![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
Primary hyperthyroidism is caused by
|
Thyroid hyperplasia (Graves)
Hyperfunctional Multinodular goiter Hyperfunctional thyroid adenoma |
|
|
Secondary hyperthyroidism is caused by
|
pituitary thyrotroph adenomas, excess exogenous thyroid hormone (treatment for hypothyroidism) and thyroid inflammatory disease
|
|
|
What are the clinical feats of hyperthyroidism
|
-weight loss despite increased appetite
-heat intolerance and sweating -tachycardia with increased CO -arrhytmia (atrial fib) especially in the elderly -Tremor, anxiety, insomnia and heightened emotions -Starring gaze with lid lag -diarrhea -oligomenorrhea -Bone resorption with hypercalcemia (risk of osteoporosis) -Decreased muscle mass with weakness -Hypocholesterolemia -Hyperglycemia |
|
|
Graves disease (primary caused of hyperthyroidism) presents with a clinical triad
|
-hyperthyroidism due to hyperfunctional, diffuse thyroid enlargement
-Infiltrative ophthalmopathy with resultant exophthalmos -Localized infiltrative dermopathy present in a minority of its |
|
|
Who gets Graves disease usually?
|
Women 20-40
|
|
|
Grave's disease is an autoimmune disease and the 3 antibodies formed work against
-Thyroid stimulating immunoglobulin -Thyroid growth stimulating immunoglobulin -TSH-binding inhibitor immunoglobulin |
-Thyroid stimulating immunoglobulin : Binds to the TSHR and mimics the action of TSH, leading to T3 and T4 release. Specific for Graves
-Thyroid growth stimulating immunoglobulin: Directed against TSHR, but these autoantibodies induce thyroid follicular epithelium proliferation -TSH-binding inhibitor immunoglobulin: Binds to TSGR and prevents TSH from interacting with the receptor. Such antibodies can mimic TSH or can inhibit thyroid cell fx |
|
|
exophthalmos seen in Graves occurs due to
|
Fibroblasts behind the orbit and overlying the skin express TSH receptors. TSH activation results in glycosaminoglycan build up, inflammation, fibrosis, and edema leading to exopthalmos and pretibial myxedema
|
|
|
Grossly how does the thryoid appear in Graves?
|
Thyroid gland is mildy and symmetrically enlarged with an intact capsule and soft parenchyma
|
|
|
Histologically how does the thyroid in graves appears?
|
Irregular follicles with scalloped colloid and chronic inflammation are seen on histology
|
|
|
What are the lab findings in graves?
|
Hypocholesterolemia
Increased serum glucose T4 and T3 are elevated and TSH is depressed |
|
|
Primary hypothyroidism can be accompanied by
|
Thyroid enlargment (goiter) . In Iodide sufficient areas of the world, the most common cause of hypothyroidism is autoimmune thyroiditis-hashimoto
|
|
|
Other causes of hypothyroidism include
|
-dietary iodine deficiency (endemic goiter, inborn errors of metabolism)
-Pendred syndrome -inactivating mutations of the TSH receptor -thyroid surgery or radiation |
|
|
Secondary hypothyroidism is caused by
|
TSH deficiency or TRH deficiency (rare)
|
|
|
The most sensitive screening test for primary hypothyroidism is
|
-Elevated TSH levels due to loss of feedback inhibition by TRH and TSH
Low T4 Clinically manifests as cretinism in children and myxedema in older children and adults. |
|
|
Initially may present as hyperthyroidism due to follicel damage. Progresses to hypothyroidism. Antithyroglobulin and antimicrosomal antibodies are often present (sign of thyroid damage)
|
Hashimoto
|
|
|
who gets hashimoto?
|
More in females 45 to 65
|
|
|
Hashimoto is an autoimmune injury mediated by
|
antibodies against thyroglobulin an thyroid peroxidase, CD8+ cytotoxic T cells.
|
|
|
Microscopically hashimoto presents as
|
chronic inflammation with germinal centers and hurtle cells (eosinophilic metaplasia of cells that line follicles). Increased risk for B cell non hdg lymphoma and it presents as an enlarging thyroid late in the course of disease
|
|
|
thyroiditis that follows a viral infection mostly in females 40-50. Pt with tender thyroid with transient hyperthyroidism.
|
Subacute granulomatous thyroiditis. DOES NOT progress to hypothyroidism. It happens less frequent than hashimoto
|
|
|
Chronic inflammation with extensive fibrosis of the thyroid gland, presents as hypothyroidism with a hard as wood nontender thyroid gland
|
Reidel fibrosing thyroiditis
|
|
|
How does reidel manifest?
|
Mimics anaplastic carcinoma, but patients are younger (40s) and malignant cells are absent
|
|
|
Pts show signs of being euthyroid (normal thyroid function) TSH levels are elevated
|
Simple (nontoxic) goiter. They can be endemic and sporadic
|
|
|
Occurs in geographic areas with low iodine levels or diets high in goitrogen (cassava, cabbage)
|
Endemic goiters
|
|
|
Mostly females present with this goiter after goitrogen ingestion or genetic abnormalities
|
Sporadic goiter
|
|
|
Simple goiter (nontoxic) has 2 stages
|
Hyperplastic (some follicles hugely distented while others are small)
Colloid involution: enlarged colloid rich gland |
|
|
Pts may present with esophageal compression with dysphagia, tracheal compression and superior vena cava obstruction. Reduced TSH
|
Multinodular goiter. Multinodular goiter is the most common disease of the thyroid in the US and is the most common indication for fine needle aspiration biopsy
|
|
|
Multinodular goiters are mostly nontoxic, but can develop into toxic ones when
|

a hyperfunctioning nodule leading to hyperthyroidism, known as Plummer syndrome) as opposed to graves this one does not cause exolthamos
|
|
|
What are thyroid adenomas?
|
Discrete, solitary masses derived from follicular epithelium and they are non functional, rarely a precursor to malignancy
|
|
|
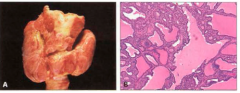
Grossly follicular adenomas are
|
Well demarcated encapsulated lesions with fibrosis, hemorrage or calcification. Encapsulation is the differentiang feat between follicular adenomas and follicular carcinomas
|
|
|
Who gets follicular carcinoma?
|
Females between 40 and 60 and there is an increased prevalence in areas of dietary iodide deficiency
|
|
|
Patient presents with slowly growing painless cold nodule.
|
Follicular carcinoma. Microscopically, nuclear feats are absent. Most exhibit microfollicular pattern with uniform, colloid filled follicles like normal thyroid. Hurtle cells may be seen
|
|
|
How does follicular carcinoma spread?
|
Hematogenous to bone, lung and liver. Minimal invasive follicular carcinoma has a 10 year survival rate more than 90%, while invasive carcinoma with metastases has a 50% 10 year mortality.
|
|
|
Whats the therapy for follicular carcinoma?
|
Resection, radioactive iodine to ablate metastatic lesions and thyroid hormone administration to reduce TSH that could potentially be stimulatory for malignant epithelium.
|
|
|
These type of carcinoma presents as isolated, asymptomatic cold thyroid nodule. The first sign may be cervical node metastases. Hoarseness, dysphagia, cough or dyspnea suggests advanced disease
|
Papillary carcinomas. Exposure to ionizing radiation in childhood is major risk factor. Females 40-60 get it predominantely in areas of dietary iodine deficiency
|
|
|
Microscopically papillary carcinoma looks like
|
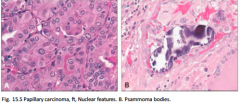
Papillae lined by cells with clear "Orphan Annie Eye" nuclei and nuclear grooves. Associated with psommonas bodies
|
|
|
Whats the prognosis of papillary carcinoma?
|
95% survival 10 years
|
|
|
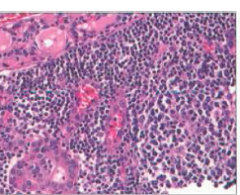
Malignant proliferation of parafollicular C cells
|
Medullary carcinoma. Cells are polygonal to spindle shaped and are arrayed in nests, trabeculae and ocassionally follicles. Stromal amyloid deposits (from altered calcitonin) are often present
|
|
|
Medullary carcinoma familial cases
|
due to multiple endocrine neoplasia (MEN) 2A and 2B which are associated with mutations in the RET oncogene. Detection of RET mutation warrants prophylactic thyroidectomy.
MEN 2B are aggresive and metastasize often. |
|
|
Thyroid mass there may be dysphasia, hoarseness. Initial manifestations may be cushing syndrome, or hypocalcemia
|
sporadic medullary carcinoma
|
|
|
Thyroid or extrathryoid neoplasm or identified through screening of asymptomatic relatives of affected patients
|
familial medullary carcinoma. Multifocal C cell hyperplasia is often present in familial cases but it is absent in sporadic cases.
|
|
|
Aggresive thyroid carcinoma in elderly patiens (older than 65) and associated with prior or concurrent well differentiated thyroid cancer
|
Anaplastic (undifferentiated) carcinoma.
|
|
|
Microscopically anaplastic carcinoma look like
|
highly anapestic, cells and large pleomorphic giant cells and spindle cells with sarcomatous appearance.
|
|
|
How does anaplastic carcinoma present clinically?
|
Rapidly enlarging bulky masses that have already invaded neck structures or metastasized to lung at the time of diagnosis. Death is secondary to aggresive local growth.
|

