![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back

Dark red-blue mottling, gross appearance 12-24 hrs post MI, stagnant blood
|
-
|
|

yellow pallor due to coagulative necrosis, occurs in the first week post MI acute inflammation (neuts=>macs), note the risk of fibrinous pericarditis
|
-
|
|
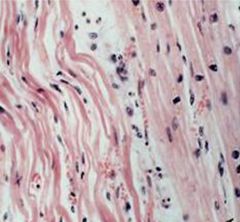
Wavy fibers and coagulative necrosis within 1 day of infarct
|
-
|
|

Papillary rupture within 1 week post MI, complication of macrphoage degradation of structural components during the inflammation stage
|
-
|
|
|
define IHD
|
imbalance between supply and demand for oyxgen and nutrients and removal of metabolites, ischemia worse than hypoxia
|
|
|
main cause of IHD (90%)
|
reduced coronary blood flow due to atherosclerotic narrowing (fixed plaque, acute plaque change, thrmobosis, vasospasm)
|
|
|
Describe the degree of stenosis required to cause ischemia with exercerise (stable angina) and at rest (unstable angina)?
|
with exercise-70%, at rest 90%;
|
|
|
describe acute plaque change
|
unpredictable abruput converstion of stable plaque to an unstable atherothrombic lesion that results in ischemia. Rupture/fissure/ ulceration exposes underling thrombogenic substnaces, hemorrhage into atheroma expands the plaque and narrows the vesseel lumen further. results in acute coronary syndromes: MI, unstable angina, sudden cardiac death
|
|
|
Causes of acute plaque change (intrinsic and extrinsic)
|
intrinsic-composition of the plaque(large area of foam cells/lipid with thin cap), most dangerous lesions are the moderately stenoti lipid rich atheromas, abundant inflammation, few SMCs. Extrinsic-adrenergic stimulation -upon awakening, emotional
|
|
|
outcome of coronary thrombosis total vs. incomplete occulsion
|
total-acute transmural MI or sudden death, incomplete=unstable angina, acute subendocardial infarct, sudden death, emboli
|
|
|
Causes of vasoconstriciton leading to severe but transient reduction in coronary blood flow
|
adrenergic agonist, locally released platelet contents, endothelial dysfxn, mast cell mediators
|
|
|
four syndromes of IHD
|
angina, MI, CIHD, sudden cardiac death
|
|
|
define angina
|
paroxysmal and recurrent attacks of chest pain caused by transient myocardial ischemia 15 seconds to 15 minutes
|
|
|
three patterns of angina
|
stable, prinzmetal, unstable
|
|
|
cause of stable angina
|
produces by physical activity or emotinoal excitement, stenosis of coronary artery 70-90%, subendocardial ischemia, reversible injury
|
|
|
cause of prinzmetal angina
|
coronary vasospasm at rest, reverislbe injury, transmural ischemia
|
|
|
cause of unstable angina
|
>90% stenosis, or acute plaque change=> thrombosis w/ incomplete occlusion, often prodrome of MI, reverisble injury, subendocardial ischemia
|
|
|
risk factors for MI
|
M>F, age, atherosclerosis (HTN, smoking, DM, increased cholesterol/ lipids)
|
|
|
Pathogenesis of MI
|
90%=acute plaque change resulting in thrombisis and emoblism of coronary a., 10% vasospasm, emboli, or unexplained
|
|
|
Transmural vs. subendocardial vessel distribution, degree of obstruciton, ECG
|
transmural-confined to 1 vessel districution, complete obstruction, ST elevation; subendocardial-non-occlusive thrombus or hypotension, extends laterally beoynd 1 vessel, ST depression
|
|
|
timeline of myocardial response to ischemia
|
60sec- loss of contractility, 20-40 min-irreversible damage
|
|
|
frequency of arteries occluded in MI
|
LAD-40-50%> RCA-30-40%> LCA-15-20%
|
|
|
pattern of ischemia with global hypotension
|
circumfrential subendocardial
|
|
|
describe the progression of gross myocardial findings post MI
|
<4 hrs=none. 1 day=dark red-blue mottling, post 1 day- 1 week=yellow pallor , post 1 week- 1 month=red boarder at edge of infarct=>white scar (hint: 1 day 1 week 1 month, necrosis, inflammation, healing0
|
|
|
describe the progression of microscopic myocardial findings post MI
|
<4hrs=none, 1 day=coagulative necrosis,contraction bands, 1day-1 week=marcophages, 1 week-1 month=granulation tissue=>fibrosis (hint: 1 day, 1 week, 1 month, necrosis, inflammation, healing)
|
|
|
describe the progression of clinical complication you would expect post MI
|
<4 hrs=cardiogenic shock, CHF, arrythmia, 1 day=arrhythmia, 1day-1 week=fibrinous pericarditis-rupture, months=aneurysm, mural thrombis, Dressler's syndrome
|
|
|
when in the course of an MI is arrhthmia a risk
|
early, less than 1 day
|
|
|
When in the course of an MI is fibrinous pericarditis a possible complication
|
earnly in the inflammation phase (1 day-1 week), only transmural infacrt, note chest pain w/ friction rub
|
|
|
when in the course of an MI is rupture a risk. What can rupture
|
Late in the inflammation phase (1day-1 week), macropahges degrade structural components-ventricular free wall-tamponade, IV septum-shunt, Papillary m.-MV insufficiency (if RCA infarct)
|
|
|
when in the couse of an infacrt is aneurysm ,mural thrombus, and Dressler's syndrome a risk
|
post healing phase, months,
|
|
|
what is dressler's syndrome
|
occurs months after MI, rate autoimmune reaction due to Ab's angainst pericardial antigens
|
|
|
Coagulative necrosis would be found when after an MI
|
4hrs-1 day, note loss of myocyte nuclei, wavy fibers, contraction bands
|
|
|
Neutrophils would be present in a sample of myocardium when after an MI
|
early in the inflammation phase (1 week-1 day), note the risk for fibrinous pericarditis
|
|
|
macrophages would be present in a sample of myocardium when after an MI
|
late in the inflammation phase (1day-1 week), note the risk of rupture of ventricular free wal, TV septum, or papillary m.
|
|
|
Granulation tissue would be present in a sample of myocardium when after an MI
|
during the healing phase (1 week-1 month), note plump fibroblasts, collagen and vessels
|
|
|
A white scar and fibrosis would be present in the myocardium when after an MI
|
post healing phase (1week-1 month) note the risk of aneurysm, mural thrombus, Dresseler's syndrome
|
|
|
wavy fibers would be present when after an MI
|
acute inflamation phate less than 1 day post
|
|
|
describe reperfusion injury
|
reperfusion prevents necrosis if occurs in less than 20 min but can lead t ohemorrhage into infarcted tissue, contraction bands, free radiacal release and microvascular injry, platelet and complement activation
|
|
|
Clincial signs/ sxs of MI
|
severe crushing substernal chest pain that radiates into the l. arm, neck, jaw, epigastrium, last several minutes to hours, no relief by NG, rapid weak pusle, diaphoresis, dyspnea
|
|
|
Acute and long term MI prognosis factors
|
acute-depends on infarct size, site, extent of wall penetration, Long term-depneds on quality of LV fxn and extent of vascular obstruction
|

