![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
what are common cell types found in the AIRWAYS (except vocal cords):
a. stratified squamous epithelium b. pseudostratified columnar epithelium c. simple squamous epithelium d. transitional epithelium |
pseudostratified columnar epithelium (ciliated cells and goblet cells)
|
|
|
What 2 cellular components are present in airway and absent in brionchioles:
a. alveoli b. type II pneumocytes c. submucosal glands d. goblet cells |
glands and goblet cells are only found in airway part of tarchea
alveoli usually consists of: simple squamous epithelium, type I and II pneumocytes, subendothelial CT, capillary endothelium and some macrophages |
|
|
Atelectasis is collapse or incomplete expansion of alveoli leading to perfusion but NO ventialation leads to an increased risk for infections. Which type is localized in the vicinity of scars:
a. absorptive b. compressive c. contraction d. patchy |
contraction
|
|
|
this type of atelectasis is secondary to pleural effusin due to fluid accumulation or tumor:
a. absorptive b. compressive c. contraction d. patchy |
compressive
|
|
|
this type of atelectasis is often seen in premies due to lack of surfactant:
a. absorptive b. compressive c. contraction d. patchy |
patchy
|
|
|
what is a common hemodynamic cause of pulmonary edema?
a. capacity of lymphatics to drain the interstitium is exceeded b. osmotic pressure decreases c. lymphatic obstruciton d. hypoalbumin |
capacity of lympahtic to darin the interstitium is exceeded
LEAKY vessels 2) LHF 3) decreased oncotic P |
|
|
Pulmonary edema can result in two stages including loss of lung compliance leading to stiff lungs and alveolar edema which leads to:
a. barrier to gas exchange b. decrease in elastic recoil c. stop in ventilation (ARDS) d. increase in fibrosis |
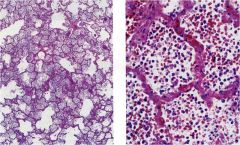
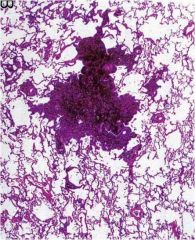
pulmonary edema
1) interstitial edema: loss of lung compliance and barrier to gas exchange 2) stop in ventilation (hypoxemia) and good culture medium for bacterial growth can lead to pneumonia |
|
|
What is a common cause of pulmonary congestion:
a. contraction (scarring) b. lack of surfactant c. microvascular injury (leaky vessels) d. tumors |
pulmonary congestion is usually due to microvascular injury (leaky vessels) this can be dangerous since it can cause tiny hemorrhages into alveoli --> gobbled via macrophages --> hemosiderin laden cells (heart failure cells)
|
|
|
these 2 pts are at risk for pulmonary emboli:
a. pregnancy b. long car or plane trip c. bicycling d. cardio workout |
bed rest, long car or plane trip, immobilization of extremeties, RHF
since all can lead to venous stasis. pregnancy, burns, post-op, CA IV lines 3 factors important in pulmonary emboli: 1) venous stasis 2) hypecoagulation 3) damaged endothelium |
|
|
What non-hemodynamic action can also lead to pulmonary edema?
a. toxic gases b. NSAIDS c. AIDS d. volume overload |
toxic gases... also infecitons, drowning injury, drugs..
|
|
Toxic gases led to "stiff" lungs, dyspnea and potential risk for hypoxemia
a. contraction atelectasis b. pulmonary edema c. obstructive atelectasis d. pulmonary carcinoma |
pulmonary edema
|
|
Results from volume overload or LHF
a. pulmonary edema b. obstructive atelectasis c. patchy atelectasis d. CHF |
pulmonary edema
|
|
|
Pulmonary congestion can lead to diffuse alveolar damage what are 2 common causes:
a. infection b. severe trauma c. hypoxia d. fluid overload |
infection
severe trauma aspiration inhalation (smoke and toxins) drug injury (chemo) burns near drowining |
|
|
what pulmonary condition is frequently underdiagnosed and is asymptomatic:
a. pulmonary edema b. pulmonary carcinoma c. pulmonary emboli d. pulmonary fibrosis |
pulmonary emboli: common, underdiagnosed and asymptomatic
can detect with CT, angiogram, D-dimer test originate in large veins of legs and pelvis |
|

This pulmonary dysfunction is common, udnerdiagnosed, and asymptomatic detected via CT, angiogram, D-dimer test; small don't usually cause an infarct. OFTEN FATAL!!
a. p.edema b. p.emboli c. p.congestion d. p.carcinoma |
pulmonary embolus
|
|
|
Pulmonary HTN is caused due to an increase in Resistance to blood flow and is usually secondary to what 2 condition:
a. RSHF (heart failure) b. LSHF (heart failure) c. CKD (chronic kidney disease) d. COLD (chronic obstructive lung disease) |
LSHF (mitral stenosis)
Chronic obstructive lung disease (vasoconstriction of arterioles supplying under oxygenated alveoli) |
|
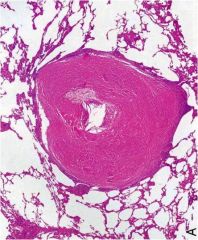
Leads to thickened arteriolar wall:
a. pulmonary emboli b. pulmonary edema c. pulmonary hypertension d. pulmonary atelectasis |
pulmonary HTN usually secondary to
chronic obstructive lung disease LSHF (mitral stenosis) |
|

Pulmonary artery atherosclerosis implies:
a. pulmonary emboli b. pulmonary edema c. pulmonary hypertension d. pulmonary atelectasis |
pulmonary HTN
|
|
|
What is the main cause of increased pulmonary vascular resistance:
a. increased flow through pulmonary arteries b. increased turbulent flow through pulmonary arteries c. hypoxic vascular response d. increase in surface tension due to lack of surfactant |
hypoxic vascular response --> reflex vasoconstriction of arterioles supplying under oxygenated alveoli leading to chronic obstructive lung disease
|
|
|
Pt presents with acute onset of respiratory illness with NO clincial evidence of LHF and hypoxemia (decreased ventilation). Upon review of CXray you notice bilateral opacies, what can be a possible diagnosis:
a. pulmonary edema b. pulmonary HTN c. acute respiratory distress syndrome d. pneumonia |
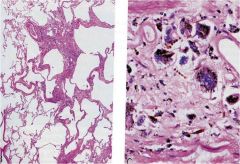
ARDS due to diffuse alveolar damage
common clinical features: *acute onset of respiratory illness **bilateral opaciteis ***hypoxemia no clinical evidence of LHF and usually an inciting event is present |
|
|
common causes of ARDS EXCEPT;
a. infection (sepsis) b. severe trauma c. aspiration d. mitral stenosi |
mitral stenosis not a cause for ARDS
infection (spesis or pneumonia) severe trauma aspiration inhalation (smoke or toxic gases) burns drug injury near drowning |
|
|
the physiological response to severe injury to epithelium and /or enodthelium of alveoli occurs as follows:
a. defective ep BM --> increase matrix components --> CT migrate into airspace --> type II resurface b. increase matrix components --> type II resurface --> defective epithelial BM c. defective epBM --> CT cell migrate into airspace --> increase matrix components --> type II resurfaced d. CT migrate into airspace --> type II resurface |
defective epBM --> CT cell migrate into airspace --> increase matrix components --> type II resurfaced
(see diagram) |
|
defective epBM --> CT cell migrate into airspace
resulting in edema (0-2d) hyaline membrane (1-9d) phase of ARDS a. organizing b. exudate c. fibrotic d. inflammatory |
exudate
1) edema (0-2d) 2) hyaline membrane (1-9d) |
|
What ARDS phase:
interstitial inflammation and fibrosis a. exudate b. organizing c. fibrotic d. edematous |
organizing
1) interstitial inflammation 2) interstitial fibrosis |
|
|
5 common cancers present in SMOKERS?
a. kidney, bone, pancreatic, lung, throat b. mouth, throat, larynx, esophageal, oral c. bladder, kidney, bone, pancreatic, esophageal d. mouth, throat, bladder, bone, esophageal |
mouth, larynx, throat, esophageal, oral (smokeless tobacco)
|
|
|
Pt chews smokeless tobacco, what is his/her cancer risk
a. mouth b. larynx c. oral d. esophageal |
oral
|
|
|
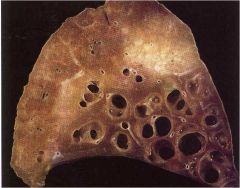
What is defective after damage to alveolar walls in emphysema that is vital in preventing the small airways from collapsing during exhalation:
a. compliance b. elastic recoil c. surface tension d. thickness |
elastic recoil resulting in collapse of small airways
|
|
|
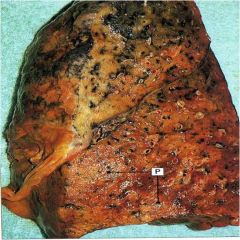
Heavy smoker presents with barrel chest, dyspneic, and pursed lips. what condition can cause these symptoms:
a. centilobular emphysema b. panacinar emphysema c. cystic fibrosis d. chronic asthma |
centilobular emphysema resulting from smoke accumulation leading to increase in proteases of UPPER lobes
"smoker" emphysema |
|
|
Pt presents with LOWER lobular damage, dyspnea, cough, wheezing, weight loss. You notice permanent enlargement of airspace due to alveolar destruction.
a. centilobular emphysema b. panacinar emphysema c. cystic fibrosis d. chronic asthma |
panacinar emphysema resulting from a genetic condition (alpha -1- antitrypsin deficiency) leading to failure to destroy proteases common in LOWER lobes
|
|

common in UPPER lobes, resulting from increased smoking:
segmental pigments clinical: barrel chest, dyspneic, prolonged expiration, pursed lips, expiration limitation a. centilobular emphysema b. panacinar emphysema c. cystic fibrosis d. chronic asthma |
centilobular emphysema
|
|
leads to entire lobe destruction in LOWER lobes due to a genetic defect alpha -1- antitrypsin deficiency
a. centilobular emphysema b. panacinar emphysema c. cystic fibrosis d. chronic asthma |
panacinar emphysema
|
|
|
Pt presents with a persistent cough w/SPUTUM production for the past 3 months. Pt admits this has been going on for at least 2 years. Pt admits to smoking for over 10 years. What is the major risk factor of his condition (chronic bronchitis)
a. smoking interfere with ciliary action of respiratory epithelium -- >damage airways --> can't clear bacteria b. hypersecretion of MUCUS --> hypertrophy of submucosal glands in trachea and bronchi --> obstruction c. neutrophiles --> release elastase, catehpsin --> mucus hypersecretion --> increase in goblet cells |
a. Smoking ...although neutrophiles are increases and do lead to hypersecretion of mucus; SMOKE is a major risk factor since it interferes with ciliary action of respiratory epithelium, causing damage to airway epithelium, inhibits the ability of bronchial and alveolar leuckocytes to clear bacteria
|
|
|
Pt presents with chronic necrotizing infection (destruction of the muscles and elastic tissue) leading to permanent dilation of bronchi and bronchioles, clinically a FOUL smelling sputum; what can this be:
a. chronic bronchitis b. bronchiectasis c. bronchpneumonia d. lobar pneumonia |
bronchiectasis permanent dilation of bronchi and bronchioles caused by destruction of muscle and elastic tissue (necrotizing infections)
|
|
|
Risk factors associated with bronchiectasis: permanent dilation of bronchi and bronchioles caused by destruction of muscle and elastic tissue: EXCEPT
a. cytstic fibrosis b. bronchial tumors c. smoking d. ciliary problems |
cystic fibrosis
bronchial tumor ciliary problems all lead to permanent airway OBSTRUCTION!! EXCEPT smoking |
|
Presents with FOUL smelling sputum; common causes include CF, bronchial tumors, and ciliary problems (bronchial OBSTRUCTION)
a. chronic bronchitis b. bronchiectasis c. broncopneumonia d. atypical pneumonia |
bronchiectasis
|
|
|
What conditions lead to a decrease in ciliary activity (high risk for bronchiectasis):
a. CF b. sarcoidosis c. ciliary dyskinesia d. Kartagener's syndrome e. asperguillus |
CF
ciliary dyskinesia Kartagener's syndrome aspergiullus (allergic reaction --> IgE plug) |
|
|
A 63 year old man has had progressively worsening dyspnea over the past 10 years. He has noticed a 10 lb. weight loss over the past 2 years. He had a chronic cough with minimal sputum production. On physical exam, he is afebrile and normotensive. A CXR shows extensive interstitial disease. Pulmonary function testing shows low FVD and a normal FEV1/FVC ratio. Increased exposure to which of the following is most likely to produce these findings?
a. Silica b. Tobacco smoke c. Ozone d. Wood dust e. Carbon monoxide |
silica
|
|
|
A 45 year old man had smoked two packs of cigarettes per day for 20 years. For the past 4 years, he has had a chronic cough with copious mucoid expectoration. During the past year, he has had several episodes of respiratory tract infections that were diagnosed as “viral flu,” and he developed difficulty breathing, tightness in the chest, and audible wheezing. His breathing difficulty was relieved by inhalation of a B-adrenergic agonist and disappeared after the chest infection had resolved. Which of the following pathologic conditions best described these clinical findings?
a. Chronic bronchitis with cor pulmonale b. Chronic bronchitis with asthmatic bronchitis c. Chronic bronchitis with emphysema d. Bronchiectasis e. Hypersensitivity |
chronic bronchitis w/emphysema
|
|
|
A 34 year old man suddenly develops severe dyspnea with wheezing and is taken to the ED. A CXR shows increased lucency in all lung fields. A sputum cytologic specimen shows Curschmann spirals, Charcot-Leyden crystals and acute inflammatory cells in a background of abundant mucus. Many of the inflammatory cells are eosinophils. Which of the following is the most likely diagnosis?
a. Bronchiectasis b. Aspiration c. Bronchial asthma d. Centrilobular emphysema e. Chronic bronchitis f. Obstructive sleep apnea |
bronchial asthma
|
|
|
A 50 year old man comes to the physician with gradually increasing dyspnea and a 8 lb weight loss over the past 2 years. He admits to smoking two packs of cigarettes per day for 20 years, but states that he has not smoked for the past year. PE shows an increase in the AP diameter of the chest (“barrel chest”). Auscultation of the chest shows decreased lung sounds. A chest radiograph shows bilateral hyperlucency, especially in the upper lobes. Pulmonary function tests show that the FEV1 is markedly decreased, but the FVC is normal. The FEV1/FVC is decreased. Which of the following is most likely to contribute to the pathogenesis of his disease?
a. Impaired hepatic release of a1-antitrypsin b. Release of elastase from neutrophils c. Abnormal epithelial cell chloride ion transport d. Decreased ciliary motility with irregular dynein arms e. Macrophage recruitment and release of interferon gamma |
release of elastase from neutrophiles
|
|
|
A 50 year old man had developed truncal obesity, back pain, and easily bruisable skin over the past 5 months. He is afebrile and his BP is 160/95 mmHg. A CXR shows an ill-defined 4 cm mass involving the left hilum of the lung. Cytologic exam of bronchial washings shows round cells that have the appearance of lymphocytes but are somewhat larger. The patient is told that, although his disease is apparently localized to the lung, surgical treatment in unlikely to be curative. He is advised to stop smoking. Which of the following neoplasms is most likely to be present in this patient?
a. Adenocarcinoma b. Bronchial carcinoid c. Bronchoalveolar carcinoma d. Large cell carcinoma e. Metastatic renal cell carcinoma f. Non-Hodgkins lymphoma g. Small cell carcinoma h. Squamous cell carcinoma |
small cell carcnioma
|
|
|
A 70 year old woman is referred to an ophthalmologist because of difficulty with her right eye. She also has pain in the right upper chest. The findings of physical exam include enophthalmos, meiosis, ptosis, and anhidrosis. A CXR shows right upper lobe opacification and bong destruction of the right first rib. Which of the following conditions is most likely to be present?
a. Bronchopneumonia b. Bronchiectasis c. Brochogenic carcinoma d. Sarcoidosis e. Tuberculosis |
brochogenic carcinoma
|
|
|
A 56 year old man with ischemic heart disease undergoes a CABG procedure under general anesthesia. Two days postoperatively, he experiences increasing respiratory difficulty with decreasing arterial oxygen saturation. He is afebrile, HR is 78/min, R are 20/min, BP is 135/85 mmHg. Hemoglobin is unchanged at 13.7 g/dL. After he coughs up a large amount of mucoid sputum, his condition improves. Which of the following is the most likely explanation of these findings?
a. Resorption atelectasis b. Compression atelectasis c. Microatelectasis d. Contraction atelectasis e. Relaxation atelectasis |
resorption atelectasis
|
|
|
A 20 year od man has had mild fever with nonproductive cough, headache and myalgia for the past week. He goes to the physician who records a temperature of 37.9 degrees C and notes erythema of the pharynx. Diffuse crackles are heard on ausculation. A CXR shows bilateral extensive patchy infiltrates. A sputum gram stain shows normal flora. The cold agglutinin titer is elevated. He received a course of erythromycin therapy and his condition improves. Infection with which of the following organisms is most likely to produce these findings?
a. Legionella b. Mycobacterium fortuitum c. Mycoplasma pneumoniae d. Nocardia asteroids e. Respiratory syncytial virus |
mycoplasma pneumoniae
|
|
|
A 35 year old man who is HIV positive complains of a bad taste in his mouth and discoloration of his tongue for the past 6 weeks. On physical exam, there are areas of adherent, yellow-tan plaque on the lateral aspects of the tongue. This plaque is scraped off to reveal an underlying granular, erythematous base. Which of the following is the most likely diagnosis?
a. Aphthous ulcer b. Cheilosis c. Hairy leukoplakia d. Herpetic stomatitis e. Leukoplakia f. Glossitis g. Oral thrush |
oral thrush
|
|
|
A 68 year old man goes to the physician for a routine health maintenance exam. He has some disecrete white patches with a leathery surface covering the right buccal mucosa of the oral cavity. A biopsy from one of the lesions shows squamous epithelia acanthosis with marked hyperkeratosis. Which of the following risk factors is most likely to cause these lesions?
a. Eating chili peppers b. Chewing spearmint gum c. French kissing d. Chewing tobacco e. HIV infection |
chewing tobacco
|
|
|
The family of a 63 year old woman noticed that she has become more forgetful over the past 6 weeks. One month later the woman has difficulty ambulating and is unable to care for herself. She has myoclonus and is afebrile. CT scan shows minimal cerebral atrophy. EEG shows low-amplitude, slow background activity with periodic complexes and occasional repetitive, sharp waves with intervals of 0.5 to 1 sec. Which of the following histologic abnormalities is most likely to be found in the cerebral cortex?
a. Numerous pleuritic plaques b. Plaques of demyelination c. Lewy bodies d. Microglial nodules e. Spongiform encephalopathy |
spongiform encephalopathy (Creutzfeld-jakob)
|
|
|
A 40 year old previously healthy man is brought to the emergency department after sudden onset of a grand mal seizure. Physical exam yields no remarkable findings except for a 1 cm darkly pigmented lesion on the skin of the upper back. CT scan of the head shows five sharply circumscribed mass lesions located in the cerebral hemispheres at the gray-white junction of the parietal and frontal lobes. Which of the following is the most likely diagnosis?
a. AIDS b. Metastases c. Infective endocarditis d. Neurofibromatosis type I e. Cysticerosis |
metastases
|
|
|
A 38 year old woman who fell to the ground and hit her head is taken to the emergency department. There are no remarkable findings on physical exam. CT scan of the head shows no hemorrhage or fracture, but there is a 5 cm mass beneath the dura that compresses the underlying left superolateral parietal lobe. The mass is surgically removed. Histologic analysis shows elongated cells with pale, oblong nuclei and pink cytoplasm with occasional psammoma bodies. Which of the following is the most likely diagnosis?
a. Meningioma b. Tuberculoma c. Medulloblastoma d. Schwannoma e. Ependymoma |
meningioma
|
|
|
A 53 year old man dies of aspiration pneumonia after a 6 year illness, characterized by progressive, symmetric muscular weakness. At autopsy, the brain and spinal cord appear normal on gross exam. Microscopic sections show gliosis in the motor cortex, pallor of the lateral corticospinal tracts and neuronal loss in the anterior horns of the spinal cord. Which of the following is the most likely underlying cause of death?
a. Becker muscular dystrophy b. Neurofibromatosis type II c. Guillain-Barre syndrome d. Creutzfeldt-Jakob disease e. Amyotrophic lateral sclerosis |
amyotrophic lateral sclerosis
|
|
|
A 19 year old snowboarder wearing protective equipment consisting of a baseball cap, baggy shorts and a letterman’s jacket flew off a jump and hit a tree. He was initially unconscious and then “came to” and wanted to try another run, but his friends thought it best to call for help. On the way to the emergency department, he became comatose. Physical exam shows left papilledema. Skull radiographs show a linear fracture of the left temporal-parietal region. A serum drug screen is positive for cannabinoids. The clinical picture is most consistent with which of the following lesions?
a. Contusion of frontal lobes b. Epidural hematoma c. Ruptured berry aneurysm d. Acute leptomeningitis e. Acute subdural hematoma |
epidural hematoma
|
|
|
13. 36 hours after falling down a flight of stairs, a 72 year old woman develops a headache and confusion and is taken to the emergency department. On physical exam, she is conscious and has a scalp contusion on the occiput. Which of the following is the most likely location of an intracranial hemorrhage in this patient?
a. Pontine b. Subarachnoid c. Basal ganglia d. Epidural e. Subdural |
sudural
|
|
|
A 30 year old woman has noted minimal fetal movement. An ultrasound show a defect in skull development. Which of the following laboratory findings is most likely to be present?
a. Fetal hyperbilirubinemia with anemia b. High maternal cytomegalovirus IgM titer c. Elevated maternal serum AFP level d. Elevated maternal hemoglobin A1C e. 47, XX, +21 fetal karyotype |
elevated maternal serum AFP level
|
|
|
While working at her desk as an accountant, a 50 year old woman develops sudden, severe headache and is taken to the emergency department. On examination, she has nuchal rigidity. A lumbar puncture is performed. The CSF shows numerous RBCs, no neutrophils, a few mononuclear cells and a normal glucose level. The gram stain result is negative. Which of the following events has most likely occurred?
a. Middle cerebral artery thromboembolism b. Tear of subdural bridging veins c. Ruptured intracranial berry aneurysm d. Bleeding from cerebral amyloid angiopathy e. Hypertensive basal ganglia hemorrhage |
ruptured intarcellular berry aneurysm
|
|
|
A 55 year old man had increasing difficulty with initiation of voluntary movements and increasing inability to perform activities of daily living for 1 year. He became bedridden and died of pulmonary thromboembolism. The gross appearance of the midbrain shows lack of pigmentation. Which of the following additional clinical features is most closely associated with this lesion?
a. Pill-rolling tremor at rest b. Symmetric weakness in the extremities c. Choreiform movements d. Difficulty with short-term memory e. Paraplegia |
pill-rolling tremor at rest
|
|
|
A 20 year old man with HIV infection has had a decreased level of consciousness for the past week. He now experiences a seizure. On physical exam, his temperature is 37.6 degrees C. MRI of the brain shows several 1 to 3 cm ring-enhancing lesions in the cerebral gray matter bilaterally. Stereotaxic biopsy is performed. Which of the following pathologic findings is most likely to be present on the microscopic examination of the biopsy specimen?
a. Large atypical lymphocytes b. Budding cells with pseudohyphae c. Spongiform encephalopathy d. Toxoplasma pseudocytes e. Metastatic squamous cell carcinoma |
toxoplasma pseudocytes
|
|
|
Three months ago, a 27 year old woman had an episode of weakness, which she attributed to job stress and fatigue. She now sees her physician because she has had decreased vision in her left eye for the past week. The neurologic exam shows mild residual weakness with 4/5 motor strength in the right lower extremity. A lumbar puncture is performed. Lab exam of the CSF shows increased IgG levels with prominent oligoclonal bands. MRI of the brain shows small scattered areas consistent with demyelination, most of which are located in the periventricular white matter. Which of the following is the most appropriate information to give the patient about these findings?
a. No further neurologic problems will be experienced b. Relapses and remissions will occur over many years c. This disease can be passed on to your children d. Further debilitation and death will occur within 5 years e. A test for HIV will be positive |
relapse and remission will occur over many years
|
|
|
Within the two types of bacterial pneumonia (bronchopneumonia and lobar) this organism often results in hospital-acquired pneumonia (bronchopneumonia):
a. streptococcus b. mycoplasma c. staphylococcus aures d. legionella |
staphylococcus aures (Hospitial acquired or bronchopneumonia)
|
|
|
Pt presents with patchy spotey suppurative inflammation in lungs, most frequently due to increased neutrophile exudate. what organism is common in this attack:
a. streptococcus b. mycoplasma c. staph aures d. legionella |
presentation of patchy spoty bilateral suppurative inflammation is common in bronchopneumonia (HOSPITAL - acquired)
|
|
|
Pt presents with congestion and it appears that the infiltrate has spread throughout a lower chunk of the lung. what can be a possible culprit of this lobar pneumonia (community acquired)
a. streptococcus b. staph aurees c. enterobacteria d. gram (-) rod |
streptococcus pneumonia frequently result in community acquired pneumonia
four stages: congestion red hepatization gray hepatization resolution |
|
|
This pneumomia frequently involves massive confluence of exudate including neutorphiles, red cells, fibrin in alveolar spaces. What organisms can be involved EXCEPT:
a. streptococcus b. haemophilus influenza c. enterobacteria d. chlamydia |
all are cause lobar pneumonia (community acquired) except enterobacteria often common in (hospital acquired pneumonia)
|
|
|
Pt presents with ABRUPT onset of symptoms, fever, shaking chills, cough, and muco-purulent sputum. What can be a possible diagnosis that could be prevented with a vaccine:
a. staphylococcus aures b. pseudomonas aeruginosa c. streptococcus pneumoiniae d. enteric Gram (-) bacilli |
streptococcus pneumonia is a community acquired pneumonia often present as a lobar pneumonia involving the entire sections of lobe
|
|
Consolidated areas of PATCHY suppurative inflammation; usually as a result of what organism:
a. streptococcus pneumoniae b. mycoplasma pneumoniae c. haemophilus influenzae d. staphylococcus aures |
hospital acquired pneumonae is often call bronchopneumoina "patchy"
staphylococcus aures enteric Gram (-) bacilli pseudomonas aeruginosa anaerobes |
|
acute suppurative inflammation (increased number of NEUTROPHILES)
exudate of fluid, Neutros, and macros into alveoli a. streptococcus b. mycoplasma c. chlamydia d. staphylococcus aures |
staphylococcus aures (hospital acquired pneumoniae)
|
|

lobar pneumonia; exudates in alveoli with macrophages, loss CT organization (fibroblast) against alveolar wall (usually restore and return to normal)
infects whole lobe at times giving a radio-opaque Xray a. streptococcus pneumonia b. staphylococcus aures c. enteric Gram (-) bacilli d. pseudomonas aeruginosa |
steptococcus pneumonia result in lobar pneumonia affecting entire lobe
|
|
|
What is a common culprit of atypical pneumonia resulting in moderate amount of sputum, patchy inflammatory changes in the lung.
a. streptococcus pneumoniae b. staph aures c. haemophilus influenzae d. mycoplasma pneumoniae |
mycoplasma pneumoniae
|
|
|
Pt presents with inflammation of the lung due to prolonged exposure to ANTIGEN such as asbestos, silica, or radiation resulting in difficulty breathing and cough. what can result:
a. bronchopneumonia b. lobar pneumonia c. penumonitis d. atypical pneumonia |
pneumonitis; common antigens are: asbestos, silica, drugs, radiation, and poultry, pigeons, or pet birds, molds..
|
|
|
What is the mechanism of actions in pneumonitis:
a. suppurative inflammation with increased neutrophiles b. four stages of inflammatory response c. damage to alveoli leading to serious chronic fibrotic lung disease d. organism attaches and results in necrosis leading to inflammation |
c. damage to alveoli (due to ANTIGEN) leading to serious chronic fibrotic lung disease
the other are: a. suppurative inflammation with increased neutrophiles (bronchpneumoina HA) b. four stages of inflammatory response (lobar pneumonia CA) d. organism attaches and results in necrosis leading to inflammation (atypical pneumonia) |
|
|
common complications of pneumonia include all EXCEPT:
a. abscess b. empyema c. edema d. sepsis |
abscess (tissue destruction and necrosis), empyema (spread of infection), sepsis (bacteremic dissemination)
NOT edema |
|
|
All are common complications of pneumoina EXCEPT:
a. tissue destruction and necrosis b. accumulation of fluid c. spread of infection to pleural space d. bacteremic dissemination |
abscess (tissue destruction and necrosis), empyema (spread of infeciton), sepsis (bacteremic dissemination)
NOT edema (accumulation of fluid) |
|
|
A debilitated pt presents in the ED with repeated vomiting, what is a major risk factor in this patient related to his lung function:
a. bronchopneumonia b. lobar pneumonia c. pneumonitis d. aspiration pneumonia |
aspiration pneumonia often in debilitated, unconscius or pt with repeated vomiting
because they have a abnormal gag response and swallowing refelx --> leads to abscess in lung |
|
|
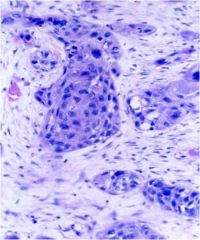
A sarcoidosis is usually a result of increased CD4 cells in the lungs what are common features in the biopsy:
a. caseating granuloma obstructing bronchi b. non-caseating granuloma in many tissues and organs with nodular lesions and invasion into hilar lymph nodes c. non-caseasting granuloma localized in the apex of the lung d. caseating granuloma with nodular lesions on lung and hilar lymph nodes |
non-caseating (hard) granulomas in many tissues and organs with nodular lesions into hilar lymph nodes
|
|
|
Pt presents usually asymptomatic or sob, cough, fever hemotysis, weight loss at risk of leading to pulmonary fibrosis; what are some differentials
a. granuloma (mycobacteria b. fungal infeciton c. berrylliosis d. lobar pneumonia |
granuloma (mycobacteria)
fungal infecitno berrylliosis NOT lobar pneumonia |
|
|
What is the MAJOR risk factor for lung cancer:
a. radon b. asbestos c. smoking d. etoh |
SMOKING
|
|
Keratin production cancer resulting in pearls and intracellular bridges (MICRO) often seen CENTRAL during gross findings:
a. squamous b. adenocarcinoma c. bronchioalveolar type d. small cell |
squamous cell carcinoma
treat with surgery or radiation |
|
this tumor leads to paraneoplastic syndrome releasing PTH leading to hypercalcemia; it's often CENTRAL and produces keratin
a. squamous cell b. adenocarcinoma c. bronchioalveolar type d. small cell |
squamous cell carcinoma
|
|
What is the difference between this cancer and squamous cell carcinoma:
a. keratin production leading to pearls and intracellular bridges b. grows along pre-existing structures c. mucin producing and coin lesions d. central small cells and very aggressive |
mucin producing and coin lesion (adenocarcinoma now the most common due to filters put in cigarettes)
|
|
|
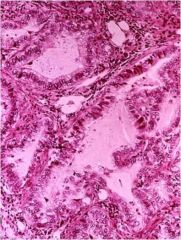
this lung cancer resembles pnuemonia in a CXRAY, it often grows along pre-existing structures (not much damage is caused to alveolar archi)
What is the difference between this cancer and squamous cell carcinoma: a. squmaous cell b. adenocarcinoma c. bronchioalveolar type d. small cell |
bronchioalveolar type
|
|
CENTRAL cells with SCANT cytoplasm and many mitosis, abundant necrosis METASTATIC and very AGGRESSIVE!!
a. squamous cell b. adenocarcinoma c. small cell d. large cell |
small cell carcinoma (NO surgery only radiation and chemotherapy due to risk of metasteses) usually poor prognosis
|
|
In addition to being a very aggressive cancer this action distinguished it from squamous cell carcinoma, although both are paraneoplastic
a. secretes MUCIN b. secretes PTH c. secretes ACTH and ADH d. has no squamous or glandular differentiation |
small cell CA secretes ACTH and ADH, where squamous cell carcinoma secretes PTH
|
|
Pt presents with a low-grade malignancy with neuroendocrine origin, there are no know risk factors
a. squamous cell b. adenocarcinoma c. bronchioalveolar type d. carcinoid |
carcinoid usually presents with GOOD prognosis but can metastosize to the liver
|
|
this low-grade malignancy originates from the bronchi and is often due to no known risk factors can lead to obstruction and is common in < 40y/o non-smokers
a. squamous cell b. adenocarcinoma c. large cell d. carcinoid |
carcinoid
|
|
|
What 2 lung cancers are related to SMOKING:
a. adenocarcinoma b. squamous cell c. small cell d. large cell |
Squamous and Small cell (Smoking)
|
|
|
What lung carcinoma can often lead to Cushing's syndrome due to increase in ACTH
a. adenocarcinoma b. squamous cell c. small cell d. large cell |
small cell carcionma
|
|
|
What lung carcinoma can often lead to hypercalcemia due to increase in PTH
a. adenocarcinoma b. squamous cell c. small cell d. large cell |
squamous cell carcinoma
|
|
|
What lung carcinoma can often lead to hyponatremia due to secretion of ADH?
a. adenocarcinoma b. squamous cell c. small cell d. large cell |
small cell carcinoma
|
|
|
The AMOUNT of particles retained in lungs is usually determined by EXCEPT:
a. [particle] b. duration of exposure c. effectiveness of clearance mechanism d. size of the particle |
[particle], duration of exposure, effectiveness of clearance mechanism, and also mucociliary aparatus (smoking), NOT size of particle
|
|
|
What are the size of MOST dangerous particles and why?
a. 1-5 micrometers b. 5-7 micrometers 7-10 micrometers |
1-5 micrometers because they can reach the terminal small airways and sacs
|
|
|
What cell is responsible for eliminating infiltration into lungs?
a. PMN's b. mast cells c. macrophages d. Tcells |
macrophages pahgocytose infiltrates and dispose of them, however if there are large amounts they can get overwhelmed and interactions b/w cells and chemicals results in more problems
|
|

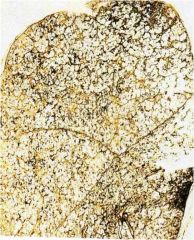
Usually asymptomatic with minimal lung destruction and affects UPPER LOBE; can progress to PMF (progressive massive fibrosis)
a. coal workers pneumoniosis b. asbestosis c. silicosis d. usual interstitial pneumonia |
coal workers pneumoniosis
|
|
This condition varies from asbestos in that:
a. it involves the UPPER lobe b. it involves the LOWER lobe c. it is associated with very long, but thin fibers d. it is the MOST chronic clinical disease |
Coal Workers Pneumoconiosis usually affects the UPPER lobe, while
asbestosis LOWER lobe and is associated with very long, but thin fibers silicosis is the MOST chronic clinical disease |
|
This condition has a strong syndergism with SMOKING and is often affecting the LOWER lobe and penetrates into PLEURAL leading to fibrotic lesions
a. involves blackened scar complexes b. very long, thin fibers c. involves inhalation of crystalline silicone dioxide d. is the MOST chronic occupational diseas |
asbestosis LOWER lobe and penetrates PLEURAL space synergistic with SMOKING
|
|
Pt is diagnosed with the most CHRONIC occupational disease affecting LOWER lobe of lungs as the particles damage epithelial leading to macrophage secretion of IL-1, fibronectin, O2 readicals, and fibrogenic cytokines resulting in Hard, collagenous SCARS; what was the pt exposed to:
a. coal b. asbestos c. dust d. silica |
silica can also be viewed with polarization
|
|
This inhaled particle similar to coal workers pneumoconiosis in that it affects the UPPER lobe, but differs microscopically in what way?
a. results in blackened scar complexes b. infiltration of very long, thin fibers c. results in nodular fibrotic lesions and can be viewed with polarization d. is synergistic with smoking |
results in nodular fibrotic lesions and can be viewed with polarization
|
|
This inhaled product results in pleural plaques as the very long, but thin fibers and penetrate through PLEURAL
a. also synergistic with smoking b. results in blackened scar complexes c. affects the UPPER lobe d. is considered the most CHRONIC occupational disease |
asbestosis also synergistic with smoking
|
|
|
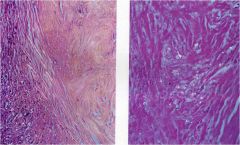
Pt presents with restrictive defects on pulmonary function test, long standing history of smoking. In the past he has not responded well to anti-inflammatory drugs. What is a common mechanism of action of this pathology
a. macrophages phagocytose inhaled particles, but due to an increased of particles there is an overwhelmed response resulting in problems b. increase in proteases damages lung parenchyma resulting in poor PFT results c. chronic inflammation results in fibrosis due to epithelial activation and/or injury d. smoking injuries to epithelial cells and vascular leakage leading to edema |
if it is usual interstitial pneumonitis (idiopathic) then pulmonary fibrosis --> unidentified insult (inhaled agents, blood borne toxins, or unk antigens) activate macrophage resulting in chronic inflammation --> fibrosis "repeated cycles" of epithelial activation and/or injury causing restrictive defect on PFT's
|
|
|
What are 4 common causes of pulmonary fibrosis:
a. interstitial fibrosis b. cryptogenic organizing pneumonia c. malignant mesothelioma d. CT diseases e. pneumoconioses |
interstitial fibrosis
cryptogenic organizing pneumonia (fibroblast balls) CT disease associated (SLE, rheumatoid arthiritis, PSS) Pneumoconioses (air-borne agents) NOT malignant mesothelioma |
|

common finding of a "honeycomb" lung include all EXCEPT:
a. decrease in compliance b. decreased vascular R c. pulmonary HTN d. hypoxemia |
decrease lung compliance, no gas exchange, hypoxemia, increased Vascular R, and pulm HTN
NOT decrease in v.R |
|

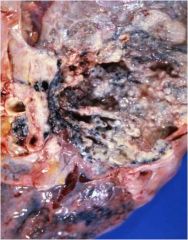
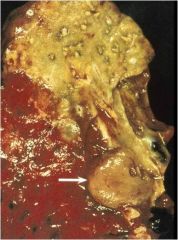
Pt presents with chest pain, dyspnea, recurrent PLEURAL effusion with a history of ASBESTOS exposure
a. malignant mesothelioma b. adenocarcinoma c. reactive pleural fibrosis d. pulmonary harmartoma |
malignant mesothelioma
|
|
|
A 7 year old boy accidentally inhales a small peanut, which lodges in one of his bronchi. A chest x-ray reveals the mediastinum to be shift toward the side of obstruction. Which of the following pulmonary abnormalities is most likely present in this boy?
a. Absorptive atelectasis b. Compression atelectasis c. Contraction atelectasis d. Patchy atelectasis e. Hyaline membrane disease |
absorpiton atelectasis
|
|
|
A 26-year old man barely survives a house fire. He is taken unconscious to the hospital where over the next several days he develops worsening signs of respiratory failure. A chest x-ray on the third hospital day reveals a complete “white-out” of both lungs. Lab evaluation finds severe hypoxemia that does not improve with 100% oxygen. Which of the following histologic changes is most likely to be seen in a biopsy specimen taken from his lungs?
a. Angioinvasive infiltrates of pleomorphic lymphoid cells b. Deposits of need-like crystals from the membranes of eosinophils c. Infiltrating groups of malignant cells having intercellular bridges d. Irregular membranes composed of edema, fibrin, and dead cells lining alveoli e. Plexiform lesions within pulmonary arterioles |
irregular membranes composed of edema, fibrin, and dead cells lining alveoli
|
|
|
While recovering in bed 1 week after an abdominal hysterectomy, a 42-year old woman develops acute shortness of breath with hemoptysis. Physical exam finds the patient to be afebrile with moderate respiratory distress, calf tenderness, and a widely split S2. Which of the following is the most likely diagnosis?
a. Atelectasis b. Bacterial pneumonia c. Pulmonary embolus d. Pulmonary hypertension e. Viral pneumonia |
pulmonary embolus
|
|
|
A 19-year old woman presents with urticaria that developed after she took aspirin for a headache. She has a history of chronic rhinitis, and physical examination reveals the presence of nasal polyps. This patient is at an increased risk for developing which of the following pulmonary abnormalities following ingestion of aspirin?
a. Contraction atelectasis of the lower lung lobes b. Destruction of the alveolar walls c. Fibrosis of the alveolar interstitium d. Mucous plugging of the bronchioles e. Sclerosis of the small blood vessels |
mucous plugging of bronchioles
|
|
|
A 37-year old woman presents with the acute onset of a productive cough, fever, chills, and pleuritic chest pain. A chest x-ray reveals consolidation of the entire lower lobe of her right lung. She unexpectedly dies before treatment due to a cardiac arrhythmia. Histologic examination of lung tissue taken at the time of autopsy reveals multiple suppurative, neutrophil-rich exudates filling the bronchi, bronchioles, and alveolar spaces. The majority of lung tissue from her right lower lung is involved in this inflammatory process. Hyaline membranes are not found. Which of the following is the most likely diagnosis?
a. Bronchiectasis b. Bronchopneumonia c. Interstial pneumonitis d. Lobar pneumonia e. Pulmonary abscess |
lobar pneumonia
|
|
|
44-year old alcoholic man presents with fever and a productive cough with copious amounts of foul-smelling purulent sputum. Physical exam finds that changing the position of this individual produces paroxysms of coughing. Which of the following is the most likely cause of the patient’s signs and symptoms?
a. Esophageal cancer b. Esophageal reflux c. Myocardial infarction d. Pulmonary abscess e. Pulmonary infarction |
pulmonary abscess
|
|
|
7.) A 54-year old man presents with several problems involving his face and pain in his shoulder. He states that he has smoked 2 packs of cigarettes a day for almost 40 years. Physical exam reveals ptosis of his left upper eyelid, constriction of his left pupil, and lack of sweating (anhidrosis) on the left side of his face. No other neurologic abnormalities are found. Which of the following tumors is most likely to be present in this individual?
a. A bronchioloalveolar carcinoma involving the upper lobe b. A small-cell carcinoma involving the hilum of his left lung c. A squamous cell carcinoma involving the left mainstem bronchus d. An adenocarcinoma involving the apex of his left lung e. An endobronchial carcinoid tumor involving the right mainstem bronchus |
an adenocarcinoma involving the apex of the left lung
|
|
|
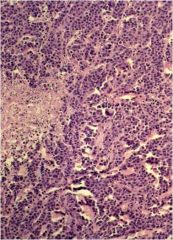
8.) A 67 year old man who is a long-term smoker presents with weight loss, a persistent cough, fever, chest pain, and hemoptysis. Physical exam reveals a cachectic man with clubbing of his fingers and dullness to percussion over his right lower lobe. A chest x-ray reveals a 3.5 cm hilar mass on the right and postobstructive pneumonia of the right lower lobe. Sputum cytology is suspicious for malignant cells. Histologic examination of a transbronchial biopsy specimen reveals infiltrating groups of cells with scant cytoplasm. No glandular structures or keratin production are seen. The nuclei of these cells are about twice the size of normal lymphocytes and do not appear to have nucleoli. Which of the following is the most likely diagnosis?
a. Adenocarcinoma b. Hamartoma c. Large-cell undifferentiated carcinoma d. Small-cell undifferentiated carcinoma e. Squamous cell carcinoma |
small cell undifferentiated CA
|
|
|
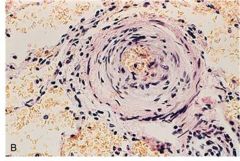
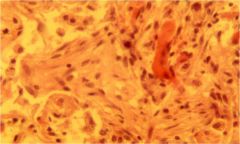
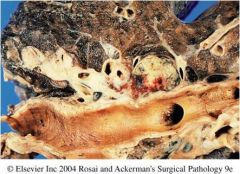
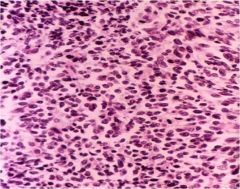
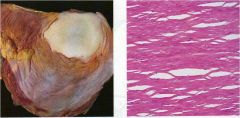
9.) Increasing dyspnea for several years has greatly restricted the physical activity of a 48 year old woman who works as a hairdresser. She otherwise has no major health problems. A chest radiograph reveals a bilateral reticulonodular pattern along with hilar adenopathy. A transbronchial biopsy is performed and shows the findings depicted here microscopically. The most likely diagnosis is:
a. Primary tuberculosis b. Nocardiosis c. Silicosis d. Sarcoidosis e. Berylliosis |
sarcoidosis
|
|
|
10.) A 49-year old man presents with shaking chills and fever, pleuritic chest pain, and increasing shortness of breath. A chest x-ray reveals a right-sided pleural effusion. The lung in this area appears to be consolidated. The pleural fluid is tapped, and lab examination reveals moderate acute inflammatory cells. Which of the following is the basic defect that caused the accumulation of this pleural fluid?
a. Collagen vascular disease involving the pleura b. Obstruction of lymphatics by tumor c. Right-side CHF d. Rupture of aortic aneurysm e. Suppurative infection of adjacent lung tissue |
suppurative infeciton of adjacent lung tissue
|
|
|
A 19 year old woman presents with sudden, severe right-sided chest pain that developed shortly after she had been placing heavy boxes on shelves in the garage. Physical exam reveals an afebrile women in mild respiratory distress. Breath sounds are markedly decreased on the right, and the right lung is hyperresonant to percussion. Which of the following is most likely present in this individual?
a. Pneumoconiosis b. Pneumocystis infection c. Bacterial pneumonia d. Viral pneumonia e. Pneumothorax |
pneumothorax\
|
|
|
A 35-year old woman presents with slowly progressive weakness involving the left side of her face. She says she cannot completely close her left eye. Physical examination finds facial asymmetry characterized by flattening of the entire left side of her face, but no abnormalities are seen on the right side. A 1.5-cm mass is found involving the deep portion of the left parotid gland. At the time of surgery the mass is found to be infiltrating along the facial nerve. What type of lesion does this patient most likely have?
a. Pleiomorphic adenoma b. Warthin’s tumor c. Acinar cell tumor d. Mucoepidermoid carcinoma e. Adenoid cystic carcinoma |
adenoid cystic CA
|

