![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
30 Cards in this Set
- Front
- Back
|
-Acute endometritis: most commonly associated with
|
with prior delivery or miscarriage
|
|
|
Non-specific chronic or acute endometritis may be associated with
|
Chlamydia
|
|
|
bleeding at inappropriate time in menstrual cycle
|
Metrorrhagia
|
|
|
dysfunctional uterine bleeding
|
abnormal bleeding without definable organic cause; usually due to anovulatory cycles, which lead to estrogen stimulation unopposed by progesterone-continued proliferative activity of the glands which may become irregular (“disordered proliferative endometrium”)
|
|
|
Causes of AUB may vary with age
Prepuberty: Adolescence: Reproductive age: Perimenopausal: Postmenopausal |
Prepuberty: Precocious puberty of hypothalamic, pituitary, or ovarian origin
Adolescence: Anovulatory cycle, coagulation disorders Reproductive age:Complications of pregnancy (always think of this first!), organic lesion,DUB Perimenopausal:DUB, organic lesion Postmenopausal:Atrophy, organic lesion |
|
|
Endometrial polyps are
|
Fibromuscular stroma,thick-walled blood vessels, glands which may be irregular in distribution and/or configuration
|
|
|
Endometrial polyps are unresposive to
|
estrogen but not progesterone; may be seen in tamoxifen-treated patients (weak estrogenic effect on endometrium)
Chromosome 6p21 rearrangements may be seen, in common with benign mesenchymal tumors --Not premalignant, but adenocarcinoma may arise within them |
|
|
Endometrial tissue present in the myometrium of the uterine wall; downgrowth of the endometrium
--“Globular” uterus |
Adenomyosis
|
|
|
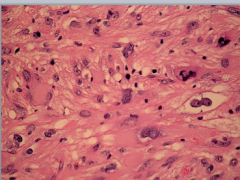
Chronic endometritis are characterized by
|
lymphocytes and plasma cells, the plasma cells are neccesary for the diagnosis of chronic endometritis given that lymphocytes are normally found in the endometrium
|
|
|
What causes chronic endometritis?
|
retained products of concepcion, chronic pelvic inflammatory disease, IUD, TB. Presents as abnormal bleeding and infertility
|
|
|
Whats the anovulatory cycle?
|
Lack of ovulation that results in an estrogen driven proliferative phase without a subsequent progesterone driven secretory phase
|
|
|
What is endometriosis and how does it present?
|
Endometrial glands and stroma outside of the uterine endometrial lining most likely due to retrograde menstruation with menstruation at an ectopic site
Presents with pain during menstruation and pelvic pain; may cause infertility |
|
|
Endometriosis most typically affects the ovary, however when the myometrium is involved it is called
|
adenomyosis
|
|
|
Endometriosis increases the risk of carcinoma especially when it affects the
|
the ovary
|
|
|
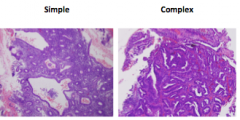
Endometrial hyperplasia occurs as consequence of
|
unopposed estrogen due to obesity. polycistic ovary syndrome and estrogen replacement. And it is classified histologically based on architectural growth pattern (simplex or complex) and presence or absence of cellular atypia
|
|
|
Endometrial hyperplasia presents as
|
postmenopausal uterine bleeding
|
|
|
The major complication in endometrial hyperplasia leading to carcinoma progression is
|
presence of simple hyperplasia with atypia
|
|
|
What is the most common invasive carcinoma of the female genital tract
|
Endometrial carcinoma
|
|
|
Endometrial carcinoma presents in 2 types, hyperplasia or type 1 and sporadic or type 2. At what ages do each present?
|
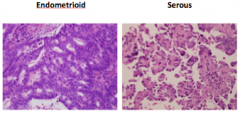
type 1: avg age is 60
Type 2: avg age is 70 |
|
|
The risk factors involved in type 1 endometrial hyperplasia are
|
with obesity, hypertension, diabetes, unopposed estrogen. Usually it is low grade and indolent
|
|
|
What are the characteristic of type 2 endometrial carcinoma?
|
It is serous and is characterized by papillary structures with psammoma body formation and p53 mutation is common. This are aggresive tumors
|
|
|
what is a malignant mixed mullerian tumor?
|
poorly-differentiated carcinoma with sarcomatous differentiation which may be homologous (like tissue normally found in the uterus) or heterologous (like tissue not found in the uterus-skeletal muscle, cartilage, bone)
|
|
|
where does MMMT arise?
|
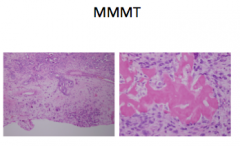
in the setting of endometrial atrophy with Endometrial Intraepithelial Carcinoma-malignant-appearing cells in pre-existing epithelium
-p53 mutation is early event in carcinogenesis -Usually high stage at presentation, aggressive |
|
|
most common tumor in women
|
Leiomyoma (benign)=”fibroids arising from myometrium usually asymptomatic that presents in premenopausal women and during pregnancy gets enlarged and shrinks after menopause
|
|
|
What would gross exam on a women with Leiomyoma show?
|
well defined, white whorled mass that may distort the uterus and impinge on pelvic structures
|
|
|
what is a Leiomyosarcoma
|
it's a malignant smooth muscle arising from the myometrium and arises de novo and do not arise from leiomyomas.
|
|
|
Who gets Leiomyosarcoma and what would gross exam reveal?
|
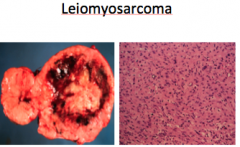
Post menopausal women. Single lesion with areas of necrosis and hemorrhage.
|
|
|
Tumors of spindle-shaped smooth muscle cells with some features of malignancy but which do not meet diagnostic criteria for malignancy
|
Smooth muscle tumors of uncertain malignant potential (STUMP)
|
|
|
-well-circumscribed nodule of endometrial stromal cells; benign
|
Endometrial stromal nodule
|
|
|
infiltrating neoplasm of endometrial stromal cells; low grade malignancy
|
-Endometrial stromal sarcoma
|

