![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
- 3rd side (hint)
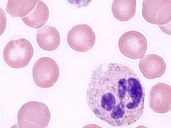
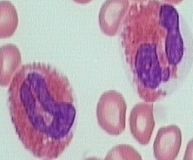
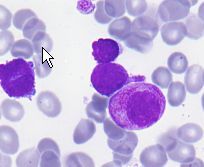
What are the blue cytoplasmic inclusions and what does it indicate?
|
Dohle Bodies (rER remnants) due to left shifts
|
|
|
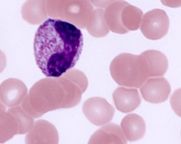
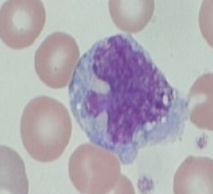
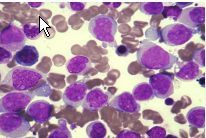
What is occurring with this cell? why?
|
Toxic Granulation- due to impaired cytoplasmic maturation due to Left shift
|
|
|
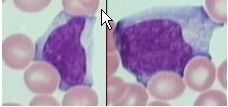
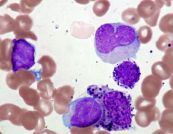
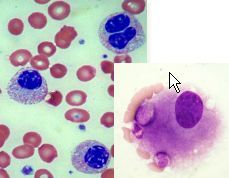
What infection is characterized by these large atypical B cells infected with Epstein-Barr virus?
|
Infectious Mononucleosis
What helps clear the infected cells? |
cytotoxic/suppressor CD* (+) T cells
|
|
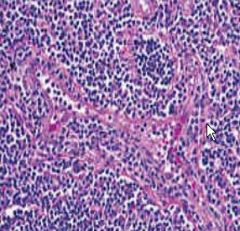
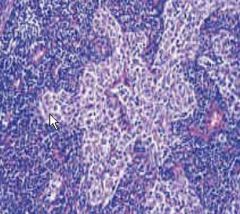
Classify this reactive lyphoid hyperplasia
|
Paracortical hyperplasia
main cell type? |
T cells
|
|
|
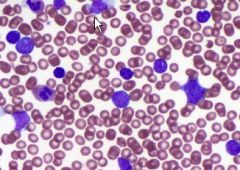
Most common cause of basophilia?
|
CML
|
|
|
|
define Leukoerythroblastosis
|
Leukomoid reaction with addition of nucleated red blood cells.
cause? |
myelofibrosis of BM due to metastatic cancer or hemoatologic malignancy leading to extramedullary hematopoesis
|
|
|
define chronic granulomatous disease
|
lethal sex-linked disorder where neutrophils can phagocytose but not kill due to impaired respiratory burst oxidase system -> chronic infections
|
|
|
|
reactive follicular hyperplasia may closely resemble what cancer??
|
metastatic cancer or follicular lumphoma
main cell type |
B cell
|
|
Define this reactive lymphoid hyperplasia
predominant cell type? |
sinus hyperplasia
T cells |
|
|
define the cell type- increased numbers of these cells are due to?
|
eosinophils- allergic rxns, parasites, CML, tumors, Hodgkin's lymphoma
|
|
|
define the cell type- increased numbers of these cells are due to?
|
basophil- allergic reaction, CML, and other MPDs, hypothyroidism, splenectomy
|
|
|
|
congenital neutropenia results in?
|
cyclic neutropenia- abnormality of feedback mechanisms
|
|
|
|
DD of neutrophilia in leukocytosis?
|
bacterial infection, inflammation, emotions, drugs, neoplasm, hematologic abn
|
|
|
|
Major difference between acute and chronic leukemia
|
Acute Leukemia- uncontrolled blast proliferation
Chronic leukemia- uncontrolled proliferation of mature cells |
|
|
|
acute lymphoblastic vs myeloid leukemia- age? categorized by?
|
ALL- children, B/Tcell (phenotype)
AML- adults, chromosomal translocations |
|
|
|
Stages of lymphomas
|
I- one lymph node
II- 2+ lymph nodes, same side diaphragm III- opp sides of diaphragm IV- extranodal site |
|
|
|
T cell markers
|
CD 1,2,3,4,7,8
|
|
|
|
B cell markers
|
CD10 and up
|
|
|
|
what type of non-Hodgkin lymphoma has the highest incidence?
|
B-cell
|
|
|
|
what is needed for the diagnosis of acute leukemia?
|
blasts in periph blood, 20%blasts in BM
|
|
|
|
three types of acute leukemias
|
myeloid (AML), B lymphoblastic & T-lymphoblastic (ALL)
|
|
|
|
what is the most common childhood cancer? peak ages?
|
ALL-
Bcell type (85%) ~3yrs Tcell type (15%) adolescence, male |
|
|
|
How do you differentiate between T and B-ALL?
|
immunophenotype (not morphology!)
|
|
|
|
phenotypic detection of B-ALL and early/late differentiation
|
CD19 (pan B-cells)
early= no CD10 late= CD10, CD20 & cytoplamic IgM heavy chain |
|
|
|
Good prognosis factors for B-lymphoblastic leukemias
bad prognosis factors |
2-10 yrs
low White Cell Count hyperdipoidy (>50 chrom) t(12;21) TEL-AML1 genes |
<2/adolescence/adult
high WCC t(9;22) BCL-ABL (phili chrom) 11q23 translocations (MLL)- associated w/ age<2 hypodipoid (<44 genes) |
|
|
Most common lymphoblastic lymphoma?
|
T-LBL (85-90%)
most common in what patient pop? |
adolescent males
|
|
|
phenotypic markers for T-lymphoblastic leukemias
|
CD1,2,5,7
early vs late markers |
late- (+) for CD 3,4,8
|
|
|
(T/F) cytogenetic abnormalities do not play a prominent role in the prognosis of B-ALL
|
False- they do not play a prominent role in the prognosis of T-ALL
what does? |
age, stage, LDH levels
|
|
|
common cytogenetic abnormalities in T-lymphoblastic leukemias
|
mutation of NOTCH 1 gene (normal T-cell development)
T cell receptor gene translocations |
|
|
|
main cell type in Burkitt's leukemia/lymphoma, markers? appearance?
chromosomal abnormalities? treatment? |
mature B-cells with Blastic morphology, CD20 & CD10/BCL6 germinal center markers, vacuolated cytoplasm
t(8;14) treated as an acute leukemia |
|
|
|
clinical presentation of AML
|
fatigue, bleeding, infections, no lymph node enlargement, granulocytic sarcomas, skin and gingival involvement, DIC
|
|
|
|
AML with Good prognosis, presents young, "AML with maturation"
|
t(8;21)
|
|
|
AML with Good Prognosis
|
inv(16)
|
|
|
AML with the best Prognosis, inc risk of DIC, and is treated with ATRA
|
t(15;17) characterized by promyelocytes
ATRA= all-trans retinoic acid |
|
|
AML characterized by intermediate prognosis with t(9;11) as the best one to have
|
11q23 abnormalities
|
|
|
AML characterized by poor prognosis
|
MDS- related changes with dysplasia (hypolobulation/granulation)
|
|
|
|
AML can result from cancer therapy such as
|
alkylating agents (cyclophosphamid), ionizing radiation, and topoisomerase II inhibitors (doxorubicin)
|
|
|
|
Compare AML and ALL:
age- blasts w/ granules- MPO, non-sp esterase- tdt- Lymph node and organ involvement- cytogenetic importance- |
AML:
age- adults blasts w/ granules- yes MPO, non-sp esterase- (+) tdt- (-) Lymph node and organ involvement- no cytogenetic importance- yes |
ALL:
age- kids blasts w/ granules- no MPO, non-sp esterase- (-) tdt- (+) Lymph node and organ involvement- yes cytogenetic importance- in B-ALL |
|
|
cytogenetic abnormality associated with Burkitt's leukemia/lymphoma?
|
t(8;14)
|
|
|
|
Precautions needed when treating Burkitts lymphoma
|
-treat spinal fluid due to high CNS relapse
-b/g w/ chemo reduction b/c of high lysis risk -b/g on low chemo doses to avoid tumor breakdown products overwhelming kidney -> renal failure -high cure rate -use CD20 therapy targets |
|
|
8 yr old boy presents with frequent respiratory infections, enlarged lymph nodes, hepatosplenomegaly, and CD (+) 2,3,5, & 7
|
T-ALL
|
|
|
|
11q23 rearrangement and prognosis of ALL and AML
|
poor prognostic of ALL
intermediate prognostic in AML |
|
|
|
which AML chromosomal abnormalities are associated with a lower relapse rate?
|
inv (16) and t(8;21)
|
|
|
|
Myelodysplastic syndrome (MDS) has a high risk of transformation to what?
|
AML
|
|
|
|
Difference between primary and secondary MDS
|
Primary= de novo
secondary= to prior genotoxic exposure (chemotherapy)- most likely to progress to AML |
|
|
|
MDS- chromosomal abnormalities: Good/bad/worse prognosis
|
Good- 5q-
Bad- monosomy 5 or 7, 7q or 20q deletions, trisomy 8 worse- complicated karyotype |
|
|
|
4 Examples of Dysplastic Morphologic Changes in MDS
|
1) erythoid- ringed sideroblasts, megaloblastoid
2)bilobed neutrophils 3)megakaryocytes- hypo/ersegmented/ & giant platlets 4)myeloid blasts w/ auer rods |
|
|
|
Morphologic change of MDS that holds the highest risk of transformation to AML
|
Auer rods
|
|
|
|
define preleukemia
|
refractory anemia with excess blasts (>5% but <20%)
|
|
|
|
main molecular cause of MPN's?
|
mutated tyrosine kinase genes (JAK2 or BCL/ABL)
|
|
|
|
Cells predominantly elevated in CML
|
neutrophilic granulocytes
|
|
|
|
Cells predominantly elevated in PMF
|
megakaryocytes wich induce fibroblasts to make collagen
(primary myelofibrosis) |
|
|
|
Cells predominantly elevated in PV
|
RBC precursors
(Polycythemia rubra vera) |
|
|
|
Cells predominantly elevated in ET
|
megakaryocytes and platlets
(essential thrombocythemia) |
|
|
|
What is Gleevec?
|
protein-tyrosine kinase inhibitor (competitive inhibitor of bcr-abl TK)
|
|
|
|
mutation associated with polycythemia vera?
|
JAK2
|
|
|
|
treatment for PV (polycythemia vera)
|
phlebotomy (remove excess RBC's), mild chronic chemotherapy (hydroxyurea therapy), and mild radionucleotide therapy (radioactive Fe damages RBC precursors in BM)
|
|
|
|
PMF (primary myelofibrotic) patients are at risk for what?
|
infection, hemorrhage, thrombosis, and progression to AML
|
|
|
|
neoplastic megakaryocytes in PMF secrete what factors?
|
platelet derived growth factors and TGF-beta (both stimulate fibroblasts)
|
|
|
|
CLL/SLL
age- symptoms- lymph node- smear abnormalities- lymph node- |
age= over 60
symptoms= fatigue, wt loss, anorexia, lymphadenopathy & hepatosplenomegaly, hypogammaglobinemia, inc infection, autimmune hemolytic anemia/ thrombocytopenia |
lymph node- diffuse infiltration with proliferation centers with larger activated lymphocytes
-smear= smudge cells! |
|
|
CLL
phenotype |
B cell markers (CD19, 20, 79a)
CD5 & CD23 coexpression dim surface Ig ZAP-70 associated with worse prognosis |
|
|
|
CLL cell of origin
|
pre-germinal naive B cell - worst prognosis
post-germinal B-cell (memory cell) - better prognosis |
|
|
|
CLL- Good/Bad genetic prognostic factors
|
Good- 13q14.3
Bad- 11q22-23, 17p |
|
|
|
What two neoplams can progress to diffuse large B-cell lymphoma?
|
CLL and follicular lymphoma
|
|
|
|
Follicular lymphoma
age/gender- symptoms- lymph node- |
middle age- no sex predilection
painless lymphadenopathy expanded germinal centers, no mantle zone, deminished interfollicular zones |
|
|
|
Follicular lymphoma
types of cells, translocation, and phenotype |
centrocytes and centroblasts (small cleaved cells and large non-cleaved cells with nucleoli)
t(14;18) 14=IgH, 18=Bcl-2 |
phenotype-
B cell markers- CD19, 20, 79a GC markers- CD10, Bcl-6 antiapoptotic- Bcl-2 |
|
|
Diffuse B-cell lymphoma
age- associated with? cells of origin? |
60 years
Infection with HIV (EBV), or follicular lymphoma/ CLL origin- GC's, post-GC cells |
|
|
|
Diffuse B-cell lymphoma
phenotype cytogenetics cells of origin clinical features |
B-cell markers (CD19,20 79a)
variable GC markers CD10 & Bcl-6 t(14;18), or dysregulation of Bcl-6 or p53 |
rapidly growing, nodal or extra-nodal, BM involvement is rare
GC or Post GC cells |
|
|
difference in chemotherapy between follicular lymphoma and diffuse lg B-cell lymphoma
|
folliuclar= low dose, diffuse requries high dose
|
|
|
|
Burkitt Lymphoma-
unique morphology? cell markers genetics age sites of mass? |
starry sky- vacuolated cytoplasm
B-cell markers (19,20,79a), GC marks (CD10, Bcl-6) t(8;14) increases c-myc |
kids/young adults
mandibular mass or abdominal mass |
|
|
aggressive but curable NHLs?
indolent but incurable? |
Burkitt, DLBL
|
CLL, follicular
|
|
|
What is the cause of lytic bone destruction in MM
|
cytokine IL-6 released by tumor and BM stroma that stimulate osteoclasts
|
|
|
|
symptoms of mm
|
CRAB
hypercalcemia, renal impairment, anemia, bone disease |
|
|
|
difference between MGUS and multiple myeloma?
|
MGUS had ,10% plasma cells in BM, serum M protein , 3g/dl, asymptomatic, no therapy required
|
|
|
|
waldenstrom macroglobulinemia is a complication of what neoplasm? due to? leads to?
|
multiple myeloma- due to IgM, leads to hyerviscosity, visual disturbances, confusion, CHF
|
|
|
|
Reed sternberg cells
|
binucleated cells classic of hodgkin lymphoma, secrete IL-5, which attracts inflammatory cells (eosinophils)
|
|
|
|
Hodgkin Lymphoma
age- differences from non-hodgkin- |
young adults and over 50
single group of nodes, contiguous spread, no mesenteric nodal involvement, extranodal presentation rare |
|
|
|
difference between classical HL and nodular lymphocyte predominant HL
|
classical: CD15+, CD30+, CD20-
nodular:CD15-, CD30-, CD20+ popcorn cells! |
|
|
|
Four types of Classical hodgkin lymphoma
|
nodular sclerosis- fibrous bands!
mixed celluarity lymphocyte rish lyphocyte depleted |
|

