![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
What is another word for pin worms?
|
Oxyurids.
|
|
|
Where do Oxyuris equi live? What effect do they have?
|
Horse pinworm - Lower intestine – moderate to severe (but rare) inflammation and damage to mucosa
|
|
|
Where do horse pin worms deposit their eggs?
What would the presentation be? NEED TO KNOW |
They leaves anus to deposit eggs
_Itching, rectal irritation, tail rubbing_ |
|
|
At what age are horse pin worms infective?
When is their prepatency? NEED TO KNOW |
Eggs embryonate and are infective after _4-5_d.
Prepatency around _5 mo_. |
|
|
How do you treat horse pin worms?
What is the danger of this treatment? |
Usually responds well to ivermectin or pyrantel
But now resistance to ivermectin is being reported! “Virtually all three classes of dewormers are affective against pinworms, although there have been some reports of ivermectin failing to clear pinworm infections” |
|
|
How much time to pinworms spend outside of the intestines in their life cycle?
What is the signifigance in treatment in this? |
No _extraintestinal_migration
One of the only parasites that spend their whole life cycle in the lumen of the gut. This is signifigant in treatment because you only have to target one area. |
|
|
Besides horse pinworms, what other species are effected by pinworms?
What symptoms do these animals show? What is the signifigance of these particular animals having pinworm infections? |
Lab mice, rats, and rabbits.
symptoms are: poor condition, rough hair coats, reduced growth rate, rectal prolapse, glomerulonephritis, etc. Usually don’t cause overt clinical disease However….. Cause “non-protocol induced variation in research experiments” (due to the above symptoms) Differences in electrolyte transport and weight gain. Impact 5: Restrictions on shipments (this is the fifth impact from his first lecture of parasitic infections of food animals) |
|
|
What order do the "true strongyles" come out of?
|
Order Strongylida
|
|
|
What are hair worms also known as?
|
Trichostrongyloidea - they are little guys.
|
|
|
What is the family of Strongylida with the 6 most predominant genera in veterinary medicine? Of those 6, which is the most important?
|
Family Trichostrongylidae "trichostrongyles" - dominant gastro-intestinal nematodes of sheep and cattle, important in horses and pigs.
(often referred to as just "strongyles", but technically they are "trichostrongyles") Genus Trichostrongylus (we'll discuss) Genus Haemonchus - most prevalent (we'll discuss) Genus Ostertagia/Teladosargia (most prevalent in cattle. we'll discuss) Genus Nematodirus (we'll discuss) Genus Cooperia and others |
|
|
What do trichostrongyloidea predominantly cause?
|
parasitic gastroenteritis
|
|
|
What are trichostrongyles characterized by? (4 things)
|
being small (7-30 mm)
absence (or extreme reduction) of leaf crowns (corona radiata) absence or extreme reduction of buccal capsule presence of a well-developed bursa |
|
|
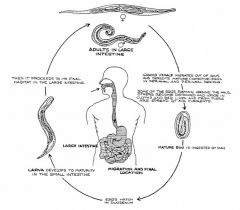
What is the life cycle of the trichostrongyle?
How long does it take to be infective? What is their period of prepatency? |
As the egg is released, the larvae quickly hatches and proceeds to L3 and then waits to be ingested by a grazing animal. So they have a few days in the environment before they are infectious.
Prepatency Period = 2-3 weeks. Once ingested, the L3’s penetrate the mucosa of the gut and hang out for a while before emerging patent. (right?) |
|
|
What is arrested development known as in parasitology?
Why do some worms do this? - NEED TO KNOW |
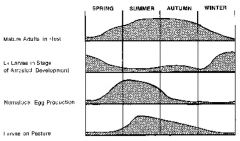
Understanding of epidemiology of some nematodes (e.g. trichostrongyles) is complicated by the fact that many species may undergo arrested development or hypobiosis.
Why? Probably complex, but may relate principally to helping worms survive over winter (or over-summer!). If a worm infects an animal in the fall, it doesn't do them good to have their eggs released in winter - the L4's just hang out in the tissues until they are triggered to release in the spring or summer to infect the next generation (that's important to know). |
|
|
What is spring rise?
What is its signifigance in worms? |
Spring rise = sudden rapid rise in fecal “eggs per gram” (epg) in spring.
Just in time to infect naïve, underyearlings Caused by completion of development of trichostrongyles in arrested development for winter. Further complicated by interplay of host's immune system – e.g., pregnancy in dogs with Toxocara infections |
|
|
how long will pinworm eggs wait to hatch?
|
could be months, until they are ingested and in optimal conditions
|
|
|
What is the infective delay of Haemonchus? How long will they remain infective?
What is the prepatency period? Do they undergo hypobiosis? How long do Haemonchus larvae in pasture? |
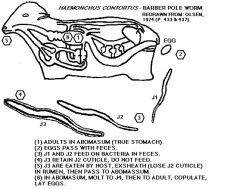
Egg to infective larvae: __4-6_d
Not immediately infective Infection to adult: about 2-3 wk Short prepatency Larvae in pasture: remain infective for About 6 mo. – long survival of off-host stage Hypobiosis In Oregon – seen in warm months |
|
|
Where do Haemonchus hang out in the host? How long do they get?
Why are the called the "Barber's Pole" worm? What is signifiganct about their buccal cavity. |

abomasum
Up to 30 mm long "Barbers Pole" worm - white gonads twisted around red blood-containing gut Buccal cavity has a small dorsal lancet for blood-letting. |
|
|
What are the pathologies/clinical signs of Haemonchus?
NEED TO KNOW |
_Anemia___
Edema, hypoproteinemia Lethargy Weight loss & death |
|
|
What are the analogs of ivermectin?
What is ivermectin effective against? |
Ivermectin (Merck) – the parasite wonder drug
Highly effective against nematodes and arthropods River blindness in humans (Onchocera volvulus) Lots of analogs – Ivermectin, Eprinomectin, Moxidectin, Selamectin, Doramectin and Milbemycin Milbemycins – related drugs |
|
|
What parasite started the resistance against ivermectin?
Why might we be in a hot spot? |
Extensively used to treat nematodes and arthropods in ruminants, small animals and horses
Now resistance has a problem – started with Haemonchus Resistance conferred across the group “Wonder Drugs” – so drug companies haven’t developed alternatives |
|
|
Where do resistant worms come from?
|
"resistant" worms exist within populations prior to the introduction of a drug. Genetic diversity in parasite populations is great. Initial frequency is very low because there's been no competitive advantage for them to thrive.
Treatment eliminates parasites whose genotype renders them susceptible. Parasites that are resistant survive and pass on their "resistant" genes. |
|
|
What causes resistance to dewormers?
|
Treating all animals at the same time.Frequent treatments - more than 3 treatments per year
Treating and moving to clean pasture - why is this bad? Under dosing Treating all animals at the same time. - one of the worst things to do - why? Treating when few larvae are on the pasture - if there are no worms in the pasture, you enhance the percentage of resistant parasites. |
|
|
What is the DRENCHRITE system?
|
Dr. Ray Kaplan, University of Georgia
Testing resistance in strongyle larvae in eggs Testing for benzimidazole/levamisole and avermectin/mibemycin (Ivomec, Cydetin) Eggs isolated from feces, placed in microtiter plates with drug Then development is followed Alternative to in vivo testing of drugs with fecal egg count (FEC) |
|
|
What is the FAMACHA system
|

Particularly useful in parasites that cause anemia. The idea is that you go through a herd, and screen animals by the color of their conjunctiva to determine if they are dose or no dose.
A strategy for treating stongyles (esp. Haemonchus) and reducing resistance Identify most severely affected animals by the presence of anemia (i. e., pale conjunctiva). Only treat severely affected animals Why would this reduce resistance?? (I don't know) |
|
|
At what percentage of resistance allele frequency does clinical detection occur?
|
50%
This emphasizes how important it is to stay on top of it, because once you can see it, it's too late> |
|
|
What is the infective stage of pinworms?
|
larval egg
|
|
|
How do sheep become infected with Haemonchus?
|
eat them
|
|
|
Characterize clinical disease associated with Haemonchus?
|
anemia
|
|
|
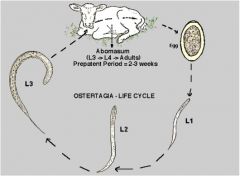
What is the most important strongyle of cattle?
|
Ostertagia ostertagia
|
|
|
Where do ostertagia ostertagia Teladorsagia spp like to hang out and in what species?
What color are they? Which end is their distinctive end? What are the distinguishing features? |
Teladorsagia spp.
in sheep & goats abomasum sheep, goats, cattle, rarely small intestine "brown stomach worms" because usually distinctively brown Front end not distinctive Distinguished by features of the bursa - accessory membrane and complex spicules. |
|
|
What are the two types of ostertagia in cattle?
|
Type-1 calves and young cattle (naïve) high burdens of adult worms in winter and spring.
Source of Infection: L3 larvae from heavily contaminated pastures in the autumn and winter after weaning. Dairy calves typically suffer type-1 disease at 5-6 months. Beef cattle are affected at 15-20 months. Type-2 disease (stress) – from hypobiotic larvae Beef cows calving for the first and second time in the autumn and winter. This coincides with the stress of calving and the emergence of thousands of inhibited L4 larvae from the lining of the stomach. “Pregnancy relaxation” Like small strongyles in horses Severe scouring, loss of weight and even death may result. Frequent drenching may be needed just to keep these cattle alive. Damage to mucosa causes pH rise. |
|
|
What causes the clinical disease in ostertagia in cattle?
|
The larvae
|
|
|
Which type of ostertagia in cattles is declining and why?
|
Decline of Type 2: "Avomec" drenches, and lower stocking rates of cattle on most properties.
|
|
|
Where do trichostrongylus spp. like to live and in what species? What are their distinguishing features?
|
Very small intestine sheep, cattle, (less often abomasum, stomach, horse & pig)
tiny worms <7 mm long no special distinguishing features on ant. end identifiable from others from ruminants, pigs & horses by size, lack of specialisation around mouth, short massive spicules and gubernaculum. T. axei – both cattle and sheep Infects abomasum |
|
|
What are the clinical presentations of trichostrongylus?
|
Diarrhea, not bloody. Weight loss.
|
|
|
What are the Effects of intestinal parasitism on growth in sheep
|
Sheep infected with 4000 L3 Trichostrongylus colubriformis per day for 83 days
Infected animals lost 48% fat lost 23% protein muscle reduced in diameter infected animals consumed 30% more feed than uninfected animal Interpreted as restriction in growth through “under nutrition” Following treatment compensatory growth occurred so that muscle recovered. |
|
|
What is the thin-necked worm of sheep? What are the different type? Is this a trichostrongyle?
What is the diagnostic feature? What is the pathology? |
It's a trichostrongyle
Nematodirus spp. – thin-necked worm of sheep Sheep: N. filicollis, N. battus, N. spathiger Cattle: N. helvetianus Diagnosis: huge egg - know why it has a huge egg! Pathology: acute diarrhea in young animals, esp. N. battus |
|
|
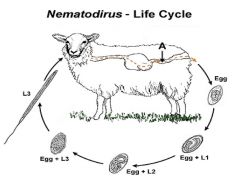
What is the life cycle of the trichostrongyle Nematodirus spp?
|
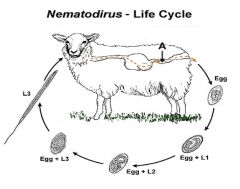
Life cycle: Direct, no extraintestinal development
|
|
|
Why is the egg of the trichostrongyle Nematodirus spp so big?
How long is its prepatency period? |
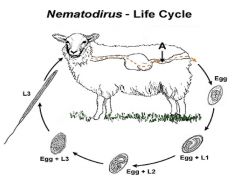
This is a strategy that the worm has developed to hang out in the egg stage much longer, which means that it needs to accommodate a larger larvae.
The preparasitic phase of Nematodirus is almost unique in the trichostrongyloids in that development to the L3 takes place within the egg shell. This development is generally very slow and in temperate climates takes at least two months. The parasitic phase is non-migratory and the pre-patent period is 15 days. |
|
|
What is the L3 infective stage of the trichostrongyle Nematodirus spp?
Does it go through hypobiosis? |
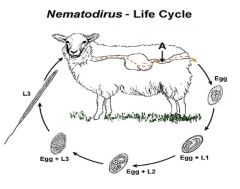
L3 infective stage, _comes from the egg__
N. battus in Europe. Requires chill then warming (> 10 C) before egg hatches Results in hyperinfections in spring Also undergoes traditional hypobiosis as L4s in sheep in North America |
|
|
What is the pathogenesis and clinical signs of Nematodirus spp
|
This is a trichostrongyle
Not usually a primary pathogen in ruminants in North America. However, Nematodirus battus does cause significant disease in lambs in Britain – concentrated L3s in spring Diarrhea followed rapidly by dehydration are the primary clinical signs. Adult ewes have developed a strong immunity to Nematodirus and are usually unaffected. |
|
|
What is premunition?
NEED TO KNOW |
Premunition – “A state of resistance to infection which is established after an acute infection has become chronic and which last while the organism is present”
Why trichostrongyles are a disease of young animals. |
|
|
Compare and contrast resistance and resilience
|
Resistance - don't get the infection.
Resilience - have the infection, but you aren't effected. |
|
|
What are the clinical signs produced by strongyles? And Haemonchus specifically?
|
abomasitis, anaemia, oedema, necrosis, reduction in weight gain, chronic diarrhea, emaciation, death.
Haemonchus - blood-letting. Reduced packed cell volume and haemoglobin level. |
|
|
How much blood might strongyles remove in a day to lead to their characteristic anemia? In what life stage might fatal infection occur?
|
Worms may remove 0.05 ml of blood/day;
5000 worms will remove 250 ml blood/day. Anaemia can be fatal and in acute infections may occur in pre-patent period. |
|
|
What is the difference between light and heavy infections of strongyles?
|
Light infections not dangerous - heavy infections significant
|
|
|
What should you know about trichostrongyles?
|
that they exist as a major group of parasites in sheep/cattle (horses/pigs)
where they occur - abomasum, small intestine, (stomach of horses) be able to recognise them as a trichostrongyle know some of the genera, esp. Haemonchus understand the life-cycle understand the pathogenesis |
|
|
What is the prepatency period?
|
Per Georgis: the time between infection and the appearance of detectable stages, for eg when tapeworm eggs found in the feces.
|

