![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Chemical mediators of inflammation - main headings.
|
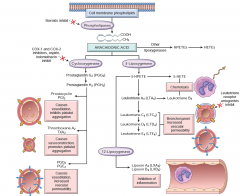
01 Vasoactive amines 02 Arachidonic acid metabolites 03 Leukotrienes 04 Lipoxins. 05 Cytokines 06 Chemokines 07 Complement system 08 Other mediators:i) Platelet activating factor ii) Products of coagulation. iii) Kinins. iv) Neuropeptides. |
|
|
|
Histamine - preformed or de novo synthesized
|
Preformed
|
|
|
|
Histamine - vessel specific actions? |
Dilatation of arterioles and increased permeability of venules
|
|
|
|
role of lipoxins in inflammation
|
1. inhibition of inflammatory response 2. Suppression of the PMN chemotaxis. |
|
|
|
Characteristic feature of synthesis of lipoxins
|
Transcellular synthesis of lipoxins with two cell populations. PMN produces the intermediates. The lipoxins are produced by the interaction of platelets with the leucocytes. |
|
|
|
role of cytokines in inflammation
|

|
|
|
|
which interleukin is responsible for TH17 response
|
IL-1 |
|
|
|
Inflammasome is associated with which interleukin
|
IL-1
|
|
|
|
chemokines and their groups
|
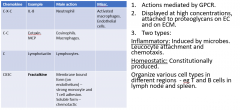
|
|
|
|
IL-6 - main role
|
Primary cytokine responsible for the liver synthesis of APR - coagulation factors, ferritin, CRP. Antagnosists developed. |
|
|
|
ways to activate complement
|
1. antigen antibody complex acting on c1. 2. Mannose residues on microbes reacting with MBLs, leading to activation of C3 convertase. 3. Alternative pathway - direct activation of C3 convertase by bacterial surface LPS, snake venom etc. |
|
|
|
Role of complement products
|
C3a and C5a - anaphylotoxins - histamine release by mast cells. C3b - opsonin. MAC - cell lysis. C5a - chemotaxis and LOX activation. |
|
|
|
cause of hereditary angioedema
|
Deficiency of C1 INH.
|
|
|
|
Role of DAF and CD59
|
DAF - cleaves C3 convertase. CD59 - inhibits MAC formation. |
|
|
|
Pathophysiology of PNH |
DAF and CD59 present on the cell surface, and linked by GPI anchor. Deficiency of this anchor. |
|
|
|
Which infections common in MAC deficiency
|
Niesserial infections.
|
|
|
|
WHy neisserial infections common in MAC deficiency?
|
MAC - increased permeability, especially in organisms with thin walls. Neisseria have thin walls.
|
|
|
|
role of IL-17
|
in acute inflammation. recruitment of neutrophils and monocytes. |
|
|
|
principal mediators causing vasodilatation
|
1. Histamine. 2. Prostaglandins - PGI2 and others. bradykinin substance P |
|
|
|
Increased vascular permeability
|
1. Histamine and Serotonin. 2. C3a and C5a. 3. LTC4, LTD4, LTE4 PGD2 and E2. Bradykinin. Substance P |
|
|
|
Chemotaxis, leucocyte recruitment and activation. |
1. TNF and IL-1. 2. Chemokines. 3. C3a and C5a. 4. LTB4. |
|
|
|
Fever
|
1. IL-1 and TNF 2. Prostaglandins - PGE2. |
|
|
|
Pain
|
1. Prostaglandin - PGE2. 2. Bradykinin. |
|
|
|
morphology of inflammation caused by viral pleuritis
|
serous.
|
not fibrinous.
|
|
|
exam : headings - morphology of acute inflammation
|
Hallmarks. Serous Fibrinous Purulent - abscess. Pseudomembranous Ulcer |
|
|
|
FCmu Morphological hallmark of acute inflamation |
Increased vascular permeability. Increased leucocytes and edema fluid accumulation in the ECM. |
|
|
|
Cm Concept of serous inflammation. |
The increase in P is not that much. Hence it is a cell poor exudate. Fibrinogen cannot come out. Hence no fibrin. Two causes of exudate - 1. from plasma - d/t increased P 2. increased mesothelial secretion - d/t irritation. |
|
|
|
Concept of fibrinous inflammation
|
FIbrin comes out becauseof increased P. Two causes - 1. increased P. 2. Local presence of procoagulant substance e.g cancer cells |
|
|
|
Cm How does an opaque scar fibrous thickening develop in fibrinous pericarditis |
Long standing fibrin - ingrowth of fibroblasts and blood vessels - so threads become dense due to collagen. Hence opacification.
|
|
|
|
Cmu Purulent inflammation |
Inflammation associated with formation of pus. Pus - exudate with neutrophils, edema fluid and necrotic liquefied cellular debris. |
|
|
|
Cmu Cause of purulent inflammation |
organisms causing liquefactive necrosis i.e. organisms which recruit inflammatory cells and then these cells release their enzymes and destroy the organisms and tissue cells - unlike coagulative necrosis. Hence pus.
|
|
|
|
Cmu Abscess definition |
Localized collection of purulent inflammatory tissue due to suppuration buried in a tissue, organ or a confined space. Cause - seeding of pyogenic bacteria in a tissue. |
|
|
|
Cm Morphology of an abscess |

|
|
|
|
Fm Define chronic inflammation |
Response of prolonged duration (weeks or months). Inflammation, tissue injury and attempts at repair co-exist, in varying combination. |
|
|
|
Fm causes of chronic inflammation |
(1) Persistent infection (2) Hypersensitivity reactions – excessive and inappropriate immune system activation. (3) Prolonged exposure to potentially toxic agents – exogenous or endogenous. (4) Diseases in which chronic inflammation is implicated in pathogenesis – e.g. DM. |
|
|
|
Cm resident macrophages are derived from? |
Early progenitors in the yolk sac and fetal liver.
|
|
|
|
Fmu Blood monocyte recruitment and conversion to macrophages occurs where |
1. site of inflammation. 2. skin. 3. intestine. |
|
|
|
Fmu How are tissue macrophages replenished? |
By the proliferation of surrounding resident tissue macrophages. |
|
|
|
Fmu
Half life of monocyte and macrophage |
Monocyte - 1 day macrophage- months to years |
|
|
|
fmu pathways of activation of macrophages |
classical - pro inflammatory alternate - anti inflammatory |
|
|
|
fmu which cytokines activate classical pathway of macrophage |
IFN gamma, produced by TH1 cells.
|
|
|
|
fmu Alternate macrophage activation, which cytokines |
IL4, IL13 Produced by TH2 macrophages. |
|
|
|
fmu cytokines secreted by classically activated macrophages |
IL1 TNF IL12 IL23 |
1, 12, 23 1 and TNF recruit neutrophils. 12 again activates T lymphocytes. |
|
|
fmu cytokines secreted by alternatively activated macrophages |
TGF beta. IL10 |
anti inflammatory and repair effects.
|
|
|
cfmu Which class of T cells can control the nature of inflammatory reaction |
CD4+ T cells, by the cytokines they secrete.
|
|
|
|
cfmu Subtypes of CD3+ TH cells with cytokines secreted |
TH1 - IFN gamma - macrophage activation, classical. TH2 - IL4, IL13 - macrophage activation, alternate. IL5 - eosinophils. TH17 - IL17 and other cytokines - PMN and monocyte recruitment. |
|
|
|
fmu what is a tertiary lymphoid organ |
clustering of lymphocytes, APCs and plasma cells at site of inflammation. synovium in RA. Thyroid in Hashimoto |
|
|
|
Neutrophils in chronic inflammation, examples
|
chronic bacterial infection of synovium. lung - smoking. |
|
|
|
fmu two types of granulomas with difference between the two |
Immune granuloma - t cell activation dependent. Foreign body granuloma. |
|
|
|
fm Cat-scratch granuloma - characteristic |
Presence of neutrophils. Steellate granulomas |
|
|
|
fm syphilitic granuloma - features |
Plasma cells. central necrotic cells WITHOUT loss of cellular outlines |
Perhaps coagulative necrosis.
|
|
|
fmu Which cytokine causes release of CRP and fibrinogen |
IL 6.
|
|
|
|
fmu Basis of ESR in inflammation |
Fibrinogen is APR. Can form rouleaux by trapping RBC. Hence increased ESR. |
|
|
|
cm CRP and SAA - role in inflammation |
opsonisation and complement fixation. binding to chromatin - clearing of nuclear debris. |
|
|
|
cfmu APR responsible for anemia of chronic disease |
Hepcidin.
|
|
|
|
cm cause of left shift in inflammation |
the post mitotic reserved pool is released first and then there is proliferation of cells in BM.
|
|
|
|
causes of leucopenia. name 2
|
Typhoid fever. Rickettsial infection. |
|
|
|
systemic effects of inflammation
|
1. fever 2. APR 3. Leucocytosis. 4. septic shock |
|
|
|
|
|
|

