![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
154 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Right to left shunts |
1- Truncus arteriosus 2- Transposition of great artery (2 artery) 3- Tricuspid atresia (Tri) 4- Tetralogy of fallot (tetra) 5- TAPVR |
|
|
|
Persistent Truncus arteriosus |
1- Truncus arteriosus fail to divide into ascending aorta and pulmonary trunk due to failure of formation of aorticopulmonary septum 2- Most patients have VSD |
|
|
|
Transposition of great artery |
1- Aorta leaves RV (anterior) and pulmonary trunk leaves LV (posterior)- separation of systemic and pulmonary circular 2- Due to failure of aorticopulmonary septum to spiral 3- Not comparable with life unless a shunt is present to allow mixing of blood (VSD, PDA or patent foreamen ovale) 4- Without surgical intervention most infants die within the first few months of life |
|
|
|
Tricuspid atresia |
1- Absent of tricuspid valve and RV hypotrophy 2- Require VSD and ASD for viability |
|
|
|
Tetralogy of fallot |
1- Anterior superior displacement of infundibular septum 2- Most common cause of early childhood cyanosis 3- 4 component 1- VSD 2- Pulmonary stenosis ( most important determinant of prognosis) 3- RV hypertrophy 4- Over riding aorta 4- Tets spells cause by crying, fever, exercise due to exacerbation of RV outflow obstruction |
|
|
|
Total anomalous pulmonary venous return TAPVR |
1- Pulmonary vein drain into right heart circulation 2- Require ASD or PDA for viability |
|
|
|
Ebstein anamoly |
1- Displacement of tricuspid valve leaflet into RV 2- Associated with 1- Tricuspid regurgitation 2- Accessory conduction pathways 3- Right sided HF |
|
|
|
Left to right shunt |
1- Acynotic VSD ASD PDA |
|
|
|
Ventricular septal defect VSD |
1- Asymptomatic at birth may manifest weeks later or remain asymptomatic throughout life 2- Most self resolve 3- Larger lesions May lead to LV overload and HF 4- O2 saturation increase RV and pulmonary artery |
|
|
|
Atrial septal defect ASD |
1- Defect in interatrial septum 2- Wide fixed split S2 systolic murmur heard at pulmonary area 3- Ostium secundum defects most common and usually an isolated finding 4- Osium primum defects rarer and usually occur with other cardiac anomalies 5- Symptoms ranges from none to HF 6- Distint from Patent Foramen Ovale in that septa are missing tissue rather thank unfused 7- Oxygen saturation increase in RA, RV and pulmonary artery 8- May lead to paradoxical emboli (systemic venous emboli use ASD to bypass lungs and become systemic atrial emboli 9- Associated with Down syndrome |
|
|
|
Patent ductus arterious |
1- In fetal period, shunt is right to left 2- In neonatal period decrease pulmonary vascular resistance - shunt becomes left to right - progressive RVH and/or LVH and HF 3- Associated with continuous machinery murmur 4- Patency is maintained by PGE synthesis and low O2 tension 5- Uncorrected PDA can eventually result in late cyanosis in lower extremities differential cyanosis 6- PDA normal in uterus and closes after first breath |
|
|
|
Eisenmenger syndrome |
1- Uncontrolled left to right shunt (VSD, ASD,PDA) - increase pulmonary blood flow - pathologic remodeling of Vasculature- Pulmonary artery hypertension 2- RVH occurs to compensate- Shunt becomes right to left 3- Causes late cyanosis, clubbing and polycythemia 5- Age of onset varies |
|
|
|
Coarctation of the aorta |
1- Narrowing if the aorta near intersection of Ductus arteriosus 2- Associated with bicuspid aortic valve, other heart defect and Turner syndrome 3- Hypertension in upper extremities and weak delayed pulse in lower extremities (radio-femoral delay) 4- With age, intercostal arteries enlarge due to collateral circulation, arteries erode ribs- notched appearance on CXR 5- Complication 1- Berry aneurysm 2- Aortic rupture 3- Endocarditis |
|
|

Diagnosis |
Tetralogy of fallot Boot shaped heart due to RV hypertrophy |
|
|
|
What is the structural difference between ASD and PDA |
In ASD the septal tissue is missing in PDA septal tissue there but not fused |
|
|
|
What drug when taken during pregnancy cause tricuspid regurgitation and attialization of the right ventricle in a newborn |
Lithium |
|
|
|
What is the most common cause of cyanosis heart disease in children |
Tetralogy of fallot |
|
|
|
What is the common finding on chest X-ray for infants with transposition of great artery |
Egg on a string |
|
|
|
Why patients squat in tetralogy of fallot |
Increase systemic vascular resistance decrease right to left shunt |
|
|
|
Name a congenital heart disease and genetic disease associated with coarctation of the aorta |
1- Bicuspid aortic valve 2- Tuner syndrome |
|
|
|
X ray finding in coarctation of aorta |
Notched ribs due to collateral circulation enlarging the intercostal arteries and eroding b the ribs |
|
|
|
Describe the progression of small VSD in children |
1- Most are asymptomatic at birth and may manifest weeks later or remain asymptomatic 2- Majority eventually resolve |
|
|
|
What congenital abnormality associated with tetralogy of fallot is characterized by frequent infections developmental delay and cleft palate |
DiGeorge syndrome |
|
|
|
Congenital anomalies with Alcohol exposure in uterus |
1- VSD 2- ASD 3- PDA 4- Tetralogy of fallot |
|
|
|
Congenital anomalies with congenital rubella |
1- PDA 2- Pulmonary artery stenosis 3- Septal defect |
|
|
|
Congenital anomalies with Down’s syndrome |
1- AV septal defect (Endocardial cushion) 2- ASD 3- VSD |
|
|
|
Congenital anomalies with infants of diabetic mother |
1- Transposition of great artery 2- VSD |
|
|
|
Congenital anomalies with Marfan syndrome |
1- Mitral valve prolapse 2- Thoracic artery aneurysm/dissection 3- Aortic regurgitation |
|
|
|
Congenital anomalies with lithium exposure |
Ebstein anamoly |
|
|
|
Congenital anomalies with Turner syndrome |
1- Bicuspid Heart valve 2- Coarctation of aorta |
|
|
|
Congenital anomalies with Williams syndrome |
Supravalvular aortic stenosis |
|
|
|
Congenital anomalies with DiGeorge syndrome |
1- Tetralogy of fallot 2- Truncus arteriosus |
|
|
|
Hypertension |
Persistent BP > 130/80 |
|
|
|
Hypertension |
Persistent BP > 130/80 |
|
|
|
Risk factor for hypertension |
Modifiable 1- Obesity 2- Lack of physical activity 3- Excess salt intake 4- Excess alcohol use 5- Smoking Non modifiable 1- Age 2- DM 3- Family history 4- African American > Caucasian> Asian
|
|
|
|
Features of hypertension primary vs second |
1- 90% of Hypertension is primary/essential 2- 10% secondary due to 1- renal artery stenosis 2- Fibromuacular dysplasia 3- Primary hyperaldosterone syndrome (Conns syndrome) |
|
|
|
Features of hypertension primary vs second |
1- 90% of Hypertension is primary/essential 2- 10% secondary due to 1- renal artery stenosis 2- Fibromuacular dysplasia 3- Primary hyperaldosterone syndrome (Conns syndrome) |
|
|
|
Hypertensive urgency |
BP > 180/120 without end organ damage |
|
|
|
Features of hypertension primary vs second |
1- 90% of Hypertension is primary/essential 2- 10% secondary due to 1- renal artery stenosis 2- Fibromuacular dysplasia 3- Primary hyperaldosterone syndrome (Conns syndrome) |
|
|
|
Hypertensive urgency |
BP > 180/120 without end organ damage |
|
|
|
Hypertensive emergency |
BP > 180/120 with end organ damage Stroke Encephalopathy Retinal hemorrhage Retinal Exudate Papilloedema MI HF Aortic dissection Kidney injury Microangiopathic hemolytic anemia Eclampsia |
|
|
|
Hypertension leads to |
1- Stroke 2- Encephalopathy 3- Retinopathy 4- CAD 5- HF 6- LVH 7- atrial fibrillation 8- Aortic dissection 9- Aortic aneurysm 10- CKD |
|
|
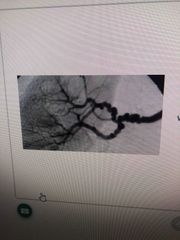
Diagnosis |
Fibromuscular dysplasia String of beads |
|
|
|
What 3 fundoscopic findings be seen in a patient with hypertensive emergency |
1- Retinal exudate 2- Retinal hemorrhage 3- Pappiloedema |
|
|
|
Hyperlipidemia signs |
1- Xanthelasma - lipid deposit on eyelids 2- Tendinous xanthoma - Lipid deposit in tendons especially archillis 3- Corneal arcus - 1- Lipid deposit in cornea 2- Common in elderly (arcus senilis ) |
|
|
|
Arteriosclerosis |
1- Hardening of artery with arterial wall thickening and loss of elasticity |
|
|
|
Arteriolosclerosis |
1- Affect small arteries and arterioles 2- Two types Hyaline - Thickening of vessel wall 2 plasma protein leaking into endothelium in essential hypertension and diabetis Hyper plastic (onion skinning) - Severe hypertension with proliferation of smooth muscle cell |
|
|
|
Monckeberg sclerosis (median calcification sclerosis) |
1- Uncommon 2- Affect medium arteries 3- Calcification of internal elastic lamina and media of artery 4- Vascular stiffness without obstruction 5- Pipestem appearance on X-ray 6- Do not cause obstruction because it does not involve the intima |
|
|
|
Atherosclerosis |
1- Common 2- Affect all arteries and cause buildup of cholesterol plaque in intima |
|
|
|
Atherosclerosis |
1- Common 2- Affect all arteries and cause buildup of cholesterol plaque in intima |
|
|
|
Location of atherosclerosis |
1- Abdominal aorta 2- Coronary artery 3- Popliteal artery 4- Carotid artery 5- Circle of Willis |
A CoPy Cat name Willis |
|
|
Risk factor for atherosclerosis |
Modifiable 1- Smoking 2- Hypertension 3- Diabetes Mellitus 4- Dyslipidemia Non modifiable 1- Age 2- Sex (male and post menopausal women) 3- Family history |
|
|
|
Symptoms of atherosclerosis |
1- Angina 2- Claudication 3- Stroke 4- Asymptomatic |
|
|
|
Pathophysiology of atherosclerosis |
Inflammatory process 1- Endothelia cell dysfunction 2- Macrophages and LDL accumulate 3- Foam cells 4- Fatty streak 5- Smooth muscle cell migrate (PDGF and FGF) proliferation and extracellular matrix deposition 6- Fibrous plaque 7- Complex arthroma 8- Calcification |
|
|
|
How does menopause affect atherosclerosis |
Post menopausal women more at risk because of decrease estrogen which is protective |
|
|
|
Traumatic aortic rupture |
1- Occurs after trauma or decelerating injury 2- Affect aortic isthmus ( proximal descending aorta just distal to the origins of subclavian artery) 3- CXR- widen mediastinum |
|
|
|
Aortic aneurysms |
1- Dilation of aorta 2- Associated with abdominal pain +/- back pain suggest leaking, dissection or rupture |
|
|
|
Abdominal aortic aneurysms |
1- Due to atherosclerosis 2- Risk factor modifiable 1- smoking 2- HTN 3- DM 4- Dyslipidemia Non- modifiable 1- Age 2- Sex 3- Family Hx 3- Presents with palpable pulsatile abdominal mass 4- Most often infra-renal (no vasa vasorum g |
|
|
|
Thoracic aorta aneurysms |
1- Due to cystic media degeneration 2- Risk factor 1- Bicuspid aortic valve 2- Marfan syndrome, Ehlers Danlos 3- Associated with tertiary syphillis (obliterated endaritis of vasa vasorum) 4- Aortic root dilation leads to aortic regurgitation |
|
|
|
What acquired condition is an important risk factor for developing thoracic aortic aneurysm |
Hypertension |
|
|
|
ECG localization of STEMI |
Anterioseptal (LAD)- V1-V2 Anterioapical (distal LAD)- V3-V5 Anteriorlateral (LAD and LCX) - V5-V6 Lateral (LCX)- lead I, aVL Inferior (RCA) - lead I, II, aVF Posterior (PDA) - V7-V9 |
|
|
|
What is the name of the accessory pathway in Wolff parkinson white syndrome |
Bundle of Kent |
|
|
|
Pathophysiology of brugada syndrome |
Na channel loss of function |
|
|
|
Paroxysmal supraventricular tachycardia |
1- Narrow QRS complex 2- Due to AV nodal re-entry circuit 3- Symptoms 1- Sudden onset palpitation 2- Diaphoresis 3- Lightheadedness 4- Treatment 1- Terminate AV node conduction (vagal stimulation, IV adenosine) 2- Cardioversion if unstable 3- Catheter ablation |
|
|
|
What region is targeted in atrial flutter |
Between tricuspid valve and inferior vena cava |
|
|
|
Subclavian steal syndrome |
1- Stenosis of subclavian artery proximal to origin of vertebral artery 2- Hypoperfusion distal to stenosis 3- Reversed shutting of blood to the ipsilateral vertebral artery 4- Decrease Cerebral perfusion with exertion of affected arm 5- Cause 1- Arm ischemia 2- Pain 3- Paraesthesia 4- vertibrobasillar insufficiency 4- >15mmHg difference in systolic pressure between arms 6- Associated with 1- arteriosclerosis 2- Takaysau artritis 3- Heart surgery |
|
|
|
Aortic dissection |
1- Longitudinal intimal tear creating a false lumen 2- Cause 1- Hypertension 2- Bicuspid aortic valve 3- Marfan 3- Symptom 1- Sudden onset tearing chest pain that radiates to the back +/- unequal BP 4- CXR- widen mediastinum 5- Can cause 1- Organ ischemia 2- Aortic rupture 3- Death 6- Two types Stanford type A - 1- Involve ascending aorta can extend into the aortic arch and descending aorta 2- May result in aortic regurgitation and cardiac tamponad 3- Treatment- surgery Stanford type B- 1- only descending aorta (below left subclavian artery) 2- Treatment Beta blocker then vasodilation
|
|
|
|
Stable angina |
1- Chest pain in exertion relieve with rest 2- Cause by atherosclerosis when 70% of artery is occluded 3- Treat rest and vasodilators 4- ECG- ST depression not elevated biomarker |
|
|
|
Vasospastic/ Prinzmatal angina |
1- Chest pain due to coronary artery vasospasm 2- Cause by smoking (hypertension and Hyperlipidemia not risk factor) worst with cocain tobacco and triptan 3- Treat - Smoking cessation, Ca channel blockers, vasodilators 4- ECG - no change but could have ST elevation no elevation in cardiac bio markers |
|
|
|
Unstable angina |
1- Chest pain at rest 2- Thrombosis with incomplete coronary artery occlusion 3- Treat vasodilators 4- ECG ST depression T wave inversion no elevation in cardiac bio markers |
|
|
|
Coronary steal syndrome |
1- Stenosis of coronary artery causing dilation of normal vessels distally 2- Administration of vasodilator cause dilation of normal vessels — Shunting of blood to well perfumed area - ischemic myocardium perfumed by stenosed vessels |
|
|
|
Sudden cardiac death |
1- Death wishing 1 hour of cardiac symptoms most commonly due to lethal arrhythmia (V.fib) 2- Can be due to Coronary heart disease, Cardiomyopathy and congenital heart disease (long QT syndrome, brugada) 3- Treat with CPR and Implantable cardioverter defibrillator |
|
|
|
Chronic ischemic heart disease |
Progressive onset of HF due to chronic ischemic myocardial damage |
|
|
|
Myocardial infarction |
1- Most often due to atherosclerotic plaques rupture - acute thrombosis 2- ST elevation of depression with elevation of cardiac biomarker 3- ST depression 1- Subendicardial infarct 2- ST depression on ECG 4- ST elevation 1- Transmural 2- Fullthickness myocardium involved 3- ST elevation and Pathological Q waves on ECG |
|
|
|
2 vasodilator that can trigger coronary steal syndrome when administered |
Dipyridamole Regadenoson |
|
|
|
Myocardial hibernation |
Potentially reversible left ventricular systolic dysfunction in the presence of chronic ischemia |
|
|
|
Myocardial stunning |
Transient left ventricular systolic dysfunction following a brief period of acute ischemia |
|
|
|
0-24 hours after MI |
1- Dark mottling (pale with tetrazolium) 2- Early Coagulative necrosis 1- Cell contents leak in blood causing edema, hemorrhage and wavy fibers 2- Reperfusion - Increase free radicals and Ca influx - hypercontraction of myofibrils (dark eosinophilic stripes) 3- Complication 1- Ventricular arrhythmia 2- Cardiogenic shock 3- HF |
|
|
|
1-3 days after MI |
1- Hyperemia 2- Extensive Coagulative necrosis release neutrophils 3- Complication 1- Fibrinous pericarditis |
|
|
|
3- 14 days after MI |
1- Hyperemic borders with centers of yellow brown softening 2- Release macrophages 3- Complication 1- Rupture of fee wall- Tamponade 2- Rupture of papillary muscle - mitral regurgitation 3- Rupture of interventricular septum- Left to right shunt 4- Pseudo-aneurysm |
|
|
|
3- 14 days after MI |
1- Hyperemic borders with centers of yellow brown softening 2- Release macrophages 3- Complication 1- Rupture of fee wall- Tamponade 2- Rupture of papillary muscle - mitral regurgitation 3- Rupture of interventricular septum- Left to right shunt 4- Pseudo-aneurysm |
|
|
|
2 weeks- months after MI |
1- Grey white scar 2- Contracted scar tissue 3- Complication 1- Dressler syndrome 2- Ventricular arrhythmia 3- True ventricular aneurysm ( risk of mural thrombus) 4- HF |
|
|
|
Which 3 coronary arteries are most likely to be occluded during a myocardial infarction |
LAD > RCA> LCX |
|
|
|
Diagnosis of myocardial infarction |
1- In the first 6 hours ECG gold standard 2- Troponin I 1- Rises in 4hrs 2- Peaks at 24hrs 3- Remain elevated for 7-10 days 3- CKMB 1- Rises in 6-12 hr 2- peaks at 16-24 hrs 3- Also found in skeletal muscle 4- Helps determine reinfarction after acute MI levels return to normal after 48 hrs 4- Large MI have greater elevation of bio markers 5- ECG changes 1- ST elevation (transmural) 2- ST depression (subendicardial) 3- Hyperacute T waves 4- Inverted T waves 5- New LBBB 6- Pathological Q wave 7- Poor R wave progression (evolving or old transmural infarct) |
|
|
|
What might pathologic Q waves and poor R wave progression suggest |
Old or evolving transmural infarction |
|
|
|
What 4 causes of left ventricular failure and pulmonary edema after MI |
1- Tamponade 2- Mitral regurgitation 3- VSD 4- Left ventricular infarction |
|
|
|
What are 2 protective factors against ventricular free wall rupture (Tamponade) after MI |
1- Previous myocardial infarction 2- LV hypertrophy |
|
|
|
What is the most important step in the management of an ST elevation myocardial infarction |
Reperfusion therapy (percutaneous coronary intervention) |
|
|
|
What are 2 medications for immediate symptom control of unstable angina |
Morphine Nitroglycerins |
|
|
|
What are the 5 standard treatment for unstable angina and non-ST elevation myocardial infarction |
1- Anticoagulant (eg heparin) 2- Antiplatelet (Aspirin and ADP receptor inhibitor) 3- ACEi 4- Beta blocker 2- Statins |
|
|
|
Dilated cardiomyopathy |
1- Most common (90%) 2- Can be idiopathic or familial.(mutation of TTN gene) 3- Other causes 1- Drugs (alcohol, cocaine and doxyrunicin) 2- Infection (Coxsackie B, Trypanosoma cruzi) 3- Metabolic (Hemochromatosis, Sarcoidosis, thyrotoxicisis, wet beri beri) 4- Postpartum cardiomyopathy 4- Symptoms 1- HF, S3, systolic regurgitation, 5- Treatment same as Herat failure 6- Causes systolic dysfunction 7- Can cause eccentric hypertrophy (Sarcoptes added in series) 8- Takotsubo syndrome - heartbreak syndrome due to increase sympathetic stimulation (apical ballooning of the heart) |
|
|
|
Hypertrophic cardiomyopathy |
1- 60-70% can be familial or autoimmune (mutation of myosin’s binding protein of beta myosin heavy chain) 2- Causes syncope and SCD in young athletes due to ventricular arrhythmia 3- Physiology 1- Asymmetric septal hypertrophy and systolic anterior motion of mitral valve 2- Outflow obstruction 3- Dyspnea and possible syncope 4- Symptoms - SF, Systolic murmur, mitral regurgitation 5- Treatment 1- Cessation of high intense activity 2- Beta blocker 3- Non-dihydropyridine Ca blocker 6- Cause diastolic dysfunction 7- Can cause concentric hypertrophy (sacraments added in Parallel) 8- Other cause of concentric hypertrophy 1- Chronic hypertension 2- Friedreich ataxia |
|
|
|
Hypertrophic cardiomyopathy |
1- 60-70% can be familial or autoimmune (mutation of myosin’s binding protein of beta myosin heavy chain) 2- Causes syncope and SCD following exercise in young athletes due to ventricular arrhythmia 3- Physiology 1- Asymmetric septal hypertrophy and systolic anterior motion of mitral valve 2- Outflow obstruction 3- Dyspnea and possible syncope 4- Symptoms - SF, Systolic murmur, mitral regurgitation 5- Treatment 1- Cessation of high intense activity 2- Implantable cardioverter defibrillator 3- Beta blocker 4- Non-dihydropyridine Ca blocker 6- Cause diastolic dysfunction 7- Can cause concentric hypertrophy (sacraments added in Parallel) 8- Other cause of concentric hypertrophy 1- Chronic hypertension 2- Friedreich ataxia |
|
|
|
Restrictive cardiomyopathy |
1- Causes 1- Post radiation fibrosis 2- Loffler endocarditis 3- Endocardial fibroelastsis 4- Amyloidosis 5- Sarcoidosis 6- Hemochromatosis 2- Cause diastolic dysfunction 3- Can see low voltage ECG dispute thick myocardium 4- Loffler endocarditis - Associated with hyper eosinophils syndrome histology eosinophils infiltrate in myocardium |
|
|
|
Endocardial fibroelastasis |
Thick fibroelastic tissue in endocardium |
|
|
|
What is the mode of inheritance in Hypertrophic cardiomyopathy |
Autosomal dominant |
|
|
|
What cardiomyopathy is seen with Friedrich ataxia |
Hypertrophic cardiomyopathy |
|
|
|
What are the 5 medication use to treat Dilated cardiomyopathy |
1- ACE inhibitor 2- Beta blocker 3- Digoxin 4- Diuretic 5- Mineralocorticoid |
|
|
|
Heart failure |
1- Cardiac output insufficiency to meet the needs of the body 2- Symptoms 1- Dyspnea 2- Orthopnea 3- PNA 4- Fatigue Signs 1- Crackles 2- Elevated JVP 3- Hepatomegaly 4- Peripheral edema 3- Diastolic dysfunction 1- Persevered EF 2- Normal EDV 3- Secondary to myocardial hypertrophy 4- Systolic dysfunction 1- Reduced EF 2- Increase EDV 3- Secondary to ischemia/ MI or dilated cardiomyopathy 5- RHF as a result of LHF 6- ACE inhibitors, Angiotensin II receptor blockers, beta blocker and spironolacton decrease morbidly and mortality 7- Loop and thiazide diuretic help with symptoms 8- Hydralazine and nitrates help with mortality and symptoms
|
|
|
|
Heart failure |
1- Cardiac output insufficiency to meet the needs of the body 2- Symptoms 1- Dyspnea 2- Orthopnea 3- PNA 4- Fatigue Signs 1- Crackles 2- Elevated JVP 3- Hepatomegaly 4- Peripheral edema 3- Diastolic dysfunction 1- Persevered EF 2- Normal EDV 3- Secondary to myocardial hypertrophy 4- Systolic dysfunction 1- Reduced EF 2- Increase EDV 3- Secondary to ischemia/ MI or dilated cardiomyopathy 5- RHF as a result of LHF 6- ACE inhibitors, Angiotensin II receptor blockers, beta blocker and spironolacton decrease morbidly and mortality 7- Loop and thiazide diuretic help with symptoms 8- Hydralazine and nitrates help with mortality and symptoms
|
|
|
|
Left sided heart failure |
Orthopnea - 1- SOB when lying flat 2- Increase venous return Paroxysmal nocturnal Dyspnea- 1- SOB waking you up from sleep 2- Increase venous return Pulmonary edema 1- Increase pulmonary venous pressure 2- Increase Pulmonary venous distention 3- Transudation of fluid 4- Histology Hemosederin laden macrophages in lungs |
|
|
|
Heart failure |
1- Cardiac output insufficiency to meet the needs of the body 2- Symptoms 1- Dyspnea 2- Orthopnea 3- PNA 4- Fatigue Signs 1- Crackles and S3 2- Elevated JVP 3- Hepatomegaly 4- Peripheral edema 3- Diastolic dysfunction 1- Persevered EF 2- Normal EDV 3- Secondary to myocardial hypertrophy 4- Systolic dysfunction 1- Reduced EF 2- Increase EDV 3- Secondary to ischemia/ MI or dilated cardiomyopathy 5- RHF as a result of LHF 6- ACE inhibitors, Angiotensin II receptor blockers, beta blocker and spironolacton decrease morbidly and mortality 7- Loop and thiazide diuretic help with symptoms 8- Hydralazine and nitrates help with mortality and symptoms
|
|
|
|
Left sided heart failure |
Orthopnea - 1- SOB when lying flat 2- Increase venous return Paroxysmal nocturnal Dyspnea- 1- SOB waking you up from sleep 2- Increase venous return Pulmonary edema 1- Increase pulmonary venous pressure 2- Increase Pulmonary venous distention 3- Transudation of fluid 4- Histology Hemosederin laden macrophages in lungs |
|
|
|
Right heart failure |
Hepatomegaly 1- Venous congestion due to increase venous pressure 2- Nutmeg liver Elevated JVP 1- Increase venous pressure Pitting peripheral edema 1- Increase venous pressure 2- Transudation of fluid |
|
|
|
How does RAAS causing edema in heart failure |
Decrease cardiac output — activation of RAAS— increase circulating Na and water reabsorption in the kidney- Increase preload - Edema |
|
|
|
What is the most common cause of right heart failure in the absence of left heart failure |
Cor pulmonale to chronic obstructive pulmonary doses Right ventricle fails because increase pulmonary arterial pressure |
|
|
|
Most common cause of right sided heart failure |
Left sided heart failure |
|
|
|
Shock |
1- Inadequate organ perfusion and tissue oxygenation 2- Irreversibly but life threatening if not treated promptly |
|
|
|
Shock |
1- Inadequate organ perfusion and tissue oxygenation 2- Irreversibly but life threatening if not treated promptly |
|
|
|
Hypovolemic shock |
1- Hemorrhage, dehydration and burn 2- Cold and clammy 3- Decrease Preload Decrease CO and Increase SV (afterload) 4- Treatment IV fluids |
|
|
|
Shock |
1- Inadequate organ perfusion and tissue oxygenation 2- Irreversibly but life threatening if not treated promptly |
|
|
|
Hypovolemic shock |
1- Hemorrhage, dehydration and burn 2- Cold and clammy 3- Decrease Preload Decrease CO and Increase SV (afterload) 4- Treatment IV fluids |
|
|
|
Cardiogenic shock |
1- Acute MI, HF, Valvular dysfunction and arrhythmia 2- Cold and clammy 3- Increase preload decrease CO increase stroke volume 4- Treatment ionotropes and diuretic |
|
|
|
Shock |
1- Inadequate organ perfusion and tissue oxygenation 2- Irreversibly but life threatening if not treated promptly |
|
|
|
Hypovolemic shock |
1- Hemorrhage, dehydration and burn 2- Cold and clammy 3- Decrease Preload Decrease CO and Increase SV (afterload) 4- Treatment IV fluids |
|
|
|
Cardiogenic shock |
1- Acute MI, HF, Valvular dysfunction and arrhythmia 2- Cold and clammy 3- Increase preload decrease CO increase stroke volume 4- Treatment ionotropes and diuretic |
|
|
|
Obstructive shock |
1- Cardiac Tamponade, Pulmonary embolism and Tension pneumothorax 2- Cold and clammy 3- Increase preload decrease CO increase Strike volume 4- Treatment - Relieve obstruction |
|
|
|
Distributive shock |
1- Sepsis, anaphylaxis, CNS injury 2- Warm and dry 3- Decrease preload, increase CO, decrease SV 4- Treatment IV fluid, pressers, epinephrine |
|
|
|
SIRS criteria |
Temperature >38 or <36 HR > 90 RR > 20 WBC >12 <4 |
|
|
|
SIRS criteria |
Temperature >38 or <36 HR > 90 RR > 20 WBC >12 or <4 Any 2 |
|
|
|
Sepsis |
SIRs and a confirmed infection |
|
|
|
Cardiac Tamponade |
1- Compression of the heart by fluid 2- Accumulation of fluid in the pericardial cavity (blood and effusion) 3- Decrease Co 4- Equilibrium of diastolic pressure in all chamber 5- Symptoms 1- Becks triad 1- Hypotension 2- Distended neck vein 3- Muffled heart sound 2- Pulsus paradox 3- ECG - low voltage QRS complex,Tachycardia and Elcetrical alternans 6- Pulsus paradox 1- Decrease systolic pressure of >10mmHg during inspiration 2- Seen in 1- constructive pericarditis 2- Pulmonary Disease (COPD, OSA, Asthma, Coup) 3- Cardiac Tamponade |
|
|
|
Types of bacterial endocarditis |
Acute 1- Staphylococcus aureus affecting normal heart valve Subacute 1- Streptococcus Viridans affection abnormal or diseases heart valve 2- Sequel of dental procedure 3- Gradual onset |
|
|
|
Types of bacterial endocarditis |
Acute 1- Staphylococcus aureus affecting normal heart valve 2- High virulence 3- Rapid onset Subacute 1- Streptococcus Viridans affection abnormal or diseases heart valve 2- Low virulence 3- Sequel of dental procedure 4- Gradual onset |
|
|
|
Symptoms of bacterial endocarditis |
1- Fever 2- Roth spot (round white spots on retina surrounded by hemorrhage) 3- Osler nodes (painful lesion on fingers and toes) 4- Murmur 5- Janeway lesion (painless erythematous lesion on Pam and soles) 7- Anemia 8- Nail bed sphincter sphincter hemorrhage 9- Emboli |
FROM JANE |
|
|
Associated conditions of bacterial endocarditis |
1- Glomerulonephritis 2- Septic arthritis 3- Pulmonary emboli |
|
|
|
Non-bacterial causes of bacterial endocarditis |
1- Malignancy 2- Hypercoagulable star 3- Lupus (Libman Sacks Endocarditis) |
|
|
|
Cause of negative bacterial endocarditis culture |
Coxiella burnetti Bartonella spp |
|
|
|
Most common valve affected in bacterial endocarditis |
1- Mitral valve 2- Tricupid valve affected in IV drug users organism 1- Staphylococcus aureus 2- Pseudomonas 3- Candida |
|
|
|
Other organism causing bacterial endocarditis |
1- Streptococcus bovis - associated with colon cancer 2- Staphylococcus epidermidis- affect prostatic heart valve |
|
|
|
Cause of native valve endocarditis |
Hemophilus Aggregotibacter Cardiobacterium Eikenella Kingella |
HÁČEK |
|
|
Diagnosis of bacterial endocarditis |
1- Multiple blood culture 2- Echocardiogram |
|
|
|
Respiration with murmurs |
Left sided increase with expiration Right side increase with inhalation |
|
|
|
Location of thrombi on heart valves sterile vs infectious |
Sterile- inferior Infectious - Superior |
|
|
|
Rheumatic fever |
1- Caused by group A beta hemolytic streptococcus 2- Can progress to rheumatic heart disease 3- Affect high pressure balances Mitral > Aortic > Tricuspid 4- Early- mitral regurgitation late- mitral stenosis 5- Type 2 hypersensitivity |
|
|
|
Associations of rheumatic fever |
1- Aschoff bodies - granuloma with giant cells 2- Anitscjkow cell - enlarge macrophages with oval wavy nucleus 3- Anti- streptolycin O titer and Anti DNAse B titer |
|
|
|
Symptoms of rheumatic fever |
1- Migratory Poly arthritis 2- Carditis - myocardial 3- Subcutaneous nodules 4- Erythema marginatum 5- Syndenam chorea |
|
|
|
Diagnosis of rheumatic fever |
Clinical 1- Fever 2- Arthritis Laboratory 1- Prolonged PR interval 2- Increase ESR or CRP Criteria 1- Positive culture for group A beta hemolytic streptococcus or positive ASO antibody And 2- 2 major or 1 major and 2 minor
|
|
|
|
Treatment of rheumatic fever |
Penicillin G |
|
|
|
Pathogenesis of rheumatic fever |
Molecular mimicry M protein produce by group A strep can cross react and bind to the heart Cross react with myosin |
|
|
|
Virulent factors if rheumatic fever |
1- Streptoycin O - 1- lyses 2- Test ASO antibody titer 2- Streptokinase- Coat Bacteria 3- Hyalauranidase- Break apart connective tissue e 4- DNAse |
|
|
|
Molecular mimicry In rheumatic fever |
1- Against M protein/myosin- myocarditis 2- Against GAGs- valvular damage 3- Against gangliosides in the brain - chorea |
|
|
|
Erythema marginatum |
An evanescence rash with ring margin |
|
|
|
Syphilitic heart disease |
1- Tertiary syphilis disrupts the vasa vasorum of aorta (obliterative endarteritis) cause atrophy of vessel wall and dilatation of aorta and valvular ring 2- Can cause calcification of aortic root, ascending aorta arch and thoracic aorta 3- Tree-bark appearance (due to fibrosis) 4- Can cause aneurysm of ascending aorta, aortic arch and aortic regurgitation |
|
|
|
Acute pericarditis |
1- Inflammation of the pericardium 2- Symptoms - pleuritic chest pain worst in inspiration and lying flat relive with sitting up and leaning forward 3- Complicated by pericardial effusion/cardiac Tamponade 4- Signs 1- Pericardial rub 2- ECG widespread ST elevation and PR depression 5- Cause 1- Idiopathy 2- Infection (coxsachie virus) 3- Autoimmune (SLE) 4- Uremia 5- Cardiovascular (post MI- Dressler syndrome) 6- Treatment - NSAID, Colchicine, glucocorticoids, dialysis (uremia) |
|
|
|
Myocarditis |
1- Inflammation of the myocardium 2- Common cause of SCD in patients <40 3- Symptoms- chest pain, SOB, arrhythmia, fever (persistent tachycardia without fever is characteristic) |
|
|
|
Causes of myocarditis |
1- Viral (Adenivirus, coxsackie B, parvovirus B19, HIV, HHV-6, lymphocytic infiltrate with focal necrosis) 2- Parasites (Trypanosoma cruzi, Toxoplasmosis) 3- Bacteria (Borrelia burg for feri, mycoplasma pneumonia, corynebacterium diphtheria) 4- Toxins (Carbon monoxide, Black widow venom) 5- Rheumatic Fever 6- Drugs (Doxorubicin, cocain) 7- Autoimmune (Kawasaki disease, sarcoidosis,SLE, Poly myositis/Dermatomyositis) |
|
|
|
Complication of myocarditis |
1- Sudden cardiac death 2- Arrhythmia 3- Heart block 4- Dilated cardiomyopathy 5- Heart failure 6- Mural thrombosis with systemic emboli |
|
|
|
What histologic finding is suggestive of myocarditis |
Lymphocytic infiltrate with focal necrosis of myocardial tissues |
|
|
|
Cardiac tumors |
1- Most common heart time is metastasis (eg melanoma ) |
|
|
|
Myxomas |
1- Most common primary cardiac tumor in adults 2- 90% develop in the atrium (left atrium) 3- Associated with a ball valve obstruction with multiple episodes of syncope 4- IL- 6 causes constitutional symptoms (fever, night sweat and weight loss) 5- Early diastolic (tumor plop) sound 6- Histology gelatinous material 7- Immerse in glycosaminoglycans |
|
|
|
Rhabdomyomas |
1- Most common primary cardiac tumor in children 2 Associated with tuberous sclerosis 3- Histology Harmartomastis growth |
|
|
|
Kussmaul sign |
1- Increase JVP during inspiration instead of normal decrease 2 Inspiration- negative intrathoracic pressure not transmitted to the heart- Reduce right ventricular filling- back up of blood in vena cava- increase JVP 3- Causes 1- Constructive pericarditis 2- Massive pulmonary embolus 3- Restrictive cardiomyopathy 4- Right sided hear failure 5- Right atrial or ventricular failure |
|
|
|
Hereditary hemorrhagic telangiectasia |
1- Also called osler-Weber-rendu syndrome 2- Autosomal dominant disorder of blood vessels 3- Findings 1- Blanching lesions of the skin and mucus membrane 2- Skin discoloration 3- Recurrent epistaxis 4- Hematuria 5- GI bleeding 6- AV malformation |
|

