![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
What is a duodenal atresia?
|
Congenital failure of duodenum to canalize; associated with Down syndrome.
|
|
|
How does duodenal atresia present?
|
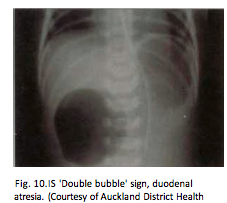
Polyhydramnios, distension of the stomach and blind loop of duodenum (double bubble sign)
Bilious vomiting |
|
|
- obstruction due to rotation or twisting of a loop of bowel around its mesenteric base of attachment. Most often occurs in the sigmoid colon, followed by the cecum.
|
Volvulus
|
|
|
caused by an infolding or telescoping of one segment of bowel (proximal) into the adjacent distal segment. Infants and children: spontaneous and reversible; in adults: tumor is usually involved.
|
Intussusception
|
|
|
string-like or band-like portions of scar tissue that form during healing after surgery or peritonitis. May result in obstruction due to kinking or compression of a portion of bowel.
|
Adhesions
|
|
|
What is a meckel diverticulum?
|
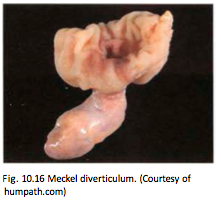
Outpouching of all 3 layers of the bowel wall and arises due to failure of the vitelline duct
|
|
|
Meckel diverticulum follows the rule of 2s
|
-Seen in 2% of the population
-2 inches long and located in the small bowel within 2 feet of ileocecal valve -Can present during the first 2 years of life with bleeding, volvus, intussusception or obstruction, however most are asymptomatic |
|
|
A pt shows with failure to pass meconium. Empty rectal vault on digital exam. Massive dilatation (megacolon) of bowel proximal to obstruction with risk for rupture
|
Hirschhsprung disease. Associated with down syndrome.
|
|
|
Hirschhsprung disease IS due to
|
congenital failure of ganglion cells to descend into myenteric (regulates motility) and submucosal (regulates blood flow)
|
|
|
Hernias are
|
a serosal lined out pouching of the peritoneum. Complications: incarceration - consists of a loop of small intestine becomes trapped within an inguinal hernia sac or an umbilical hernia sac; strangulation – the bowel may become compressed at the mouth of the hernia or twisted on itself, compromising blood supply and leading to infarction.
|
|
|
Ocurring in older individuals with coexisting cardiac or vascular disease, present with ab pain, bloody diarrhea or gross melena, ab rigidity, nausea and vomiting
|
Ischemic bowel disease.
|
|
|
Ischemic bowel disease has 2 phases
|
1)– Hypoxic injury occurs at the onset of vascular compromise. the epithelial cells lining the intestine are relatively resistant to transient hypoxia
2)reperfusion injury, is initiated by restoration of the blood supply and it is at this time that the greatest damage occurs. |
|
|
Ischemic bowel disease risk factors
|
Atherosclerosis, aortic aneurism, hypercoagulable states, embolization and vasculitis.
|
|
|
characterized by malformed submucosal and mucosal blood vessels, seen most often in the cecum or right colon, after the 6th decade of life, occurring in 1% of the adult population and accounting for 20% of major episodes of lower intestinal bleeding;
|
Angiodysplasia
|
|
|
Malabsorption can be defined as
|
defective absorption of fats, fat and water soluble vitamins, proteins , carbohydrates, electrolytes, minerals and water.
|
|
|
Malabsorption manifests as
|
diarrhea, flatus, ab pain, muscle wasting
|
|
|
The most common causes of malabsorption in the US are
|
celiac disease, pancreatic insufficiency and crohn disease.
|
|
|
Celiac disease malabsorption is due to
|
Defects in terminal digestion
Defects in transepithelial transport |
|
|
Cystic fibrosis malabsorption is due to defects in
|
Intraluminal digestion
|
|
|
Pts can be children all the way to middle aged adults, the y present with diarrhea, flatulence, weight loss and anemia
|
Celiac disease. IgA antibodies found to transglutaminase or IgA to deaminated gliadin.
|
|
|
Cystic Fibrosis malabsorption
|
Pancreatic insufficiency -> malabsorption
Treatment: replenish pancreatic enzymes |
|
|
Severe watery diarrhea
Dehydration, electrolyte imbalances |
Cholera. Shellfish. Toxin A subunit activates G protein leading to cAMP increase which opens CFTR channels and chloride moves into lumen
Fecal-oral, water |
|
|
V. Cholera affects what part of gi?
|
Small intestine
|
|
|
Watery or bloody diarrhea in travelers
|
Campylobacter. Infections can lead to Arthritis, Guillain-Barré syndrome. Found in Chickens, sheep, pigs, cattle
Poultry, milk, other foods |
|
|
Campylobacter affects
|
Colon. The major virulence factors are flagellar motility, adherance molecules to facilitate colonization, cytotoxins and a cholera like enterotoxin
|
|
|
Initially water but then it can turn Bloody diarrhea. Accompanied by fever and ab pain.
|
Shigellosis. Complications include Reiter syndrome, hemolytic-uremic syndrome. Route of transmission is Fecal-oral, food, water
|
|
|
Shigellosis affects what part of GI?
|
Left colon, ileum. Organisms highly resistant to gastric acidity, they are taken up by intestinal M cells, escape into the lamina propia and are ingested by macrophages that undergo apoptosis.
|
|
|
Watery or bloody diarrhea
|
Salmonellosis. Complications include. Sepsis, abscess. Found in Meat, poultry, eggs, milk
|
|
|
Salmonellosis affects
|
Colon and small intestine. Antibiotics not recommended because it prolongs the carrier state.
|
|
|
Pt presents with watery diarrhea, fever, ab pain, leukocytosis. Commonly found in hospital pt
|
Pseumembranous colitis by C. difficile.
|
|
|
Pseumembranous colitis affects
|
-The Immunosuppressed, antibiotic-treated
-Colon |
|
|
abdominal pain, bloody diarrhea, or weight loss; necrotizing colitis & megacolon. Examination reveals a Flask-shaped ulcers in colon,
|
Entamoeba histolytica (Amoebiasis). amoeba embolizes to liver causing abscess in 40% (also lung, heart, kidney, brain). Fecal – oral
|
|
|
Entamoeba histolytica (Amoebiasis) characteristics
|
Dysentery results when amoebae induce colonic epithelium apoptosis to invade the lamina propia and attract neutrophils.
|
|
|
→ diarrhea, malabsorption, weight loss. Normal, or villous blunting, & increased IEL. flagellated trophozoites in otherwise normal duodenal biopsies
|
Giardia lamblia. The most common pathogenic parasitic infection in humans
Fecal- oral Resistant to chlorine Endemic in unfiltered public H20 Swimming in contaminated water |
|
|
Giardia lamblia pathogenesis
|
cause decreased expression of brush-border enzymes, microvillous damage; apoptosis. Protective secretory IgA and mucosal IL-6 are important for clearance, so Giardia can persist for prolongued duration in immunocompromised
|
|
|
Self limited diarrhea in immunocompetent hosts but it can also cause chronic diarrhea
|
Cryptosporidium. Villous atrophy, crypt hyperplasia in terminal ileum and proximal colon, throughout the gut, biliary tract, and respiratory tract
|
|
|
Cryptosporidium pathogenesis
|
oocyte activated by gastric acid to produce proteases allowing release of sporozoites, actin polymerization with the brush border & and increased tight junction permeability leading to nonbloody, watery diarrhea.
|
|
|
Colorectal carcinoma usually arises from
|
adenoma-carcinoma sequence, however it can also arise from a second molecular pathway which is microsatellite instability
|
|
|
Hereditary nonpolyposis colorectal carcinoma is due to
|
inherited mutations in DNA mismatch repair enzymes, there is an increased for colorectal, ovarian, and endometrial carcinoma.
|
|
|
Hereditary nonpolyposis colorectal carcinoma arises
|
de novo (not from adematous polyps) at a relatively early age; usually Right sided.
|
|
|
left sided colon carcinoma usually grows as
|
napkin-ring lesion and presents with decreased stool caliber, left lower quadrant pain and blood streaked stool
|
|
|
Right sided carcinoma usually grows as
|
raised lesion; presents with iron deficiency anemia and vague pain. An older adult with iron deficiency anemia has colorectal carcinoma until proven otherwise
|
|
|
The serum marker useful for assesing tx response to colon carcinoma is
|
CEA and also helps detect recurrence, however it is not useful for screening.
|

