophil formation and life span
|
-Formation from myeloblast → neutrophil takes about 5 days
-Reserve of fully mature neutrophils is maintained in the bone marrow -Predominant leukocyte type in the blood of most domestic species -Only in circulation for less than 12 hours |
|
|
Megakaryopoiesis
Thrombopoiesis |
-Regulated by Thrombopoietin synthesized mostly in liver
--produced constitutively -Progenitor cell → endomitosis to become polyploid → extend cytoplasmic processes bone marrow venous sinuses → shed cytoplasmic fragments (platelets) into circulation |
|
|
Thrombopoietin
|
-Synthesized mostly in the liver
-Dominant regulator of thrombopoiesis -Produced at a constant rate |
|
|
TPO receptor
|
-Expressed by platelets and their precursors
-Binds Thrombopoietin in the plasma -Platelet mass decreases, less TPO is bound to platelet receptors --increased concentration of TPO in free plasma stimulates thrombopoiesis |
|
|
Megakaryocytes
|
-Arise from a progenitor cell
-Undergo endomitosis to become polyploid --8N-32N -Cytoplasmic processes extend into the lumina of the bone marrow venous sinusoids -Membrane-bound cytoplasmic fragments are shed into bone marrow venous sinusoids |
|
|
Diagram of Hematopoiesis
|

|
|
|
Bone marrow Aspirates
Cytology |
-Collections of cells smeared on a slide and examined microscopically
-Faster than a biopsy -More detailed evaluation of internal structures of the marrow -All you have are cells, no relationships - |
|
|
Bone Marrow Core Biopsy
|
-Histological preparations
-Sections of tissue that are fixed with formalin or embedded in paraffin/plastic -Allows for definitice determination of cellularity and fibrosis -Takes more time -Fixation can add artifacts |
|
|
General aspects of a Bone Marrow Evaluation
|
-Peripheral demands for WBCs, RBCs and platelets results in rapid shift of bone marrow cytologic profiles
--due to hyperplastic responses -Changes can be due to blood loss, diseases of bone marrow --bone marrow responds by making RBCs - |
|
|
Bone Marrow Evaluation
|
1. Cellularity and Particles
--are bone marrow spicules/particles present? --Is cellularity increased? 2. Should see all maturation sequences and morphology --all 3 lines (myeloid, erythroid, megakaryocytic) 3. Frequency of lymphocytes, macrophages, and plasma cells, other cells also 4. Adequacy of Iron 5. Presence of abnormal cells 6. Myeloid:Erythroid ratio calculation |
|
|
Myeloid:Erythroid Calculation
|
-Only erythroid and myeloid cells, NOT megakaryocytes
-Normal M:E in companion animals is 1:1 or 2:1 -Normal M:E in livestock and horses is 0.5:1 |
|
|
Common indications for a Bone Marrow Evaluation
|
-Unexplained, persistent increases or decreases in particular cell lines
-Abnormal/immature cells in curculation -Atypical cellular reactions -Fever of unknown origin -Unexplained laboratory findings -Staging of Malignancies -Systemic infections -MUST submit CONCURRENT CBC |
|
|
Indications for a Core Biopsy
|
-Bone changes
--osteosclerosis, osteopenia, osteolytic lesions -Bone marrow cellularity --hypocellular, hypercellular, aplasia -Bone marrow fibrosis -Focal lesions -Unsuccessful aspiration biopsy if aspirate is poorly cellular |
|
|
Bone Marrow Hyperplasia
|
-Increase in response to peripheral demand for a specific cell type
-Can be generalized to all cell lines or specific to one cell line -Predictable increase if animal is not diseased -Erythroid hyperplasia -Myeloid hyperplasia -Megakaryocytic hyperplasia -Lymphocytosis/plasmacytosis -Histiocytosis -Mastocytosis |
|
|
Erythroid Hyperplasia
|
-Usually due to hemorrhage of hemolysis
-Hemorrhage: internal or external blood loss -Hemolysis: RBC destruction -Low Hb → hypoxemia → EPO production stimulated → increased erythropoiesis -Increased in RBC production causes decrease in M:E ratio --more Erythroid progenitors in marrow -Immature polychromatic RBCs may appear in peripheral blood |
|
|
Causes of Hemorrhage
|
-Trauma
-Defect in hemostasis -Neoplasia -GI ulceration -Parasitism -Coagulopathies (inherited or toxins) |
|
|
Causes of Hemolysis
|
-Extravascular hemolysis:
--immune mediated --hemoparasitism --toxicity -intravascular hemolysis: --immune-mediated (IMHA) --hemoparasitism --toxicity --enzymatic deficiencies -Oxidant injury --Hypophosphatemia |
|
|
Polychromatophilic RBCs in Peripheral blood
|
-Indicate hemolysis or hemorrhage
-Polychromasia on CBC --"reticulocytes" when stained -Other cell lines stay normal but will be perceived to be decreased due to large expansion of erythroblast population |
|
|
Regenerative anemia
|
-Regeneration can occur
-increased reticulocytes indicates that regeneration is happening |
|
|
Iron stores and blood loss
|
-With acute blood loss Fe stores remain adequate
--demand for RBCs can still be met -With persistence of blood loss will have depletion of Fe --Regnerative response is less, eventually results in non-regenerative anemia -Non-regenerative anemia is secondary to Fe depletion |
|
|
Erythroid Hyperplasia with concurrent myeloid hyperplasia
|
-Acute, severe anemia due to hemolysis or hemorrhage
-Immediate, no time for tissue to respond to insult -M:E ratio can be normal due to hyperplasia of both cell lines -Acute disease in Hb → tissue O2 is compromised → tissue necrosis → myeloid hyperplasia to increase macrophages and neutrophils → peripheral leukosis -RBC line is also increasing to respond to hemorrhage |
|
|
Erythroid Hyperplasia without Anemia
|
1. Chronic O2 deprivation
--altitude, chronic lung or heart disease 2. Hyperthyroidism due to increased metabolic demands for O2 3. Compensated hemolytic disease -O2 deprivation and Hyperthyroidism can result in a peripheral erythrocytosis (high RBC count) |
|
|
Myeloid Hyperplasia
|
-Response to an increased need for granulocytes or monocytes
-Common with certain types of inflammation --infection, abscesses, any inflammatory state -M:E increases, more M than E in blood -May be a left-shift in granulocyte production within the marrow --characterized by an increase in immature forms -Marrow responds by increasing megakaryocytes -Will have more immature cells with "left shift" in maturation -Antigens or endotoxins (inflammatory state) → IL1 released from cells → TNF-a → release of additional factors |
|
|
Megacaryocytic Hyperplasia
|
1. Peripheral destruction (ITP)
2. Platelet loss due to hemorrhage 3. Consumption (DIC) |
|
|
Non-specific increases in Hematopoiesis
|
-Can be due to antigenic stimulation, chronic infections, toxic insults
-Lymphocytosis -Plasmacytosis -Histiocytosis -Mastocytosis -Increases are not helpful for cytology, have to look for something else |
|
|
Bone Marrow Hypoplasia
|
-Results in a peripheral decrease in that cell type
-Clinical signs reflect missing cell type -Changes M:E ratio -Peripheral cytopenia indicates abnormal response --low numbers of cells -Can be measurable hypoplasia of one or more cell lines or a failure to respond with appropriate hyperplasia -No response to peripheral changes is abnormal |
|
|
Bone Marrow Hypoplasia due to chronic disease or inflammation
|
-Most common cause of non-regenerative anemia
-M:E is normal or slightly increased -Marrow-based disease, marrow does not respond to insult/injury and make new RBCs -Can be due to: -- immune-mediated targeting of hematopoietic cells --Cytotoxicity or drug-induced --Infection (Parvovirus, FeLV, FIV) --Endocrine-induced (hyperestrogenism, hypothyroidism) --Iron deficiency (loss of Hb addition to RBCs) --Renal failure (decreased EPO) --Malnutrition --Idiopathic |
|
|
Hepcidin
|
-Acute-phase protein
-Synthesized in the liver -Expression increases with inflammation, infection, or Fe overload -Decreases with anemia or hypoxia -Limits Fe availability -Binds to and degrades cell surface iron efflux molecule (ferroportin) --causes functional Fe deficiency -Inhibits absorption of dietary Fe from GI -Inhibits export of Fe from macrophages and hepatocytes into the plasma |
|
|
Inflammatory cytokines contributing to anemia
|
-TNF-a and IL-1
-INhibits erythropoiesis by oxidative damage -Triggers apoptosis of developing erythroid cells -Decreases expression of EPO, EPO receptors, and stem-cell factor |
|
|
Bone Marrow Inflammation
|
-May not be recognized in bone marrow aspirates
--inflammatory cells are normal component of marrow --inflammation can be focal and missed in sampling -Acute myelitis -Granulomatous or pyogranulomatous |
|
|
Acute Bone Marrow Myelitis
|
-Fibrinous and neutrophilic
-Dogs and cats with non-regenerative IMHA can have bone marrow inflammation with fibrin deposition, edema, and neutrophils |
|
|
Granulomatous or Pyogranulomatous Bobe Marrow Myelitis
|
-Diffuse or multifocal increase in macrophages and epithelioid macrophages
|
|
|
Myelodysplastic syndrome
|
-Hematopoietic neoplasia
-Defect in myeloid stem cell, issue within the marrow -Clonal myeloid proliferative disorder -Ineffective hematopoiesis -Results in peripheral cytopenia of the affected cell populations -Hyperplasia of one or more cell line without change in the peripheral cell count -Can precede development of acute myeloid leukemia -Blast cell % is higher than normal but not higher than 20% --more than 20% = leukemia -Rare in veterinary medicine, most often occurs in cats with FeLV |
|
|
Leukemia
|
-Umbrella term for malignant hematopoietic neoplasms that originate in the bone marrow
-Typically have significant numbers of neoplastic cells in the blood -Can refer to other forms of neoplasia originating outside of the bone marrow that progress to include bone marrow and blood -Lymphocytic or myelogenous -Acute or chronic based on degree of differentiation of neoplastic cells |
|
|
Acute Myeloid leukemia
|
-Progressive anemia, decrease in functional leukocytes, or thrombocytopenia
-Peripheral blood smear detects blast cells -Marrow blasts of myeloid origin are more than 20% of all nucleated cells --lack of maturation -Extremely poor prognosis -Mostly seen in cats with FeLV |
|
|
Chronic Myeloid Leukemia
|
-Rare chronic neoplastic disorder
-Very high peripheral cell counts -Marrow hyperplasia of the affected cell line -Cells have normal morphology --Dx by elimination -Many types of CML |
|
|
Types of Chronic Myeloginous Leukemia in Animals
|
-Chronic granulocytic leukemias of neutrophils, eosinophils and basophils
-Chronic myelomonocytic leukemia -Mast cell leukemia -Essential thrombocythemia --CML of platelet lineage -Polycythemia vera --CML of erythrocyte lineage |
|
|
Acute Lymphoid leukemia
|
-Large, immature lymphocytes
--Usually in high numbers of circulating blasts -May efface the marrow -Occurs mostly in younger to middle-aged animals |
|
|
Chronic Lymphoid Leukemia
|
-Small, well-differentiated lymphocytes
-Usually do not efface the marrow -Usually occurs in older animals |
|
|
Multiple Myeloma
|
-Malignant Neoplasm of plasma cells
-Disseminated neoplasm throughout the marrow and spleen -Usually not "leukemic" but can be -Well-differentiated or pleomorphic cells -Associated with production of a single type of immunoglobulin --monoclonal or M-protein -Monoclonal population of plasma cells that make 1 type of Ig -Patient can be hypercalcemic and destroying bone -Can see "flame cytoplasm" on histology -Diagnose based on 2 out of 4 criteria: --Marrow plasma cells greater than 30% --Monoclonal protein (M-spike) --Bence-jones protein in the urine --Lytic bone lesions |
|
|
Other hematopoietic neoplasms
|
-Systemic mastocytosis
-Histiocytic sarcoma -Metastatic carcinoma |
|
|
Myelofibrosis
|
-Fibrosis of the bone marrow
-Usually reactive to injury, neoplasia, or inflammation -Generally secondary/reactive to other injury --sepsis, hematopoietic malignancies, drug toxicity, IMHA -Difficult to aspirate -Histologic diagnosis -Pancytopenia of all cells -If primary is a myeloproliferative disorder |
|
|
Organs in the Lymphatic system
|
-Thymus
-Spleen -Lymph nodes -Lymph nodules -Bursa of Fabricius (in birds) Primary lymphoid organ --animals= thymus and bone marrow --Ruminants: peyer's patches --Birds: bursa of fabricius |
|
|
Dense cell aggregates in the body
|
-Tonsils
-MALT/BALT/GALT -Peyer's patches -Bone marrow |
|
|
Secondary lymphoid organs
|
-Spleen
-Lymph nodes -Lymph nodules -Responsible for immune responses --produce antibody and cell-mediated immunity |
|
|
Lymphopoiesis
|
-Production of new lymphocytes
-T-lymphocytes= effector cells of cell-mediated immunity -B-lymphocytes= effector cells of humoral immunity -Pluripotent stem cell → T-cell or B-cell -B-cells become plasma cells and produce antibody |
|
|
T-cell development
|
-Originate in Bone marrow, migrate to the thymus to undergo differentiation, selection and maturation
-Once mature migrate to peripheral lymphoid tissue as effector cells -Prothymocyte (in bone marrow)→ Cortical thymocyte (in thymic cortex) → medullary thymocytes |
|
|
T-cells
|
-50-70% of peripheral blood mononuclear cells
-Located in paracortical regions of lymph nodes and periarteriolar sheaths of the spleen -Recognize antigen only after antigen processing into peptide fragments and associated with MHC molecules -CD4 (helper T-cells) -CD8 (cytotoxic T-cells) |
|
|
B-cell Development
|
-Development occurs in 2 phases
1. Antigen-independent phase in primary lymphoid tissue (bone marrow, ileal Peyer's patches) --B-cells express IgM and IgD on surface --Mature B-cells 2. Antigen-dependent phase in secondary lymphoid tissues (spleen, lymph nodes, tonsils, peyer's patches) --Antigen-activated mature B-cells differentiate into IgM secreting plasma cells or switch to another antibody isotype -Progenitor B-cell → pre B-cell → Immature B-cell → Mature B-cell |
|
|
B-cells
|
-5-20% of peripheral blood mononuclear cells are B-cells
-Located in lymphoid follicles -Can recognize soluble antigen |
|
|
NK cells
|
-Bone-marrow derived
-AKA "large granular lymphocytes" -5-15% of peripheral blood mononuclear cells -Non-specific cytotoxic cells --Early response to tumor cells and viral infections -Cytoplasm has cytotoxic granules with perforin and granzymes --lyse target cells -Not HMC restricted -Do not develop memory cells -Part of innate immunity |
|
|
Thymus
|
-Maximal mass relative to body size at birth
-Involutes following sexual maturity -Lymphoid and epithelial components are gradually replaced by loose connective tissue and fat -Stromal portion is made of epithelial cells (Hassall's corpuscles), macrophages, and dendritic cells --contribute to microenvironment essential for T-cell development -Thymocyte portion has T-lymphocytes at different stages of maturation |
|
|
Types of Injury to the Thymus
|
-Congenital
-Lymphoid Atrophy --infectious agents, toxins, chemotherapeutic agents, malnutrition -Inflammation -Hematomas -Neoplasia --thymoma --lymphoma -Hyperplasia |
|
|
Thymic Cysts
|
-In cranial mediastinum
-Lined by ciliated epithelium --remnrants of branchial arch epithelium -Usually incidental finding |
|
|
Thymoma
|
-Neoplasm of Epithelial portion of the Thymus
-Associated with Myasthenia gravis --progressive muscle weakness exacerbated by exercise -Associated with exfoliative dermatitis in cats, dogs, and rabbits -Seen in older dogs, cattle, cats, horses, ferrets, pigs, sheep and goats -Slow-growing encapsulated tumor -Rarely metastasize |
|
|
Thyimc Lymphosarcoma
|
-Neoplasm of lymphoid component (T-cells)
-Most often seen in younger cats (FeLV) and young cattle -Can take up a TON of space --clinical signs relate to space-occupying effect of the mass -Histologically will see lots and lots of T-cells |
|
|
Causes of Small lymph nodes
|
-Developmental disorders
-Immunodeficiency disorders -Lack of antigenic stimulation -Malnutrition -Aging -Viral infections --Canine Distemper, BVDV, EHV-1, Feline panleukopenia virus, FIV, Hog Cholera -Radiation |
|
|
Causes for Enlarged Lymph nodes
|
-More common than small lymph nodes
-Hyperplasia with or without drainage -Lymphadenitis --bacterial, viral, fungal, protozoal cause -Metastatic neoplasia -Primary neoplasia -Discoloration or pigmentation is usually associated with hyperplastic reaction |
|
|
Lymphadenopathy
|
-Regional or generalized enlargement of unknown or unspecified cause
|
|
|
Lymph Nodes
|
-Have components of 2 different systems
--monocyte-macrophage --lymphopoietic -Structurally divided into 3 zones --Superficial cortex --Deep cortex/paracortex --Medulla -Surveillance and immune function -Antigen enters lymph/blood vessels and is transported to the draining lymph node -In lymph node antigen is surrounded by macrophages and lymphocytes |
|
|
Structural divisions of the Lymph node
|
1. Superficial cortex
--B-cells form immunologically active primary follicles or active secondary follicles with germinal centers 2. Deep cortex/paracortex --T-cells 3. Medulla |
|
|
Lymphoid Hyperplasia
|
-Secondary to antigenic stimulation
-Can involve many lymph nodes (systemic disease) -Can be localized to a regional lymph node draining an inflammed area -Proliferation of lymphoid follicles with active germinal centers --germinal centers expand -Produce plasma cells that secrete antibody -Increase in T-lymphocytes in paracortical areas -Sub-capsular space is expanded -Will have many different cell types in a reactive process |
|
|
Acute Lymphadenitis
|
-Neutrophils have "set up shop" in the lymph nodes and are not draining out
-Targeted inflammation of the lymph nodes -Soft, hyperemic, edema -Usually the result of a regional lymph node draining an inflammatory site |
|
|
Chronic Lymphadenitis
|
-Capsule is thick, firm, and may be fibrotic
|
|
|
Bacterial lymphadenitis
|
-Often pyogenic
-Strep equi (equine strangles) -Arcanobacterium pyrogenes (cattle and sheep) -Streptococcus porcinus (porcine jowl abscess) -Caseous lymphadenitis in sheep and goats due to Corynebacterium pseudotuberculosis -Mycobacteriosis: focal granulomatous infammation |
|
|
Viral Lymphadenitis
|
-Porcine circovirus 2
--granulomatous with basophilic inclusion bodies --FIP |
|
|
Fungal lymphadenitis
|
-Coalescing to diffuse granulomatous blastomycosis, cryptococcosis, Histoplasma
|
|
|
Protozoal lymphadenitis
|
-Leishmania
-Toxoplasma |
|
|
Metastatic neoplasia to the Lymph nodes
|
-Carcinomas metastasize to lymph nodes
--gastric, mammary, pulmonary, squamous, etc.) -Firm, enlarged lymph odes with loss of normal architecture -Malignant Melanoma -Mast cell Tumor -Some osteosarcomas |
|
|
Lymphosarcoma
|
-Diverse group of malignancies arising in lymphoid tissues
-All lymphomas are not the same, depends on which type of cell is neoplastic --Variable treatment and diagnosis -Need to know sub-type to effectively treat! -Anatomic location -Immunophenotype -Cellular morphology -Histologic pattern -Biologic behavior |
|
|
Lymphosarcoma classification system
|
1. Anatomic location:
-multicentric -Mediastinal/thymic -Cutaneous -Misc/solitary -Primary to marrow 2. Immunophenotype: -B-cell, T-cell, or none 3. Cellular morphology -cell size -Nuclear features -Numberof mitoses 4. Histologic pattern -diffuse -follicular 5. Biologic behavior -Low-grade to high-grade |
|
|
Canine Lymphosarcoma
|
-Middle-aged or older dogs
-No retroviral cause yet -Multicentric form is most common 80-85% --generalized lymph node enlargement --Splenic and hepatic involvement is common with this form --Diffuse large B-cell Lymphoma --Peripheral T-cell Lymphoma -Alimentary, thymic, and cutaneous forms are less common -Hypercalcemia is usually associated with T-cell lymphosarcoma -Can look like whatever it wants to --will bulge on cut section |
|
|
Feline Lymphosarcoma
|
-Cats do not show lymphoadenopathy
-FeLV associated lymphoma: younger cats --mediastinal and multicentric T-lymphocyte lymphoma --uncommon with vacination -Alimentary lymphoma is most common form --older cats -Miscellaneous sites are also seen in older cats -Hodgkin-like lymphosarcoma in cats older than 6 years --unilateral mandibular or cervical lymph node enlargement |
|
|
Feline Intestinal Lymphosarcoma
|
-Most common form of feline lymphoma
-Occurs in older cats -Mostly B-cell population but can also see aggressive large granular lymphomas -Small-cell lymphoma looks like inflammatory lymphocytes |
|
|
Bovine Lymphosarcoma
|
1. BLV associated lymphoma
-Occurs in superficial/abdominal lymph nodes -Retrobulbar, abomasum, heart, uterus, spleen, kidney -cows 6-8 years old 2. non-BLV associated lymphoma -Sporadic form, calf/juvenile form -Generalized lymph node enlargement and widespread visceral and bone marrow involvement |
|
|
Forms of non-BLV lymphoma
|
-Thymic form: in beef cattle 6-24 months old
-Cutaneous form: rare and in young cattle -MMulticentric form: widespread symmetric lymph nodes --also affects liver, spleen, kidneys, and maybe skeletal muscle |
|
|
Equine Lymphosarcoma
|
-Multicentric
-Alimentary -Cutaneous/subcutaneous -Most common subtype is T-cell rich large B-cell lymphoma --most common at all sites |
|
|
Pig Lymphosarcoma
|
-Frequent tumor
-Multicentric form in lymph nodes, spleen, liver, kidney, and bone marrow -Mediastinal form affects pigs less than 1 year old |
|
|
Ferrett Lymphosarcoma
|
-Diffuse peripheral lymphadenopathy with visceral spread late in the course of the disease
--Spreads to spleen, liver, kidney -Juvenile form affects large lymphocytes in the thymus, spleen, and liver --can lead to compressiong of the lung lobes, dyspnea, and pleural effusion -Immunoblastic/polymorphous form is uncommon --peripheral lymphadenopathy and visceral distribution |
|
|
Histiocytic Sarcoma
|
-Macrophage neoplasm, affects dendritic Antigen Presenting Cells
-Common in Bernese mountain dogs, rotweillers, goldens, flat-coated retrievers -Sporadically occurs in other dog breeds and cats -Can be localized or disseminated -Localized: spleen, lymph node, lung, bone marrow, skin, and subcutis are affected -Disseminated: secondary sites throughout the body --liver, lung, hilar lymph node, bone marrow |
|
|
Discoloration/Pigment of Lymph Nodes
|
-Drainage reaction: macrophages are in medullary subcapsular sinuses with RBCs, hemosiderosis, and edema
-Anthracosis can cause carbon from the lungs to drain into tracheobronchial lymph nodes -Melanin accumulation from chronic dermatitis or mandibular melanosis -Parasitic hematin with Fasciola magna or Fasciola hepatica |
|
|
Spleen Structure
|
-Smooth Muscle
-Afferent and efferent blood vessels -Red and white pulp -3 anatomic systems: --monocyte-macrophage system --lymphopoietic system --Vasculature |
|
|
Spleen Red Pulp
|
-Meshwork of reticular cells interspersed with macrophages
-RBCs from terminal arterioles enter red pulp and traverse sinuses or meshwork, then enter terminal venules -Macrophages survey RBCs and trap antigenic material from plasma -Remove foreign material, microorganisms, senescent and altered RBCs -Store mature RBCs in red pulp vascular spaces -Hematopoietic role |
|
|
Spleen White pulp
|
-Lymphocytes and macrophages
-Surround central arterioles, form Periarteriolar lymphoid sheaths (PALS) and lymphoid follicles of B-cells -Respond to an innumological demand by producing B lymphocytes and plasma cells --produce antibody and memory lymphocytes |
|
|
Splenomegaly
Bloody Spleen |
-Uniformly bloody spleen
-Congestion due to torsion or barbituate euthanasia/anesthesia -Acute hyperemia --septicemia → microbes transported to the spleen → phagocytosis by macrophages, produces a big, bloody spleen -Acute Hemolytic Anemia congests spleen --need to remove large numbers of sequestered or parasitized altered RBCs from circulation |
|
|
Splenomegaly
Meaty Spleen |
-Uniform splenomegaly with a firm consistency
-Does not lose blood when cut -Causes: --bacteria/septicemia --chronic infectious disease --prolonged hemolytic anemia --Diffuse lymphoid hyperplasia --Neoplasia --Storage material --Extra-medullary hematopoiesis |
|
|
Septicemia as a cause for meaty spleen
|
-Hyperplasia of splenic macrophages due to need to phagocytose organisms
|
|
|
Chronic hemolytic diseases as cause for meaty spleen
|
-Less hemolysis, no RBCs no bloody spleen
-May be concurrent with lymphocyte hyperplasia |
|
|
Diffuse Granulomatous disease as cause for Meaty spleen
|
-Intracellular facultative pathogens of macrophages
--Mycobacterium bovis --tubervulosis --Brucella --Francisella tularensis -Systemic mycoses --blastomyces dermatitidis --Histoplasma capsulatum --Leishmania -Some fungi may also produce nodular enlarged spleens with formation of granulomas |
|
|
Follicular Lymphoid Hyperplasia in the Spleen
|
-May chronic diseases induce an immune response resulting in follicular lymphoid hyperplasia
-Results in "meaty spleen" -Lymphoid follicles are hyperplastic |
|
|
Neoplasms and Meaty Spleen
|
-Lymphoma
-Mast cell tumor/mastocytosis -Multiple myeloma -Lymphoproliferative disease |
|
|
Stored material causing meaty spleen
|
-Lysosomal storage diseases
-Amyloid |
|
|
Extramedullary hematopoiesis
EMH |
-Hormonal or physiological mechanisms signal synthesis of progenitor cells for systemic circulation
-Splenic EMH is often incidental -Can cause meaty spleen |
|
|
Splenic Nodules with Bloody Consistency
|
1. Hematoma
2. Hematoma induced by nodular lymphoid hyperplasia --blood pools and grows into a hematoma 3. Hemangiosarcoma All look the same |
|
|
Splenic Nodules with a Firm consistency
|
1. Focal nodular lymphoid follicular hyperplasia
2. Granuloma (mycobacterium) 3. Abscesses --strep --rhodococcus --arcanobacterium --corynebacterium 4. Neoplasms |
|
|
Neoplasia causing form splenic nodules
|
Primary:
-Lymphoma -Histiocytic sarcoma -Fibrohistiocytic nodules/complex nodular hyperplasia -Leiomyosarcoma -fibrosarcoma -undifferentiated sarcomas Metastatic sarcomas and carcinomas can seed in the spleen |
|
|
Primary tumors in the Spleen
|
1. Leiomyosarcoma
2. Fibrosarcoma 3. Lymphosarcoma |
|
|
Small Spleens
|
-Hypoplasia and atrophy
-Not common -Developmental cause: immunodeficiency diseases -Atrophy due to aging or wasting diseases -Contraction of the spleen |
|
|
Splenic Choristoma
|
-Benign nodular hyperplasia of the spleen
-If developmental, presence of normal tissue at an abnormal site --"daughter spleens" -Can also be acquired through traumatic splenic rupture --splenosis |
|
|
Siderofibrotic plaques on the spleen
|
-Gray/tan plaques on splenic capsule
-Accumulation of Iron/hematoiden and calcium -Common incidental finding in aged dogs -Usually occur along the marginal surface of the spleen |
|
|
Splenic Infarct
|
-Wedge-shaped regions of spleen
-red/black in color are acute -tan are chronic |
|
|
Pathology of the Tonsil
|
1. Lymphoid depletion
--occurs with viral infections that cause immunosuppression 2. Inflammation --only primary or hematogenous infections, no afferent lymphatics to bring stuff in --necrotizing tonsilitis 3. Inflammatory polyps (old dogs) 4. Neoplasia --only primary neoplasms, no afferent lymphatics --Squamous cell carcinoma, lymphoma, melanoma |
|
|
Primary Immunodeficiency Diseases
|
-Genetic causes
-Generally uncommon -Break in somewhere maturation cascarde from stem cell to mature cell -Lots of cross-talk in maturation process -Severe Combined Immunodeficiency (SCID) -Agammaglobulinemia -Selective immunoglobulin deficiencies -Leukocyte adhesion deficiency -Complement deficiencies |
|
|
Severe Combined Immunodeficiency in Horses
Equine SCID |
-Autosomal recessive trait
-Expressed as an absence of functional B and T lymphocytes -Defect in the catalytic subunit of DNA-dependent protein kinase --enzyme is required for receptor gene rearrangements for B and T cell maturation --no maturation of B and T cells -About 10 days old animal develops diarrhea and pneumonia -Adenovirus, cryptosporidium parvum, pneumocystis carinii are common pathogens -Affected foals die before 5 months old -Hypoplasia of the thymus, spleen, and lymph nodes |
|
|
Severe Combined Immunodeficiency in Bassett Hounds
Canine SCID |
-Mutation in gene encoding common gamma subunit of IL-2, IL-4, IL-7, IL-9, IL-15
-T-cells are unable to bind and respond to IL-2 -B-cells are unable to class switching, no IgG formed -Animal does not grow normally and has increased susceptibility to infection -Very small thymus with unidentifiable lymph nodes and tonsils -X-linked (X-SCID) |
|
|
SCID in Corgis and Jack Russell Terriers
|
-Autosomal recessive disorder instead of mutation
-Corgis have similar disease as bassetts -Jack Russell's have mutation in DNA-Protein kinases similar to Arabian horses |
|
|
Acquired Immunodeficiencies
|
-Much more common, occur for many more reasons
-Pregnancy, aging, malnutrition -Toxins (PCBs, Iodine, lead, Cadmium, methylmercury, DDT) -Drugs (corticosteroids, chemotherapeutic agents) -FeLV -FIV -Parvovirus |

