![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
125 Cards in this Set
- Front
- Back
|
What is the critical measure that can lead to ICP?
a. > 100 mm h2o b. > 200 mm h2o c. > 300 mm h2o d. > 400 mm h2o |
> 200 mm h2o or 15mmHg
|
|
|
All of the above are space occupying lesions leading to complications EXCEPT:
a. cerebral edema b. hyrocephalus c. cerebral ischemia d. ventricular obstruciton |
cerebral edema, hydrocephalus, and ventricular obstruction --> lead to increase in ICP
NOT cerebral ischemia |
|
|
Pt presents with cerebral tumor or cerebral abscess, what type of cerebral edema can present?
a. vasogenic b. cytotoxic c, interstitial d. peripheral |
vasogenic -- fluid in ECS due to damaged capillaries leading to increased vascular permeability
|
|
|
Neonate presents with congenital abnormality leading to hemorrhage in the entire ventricular system, what kind of hydrocephalus?
a. noncommunicating b. communicating c. ex vaco d. no pressure |
communicating due its affect on the ENTIRE ventricular system
|
|
|
After review of an MRI you notice portions of ventricles enlarged due to CSF overproduction or decreased resorption, what kind of hydorcephalus?
a. noncommunicating b. communicating c. ex vaco d. no pressure |
communicating due to overproduction or decreased resroption of CSF
|
|
|
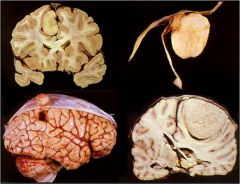
A 82 y/o male suffering from Alzheimer's disease suffers from atrophy of the brain resulting in what type of hydorcephalus?
a. noncommunicating b. communicating c. ex vaco d. normal pressure |
hydrocphalus ex vaco due to atrophy of the brain structures
|
|
|
This hydrocephalus develops SLOWLY and can be due to unknown causes, head injury, meningitis, and stroke what is a possibility:
a. noncommunicating b. communicating c. ex vaco d. normal pressure |
normal pressure hydrpcephalus due to excess accumulation of CSF as a result of decrease in CSF resorption
Dementia Urinariy incontinence Gait ataxia |
|
|
Pt presents with headache, confusion, and papilledema, what can be problematic in the brain?
a. hydrocephalus b. herniation c. meningitis d. tumor |
herniation due to compression of gyri and flattened brain surfaces
|
|
|
This herniation compresses the ACA, forcing the cingualte gyrus under falx cerebri?
a. subfalcine b. unicate c. cerebellar d. transcalvarial |
subfalcine (cingulate) herniation
|
|
|
You notice pt presented with dilated pupils on the side of the lesion after viewing a herniation on an MRI?
a. subfalcine b. unicate c. cerebellar d. transcalvarial |
unicate or transtentorial leading to compression of CNIII (occulomotor) resulting in pupil dilation on the side of the lesion
|
|
|
This herniation leads to compression of medulla structures increasing the risk for respiration and cardiac problems?
a. subfalcine b. unicate c. cerebellar d. transcalvarial |
cerebellar (tonsil)
|
|
|
a spontaneous hemorrhage in the pons, durte can lead to these 2 types of herniations?
a. subfalcine b. unicate c. cerebellar d. transcalvarial |
unicate (transtentorial) and cerebellar (tonsile)
|
|
Neonate presents with neck stiffness, fever and irritability.
lab: CSF turbid, > protiens, < glucose and some neurtophiles a. bacterial meningitis (acute) b. lymphocytic meningitis (acute) c. fungal meningitis d. brain abscess |
acute bacterial meningitis
|
|
spontaneous hemorrhage in pons leading to transtentorial herniatin (cerebellar) or foramen magnum herniation (tonsilar)
a. durte hemorrhage b. subarachnoid hemorrhage c. subdural hemorrahge d. intracranial hemorrhage |
durte hemorrhage
|
|
|
Results in acute bacterial meningitis in infants and children?
a. EColi b. HInfluenza c. NMeningitis d. Pneumococcus |
H. INfluenza
|
|
|
Common cause of acute bacterial meningitis in adolescents and young adults?
a. E.Coli b. H. Infliuenza c. N. Meningitis d. Pneumococccus |
N. Meningitis
|
|
|
Pt presents with headache, mental confusion and vomiting what is a possible pathogen of chronic bacterial meningitis?
a. E. Coli b. H. Influenza c. Tuberculosis d. Pneumococcus |
TB
|
|
|
Pt presents with these lab results:
clear CSF, normal glucose, and lymphocytes? a. acute meningitis b. chronic meningitis c. acute lymphocytic meningitis d. fungal meningitis |
acute lympocytic meningitis more subtle symptoms due to a viral infection (ECHO, mumps, Coxsackie, EPB, and Herpes)
|
|
|
This is an opportunistic infection often high risk for HIV/AIDS pts. leads to "soup bubbles
and tissue destruction a. acute meningitis b. chronic meningitis c. acute lymphocytic meningitis d. fungal meningitis |
fungal meningitis (crytococcus)
|
|
|
This virus usually affects the spinal cord and cerebellum in elderly and ICP's. Usually presents as asymptomatic or fever with flu-like symptoms.
a. west nile virus b. hepres virus c. poliomyelitis d. rabies |
west nile virus
|
|
|
Adult pt presents with aphasia, behavioral disturbances, convulsions, disorientation, and can possibly lead to coma, what caused this encephalitis?
a. viral entering to spinal cord and cererbellum b. viral entry through tirgeminal and olfactory nerves c. viral entry into LMN (anterior horn) d. cerebellum inclusion bodies |
herpes type I (adult) viral entering through trigeminal and olfactory nerves
|
|
This syndrome can reactive in 25-30 yrs. often presents in LMN (anterior horn of spinal cord) can lead to flaccid paralysis of muscles. starts in the BS --> respiratory failure
a. west nile virus b. herpes c. poliomyelitis d. rabies |
poliomyelitis
|
|
|
Aseptic meningitis is common in pts with
a. HIV b. syphillis c. Herpes d. Spongioform E |
HIV slow virus (latent period)
|
|
|
Pt presents with meningio-vascular encephalitis at the base of the brain, normally presents in tertiary stage.
a. HIV b. syphillis c. Herpes d. spongioform E |
syphillis
|
|
|
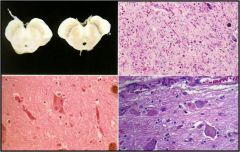
This results in Creutzfelt-Jakob disease resulting in degenerative changes in cerebral and cerebellar cortex. What are the changes seen:
a. PrP protiens in neurons undergo confirmational changes b. multiple demyelinated ares result from viral inclusions c. cognitive decline from spasticity of extremities d. general paresis |
transmissable spongioform E results from PrP (prion protein) conformational changes
|
|
|
Leads to a dissolution of cognitive function --> cerebellar ataxia, muscle fasiculations with myoclonic jerks, often called Creutzfelt Jakob disease:
a. PrP protiens in neurons undergo confirmational changes b. multiple demyelinated ares result from viral inclusions c. cognitive decline from spasticity of extremities d. general paresis |
PrP confirmational changes
|
|
|
The only abnormality in CSF that presents with TURBID appearance and neutrophils:
a. encephalitis b. bacterial meningitis c. viral meningitis d. brain abscess |
bacterial meningitis
|
|
|
These two conditions present with low glucose, but to differentiate them you must look at cultures:
a. encephalitis b. bacterial meningitis c. viral meningitis d. tuberculour meningitis |
b and d
bacterial meningitis (Gram stain) mycobacterial culture |
|
|
These two conditions present with lymphoctyes in CSF and only what can differentiate them?
a. encephalitis b. aicd fast c. bacterial culture d. viral culture |
encephalitis and viral meningitis both have LYMPHoctyes can be differentiated with viral culture
encephalitis (+ 30%), while in viral meningitis (+ 70%) |
|
|
What can help you distinguish viral and bacterial meningitis?
a. gross appearance of CSF b. glucose c. cells d. protein content |
all components
bacterial viral turbid clear > protein slight protein < glucose norm glucose neurtos lymphos |
|
|
This condition may present with very high pressure and elevated protein, as well as occasionally positive bacteria?
a. encephalitis b. bacterial meningitis c. viral meningitis d. brain abscess |
brain abscess
|
|
|
What are common causes of cerebral vascular disease, an acute abnormality of the brain caused by pathological processes of blood vessels:
a. thrombosis b. embolus c. hemorrhage d. edema |
thrombus
embolus hemorrhage |
|
|
A CVD often seen in the carotid bifurcaitons, origin of MCA, or on either end of the BA can be due to
a. cardiac mural thrombi b. hemorrhage c. atherosclerosis d. ischemia |
atheroscloerosis (thrombosis) from DM or HTN
|
|
|
Common site of embolus or hemorrhage due to reperfusion of collateral blood vessels in the cerebral vasculature
a. BA b. carotid bifurcation c. MCA d. origin of MCA |
MCA (embolus)
|
|
|
Results in a pale appearance in the brain often due to vasculitis, hypercoagulable states, and drug abuse:
a. thrombosis b. embolus c. hemorrhage d. meningitis |
thrombus
|
|
|
What happens when blood flow is reduced/ischemia in the cortex. survival depends on:
a. time and location of damage b. primarily on the area of damage c. availability of collateral circulation and duration of flow d. level of obstruction |
survival depends on availability of collateral circulation and duration of reduction of flow
|
|
|
What is global ischemia clinically ?
a. embolic occlusion b. thromotic arterial occlusion c. caridac arrest d. vasculitis |
cardiac arrest (also shock and hypotension, CO intoxication) if present for a long period of time can lead to tissue damage and brain death
all the other options (embolic or thrombotic arterial occlusion, vasculitis can lead to localized ischemia |
|
|
What kind of ischemia is often seen with strokes
a. generalized b. localized |
localized due to arterial occlusion with central core (low perfusion) surrounded via area of dysfunction caused by metabolic and ionic disturbances
|
|
|
This is referred to as an area at risk, but can be salvaged if reperfusion therapy is rapid and successful?
a. central core b. penumbra c. local ischemia d. periphery circle |
penumbra often becomes smaller and smaller with increased damage once structural integrity is compromised
|
|
|
Results from a generalized reduction of perfusion, resulting from cardiac arrest, shock, hypotension, and CO intoxication:
a. global ischemia b. localized ischemia c. embolic occlusion d. thrombotic arterial occlusion |
global ischemia
|
|
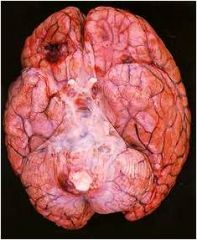
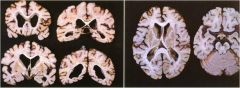
Thrombosis in internal carotid artery leading to massive infarct of MCA and ACA, what are the two factors that lead to mass effect seen in the figure:
a. edema and increase in ICP b. hydrocephalus and increase in ICP c. edema and hemorrhage d. hemorrhage and increase in ICP c. |
edema and hemorrhage
|
|
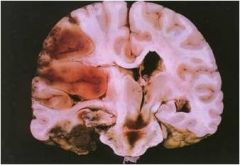
This condition is often secondary to increase in ICP due to edema, causing brain to be forced downward to foramen magnum
a. unciate herniation b. cingulate herniation c. hemorrhage of duret d. thrombus of MCA |
hemorrhage of duret
|
|
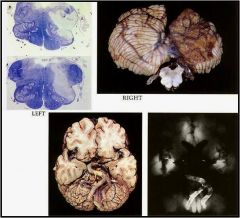
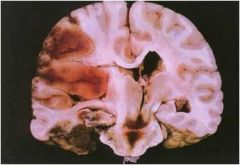
Where is the infarct ?
a. ICA b. basilar aretry c. MCA d. ACA |
basilar artery as a result of thrombosis
|
|
|
Can lead to localized ischemia with penumbra occlusion of MCA
a. infarct b. embolism c. thrombus d. hemorrhage |
thrombus of MCA
|
|
|
Two major medical conditions that put pts at risk for strokes?
a. Diabetes b. CHF c. renal failure d. HTN |
DM and HTN
|
|
|
What is a vital measure that reduces the risk for strokes?
a. treating HTN with medications b. exercise c. diet d. thrombolysis |
thrombolysis when treated within 3 hours of onset
|
|
|
Cerebral infarcts can be described as complete and incomplete occlusions, which affects proximal more than distal portions, sparing the distal due to what kind of reserve?
a. complete occlusion, collateral circulation b. incomplete occlusion, no collateral circulation c. incomplete occlusion, collateral circulation d. complete occlusion, no collateral circulation |
complete occlusion with distal spared as it receives collateral circulation
|
|
|
In an incomplete occlusion the distal is more occluded when compared to proximal, why?
a. due to collateral circulation in proximal portion b. last field of integration recieves the least supply and the flow changes is not enough to open collateral circulation c. distal is the greatest affected via the infarct d. proximal is not affected via infarct |
in an incomplete occlusion the distal > proximal portion because the last field of irrigation receives the least supply and the flow change is not enough to pen collateral circulation
|
|
|
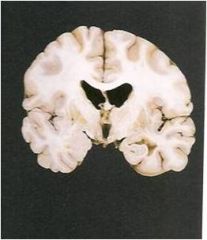
Occluding the striate arteries of MCA causes an infarct in what structures and what clinical implications?
a. basal ganglia and caudate; hemiplegia b. basal ganglia and internal capsule; hemiplegia c. caudate nuclesu and internal capsule; hemiplegia d. globus pallidus and putamen; hemiplegia |
basal ganglia and internal capsule leading to hemiplegia; after 10d infarct undergoes liquefaction necrosis with the development of cystic activity in 1-2 months
|
|
Most common cause of this conditions (embolus)?
a. valbular disease (endocarditis) b. cardiac mural thrombi c. carotid artery thrmobosis d. athertosclerotic emboli |
most common cause of a embolus as noted in the figure is cardiac mural thrombi -- the others are also causes but not most common
|
|
|
A pt presents with sudden focal neurological deficits that last a short period of time but suddenly up to 24 hrs. Usually at the MCA. This sounds like a TIA (transient ischemic attach) common due to:
a. cardiac mural thrombi b. valbular disease c. carotid artery complicated artherosclerosis d. atherosclerotic emboli |
d. atherosclerotic emboli leads to TIA (transient ischemic attack) you may also notice an imbalance, dysphasia, dysarthria, mononuclear blindness, circumoral numbness or hemiparesthesia or hemiparesis (mini stroke or warning stroke)
|
|
|
Arterial aneurysms are common 30% in all of the listed arteries, EXCEPT
a. internal carotid b. anterior communicationg c. middle cerebral d.l verterbrobasilar |
all are 30% except the vertobrobasilar 10%
|
|
|
What is the major cause of a SUBARACHNOID meningeal hemorrhage?
a. arteriovenous malformation b. intraparenchymal cerebral hemorrhage c. intracranial arterial aneurysm d. lacunar infarct |
intracranial arterial aneurysm or localized saccular dilation resulting from medial wall defect, artherosclerosis, or berry aneurysm
|
|
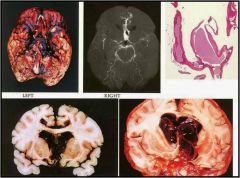
Pt presents with sudden onset of SEVERE headache and collapses, what is the condition
a. arteriovenous malformation b. intraparenchymal cerebral hemorrhage c. intracranial arterial aneurysm d. lacunar infarct |
intracranial arterial aneurysm causing a SUBARACHNOID hemorrhage
|
|
|
Although both intracranial arterial aneurysm "berry" and arteriovenous malformations both result in SUBARACHNOID hemorrhage what is a major difference occurring in arteriovenous malformations?
a. due to the lack of capillary networks you will notice spontaneous rupture b. clinical sign is a sudden onset of severe headache c. vasospasms of adj vessels cause further ischemia d. damage is due to medal wall defects and artherosclerosis |
arteriovenous malformation is vascular clusters that form direct arteriovenous shunts w/out intrermediary capillaries leading to spontaneous rupture --> SUBARACHNOID hemorrhage
|
|
|
What is the most common cause of intraparencymal cerebral hemorrhage?
a. DM b. HTN c. viral meningitis d. thrombosis |
HTN (due to accelerated atherosclerosis and hyaline arteriolar sclerosis of small vessels
|
|
|
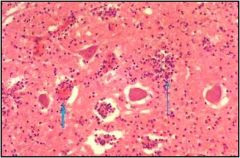
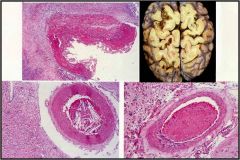
Pt presents with micoraneurysms or CHARCOT-BOUCHARD aneurysm what is a possible cause?
a. intracranial arterial aneurysm b. arteriovenous malformation c. intraparenchymal cerebral hemorrhage d. lacunar infarct |
intraparenchyma cerebral hemorrhage leads to these micoraneurysms which can potentially rupture, common site is the putamen often due to HTN
|
|

a. berry aneurysm
b. subarachnoid hemorrhage c. charcot-bouchard aneurysm d. cerebral amyloid |
charcot-bouchard aneurysm
|
|
|
What is the mechanism of action of HTN Cerebral vascular disease?
a. arteriolar sclerosis without fibrosis b. amyloid deposits in vessels resulting in weakening c. deposition of lipid and hyaline in the vessel walls leading to arteriolar sclerosis and microaneurysms d. abnormalities in large arteries |
a and b describe (cerebral amyloids)
while c describes HTN causes of intracranial hemorrahge so c deposits of lipid and hyaline in the wall of blodd vessels (lipohyalinosis) results in arteriolar sclerosis and microaneurysms |
|
|
HTN causes what abnormalities in small vessel walls:
a. atherosclerosis b. hyaline arteriosclerosis c. proliferative changes and necrosis d. minute aneurysms |
hyaline arteriosclerosis (small vessels)
atherosclerois (large vessels) proliferative changes and necrosis (arterioles) minute aneurysm (basal ganglia) |
|
|
Cerebral amyloid results from deposits of
a. PrP proteins b. plaques and tangles c. amyloidgenic peptide deposits d. lacunar infarct |
amyloidgenic peptide deposits
|
|
Common in the elderly due to amyloidgenic deposits in the vessels resulting in weakening
a. cerebral amyloid b. lacunar infarct c. HTN encephalopathy d. intraparenchymal cerebral hemorrhage |
cerebral amyloid
|
|
Can results from dominant polycystic kidney disease (HTN), Ehlers-Danlos syndrome type IV, neurfibromastosis type I, and Marfan syndrome. What are some risk factros
a. CHD b. etoh c. smoking d. obesity |
smoking (this is a saccular aneurysm can lead to SUBARACHNOID hemorrhage
|
|
This trauma begins in the temple, resulting in a lucid period with slow progression of neurological symptoms. The clinical presentation include vomit/nausea. What is vessel ruptured?
a. bridging veins b. MMA c. ICA d. leptomeningeal |
MMA since this is a epidural hematoma resulting in bleeding into epidural space
|
|
This usually presents 24-48hrs with clinical symptoms due to rupture of bridging veins, commonly found in what 2 population?
a. adolescents b. smokers c. elderly d. etoh users |
subdural hematoma common in elderly and etoh users
|
|
|
Clinical symptoms are often immediate and there is transient loss of consciousness; amnesia to event. With repeated episodes can lead to long term degenerative CNS effects.
a. concussion b. contusion c. subdural hematoma d. epideral hematoma |
concussion (trauma)
|
|
|
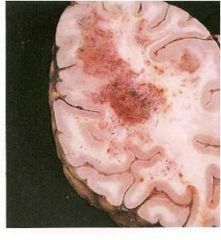
Usually in the frontal and temporal lobes resulting from localized possibly impact leading to edema.
a. concussion b. contusion c. epidural hematoma d. subdural hematoma |
contusion
|
|
common suptratentorial tumors more specifically in central lobe tumor:
a. astrocytoma b. ependymomas c. medulloblastoma d. meningioma |
astrocytoma
|
|
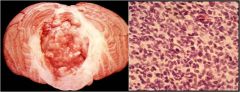
What is a distinguishing feature of glioblastoma from astrocytoma since they are both supratentorial tumors. Glioblastomas ..
a. occur later in life and are highly anaplastic, while they grow rapidly b. obstruct ventricular system c. grossly cystic d. often radiosensitive |
occur later in life and highly anaplastic; while they grow rapidly
obstruct vascular system (ependymoma) grossly cystic (piloctytic astrocytoma) often radiosensitive (medulloblastoma) |
|
This tumor is has a good long term prognosis with minimal recurrence after resection
a. occur later in life and are highly anaplastic, while they grow rapidly b. obstruct ventricular system c. grossly cystic d. often radiosensitive |
grossly cystic -- pilocytic astrocytoma
|
|

Presents with a 5-10yr survival with cerebrum calcifications
a. occur later in life and are highly anaplastic, while they grow rapidly b. obstruct ventricular system c. oligoendoroglioma d. often radiosensitive |
oligoendoroglioma
a. glioblastoma -- occurs later in life & highly anaplastic b. ependymoma-- obstruct VS d. medulloblastoma -- radiosensitive |
|
Often presents in children resulting in hyrdocephalus with increased ICP, but can also present in adults in the spinal cord. It is a slow growing tumor and very difficult to treat
a. occur later in life and are highly anaplastic, while they grow rapidly b. obstruct ventricular system c. grossly cystic d. often radiosensitive |
ependymoma -- obstruct the ventircular system leading to hydorcephalus in children
|
|
Common in children, fortunately very radiosensitive leading to elimination. It is a poorly differentiated tumor and does not interfere with ventricular system?
a. occur later in life and are highly anaplastic, while they grow rapidly b. obstruct ventricular system c. grossly cystic d. midline tumor |
medulloblastoma -- midline tumor (radiosensitive)
|
|
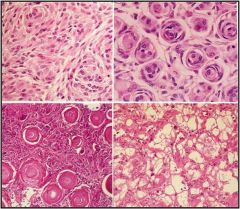
This tumor may be a result of radiation. It is a well defined, slow growing tumor in the arachnoid cells. Often identified by specific MICRO distinctions?
a. tangles and plaques b. reactive gliosis c. neutrophile infiltration d. psomomma bodies |
psomomma bodies (this is a meningioma)
|
|
Slow growing aracnoid cell tumor, often well defined. Can be easily diagnosed using an MRI scan.
a. ependymoma b. meningioma c. olioendoroglioma d. pilocytic astrocytoma |
meningioma
|
|
Pt presents with tumor that rarely involves tissue outside CNS and is most commonly found in what kind of pts?
a. elderly b. children c. ICP's (AIDS) d. young adults |
ICP's (AIDS) it is a very aggressive tumor and poorly responds to chemotherapy; often of B-cell origin
|
|
What is the primary source of a metastatic tumor into the CNS?
a. lungs b. breast c. skin d. kidney |
LUNGS
|
|
27y/o female presents with distinct episodes of neurological deficits separated in time and space, including bilateral internuclear opthalmoplegia (medial longitudinal fasiculus), sensory and motor dysfunction, and optic neuritis. What is a possible mechanism of action of this condition.
a. direct infection of oligodendrocytes b. allergic reaction following a viral infection or vaccination c. antibodies against myelin basic protein in oligodendrocytes destroy axon sheaths d. autoimmune inflammation with demyelination of peripheral motor fibers |
c. antibodies against myelin basic protein in oligodendrocytes destroy axon sheaths (multiple sclerosis)
a. direct infection of oligodendrocytes (viral infeciton) b. allergic reaction following a viral infection or vaccination (pervenous encephalomyelitis) d. autoimmune inflammation with demyelination of peripheral motor fibers (guillain-barre syndrome) |
|
What would you expect to see in the CSF of a 28y/o female presenting with distinct episodes of neurological defecit in time and space after reviewing MRI or CT with periventricular demyelination?
a. increase protein and glucose b. IgG oligoclonal bands c. IgE oligoclonal bands d. IgM oligoclonal bands |
IgG oligoclonal bands
|
|
This degenerative neurological disorder MICRO presentation is distinct from others due to what kind of inclusion, that result from aggregate resistance to normal cellular mechanism via the ubiquitin proteasome?
a. plaques and tangles b. Lewy bodies c. genetic expanded repeats d. white matter lesions |
Alzheimer's disease presents with plaques (AB protein) and tangles (tau protein)
b. Lewy bodies (parkinson's) c. genetic expanded repeats (huntingtons) d. white matter lesions (mutltiple sclerosis is a demyelinating disease) |
|
How can you distinguish a pt presenting with symptoms of alzheimer's from a pt presenting with symptoms of parkinson's. A pt with alzheimer's will present
a. expressionless face, stopped posture, slow voluntary movements, and with a pill rolling tremor b. hyperkinetic, chorea movements c. disorientation, memory loss and aphasia, progressive loss of cognitive function d. relapse and remission neurological deficits |
disorientation, memory loss, and aphasia leading to progressive loss of cognitive function
a. expressionless face, stopped posture, slow voluntary movements, and with a pill rolling tremor (parkinson's disease) b. hyperkinetic, chorea movements (huntington's disease) d. relapse and remission neurological deficits (multiple sclerosis) |
|
This is one of the few neurodegenrative diseases that is autosomal DOMINANT, unfortunately leading to DEMENTIA
a. expressionless face, stopped posture, slow voluntary movements, and with a pill rolling tremor b. hyperkinetic, chorea movements c. disorientation, memory loss and aphasia, progressive loss of cognitive function d. relapse and remission neurological deficits |
hyperkinetic, chorea movements (huntigton's disease)
a. expressionless face, stopped posture, slow voluntary movements, and with a pill rolling tremor (Parkinsons) c. disorientation, memory loss and aphasia, progressive loss of cognitive function (Alzheimer's disease) d. relapse and remission neurological deficits (multiple sclerosis is a demyelination disease) |
|
What is the mechanism of action of this disease leading to expressionless faces, stopped posture, slowness of voluntary movements, pill rolling tremor, and festinating gait.
a. aggregation of AB peptide due to resistance of ubipquitin proteosome b. disturbance in the DOPAMINERGIC pathway c. degeneration of strial neurons d. degeneration of myelin sheath |
disturbance of DOPAMINERGIC pathway and depigmentatin of substantia nigra (< Dopamine synthesis)
|
|
|
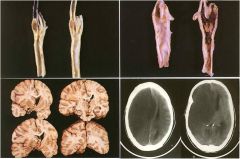
Only VERTEBRAL defect results in what neural tube defect?
a. spina bifida occulta b. meningocele c. meningomyeolcele d. myelocele |
spina bifida occulta
|
|
|
How can you differentiate the spina bifida occulta from meningiocele:
a. vertebral defect b. DURA and ARACHNOID herniation through vertebral defect c. DURA and ARACHNOID herniation through vertebral defect with spinal cord and nerve roots involved d. defective CLOSURE of spinal cord with no skin covering the surface |
DURA and ARACHNOID herniation through vertebral defect
|
|
|
Which neural tube defect is easily identified?
a. spina bifida occulta b. meningocele c. meningomyeolcele d. myelocele |
myelocele since there is NO skin covering the surface
|
|
|
How can you distinguish a meningiocele and meningomyeolcele neural tube defect?
a. vertebral defect b. DURA and ARACHNOID herniation through vertebral defect c. DURA and ARACHNOID herniation through vertebral defect with spinal cord and nerve roots involved d. defective CLOSURE of spinal cord with no skin covering the surface |
DURA and ARACHNOID herniation through vertebral defect with spinal cord and nerve roots involved
|
|
|
What is an important chemical marker to measure in pregnant women at about 16 weeks to determine if there are neural tube defects ?
a. low AFP b. high AFP c. low hCG d. high hCG |
high AFT (neural tube defect), while low AFT (Downs syndrome)
|
|
|
Why are epidural hemorrhage more common in spinal cord injuries when compared to subdural hemorrhages?
a. due to the richness of epidural space with vasculature and its looseness b. due to their close location to the surface c. due to frequent falls and contussions d. their occur equal amounts |
epidural space in rich in vasculature and pretty loose
|
|
|
Spinal cord compressions from tumors result in all EXCEPT:
a. motor and sensory deficit b. infarct due to blood vessel compression c. severe radiating pain in the leg d. irreversible neurological deficits |
no severe radiating pain in the leg this is a result of herniated disc
|
|
|
This spinal cord compression is a form of degenerative arthritis leading to osteophyte or spur formation of verterbrae
a. tumor b. cervical spongylosis c. herniated disc d. radiation myelopathy |
cervical spongylosis
|
|
|
This nerve root compression is related to the use of radiation, often 6mo - 2yrs later, dose related and leads to
a. degenerative arthritis b. degenerated intervertebral discs and ligaments weaken c. degeneration and necrosis of white or gray matter d. intermedullary gliomas |
radiation caused radiation myelopathy resulting in degeneration and necrosis of white or gray matter (spinal cord and nerve roots)
|
|
|
This disease often leads to twitiching, cramping, or muscle stiffness. Muscle weakness often affect the arm or a leg. There is progressive weakness and respiratory failure due to weakness of respiratory muscles and infections. There is severe degeneration of
a. myelin sheath b. sensory neurons c. motor neurons d. white matter in cortex |
meylin sheath would be multiple sclerosis, while degeneration of motor neurons results from amytrophic lateral sclerosis (LouGehrig's Disease) loss of MOTOR neurons and gliosis in spinal cord, BS, and cortex (often degeneration of CST)
|
|
|
50-year-old man presents with headaches, vomiting, and weakness of his left side. Physical exam reveals his right eye to be pointing ‘down and out’ along with ptosis of his right eyelid. His right pupil is fixed and dilated and does not respond to accommodation. Marked weakness is found in his left arm and leg. Swelling of the optic disk (papilledema) is found during examination of his retina. Which of the following is most likely present in this individual?
a. Aneurysm of the vertebrobasilar artery b. Arteriovenous malformation involving the anterior cerebral artery c. Subfalcine herniation d. Tonsillar herniation e. Uncal herniation |
uncal herniation
|
|
|
This lesion appeared on CT scan as a discreet mass beneath the dura and was seen to compress the underlying cerebral hemisphere. The patient is a 45 year old female who presented with headaches for the past month. The best diagnosis is:
a. Maningioma b. Astrocytoma, low grade c. Ependymoma d. Metastasis e. Tuberculoma |
meningioma
|
|

2.) This lesion appeared on CT scan as a discreet mass beneath the dura and was seen to compress the underlying cerebral hemisphere. The patient is a 45 year old female who presented with headaches for the past month. The best diagnosis is:
a. Meningioma b. Astrocytoma, low grade c. Ependymoma d. Metastasis e. Tuberculoma |
meningioma
|
|
|
3.) An 18 year old male high school baseball player gets hit in the head with a fastball in the temporal area. He does not lose consciousness, but afterward develops a slight headache. He is not taken to the ER. By evening her develops a severe headache with vomiting and confusion. At that time he is taken to the ER, where, after being examined by a neurosurgeon, he is taken to the operating room for immediate surgery for an epidural hematoma. Which of the following is most likely present in this individual?
a. Transaction of a branch of the middle meningeal artery b. Bleeding from torn bridging veins c. Ruture of a preexisting berry aneurysm d. Rupture of an arteriovenous malformation e. Cortical bleeding occurring opposite the point of traumatic injury |
transaciton of a branch of the MMA
|
|
|
4.) A 27 year old woman presents with the acute onset of severe headaches and vomiting. She describes these headaches as being the “worst headaches” she has ever had. There is no history of trauma. She is afebrile, and her blood pressure is within normal limits. Physical examination reveals stiffness in her neck, but papilledema is not present. A lumbar puncture reveals blood within the CSF, but the cell count and the glucose levels are within normal limits. The signs and symptoms in this individual are most likely the results of an abnormality located in which one of the following anatomic sites?
a. Anterior thalamic nucleus b. Circle of Willis c. Medial inferior pons d. Superior cerebellar artery e. Superior sagittal sinus |
Circle of willis "berry aneurysm"
|
|
|
5.) A lumbar puncture is performed on a patient with headaches, photophobia, clouding of consciousness, and neck stiffness. If these symptoms are the result of bacterial infection of the meningies, which of the following would examination of the C
SF most likely reveal? Pressure Appearance Protein Glucose Inflammation a. Increased Cloudy Increased Decreased Neutrophils b. Increased Clear Increased Normal Lymphocytes c. Increased Clear Increased Normal Mononuclear d. Decreased Clear Decreased Normal Lymphocytes e. Increased Clear Increased Normal Mixed |
P (increase)
A (cloudy) Pr(increase) G (decrease) infl(neutro) |
|
|
75 year old female has had progressively worsening mental function, as indicated by her son when he brings his mother to see you. The son states that his mother is now frequently getting lost in the neighborhood. He relates that she cannot easily feed or dress herself. She often does not seem to know who he his. After a year-long course in a nursing home, she dies from a respiratory infection. The brain at autopsy weighs 1025 gm and demonstrates frontal and parietal atrophy, with ex vacuo ventricular dilation. The light microscopic appearance of the frontal cortex is seen here with Bielschowsky silver stain. Which of the following statements best characterizes this process:
a. A bloodborne pathogen led to this illness b. An amyloid angiopathy can be present c. Inheritance of this disease occurs in an autosomal dominant fashion d. A response to dopaminergic pharmacologic agents is often observed e. Aluminum toxicity can explain these findings |
amyloid angiopathy can be present
|
|
|
7.) A 45-year old man presents with weakness and cramping that involves both of his hands. Physical exam reveals atrophy of the muscles of both hands, hyperactive reflexes and muscle fasiculations involving the arms and legs, and a positive Babinski reflex. Sensation appears normal in the arms and legs. Which of the following is the most likely diagnosis?
a. Metachromatic leukodystrophy b. Amyotrophic lateral sclerosis c. Guillian-Barre syndrome d. Huntington’s disease e. Wilson’s disease |
amyotrophic lateral sclerosis ALS
|
|
|
41 year old man presents with involuntary rapid jerky movements and progressive dementia. He soon dies and gross exam of his brain reveals marked degeneration of the caudate nucleus. Which of the following is the most likely cause of this individual’s symptoms?
a. Decreased functioning of GABA neurons b. Increased functioning of dopamine neurons c. Relative increased functioning of acetylcholine neurons d. Relative decreased functioning of acetylcholine neurons e. Decreased functioning of serotonin neurons |
Huntingtons disease -- decrease infunction of GABA neurons
|
|
|
44 year old woman presents with the new onset of seizures along with increasing frequency of severe headaches. Her medial history is otherwise unremarkable. Physical exam reveals bilateral neurologic defects. Workup reveals a large, ill-defined, necrotic mass that involves both the right and left cerebral cortex. Histologic sections from this lesion reveal a hypercellular tumor with pseudopalisading of tumor cells around large areas of serpentine necrosis. Marked vascular endoneural proliferation is present. Numerous atypical nuclei and mitoses are seen. This tumor is best classified as what type of high grade neoplasm?
a. Astrocytoma b. Lymphoma c. Medulloblastoma d. Oligodendroglioma e. Schwannoma |
Glioblastoma multiforme -- astrocytoma
|
|
|
10.) A 40-year-old man has had decreased mentation with confusion for the past 6 weeks. On physical examination he exhibits incoordination and reduced movement in his right arm. MR imaging of the brain shows 0.5 to 1.5 cm lesions in cerebral hemispheres in white matter and at the grey-white junction that suggest demyelination. A stereotatic biopsy is performed, and immunohistochemical staining of the tissue reveals JC papovavirus in oligodendrocytes. Which of the following abnormal laboratory test findings is this patient most likely to have?
a. Oligoclonal bands in CSF b. Hemoglobin AIC of 9.8% c. CD4 lymphocyte count of 90/microliter d. Serum sodium of 109 mmol/L e. HDL cholesterol of 12 mg/dL |
CD4 lymphoctye count of 90/mL
|
|
|
A 63 year old man has had progressively worsening dyspnea over the past 10 years. He has noticed a 10 lb. weight loss over the past 2 years. He had a chronic cough with minimal sputum production. On physical exam, he is afebrile and normotensive. A CXR shows extensive interstitial disease. Pulmonary function testing shows low FVD and a normal FEV1/FVC ratio. Increased exposure to which of the following is most likely to produce these findings?
a. Silica b. Tobacco smoke c. Ozone d. Wood dust e. Carbon monoxide |
silica
|
|
|
A 45 year old man had smoked two packs of cigarettes per day for 20 years. For the past 4 years, he has had a chronic cough with copious mucoid expectoration. During the past year, he has had several episodes of respiratory tract infections that were diagnosed as “viral flu,” and he developed difficulty breathing, tightness in the chest, and audible wheezing. His breathing difficulty was relieved by inhalation of a B-adrenergic agonist and disappeared after the chest infection had resolved. Which of the following pathologic conditions best described these clinical findings?
a. Chronic bronchitis with cor pulmonale b. Chronic bronchitis with asthmatic bronchitis c. Chronic bronchitis with emphysema d. Bronchiectasis e. Hypersensitivity |
chronic bronchitis w/emphysema
|
|
|
A 34 year old man suddenly develops severe dyspnea with wheezing and is taken to the ED. A CXR shows increased lucency in all lung fields. A sputum cytologic specimen shows Curschmann spirals, Charcot-Leyden crystals and acute inflammatory cells in a background of abundant mucus. Many of the inflammatory cells are eosinophils. Which of the following is the most likely diagnosis?
a. Bronchiectasis b. Aspiration c. Bronchial asthma d. Centrilobular emphysema e. Chronic bronchitis f. Obstructive sleep apnea |
bronchial asthma
|
|
|
A 50 year old man comes to the physician with gradually increasing dyspnea and a 8 lb weight loss over the past 2 years. He admits to smoking two packs of cigarettes per day for 20 years, but states that he has not smoked for the past year. PE shows an increase in the AP diameter of the chest (“barrel chest”). Auscultation of the chest shows decreased lung sounds. A chest radiograph shows bilateral hyperlucency, especially in the upper lobes. Pulmonary function tests show that the FEV1 is markedly decreased, but the FVC is normal. The FEV1/FVC is decreased. Which of the following is most likely to contribute to the pathogenesis of his disease?
a. Impaired hepatic release of a1-antitrypsin b. Release of elastase from neutrophils c. Abnormal epithelial cell chloride ion transport d. Decreased ciliary motility with irregular dynein arms e. Macrophage recruitment and release of interferon gamma |
release of elastase form neurtophils
|
|
|
A 50 year old man had developed truncal obesity, back pain, and easily bruisable skin over the past 5 months. He is afebrile and his BP is 160/95 mmHg. A CXR shows an ill-defined 4 cm mass involving the left hilum of the lung. Cytologic exam of bronchial washings shows round cells that have the appearance of lymphocytes but are somewhat larger. The patient is told that, although his disease is apparently localized to the lung, surgical treatment in unlikely to be curative. He is advised to stop smoking. Which of the following neoplasms is most likely to be present in this patient?
a. Adenocarcinoma b. Bronchial carcinoid c. Bronchoalveolar carcinoma d. Large cell carcinoma e. Metastatic renal cell carcinoma f. Non-Hodgkins lymphoma g. Small cell carcinoma h. Squamous cell carcinoma |
small cell CA
|
|
|
A 70 year old woman is referred to an ophthalmologist because of difficulty with her right eye. She also has pain in the right upper chest. The findings of physical exam include enophthalmos, meiosis, ptosis, and anhidrosis. A CXR shows right upper lobe opacification and bong destruction of the right first rib. Which of the following conditions is most likely to be present?
a. Bronchopneumonia b. Bronchiectasis c. Brochogenic carcinoma d. Sarcoidosis e. Tuberculosis |
bronchogenic CA
|
|
|
A 56 year old man with ischemic heart disease undergoes a CABG procedure under general anesthesia. Two days postoperatively, he experiences increasing respiratory difficulty with decreasing arterial oxygen saturation. He is afebrile, HR is 78/min, R are 20/min, BP is 135/85 mmHg. Hemoglobin is unchanged at 13.7 g/dL. After he coughs up a large amount of mucoid sputum, his condition improves. Which of the following is the most likely explanation of these findings?
a. Resorption atelectasis b. Compression atelectasis c. Microatelectasis d. Contraction atelectasis e. Relaxation atelectasis |
resorption atelectasis
|
|
|
A 20 year od man has had mild fever with nonproductive cough, headache and myalgia for the past week. He goes to the physician who records a temperature of 37.9 degrees C and notes erythema of the pharynx. Diffuse crackles are heard on ausculation. A CXR shows bilateral extensive patchy infiltrates. A sputum gram stain shows normal flora. The cold agglutinin titer is elevated. He received a course of erythromycin therapy and his condition improves. Infection with which of the following organisms is most likely to produce these findings?
a. Legionella b. Mycobacterium fortuitum c. Mycoplasma pneumoniae d. Nocardia asteroids e. Respiratory syncytial virus |
mycoplasma pneumoniae
|
|
|
A 35 year old man who is HIV positive complains of a bad taste in his mouth and discoloration of his tongue for the past 6 weeks. On physical exam, there are areas of adherent, yellow-tan plaque on the lateral aspects of the tongue. This plaque is scraped off to reveal an underlying granular, erythematous base. Which of the following is the most likely diagnosis?
a. Aphthous ulcer b. Cheilosis c. Hairy leukoplakia d. Herpetic stomatitis e. Leukoplakia f. Glossitis g. Oral thrush |
oral thrush
|
|
|
A 68 year old man goes to the physician for a routine health maintenance exam. He has some disecrete white patches with a leathery surface covering the right buccal mucosa of the oral cavity. A biopsy from one of the lesions shows squamous epithelia acanthosis with marked hyperkeratosis. Which of the following risk factors is most likely to cause these lesions?
a. Eating chili peppers b. Chewing spearmint gum c. French kissing d. Chewing tobacco e. HIV infection |
chewing tobacco
|
|
|
11. The family of a 63 year old woman noticed that she has become more forgetful over the past 6 weeks. One month later the woman has difficulty ambulating and is unable to care for herself. She has myoclonus and is afebrile. CT scan shows minimal cerebral atrophy. EEG shows low-amplitude, slow background activity with periodic complexes and occasional repetitive, sharp waves with intervals of 0.5 to 1 sec. Which of the following histologic abnormalities is most likely to be found in the cerebral cortex?
a. Numerous pleuritic plaques b. Plaques of demyelination c. Lewy bodies d. Microglial nodules e. Spongiform encephalopathy |
spongiform encephalopathy Crueutz-Jakob
|
|
|
`12. A 40 year old previously healthy man is brought to the emergency department after sudden onset of a grand mal seizure. Physical exam yields no remarkable findings except for a 1 cm darkly pigmented lesion on the skin of the upper back. CT scan of the head shows five sharply circumscribed mass lesions located in the cerebral hemispheres at the gray-white junction of the parietal and frontal lobes. Which of the following is the most likely diagnosis?
a. AIDS b. Metastases c. Infective endocarditis d. Neurofibromatosis type I e. Cysticercosis |
metastases
|
|
|
13. 36 hours after falling down a flight of stairs, a 72 year old woman develops a headache and confusion and is taken to the emergency department. On physical exam, she is conscious and has a scalp contusion on the occiput. Which of the following is the most likely location of an intracranial hemorrhage in this patient?
a. Pontine b. Subarachnoid c. Basal ganglia d. Epidural e. Subdural |
sudural
|
|
|
A 38 year old woman who fell to the ground and hit her head is taken to the emergency department. There are no remarkable findings on physical exam. CT scan of the head shows no hemorrhage or fracture, but there is a 5 cm mass beneath the dura that compresses the underlying left superolateral parietal lobe. The mass is surgically removed. Histologic analysis shows elongated cells with pale, oblong nuclei and pink cytoplasm with occasional psammoma bodies. Which of the following is the most likely diagnosis?
a. Meningioma b. Tuberculoma c. Medulloblastoma d. Schwannoma e. Ependymoma |
meningioma
|
|
|
15. A 53 year old man dies of aspiration pneumonia after a 6 year illness, characterized by progressive, symmetric muscular weakness. At autopsy, the brain and spinal cord appear normal on gross exam. Microscopic sections show gliosis in the motor cortex, pallor of the lateral corticospinal tracts and neuronal loss in the anterior horns of the spinal cord. Which of the following is the most likely underlying cause of death?
a. Becker muscular dystrophy b. Neurofibromatosis type II c. Guillain-Barre syndrome d. Creutzfeldt-Jakob disease e. Amyotrophic lateral sclerosis |
amyotrophic lateral sclerosis
|
|
|
A 19 year old snowboarder wearing protective equipment consisting of a baseball cap, baggy shorts and a letterman’s jacket flew off a jump and hit a tree. He was initially unconscious and then “came to” and wanted to try another run, but his friends thought it best to call for help. On the way to the emergency department, he became comatose. Physical exam shows left papilledema. Skull radiographs show a linear fracture of the left temporal-parietal region. A serum drug screen is positive for cannabinoids. The clinical picture is most consistent with which of the following lesions?
a. Contusion of frontal lobes b. Epidural hematoma c. Ruptured berry aneurysm d. Acute leptomeningitis e. Acute subdural hematoma |
epidural hematoma
|
|
|
A 30 year old woman has noted minimal fetal movement. An ultrasound show a defect in skull development. Which of the following laboratory findings is most likely to be present?
a. Fetal hyperbilirubinemia with anemia b. High maternal cytomegalovirus IgM titer c. Elevated maternal serum AFP level d. Elevated maternal hemoglobin A1C e. 47, XX, +21 fetal karyotype |
elevated maternal AFP level
|
|
|
While working at her desk as an accountant, a 50 year old woman develops sudden, severe headache and is taken to the emergency department. On examination, she has nuchal rigidity. A lumbar puncture is performed. The CSF shows numerous RBCs, no neutrophils, a few mononuclear cells and a normal glucose level. The gram stain result is negative. Which of the following events has most likely occurred?
a. Middle cerebral artery thromboembolism b. Tear of subdural bridging veins c. Ruptured intracranial berry aneurysm d. Bleeding from cerebral amyloid angiopathy e. Hypertensive basal ganglia hemorrhage |
rupture intracranial berry aneurysm
|
|
|
A 55 year old man had increasing difficulty with initiation of voluntary movements and increasing inability to perform activities of daily living for 1 year. He became bedridden and died of pulmonary thromboembolism. The gross appearance of the midbrain shows lack of pigmentation. Which of the following additional clinical features is most closely associated with this lesion?
a. Pill-rolling tremor at rest b. Symmetric weakness in the extremities c. Choreiform movements d. Difficulty with short-term memory e. Paraplegia |
pill rolling tremor at rest
|
|
|
A 20 year old man with HIV infection has had a decreased level of consciousness for the past week. He now experiences a seizure. On physical exam, his temperature is 37.6 degrees C. MRI of the brain shows several 1 to 3 cm ring-enhancing lesions in the cerebral gray matter bilaterally. Stereotaxic biopsy is performed. Which of the following pathologic findings is most likely to be present on the microscopic examination of the biopsy specimen?
a. Large atypical lymphocytes b. Budding cells with pseudohyphae c. Spongiform encephalopathy d. Toxoplasma pseudocytes e. Metastatic squamous cell carcinoma |
toxoplasma pseudocytes
|
|
|
21. Three months ago, a 27 year old woman had an episode of weakness, which she attributed to job stress and fatigue. She now sees her physician because she has had decreased vision in her left eye for the past week. The neurologic exam shows mild residual weakness with 4/5 motor strength in the right lower extremity. A lumbar puncture is performed. Lab exam of the CSF shows increased IgG levels with prominent oligoclonal bands. MRI of the brain shows small scattered areas consistent with demyelination, most of which are located in the periventricular white matter. Which of the following is the most appropriate information to give the patient about these findings?
a. No further neurologic problems will be experienced b. Relapses and remissions will occur over many years c. This disease can be passed on to your children d. Further debilitation and death will occur within 5 years e. A test for HIV will be positive |
relapses and remission will occur over many years
|

