![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
71 Cards in this Set
- Front
- Back
|
Pt presents with dysphagia and drooling. He complains of regurgitation of food, frequent heartburn, and unexpected weight loss in the past 2 months. What are possible differentials, EXCEPT:
a. esophageal stricture b. PUD c. GERD d. neurological damage |
this pt has dysphagia complaints (difficulty swallowing)
esophageal stricture, GERD and neurological damage are possible causes, PUD would NOT be a cause of dysphagia |
|
|
23y/o pregnant women presents with odynophagia, including a burning sensation during swallowing. This is the most common cause of esophagitis. The pathology reflects the damage, in that the damaged EP reheals with columnar EP cells (goblet cells) rather than the original squamous EP, for protection. What are 3 of the complications, EXCEPT:
a. inflammation b. erosion/ulceration c. intestinal metaplasia Barrett's esophagus d. Mallory Weiss syndrome |
NOT mallory weiss syndrome caused via severe stretching at the GE junction most common in alcoholics
a. inflammation b. erosion/ulceration c. intestinal metaplasia Barrett's esophagus gastric esophagitis occurs due to incompetent lower esophageal sphincter, impaired clearance and impaired mucosal resistance |
|

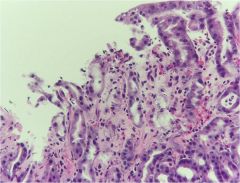
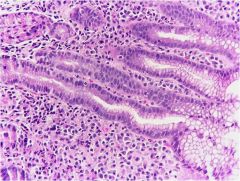
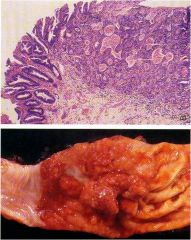
32y/o pt presents with long history of dysphagia and (GERD) resulting in repeated exposure to stomach acid into esophagus resulting in severe damage of cells. There was some hematemasis in the past 24hr. How would you describe MICRO of esophagus?
a. presence of stratified squamous EP b. presence of glandular EP above normal squamocolumnar junction c. presence of cloumnar EP above normal squamocolumnar junction d. presence of squamous EP above normal squamouscolumnar EP |
Incidence of adenocarcinoma in Barrett’s is 30- to 40-fold above the general population (but most pts don’t usually get CA)
note the GOBLET cells present and intestinal metaplasia GET an endoscope quickly |
|

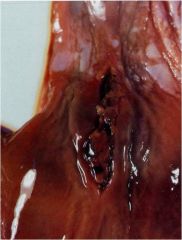
63y/o pt presents to clinic after the abdomen exam you notice caput medusa veins. Pt also complained of black tar stool (melena). After some medical hx, pt states he suffers from cirrhosis!! What is the major cause of his illness:
a. PUD b. GERD c. portal HTN d. CVD |
portal HTN causing esophageal varices
common in pts w/cirrhosis (etoh induced) cause derangement in liver vasculature centers, blood bypasses portal circulation due to liver damage and enters collateral veins: |
|

Often seen in 90% of cirrhotic pt's. Appear as tortuous dilated veins in the esophagus submucosa. What of often the complications that can lead to death.
a. infection b. massive hemorrhage c. malabsorption d. compromised immune system |
massive hemorrhage due to rupture difficult to STOP the bleeding due to high Pressure
|
|
23y/o pregnant female presents complaining of increased morning sickness, she has lost over 10 lbs in the past 2 months due to pregnancy gravidarum or hyperemesis. What is she at increased risk for, if she presents with hematemesis, melena, light-headedness, dizziness, syncope and abdominal pain. Pay attention to this because it can cause DEATH
a. esophageal varacies b. esophagitis c. achalasia d. mallory weiss |
mallory weiss also common in alcoholics due to the increase in vomiting (anything that increases vomiting can result in an increased risk)
esophageal varices -- cirrhosis esophagitis odynophagia achalasia absent peristalsis |
|
13 y/o female recently came from a trip to Brazil. She presents to clinic with dysphagia and complaints of frequent regurgitaiton and aspiration. In addition, mother adds she has "foul breath" for the past few days. Unfortunetly, peristalsis appears to be ABSENT. Although there are 2 common causes of this disease, this case is not due to the primary or most common cause, or changes in innervation, but
a. portal HTN b. hyperemesis c. destruction of myenteric plexus d. barrett's esophagus |
she contracted Chaga (Trypanosoma cruzi while in Brazil) the kissing disease leading to destruction of myenteric plexus causing absent peristalsis
portal HTN -- espophageal varices hyeremesis -- Mallory Weiss barrett's esophagus -- adenocarcinoma |
|
An acute event such as trauma can accompany transient hemorrhage often leading to
a. acute gastritis b. chronic gastritis c. H.pylori infeciton d. reactive gastritis |
acute gastritis important cause of GI bleed
|
|
16y/o pt in the hospital after being saved from his burning home. After several days, he has developed some abdominal ulcerative damage. You suspect there is some GI bleeding and would like to take care of this b/c if resolved it will not lead to scarring. What are some other causes of GI bleed, as the injury is thought to be related to acidic reduced blood flow, disruption in protective mucus, and direct EP damage.
a. shock b. smoking c. chemotherapy d. NSAIDs |
all damage the EP decreasing the bicarbonate buffer or increase secretions leading to acute gastritis
remember the most common complication is GI bleed acute gastritis DOES not result in scarring, atrophy, or metaplasia |
|
|
The presence of chronic mucosal inflammatory changes leading eventually to mucosal atrophy and intestinal metaplasia, usually in the absence of EROSiON!! Often presents with abdominal pain and anemia. What are 3 pathogenesis?
a. cirrhosis b. portal HTN c. Helicobacter pylori d. autoimmune gastritis e. reaction to a toxin (bile, etoh, smoking) |
this is chronic Gastritis due to its absence of erosion
c. Helicobacter pylori d. autoimmune gastritis e. reaction to a toxin (bile, etoh, smoking) |
|
|
This condition leads to complications such as: atrophy of the mucosa resulting in inhibition of acid secretions. In addition, intestinal metaplasia results which predisposes to dysplasia and carcionoma.
a. acute gastritis b. chronic gastritis c. autoimmune gastritis d. reactive gastritis |
complications of chronic gastritis
|
|
|
H. pylori infection is the most common cause of chronic gastritis, recently added to the list of carcinogens due to its link to gastric malignancy. What part of the stomach is predominately affected?
a. fundus b. body c. pyloris d. pyloric sphincter |
fundus to body (upper portion of the stomach on the mucus surface0
|
|
|
Aside from the higher incidence of gastric carcinoma and gastric MALT lymphoma, H.pylori also causes what 2 benign diseases?
a. acute gastritis b. chronic gastritis c. GERD d. PUD |
chronic gastritis and PUD
|
|
|
What is the current GOLD standard for diagnosing H.pylori?
a. endoscope and biopsy b. culture c. rapid urease test d. urea breath test (UBT) |
endoscope and biopsy
|
|
|
Although H.pylori infection moves from intestinal metaplasia, it predominatly focused in what GI tract layer?
a. mucus b. mucosa c. muscularis mucosae d. submucosa |
mucus
|
|
Often slow developing process with lymphocytes and plasma cells and altered mucosal architecture.
a. acute gastritis b. chronic active gastritis c. chronic gastritis d. autoimmune gastritis |
chronic gastritis
|
|

Often a complication of chronic gastritis, may contain H.pylori, but not necessary. NO erosions or shedding of superficial mucosa.
a. acute gastritis b. chronic gastritis c. mucosal atrophy d. chronic gastritis with intestinal metaplasia |
intestinal metaplasia
|
|
|
When would you have neutrophilic inflammation in a chronic gastritis biopsy, such that it should not be confused with acute gastritis?
a. during a systemic infeciton b. during sepsis c. during chronic active gastritis d. during trauma |
during chronic active gastritis
|
|
|
Results from the development of antibodies against gastric parietal cells and intrinsic factor often lead to what complication?
a. gastric carcinoma b. gastric MALT lymphoma c. reactive gastritis d. pernicious anemia |
autoimmune gastritis can lead to pernicious anemia due to lack of B12 (due to loss of intrinsic factor)
|
|
|
Which pair is wrong, involved in the function of absorption?
a. pancreas (digestive enzymes) b. stomach (pepsin) c. liver (bile) d. small intestine (brush border) |
stomach (pepsin) --> not really involved in absorption; all other are vital to achieve proper absorption:
pancreas (digestive enzymes), liver (bile), and small intestine (brush border) |
|
|
Pt presents with increased difficulty in absorbing vital vitamins, proteins and carbohydrates, all can be affected EXCEPT:
a. cystic fibrosis b. biliary obstruction c. pancreatic cancer d. H.pylori infection |
H.pylori infection will not lead to malabsorption, but rather chroinic gastritis or PUD, also malignancy
chronic pancritis, pancreatic CA, and cystic fibrosis all affect the pancrease, while biliary obstruction or impaired bile excretion affect malabsorption due to ineffective bile salts |
|
|
These parasites are associated with malabsorption, EXCEPT:
a. Giardia lamblia b. Necator americanus (hookworm) c. H.pylori d. Strongyloides stercoralis |
EXCEPT H.pylori
|
|

Most common surgical condition of the GI tract. Often associated with 50-80% obstruction, usually a fecalith (piece of poop). It is infiltrated via PMN's especially in mucosa. As the inflammatory process worsens, ulceration and supperative necrosis occurs.
a. hernia b. adhesions c. intussusception d. appendicitis |
appendicitis
|
|

23y/o female presents to clinic complaining of fever, pain, dysentery several days ago. She recently finished a treatment of antibiotics for tuberculosis. You go on to seek the toxin. What organism was allowed to overgrow after the use of antibiotics resulting in damage of intestines, due to lack of protection from bacteria.
a. E. Coli b. Campylobacter jejuni c. Clostridium difficile d. Shigella |
she has pseudomembranous colitis
Clostridium difficile, antibiotic use is notorious for causing this due to the sweep of bacteria from intestine leading to minimal protection from C.d sitting there like a watch dog for bacteria to be removed!! |
|
|
Three most common causes of malabsorption in the US are?
a. Giardia lamblia infection b. Celiac sprue c. chronic pancreatitis d. crohn disease |
b. Celiac sprue
c. chronic pancreatitis d. crohn disease bacterial infection with giardia can cause malabsorption but is not the most common cause |
|
|
Melena and hematochezia are important clinical for differential diagnosis, why?
a. result in dysentery b. occur frequently in most GI diseases together c. provide a distinction between UGI and LGI bleed d. are only prevalent in erosive conditions |
provide a distinction b/w UGI and LGI for example melena is common in mallory weiss while hematochezi is common in chron's dx
|
|
|
Melena is common in all, EXCEPT:
a. Mallory Weiss b. gastric/duodenal erosions c. erosive esophagitis d. colonic polyps |
colonic polyps results in hematochezia (LGI bleeding)
|
|
|
Hematochezia is common in, EXCEPT:
a. erosive esophagitis b. colitis c. diverticular dx. d. croh's dx |
erosive esophagitis results in melena (UGI bleeding)
|
|
|
in order to distinguish Crohn's disease and ulcerative colitis, the GI involvement is important as well as, for distinction:
a. cause melena or hematochezia b. pattern of inflammatory changes c. absence of neutrophiles d. inflammatory components involved |
pattern of inflammatory changes
|
|

35y/o femal presents with crampy abdominal pain and dysentary. After several tests and review of micro you notice granulomatous TRANSMURAL inflammation as well as SKIP lesions through the GI tract. There are also protusions or fistuals throughout. What is another vital aspect of this disease.
a. affects only the large intestine b. affects only the duodenum c. affects through the mouth --> anus d. affects only the colon and stomach |
affects mouth --> anus
Pt has Crohn's disease due to transmural inflammatory inflammation and skip lesions. |
|

34y/o female comes in complaining of crampy abdominal pain and dysentary. In addition, after gathering more information from endoscopy. You observe a THIN bowel wall. The inflammatory disease has this distinguishing feature.
a. skip lesions b. extends from mouth to anus c. localized to rectum d. transmural inflammation |
pt has ulcerative colitis
localized to RECTUM, all the other relate to Croh's disease remember that ulcerative colitis has an increased risk of adenocarcinoma and toxic megacolon (rare) |
|
has a high risk of adenocarcionoma, often confined to the colon. What are other complications?
a. skip lesions b. granulomatous transmural inflammation c. fistulas d. pseudopolyps |
ulcerative colitis:
pseudopolyps, toxic megacolon, neutrophiles in crypts all other describe Crohn's disease |
|
Inflammatory bowel disease often results in granulomatous transmural inflammation, and what other distinguishing factors;
a. psuedopolyps b. neutrophiles c. skip lesions d. risk for adenocarcinoma |
skip lesions are common in crohn's disease, while all the other are common in ulcerative colitis
|
|

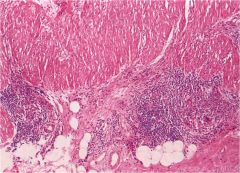
65y/o male presents with LLQ abdominal pain and constipation with intermiettent cramping. You suspect weakness in the muscularis propria and increased intraluminal pressure. This disease LOVES the SIGMOID colon. What are 3 complications?
a. inflammation and microabscess b. adenocarcionoma c. obstruction d. hemorrhage |
infammation and microabscess due to perforation; obstruction due to muscular hypertrophy; hemorrhage erosion resulting in blood stool
|
|
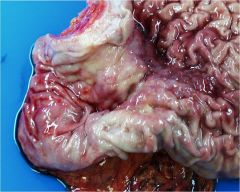
65y/o male presents with LLQ abdominal pain and constipation with intermiettent cramping. You suspect weakness in the muscularis propria and increased intraluminal pressure. This disease LOVES the SIGMOID colon. What is the complication seen on screen/
a. inflammation and microabscess b. adenocarcionoma c. obstruction d. hemorrhage |
hemorrhage erosion results in blood in stool
|
|
|
50-70% complications of Ischemic bowel obstruction results from:
a. vascular obstruction b. arterial thromboses c. arterial embolism d. sepsis |
SEPSIS
|
|
|
What can result in arterial thromboses leading to ischemia of the gut, EXCEPT?
a. atherosclerosis b. dissecting aneurysm c. hypercoagulative state d. embolism |
embolism is vascular occlusion
|
|
|
hyeprcoagulative states and cirrhosis can lead to this type of vascular compromise?
a. arterial thrombosis b. arterial embolism c. venous thromboses d. vascular occlusion |
venous thromboses
|
|
|
Why are bowel infarctions important to diagnose, as there is necrosis of the bowel wall with subsequent SEPSIS and peritonitis?
a. hypercoagulation b. internal bleeding c. 50-70% death rate d. medical emergency |
50-70% DEATH rate!!
|
|
|
Hernias are pouch like sacs of peritonium that may protrude through a weak spot in the peritonium. There are two types including incarcerated which leads to permanent trapping. What is the other type?
a. adhesions b. intussusception c. volvulus d. strangulation |
strangulation leading to necrotic end if the pressure at the neck of the pouch impairs arterial blood flow and venous drainage, the bowel segments may infarct
|
|
Pt had a surgery near peritonium about 2 years ago, often results in fibrous tissue due to healing process. Now loops of bowel have become entangled in the fibrous tissue leading to obstruction and infarction. Possible complications include, SEPSiS due to obstructed blood supply.
a. hernia b. adhesions c. intussusception d. volvulus |
adhesions
|
|

Common in children often can give them a barium edema or surgery for treatment. This occurs when
a. pouch like sac of peritonium may protrude through weak spot in peritonium b. sites of intraperitoneal inflammation or surgery scarring, form b/w loops of bowel c. one segment of intestine telescopes into the distal segment of bowel d. a loop of bowel may become twisted about its mesenteric base causing obstruction and possible necrosis |
one segment of intestine TELEScOPES into the distal segment of bowel common in children
|
|
|
Smoking and HPV are often risk factors for this type of cancer found in the oral cavity?
a. columnar b. small cell c. squamous d. neuroendocrine |
squamous cell carcinoma common in oral cavity risk factors include smoking and HPV
|
|
|
Often see Barrett's adenocarcinoma in the esophagus, what are the normal histological cells lining the esophagus?
a. squamous b. ciliated epithelium c. stratified epithelium d. columnar |
squamous leading to squamous cell carcinoma
|
|
|
Mos common cancer in the colon, includes?
a. squamous cell b. small cell c. adenocarcinoma d. carcinoid |
adenocarcinoma
|
|
|
What are the normal histological cells lining the colon leading to adenocarcinoma?
|
columnar
|
|
|
HPV is also associated with a squamous cell carcinoma in what location?
a. oral b. esophagus c. rectum d. anus |
anus (squamous cells)
|
|
|
HPV is associated with 2 organs leading to squamous cell carcinoma?
a. oral and esophagus b. oral and anus c. colon and rectum d. oral and small bowel |
remember HPV is going to affecct squamous cells, so these are found in oral, esophagus, and anus; but HPV has greater ascess to oral and anus due to its prevalence of infliction as an STD
|
|
|
The behavior of this cancer is highly dependent on the location, frequently affecting columnar cells?
a. squamous cell carcinoma b. adenocarcinoma c. carcinoid d. lymphoma |
carcinoid often of neuroendocrine origin can be found in the appendix
|
|
|
Prognosis is related to stage in GI tumors.
a. true b. false |
true (staging is vital in the prognosis of tumors)
size of the tumor, whether the cancer is invasive or non-invasive, whether lymph nodes are involved, and whether the cancer has spread. The purpose of the staging system is to help organize the different factors and some of the personality features of the cancer |
|

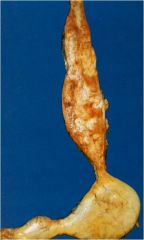
33y/o pt presents with dysphagia and pain. Pt also has a hx of long standing esophagitis with complaints of dysphagia, odynophagia, N/V, and chest pain. Upon further history pt admits to a hx of smoking for the past 10yrs. You are concerned if the disease is cancer it has extended into the mediastinum, as staging is the most important predictor of survival in this case.
|
a. adenocarcionoma (may be due to gastroesophageal reflux or barrett esophagus)
b. squamous cell carcinooma YES!! common in smoker and alcohol users, can begin as in situ but when it is diagnosed it is often too late; and yes staging is the best predictor of prognosis in this case!! c. carcinoid (endocrine origin, usually with columnar origin found commonly in the appendix) d. lymphoma (NO) |
|
|
Squamous cell carcinoma of esophagus often diagnosed in an advanced stage as it is locally extended into mediastinum (due to lack of serosa of the esophagus). Has a 5% (5year survival). What environmental factors are strongly implicated?
a. high fat diet b. increased stress c. H. pylori d. smoking |
smoking for sure !!
|
|
Squamous cell carcinoma of esophagus often diagnosed in an advanced stage as it is locally extended into mediastinum (due to lack of serosa of the esophagus). Has a 5% (5year survival). What environmental factors are strongly implicated?
a. high fat diet b. increased stress c. H. pylori d. smoking |
smoking for sure !!
|
|
often associated with Barrett's esophagus, due to its long standing complication of gastroesophageal reflux. What striking structures in esophagus are potential identifiers:
a. squamous EP b. columnar EP c. glands d. neuroendocrine cells |
GLAND (not normal) in esophagus
remember the risk of developing adenocarcinoma in pts with Barretts esophagus is X30-40 fold greater than that of the general population remember STAGE predicts survival here again treatment would be surgery |
|
There is a lower incidence of gastric carcinoma in the US, although there is an increased risk with H.pylori infection and in pts with what?
a. chronic atrophic gastritis b. Barrett's esophagus c. PUD d. hx smoking |
a. chronic atrophic gastritis YES
b. Barrett's esophagus (esophageal adenocarcinoma) c. PUD d. hx smoking (esophageal sq cell carcinoma) |
|

Early patterns of gastric carcinoma result in good prognosis, while advanced patterns resulting in ulceration (localized), mass, and penetration through what layer of the stomach is avoided, often have a limited 5 year survival rate (<10%). Here the pt would present with a very thick stomach cell wall (like a leather bottle)
a. serosa b. muscularis propia c. submucosa d. mucosa |
all the layers are infiltrated EXCEPT
a. serosa (NO this is the outer layer) b. muscularis propia YES c. submucosa YES d. mucosa YES |
|

Familial polyposis syndrome, hereditary nonpolyposis, and what other condition predisposes colon adenocarcinoma:
a. spru b. PUD c. H.pylori d. ulcerative colitis |
ulcerative colitis
|
|

Pt presents with a history of ulcerative colitis. Pt has been anemic for the past year. She is given iron pills. You are concerned that the malignancy has metastasized to the liver, as the grade of the malignancy is the best determinant of the prognosis. What other factor is common in this type of colon adenocarcinoma?
a. obstruction b. NO obstruction c. apple core lesion d. formed stools |
RIGHT sided adenocarcinoma --> NO obstruciton, all the other describe a LEFT sided colon adenocarcinoma
|
|

Pt complaining of constipation due to some constriction. Pt has a hx of familial polyposis syndrome placing them at high risk for colon adenocarcinoma. What is an identifier as to location R/L side?
a. NO obstruction b. obstruction c. fungating especially in cecum d. slow bleeding |
obstruction leading to the constipation
|
|
Although CEA is NOT a screening test for colon adenocarcinoma it is often elevated in colon CA. What is its use?
a. guides treatment b. guides preventative measures c. identifies colon adenocarcinoma d. monitor disease progression |
monitor disease progression based on baseline levels
|
|

Carcinoids are common throughout the GI tract, their level of aggressiveness depends on the location. Which location results in less frequent metastases risk?
a. ileal b. appendix c. gastric d. colon |
the figure shows the ileal high metastasis which can lead to bowel obstruction as well
ileal, gastric, colon (frequent metastases to lymph nodes) while appendix and rectum result in infrequent metastasis |
|
|
41-year-old man has a history of drinking 1 to 2 liters of whisky per day for the past 20 years. He has had numerous episodes of nausea and vomiting in the past 5 years. He experiences a bout of prolonged vomiting, followed by massive hematemesis. On physical examination in the emergency room, he has vital signs with T 36.8 C, P 110, RR 22, and BP 80/40 mm Hg. His heart has a regular rate and rhythm with no murmurs and his lungs are clear to auscultation. There is no abdominal tenderness or distension and bowel sounds are present. His stool is negative for occult blood. Which of the following is the most likely diagnosis?
a. Hiatal hernia b. Esophageal laceration (Mallory-Weiss syndrome) c. Esophageal pulsion diverticulum d. Barrett esophagus e. Esophageal squamous cell carcinoma f. Esophageal stricture |
esophageal laceration (Mallory-Weiss syndrome
|
|
|
58-year-old man has had increasing difficulty swallowing for the past 6 months. He has lost 5 kg in the past 2 months. No abnormal physical examination findings are noted. Upper GI endoscopy reveals a nearly circumferential mass with overlying ulceration in the mid esophageal region. Biopsy of the mass reveals pink polygonal cells with marked hyperchromatism and pleomorphism. Which of the following is the most likely risk factor for development of his disease?
a. Iron deficiency b. Helicobacter pylori infection c. Chronic alcoholism d. High fruit diet e. Zenker diverticulum |
C, chronic alcoholism this is a description of squamous carcinoma of the esophagus
|
|
|
40-year-old man has had mid epigastric pain and nausea for the past 2 months. On physical examination he has no abnormal findings. On upper GI endoscopy a solitary sharply demarcated 2-cm shallow gastric antral ulcer is seen. Which of the following is most likely to be present in this man?
a. Gastric achlorhydria b. Positive serology for antinuclear antibody c. Positive urea breath test d. Increased plasma cortisol e. Elevated serum gastrin |
positive urea breath test
|
|
|
23-year-old primigravida gives birth at term following an uncomplicated pregnancy to a male infant with no apparent congenital anomalies. At 2 weeks of age the infant begins to exhibit forceful vomiting after each meal. The infant had been fine previously and gaining weight normally. Which of the following conditions is the probable cause for his vomiting:
a. Congenital duodenal atresia b. Necrotizing enterocolitis c. Mallory-Weiss syndrome d. Hirschsprung disease e. Tracheo-esophageal fistula f. Pyloric stenosis |
pyloric stenosis
|
|
|
25-year-old man complains of a low volume but chronic, foul smelling diarrhea for the past year. He has no nausea or vomiting. On physical examination there is no abdominal pain or masses and bowel sounds are present. His stool is negative for occult blood. Laboratory studies include a quantitative stool fat of 10 g/day. Upper GI endoscopy is performed with biopsies taken of the duodenum, and on microscopic examination show absence of villi, increased surface intraepithelial lymphocytes, and hyperplastic appearing crypts. Which of the following therapies is most likely to be useful for this man?
a. Antibiotics b. Gluten-free diet c. Selective vagotomy d. Corticosteroids e. Segmental duodenal resection f. Aromatherapy |
Gluten free diet
|
|
|
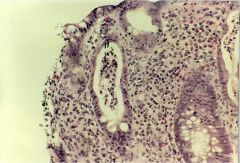
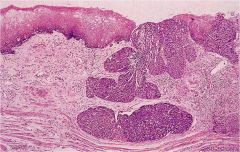
42 year old male has had episodes of substernal burning pain following meals. He has no nausea or vomiting. A stool guaiac is negative. An upper endoscopy is performed, and there are regions of the lower esophagus that appear erythematous. The microscopic appearance of a biopsy of the lower esophagus is seen here. The most likely etiology for this finding is:
a. Gastroesophageal reflux disease b. CREST syndrome c. Helicobacter pylori infection d. Chronic alcoholism e. Corticosteroid therapy |
GERD
|
|
|
51-year-old man comes to his physician for a routine examination. There are no abnormal physical examination findings except for a stool sample positive for occult blood. Colonoscopy is performed and there is a 1 cm polyp on a narrow stalk located in the descending colon at 30 cm from the anal verge. The polyp is resected and on microscopic examination shows crowded, tubular, atypical colonic-type glands. The stalk of the polyp is covered with normal colonic epithelium. Which of the following is the most likely diagnosis?
a. Adenomatous polyp b. Inflammatory fibroid polyp c. Peutz-Jeghers polyp d. Ulcerative colitis e. Hyperplastic polyp f. Crohn disease |
adenomatous polyp
|
|
|
39-year-old woman has experienced substernal burning pain following meals for the past 15 years. On physical examination there are no abnormal findings. Upper GI endoscopy is performed and there are 1 to 3 cm long tongues of erythematous mucosa extending from the gastroesophageal junction at the Z line upward into the lower esophagus. Biopsies are performed of this region and microscopic examination shows areas of gastric cardiac-type mucosa and intestinalized mucosa. Which of the following interpretations is most appropriate for this woman's findings?
a. She has a congenital anomaly b. Her risk for squamous cell carcinoma is increased c. She has chronic gastroesophageal reflux d. Formation of a diverticulum may occur e. She has iron deficiency anemia f. Her anti-centromere antibody test is positive g. Her consumption of alcohol is high |
she has chronic gastroesophageal reflux
|
|
|
45-year-old man has had malabsorption for the past year associated with a low volume diarrhea. He also has a polyarthritis and complains of occasional visual hallucinations. On physical examination there are no joint deformities. A stool sample is negative for occult blood. An abdominal CT scan reveals no masses, only generalized lymphadenopathy. On upper GI endoscopy, there are no esophageal or gastric lesions, but there are broad, flattened villi in the duodenum. Biopsies of the duodenum reveal numerous PAS-positive macrophages in the submucosa. Which of the following therapies is most likely to be useful for this man?
a. Gluten-free diet b. Corticosteroids c. Antibiotics d. Segmental duodenal resection e. Antacids f. Aromatherapy |
Antibiotics due to Whipple disease
|
|

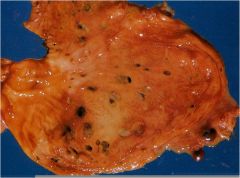
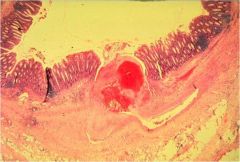
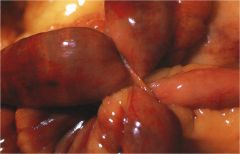
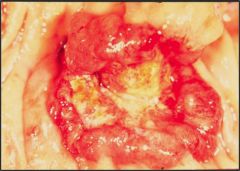
gross appearance of the colonic mucosa seen here in a 54 year old male with abdominal pain, fever, and diarrhea seen several weeks into a hospital stay marked by persistent pneumonia requiring broad spectrum antibiotic therapy is most characteristic for:
a. Ulcerative colitis b. Pseudomembranous colitis c. Acute infarction d. Candidiasis e. Crohn's disease |
pseudomembranous colitis
|

