![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
291 Cards in this Set
- Front
- Back
|
Name the 3 Cardiomypoathies?
|
1) Dilated
2) Hypertrophic 3) Restrictive |
|
|
What is the most common cause of Dilated cardiomyopathy?
|
Alcohol abuse
May also be idiopathic, infectious, or drugs. |
|
|
Dilated cardiomyopathy has symptoms similar to?
|
CHF
|
|
|
What is Dilated CM?
|
Cardiac dilatation leading to right and left systolic dysfunction and then CHF.
|
|
|
What is the first symptom of Dilated CM?
|
Exertional intolerance
|
|
|
Other S/S or dilated DCM?
|
-dyspnea, orthopnea, and edema in lower extremities.
-May have S3, chest pain, and crackles. |
|
|
DX of DCM?
|
EXG is diagnostic
Also get Cxt Xray and ECHO |
|
|
What are the ECG finding of DCM?
|
nonspecific ST and T wave changes and possible LBBB
|
|
|
What is the EF with DCM you would most likely see?
|
<30% EF
|
|
|
TX of DCM?
|
-Withdraw from alcohol
-TX CHF with diuretics, digoxin and sodium restriction. -ACE and Beta blockers, may need cardiac transplant if really bad. |
|
|
What is the most common cause of sudden death in young athletes?
|
Hypertrophic Cardiomyopathy
|
|
|
What is the death with HCM due to?
|
Ventricular arrythmias
|
|
|
What is the cause of HCM?
|
Autosomal dominant gene allele can be seen in most cases.
|
|
|
What happens on HCM?
|
-Hypertrophy of the cardiac septum leads to LV outflow obstuction and impaired diastolic filling.
|
|
|
And what does impaired diastolic filling lead to?
|
Pulmonary congestion
|
|
|
What is the most common presenting symptom of HCM?
|
Dyspnea on exertion
|
|
|
PE of HCM includes?
|
-mitral regurgitation
-possible angina and syncope -S4 -prominent left ventricular impulse |
|
|
How do you dx HCM?
|
Echo make the diagnosis
EF > 60% |
|
|
What does EKG reveal with HCM?
|
Left Ventricular Hypertrophy
|
|
|
TX of HCM?
|
-B-blockers(Propanalol)
-Ca channel blockers (Verapimil)-improves ventricular compliance. -Diuretics |
|
|
Restrictive Cardiomyopathy?
|
-Often caused by an infiltrative process
-Pulmonary congestion -Right sided heart failure |
|
|
What are the signs of Right Sided Heart Failure with RCM?
|
Elevated JVD
-may have S4, mitral and tricuspid regurgitation. |
|
|
DX of RCM?
|
ECHO is diagnostic
EF 25-50% and thickened LV wall thickness and increased atrial size Specific dx=tissue biopsy |
|
|
Tx of RCM?
|
Diuretics to tx CHF
|
|
|
What is an example of an infiltrative process that can cause RCM?
|
-Amyloidosis
-Sarcoidosis -Hemochromatosis |
|
|
Atrial Fibrillation
|

What is this?
|
|
|
What is the most common sustained arrythmia in adults?
|
Atrial Fibrillation
|
|
|
What is the increased risk with A fib that you have to worry about?
|
Inta-atrial clot formation, will need long term coagulation like Heparin acutely and Warfarin long- term.
Increased risk of stroke with the micro-emboli |
|
|
What are the EKG finding of A fib?
|
-Rapid, irregular-irregular atrial rate >400b/m
-A fib waves may be Coase, fine, and difficult to discern. -Vent rate 100-200 b/m - |
|
|
Tx of A fib?
|
1) Rate control(beta blockers, Ca channel blockers, or digoxin
2) Anticoagulation is vital 3) Rhythm control with Amiodarone and possible cardiioversion. |
|
|
What presents with a Sawtooth pattern of P waves?
|
Atrial Flutter
|
|
|
Where do you see the Sawtooth pattern of atrial flutter?
|
Leads II, III, and aVF
|
|
|
What are some to the S/S of atrial flutter?
|
-dizziness
-palpatations -cxt pain -dyspnea |
|
|
Treatment of A flutter?
|
-Cardioversion
-Beta blockers, calcium channel blockers |
|
|
Esmolol and Metroprolol are examples of?
|
Beta blockers
|
|
|
Verapimil and diltiazem are examples of?
|
Calcium channel blockers
|
|
|
Multifocal atrial tachycardia?
|
-Seen in pt's with COPD/severe systemic illness
|
|
|
EKG findings of MAT?
|
-Multiple shaped P waves
-Differing PR intervals |
|
|
What are the agents of choice for TX of MAT?
|
Calcium channel blockers
|
|
|
What is an AV block?
|
-defined as when some impulses are delayed or do not reach the ventricle.
|
|
|
What S/S may be noted with an AV block?
|
Syncope
|
|
|
Definition of a First Degree AV block?
|
-PR interval > .02 seconds
|
|
|
Definition of a second degree AV block?
|
-Some P waves fail to produce a QRS.
|
|
|
Mobitz Type I (Wenckebach)
|
-Progressive increase in PR interval, until a P wave is blocked, and the cycle is repeated.
-PR interval after interval is usually the longest |
|
|
Mobitz type II?
|
-Sudden block of a P wave with no change in PR interval.
|
|
|
Third degree block?
|
-Occurs when atria and ventricle are controlled by different pacemakers.
-Atria and ventricles are independent of each other. |
|
|
TX of Third degree block?
|
-Asymptomatic = no tx needed
-Correct reversible causes -May need atropine or isoproterenol -May need pacing |
|
|
What may develop after an acute MI on EKG?
|
Bundle Branch Block
May be seen with CM, pulm embolism, and aortic stenosis |
|
|
What is a BBB due to?
|
Conduction delay in the right or left bundle branches
|
|
|
RBBB
|
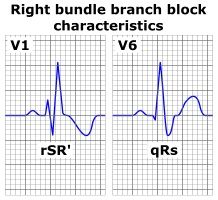
What is this?
|
|
|
Qualities of a RBB?
|
-Wide QRS >.11 seconds
-rSR in lead V1 -Wide terminal S wave in leads I and V6 -May note ST depression in V1 and elevation in I and V6 |
|
|
-Wide QRS
-Upright and notched QRS in lead I and V6 -Mostly negative QRS in lead V1 -ST elevation in V1 and depression in I and V6 |
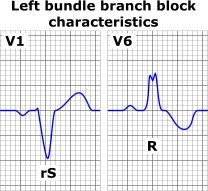
LBB?
|
|
|
WPW?
|
-WIde QRS
-A Delta wave is present at the start of the QRS complex -PR interval is short |
|
|
Tx for WPW?
|
-tx unerlying cause
|
|
|
What do you not use in WPW?
|
-Digoxin or Calcium Channel blockers, meds which slow down rate rare Contraindicated**
|
|
|
Paroxysmal Supraventricular Tachycardia?
|
-Re-entry Tachycardia
-Elderly with underlying disease -Also called AV nodal re-entry -Palpations/Anxiety |
|
|
What is the Tx of choice for PST?
|
-Adenosine (slows rate)
-Vagal man. or anti-anxiety meds too |
|
|
PAC?
|
-Underlying rhythm interupted by early beat from atria Other than SA node.
-Tx with antiarrythmic drugs. |
|
|
PVC?
|
-Underlying rhythm interupted by an early beat from the ventricles.
|
|
|
TX PVC?
|
-tx underlying cause
-May lead to life threatning Vent arrythmia -May need beta blockers |
|
|
V-Tach?
|
-Originates from below bundle of HIS at a rate > 100 b/m
|
|
|
What can cause V-Tach?
|
-electrolyte imbalances
-acid-base abnormalities -Hypoxemia -MI -Drugs |
|
|
S/S of V-tach if unstable?
|
-Syncope, cxt-pain, and dyspnea
|
|
|
What can V-tach cause?
|
-Sudden Cardiac Death!
|
|
|
Torsades De Pointes?
|
-Polymorphic VT in which the QRS complexes change in amplitude around the isoelectric axis.
|
|
|
TX Torsades De Pointes?
|
-Antiarrythmic
-cardioversion |
|
|
What can cause V-Tach?
|
-electrolyte imbalances
-acid-base abnormalities -Hypoxemia -MI -Drugs |
|
|
S/S of V-tach if unstable?
|
-Syncope, cxt-pain, and dyspnea
|
|
|
What can V-tach cause?
|
-Sudden Cardiac Death!
|
|
|
Torsades De Pointes?
|
-Polymorphic VT in which the QRS complexes change in amplitude around the isoelectric axis.
|
|
|
TX Torsades De Pointes?
|
-Antiarrythmic
-cardioversion |
|
|
Amiodarone, Lidocaine, and Procainamide are examples of?
|
-Anti-arrhythmics
|
|
|
Ventricular Fibrillation?
|
-Malignant arrhythmia with disorganized elecrical activity leading to failure of cardiac contraction and failure to maintain CO.
|
|
|
What type of pt's is V Fib seen with?
|
Ischemic heart disease
Left ventricular dysfunction |
|
|
V-Fib EKG?
|
-Irregular rhythm with and undulating low-amplitude baseline with no organized QRS or T-waves
|
|
|
Tx for V-fib?
|
Electrical Defibrillation!
|
|
|
V-Fllutter?
|
-Very rapid unstable form of VT
-Progresses to V-fib! -electrical defibrillation required |
|
|
Defect in the atrial septum allowing shunting of blood between the atria
|
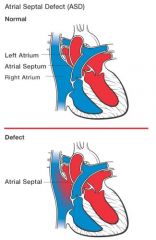
ASD
|
|
|
What is the most common type of ASD defect?
|
-Ostium Secundum defect noted in the mid-portion of the atrial septum
|
|
|
What can you see on PE for ASD?
|
-Slow weight gain history of
-Recurrent lower resp tract infections -Wide split S2 Pt may be asymptomatic |
|
|
What type of murmur is heard with ASD?
|
-Systolic Ejection Murmur in the pulmonic area
- Mid Diastolic Rumble in the lower right sternal border |
|
|
What are the murmurs and the rumble of ASD due to?
|
-increased flow across the pulmonic and tricuspid valves
|
|
|
Other findings of ASD?
|
Cxt-Xray=Cardiomegaly and increased pulmonary vasularity
EKG= Right ventricular hypertrophy with right ventricular conduction delay |
|
|
Diagnostic for ASD?
|
Echocardiogram
|
|
|
ASD tx?
|
-Spont closure in most cases in 1st year of life
-If sypmtomatic close as soon as possible -asymptomatic can close at 2-4 years of age. |
|
|
Murmur for VSD?
|
Pansystolic Murmur
|
|
|
Murmur for TOF?
|
Rough, systolic ejection murmur
|
|
|
Murmur for Aortic Stenosis?
|
Sys. ejection murmur at right upper left sternal border and a systolic click at the apex
|
|
|
Murmur for ASD?
|
-Fixed Split S2
-Sys. ejection murmur at left sternal border -Mid-diastolic murmur at the left sternal border, 4th intercostal space |
|
|
Murmur for PDA?
|
Continuous Machine-Like murmur
|
|
|
Cardiac findings for Coar. of Aorta?
|
-Decreased femoral pulses
|
|
|
Cardiac findings for Transp of Great Vessels?
|
Vary, depending on position of the VSD
|
|
|
What is best test to screen for congenital heart disease?
|
Echocardiogram
|
|
|
Turners syndrome
|
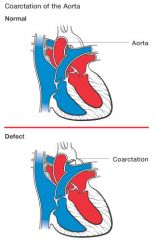
What syndrome in females is associated with Coarctation of the Aorta?
|
|
|
Where is the obstruction located with COA?
|
in the descending aorta, at the insertion of the ductus arterious.
|
|
|
Possible Clinical signs with COA?
|
-may be present w/or without symptoms
-May have CHF -Upper extremity hypertension -notched ribs maybe |
|
|
What about the pulses with COA?
|
absent or weak femoral pulses and delayed when compared to upper extremities.
|
|
|
Other possible findings of COA?
|
-Systolic ejection murmur at apex
-Enlarged aortic knob on cxt x-ray. -Right ventricular hypertrophy on EKG. |
|
|
What is dx of COA?
|
-Echocardiogram
|
|
|
connect aorta and the left pulmonary artery
|
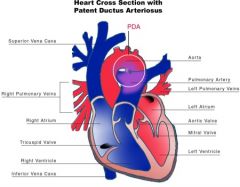
what is the function of the ductus arteriosis?
|
|
|
What type of shunt is associated with a PDA?
|
Left to Right shunt
|
|
|
When does the PDA typically close?
|
by 4 days of age
|
|
|
S/S of PDA?
|
-Small defect-no symptoms
-Large defect-CHF, slow growth, recurrent resp infections. -SOB,DOE, Cyanosis |
|
|
What type of murmur with a PDA?
|
Bounding pulses and a Machine-Like Murmur
-Murmur starts after S1, peaks at S2, and softens during systole |
|
|
Other findings of PDA?
|
Chest X-ray-small PDA-normal
Large PDA-cardiomegaly, left atrial enlargement, and increased pulmonary congestion EKG-left bi- ventricular hypertrophy may be noted with a large PDA. |
|
|
What confirms PDA?
|
Echocardiogram
|
|
|
What is the treatment for closing PDA?
|
-Indomethacin (decreases prostoglandin levels)
-May need surgical ligation |
|
|
What is a cause of cyanotic congenital heart disease?
|
TOF
Cyanosis due to right to left shunting and decreased pulmonary flow. |
|
|
4 defects of TOF?
|
1) VSD
2) Right ventricular outflow obstruction lesion 3) Right ventricular hypertrophy 4) Overriding large ascending aorta |
|
|
Neonates with TOF present cyanosis and agitation, this is a?
|
Tet spell
|
|
|
Murmur with TOF?
|
Loud systolic ejection murmur at the left sternal border
|
|
|
EKG of TOF?
Chest X-ray with TOF? |
EKG-right atrial enlargement
Chest X-ray- normal heart size and decreased pulmonary vascularity |
|
|
Echo of TOF?
|
right thick ventricular wall, overriding aorta, and VSD
|
|
|
Treatment of TOF?
|
Surgical tx at about first 3-6 months of life.
-Acute tx-vagal man, O2, vasoconstrictors, B-blockers, morphine, and fluids. |
|
|
Echo of TOF?
|
right thick ventricular wall, overriding aorta, and VSD
|
|
|
Treatment of TOF?
|
Surgical tx at about first 3-6 months of life.
-Acute tx-vagal man, O2, vasoconstrictors, B-blockers, morphine, and fluids. |
|
|
What is the most common congenital heart defect?
|
VSD
-increased communication between right and left ventricles -increased pulm blood flow that may lead to pulmonary hypertension |
|
|
S/S of VSD?
|
-Tachypnea, tachycardia, poor weight gain, trouble feeding, and edema.
|
|
|
What type of murmur with VSD?
|
Holosystolic murmur best heard at middle of left sternal border
|
|
|
Chest X-ray
EKG with VSD |
Cxt- cardiomegaly and increased pulmonary vascularity in large defects
EKG- left atrial, ventricular, or biventricular hypertrophy. |
|
|
Diagnostic for VSD
|
You guessed it, ECHO
|
|
|
What is the tx for VSD?
|
-most close by 10 years old
-large VSD may need surgical repair |
|
|
What can lead to heat failure, CHF?
|
-Valvular heart disease
-CAD -arrythmias -hypothyroidism -high cardiac output syndromes -Hypertension! Disease precipitents |
|
|
What is a big cause of cardiac failure with HTN?
|
-Medication complaince, they don't take their damn meds!
|
|
|
Presenting symptoms of CHF?
|
-Dyspnea, orthopnea, PND, fatigue, exercise intolerance, and edema
|
|
|
PE and S/S of CHF
|
PE- restless dyspneic pt
S/S-JBD, rales, right upper quadrant tenderness, ascites and peripheral edema |
|
|
Labs?
|
-Elevated liver fxn
-Elevated B-natriuretic peptide -Pre-renal azotemia Check CBC and TSH to r/o anemia and tyroid disease as possible causes of failure |
|
|
Chest X-ray with CHF?
|
-Cardiomegaly
-Increased pulmonary vasculature -Kerley B lines -Pleural Effusions |
|
|
Kerley B Lines?
|
Think CHF
|
|
|
EKG CHF?
|
LVH and possible acute MI
|
|
|
ECHO of CHF
|
-systolic/diastolic dysfunction
-decreased EF |
|
|
TX of CHF
|
-DC smoking
-diet control -Low sodium to 1-2 mg daily |
|
|
Pharm tx for CHF?
|
-Diuretics
-ACE -Vasodilators -Beta Blockers -Digitalis -O2, Morphine * ASA, NSAIDS, Ca Channel blockers should be avoided |
|
|
Class I heart failure?
|
-No cardiac symptoms with ordinary activity
|
|
|
Class II heart failure?
|
-Cardiac symptoms with marked activity but asymptomatic at rest
|
|
|
Class III heart failure?
|
-Cardiac symptoms with mild activity but asymptomatic at rest
|
|
|
Class IV heart failure?
|
-Cardiac symptoms at rest!
|
|
|
What are some examples of end organ damage with HTN?
|
-Left ventricular hypertrophy
-Angina -Heat Failure -Stroke -Chronic Kidney disease -Peripheral artery disease -Retinopathy |
|
|
DX of HTN is based on?
|
2 or more elevated BP readings
|
|
|
What may the EKG with HTN show?
|
LVH
|
|
|
What is normal BP?
|
<120/<80
|
|
|
Prehypertension?
|
120-139/80-89
|
|
|
Stage 1 HTN?
|
140-159/90-99
|
|
|
Stage 2 HTN?
|
>160/>100
|
|
|
TX of HTN?
|
1) Lifestyle changes
2) Drugs |
|
|
Lifestyle changes for HTN?
|
-Wt loss
-Ltd alcohol -Reg aerobic exercise -DC smoking -Reduce Sodium intake -Reduce sat fats and cholesterol intake |
|
|
Drug therapy with Stage 1 hypertension?
|
140-159/90-99
1) Diuretics or Beta blockers other options: 2) ACE, Ca channel blockers, and alpha blockers |
|
|
What is Secondary Hypertension?
|
Hypertension due to an identifiable cause
Secondary to a disease process |
|
|
Some examples of Secondary HTN etiologies?
|
-RV disease
-Coar of Aorta -Primary Aldosteronism -Cushing's Syndrome -Phenochromocytoma -OSA -Kidney disease |
|
|
Tx of Sedondary HTN due to RV disease?
|
-Beta blockers with elevated Renin
-No ACE with bilateral renal artery stenosis -Diuretics with ACE combo -Surgical revascularization |
|
|
What is Malignant HTN?
|
-Potentially life-threatening situation
-HTN + retinopathy, CV, or renal compromise or encephalopathy. |
|
|
Etiologies of Malignant HTN?
|
-Acute aortic dissection
-Post coronary artery bypass graft -Acute MI -Unstable Angina -Eclampsia -Head Trauma -Severe Burns |
|
|
So Malignant HTN really is?
|
HTN with end-organ disease
|
|
|
Dx of Malignant HTN?
|
Elevated BP >220/140
in the presence of headache, blurred vision, N&V, confusion, seizures, hypertensive retinopathy, heart failure, and oliguria |
|
|
TX of Malignant HTN?
|
-Gradual decrease in BP by 10% in the first hour of tx and then 15% over the next 3 hour-12 hours, to a target BP of 170/110
|
|
|
Choice of agents varies with cause:
|
-Nitrroprusside
-Propanalol -Oral Clonidine (sedation) |
|
|
What would you use for HTN emergency in a pt with hyupertensive encephalopathy, intracrainial bleeding, and heart failure.
|
IV Nitroprusside
|
|
|
Nitroprusside in combo with what for dissecting aneurysm?
|
-Propanalol
|
|
|
What is Cardiogenic shock?
|
Tissue hypoperfusion due to an acute MI or end-stage heart failure
-Poor prognosis -Accounts for most deaths after an acute MI! |
|
|
Etiologies of Cardiogenic shock?
|
-Acute MI
-Tachyarrythmia -Valvular heart disease -Traumatic Cardiac injury -Myocarditis |
|
|
What is Hypotension defined as?
|
-Systolic BP <90 or a decrease from baseline by >30
|
|
|
Symptoms of Cardiogenic shock?
|
-altered mental status
-cyanosis -oliguria -cool, clammy extremities -Hypoperfusion/hypovolemia -acute MI on EKG may be noted |
|
|
What is helpful with dx of Cardiogenic shock?
|
Echocardiogram
|
|
|
TX of Cardiogenic shock?
|
-Adequate oxygenation and treatment of arrythmias very important.
-Improve BP is critical with IV fluids -Vasopressers (Dopamine, Dobutamine) -Intra-aortic baloon pump |
|
|
Orhtostatic/Postural Hypotension?
|
-May result in Syncope that could be recurrent
-Defined as a fall in systolic BP of 30 or more or 10 or more in diastolic between laying and upright position. |
|
|
Many etiologies of orthostatic HTN
|
-Antipsychotics
-Diuretics -Alpha-Adrenergic blockers -ACE inhibitors -Alcohol -Tranquilizers -Vasodilators -Methyldopa -Polyneuropathies -Parkinson's DZ |
|
|
Clinical manifestations of Orthostatic HTN?
|
-change in mental status, cerebral hypoperfusion, weak pulse, cool extremities, reduced urine output, tachypnea, and tachycardia.
|
|
|
Tx of Orthostatic Htn?
|
Tx underlying cause, remove offending medications, and support BP.
|
|
|
What is Acute MI?
|
-Myocardial necrosis brought on by ischemia
-Most deaths occur w/i one hour of onset of symptoms |
|
|
What is most deaths of acute MI caused by?
|
-Ventricular fibrillation
Need Rapid Defibrillation!! |
|
|
S/S of Acute MI?
|
-Retrosternal pain, heavy, pressure-like, squeezing, or bandlike.
-Pain may radiate to the jaw, neck or left arm -Pain typically is > 20 minutes -Watch for atypical MI presentation in Elderly and Diabetics |
|
|
Associated symptoms of Acute MI?
|
-N&V
-Diaphoresis -Dyspnea -Weakness |
|
|
What may you see on PE?
|
-Elevated BP and possible S4 and other signs of HF may be present.
|
|
|
Lab studies for Acute MI?
|
-Myoglobin
-CPK -Troponin -Leukocytosis -Lipid profile -C-reactive protein |
|
|
When is Myoglobin detectable?
|
-1-2 hours post MI
-Found in skeletal and cardiac muscle |
|
|
CPK?
|
-Total CPK correlates with infarct size
-CPK-MB is specific for cardiac muscle |
|
|
Troponin?
|
Test of choice*****
-Not normally present in blood -Elevated in acute MI -2-6 hours post MI for up to 5-10 days. |
|
|
EKG on Acute MI?
|
-ST elevation depending on affected wall
|
|
|
Inferior MI?
|
Leads: II, III, AVF
Artery involved: RCA |
|
|
Lateral MI?
|
Leads: I,aVL, V5, V6
Artery involved: Circumflex |
|
|
Anterior MI?
|
Leads: V1-V4, I, aVL
Artery involved: LCA |
|
|
Posterior MI?
|
Leads: V1,V2
Artery involved: RCA, Circumflex |
|
|
Apical MI?
|
Leads: V3-V6
Artery involved: LAD, RCA |
|
|
Anterolateral MI?
|
Leads: I, aVL, V4-V6
Artery involved: LAD, Circumflex |
|
|
Anteroseptal?
|
V1-V3
LAD |
|
|
What confirms location of injury and coronary vessel involved?
|
Coronary angiography
|
|
|
Treatment of acute MI?
|
1) MONA + Beta Blockers
2) Thrombolytic therapy (Streptokinase and tPA) 3) Anti-platelet tx(ASA, Plavix) 4) Nitrates 5) B-blockers 6) Ace but not with hypotension 7) Antithrombin tx (Heparin) |
|
|
What do nitrates with MI do?
|
Induce vascular smooth muscle relaxation and reduce cardiac preload and afterload
|
|
|
What do B-Blockers do with MI?
|
-Reduce HR, BP, Myoc contractility, and stabilize the heart electrically.
-Limits Myoc O2 consupmtion |
|
|
What do ACEs do with MI?
|
-Improves remodelling after an acute MI
-Avoid in presence of hypotension |
|
|
What is Stable Angina?
|
-Pain that builds up rapidly in 30 seconds and dissapears w/i 5-15 minutes
-Improved with Nitro -Precipitated with activity and relieved by rest -Related to a fixed stenosis of one or more Coronary atreries |
|
|
Pain with Stable Angina?
|
-Tightness, squeezing, aching or dull discomfort
-Pain is midsternal with radiation to the neck, left shoulder, or left arm |
|
|
What may be heard with Stable Angina?
|
S4 or S3 gallop
|
|
|
EKG with Stable Angina
|
When pain free may reveal arrythmia, prior MI, or LVH
During Pain may have St depression and T wave inversion. |
|
|
DX of Stable Angina?
|
-Exercise testing
-Perfusion Scintigraphy -Coronary angiography |
|
|
TX of Stable Angina besides life-style?
|
-Lipid managment
-Antiplatelet meds -Beta Blockers -ACE -Nitrates -Calcium channel blockers -Revascularization |
|
|
What is the tx of choice for WPW?
|
-Ablation therapy
|
|
|
Define Unstable Angina
|
-Angina at rest*
-New onset angina -increasing angina |
|
|
Unstable angina may be due to?
|
Plaque rupture
Nonocclusive thrombus |
|
|
S/S of Unstable angina?
|
-dyspnea, palpatations, and fatigue
-pressure, burning, or squeezing pain -may have Nausea, SOB, and diaphoresis -Pain is retrosternal and epigastric |
|
|
What else may you find on PE with unstable angina?
|
-S4 gallop, mitral regurg murmur, and rales on lung exam
-May have normal EKG -Normal cardiac labs |
|
|
Tx of Unstable Angina?
|
Same as stable
|
|
|
Prinzmetal's Angina?
|
-Pain mostly at rest
-May awaken pt in the morning -Caused by occlusive spasm on a non-severe coronary artery stenosis -May be associated with Raynaud;s phenomenon and Migraine |
|
|
Acute Rheumatic Fever?
|
-Inflammatory disease that occurs as a response to an URT infection due to Group A Streptococci
-Proliferative and exudative inflammatory lesions on conn tissue, heart, joints, and SubQ tissue -Peak incidence in 5-15 years of age |
|
|
Jones Criteria for Acute Rheumatic Fever
Major criteria |
JONES
Joints=Polyarthritis O-obvious= Heart (carditis) N=nodule(Rheumatic) (knees, elbows, and wrists) E= Erythema Marginatum S= Syndecham Chorea (rapid, purposlesness, involuntary movements). |
|
|
Jones minor
crITERIA |
Inflammatory cells (Leukocytosis)
Temperature (fever) Esr/CRP elevation Raised PR interval Itself (previous hx of RH Fever-recent strep infection) Arthralgia |
|
|
Tx of Rheum fever
|
-Asa
-Steroids Pen G or V or sulfadiazine or Emycin for pen allergy |
|
|
Aortic Aneurism?
|
-Pathological dilation of Aorta
*most common is Abdominal AA -Atherosclerosis is major underlying cause |
|
|
Symptoms of AA
|
-hypogastric or low back pain
-with rupture pain worsens with drop in BP -Steady gnawing pain -Pulsatile abdominal mass |
|
|
DX of AA?
|
Ultrasound for screening
and CT for diagnostic* |
|
|
Older pt with flank pain and new onset hematuria what should you suspect?
|
AAA
May be misdiagnosed as renal colic |
|
|
TX of AAA
|
Serial imaging and beta blockers to reduce aortic pressure
Imaging every 6 months for AA > 4 cm |
|
|
AA > 5 cm?
|
Should be surgically repaired!
|
|
|
Aortic Dissection?
|
Tear in the aorta intima, blood enters the media, cleaving it into 2 layers.
|
|
|
What pts are at increased risk of Aortic Dissection?
|
1) Marfan syndrom
2) 60-80 year olds with history of htn |
|
|
Clinical manisfestations of Aortic Dissection?
|
-Severe retrosternal pain described as Tearing, Sharp**
-Elevated BP -Pulse deficits -Enlarged Mediatstinum on X-ray |
|
|
DX of Aortic Dissection?
|
CT, aortograph, MRI or transesophageal echocardiogram
|
|
|
Treatment of Aortic Dissection?
|
-BP control with beta blocker, nitroprusside, calcium channel blocker.
-Surgical repair is definitive treatment* |
|
|
S3?
|
CHF
|
|
|
S4?
|
MI
|
|
|
Arterial embolism/Thrombosis
|
-Cause of acute arterial insufficiency
-Arterial embolism secondary to many factors (Afib, flutter,mitral stenosis, trasnmural infarct, trauma,hypercoag states, and postarterial procedures). |
|
|
How does emobolism/thrombosis present?
|
-acute onset of pain, diminished pulses, cold limbs, and cyanosis.
-Typically unilateral presentation |
|
|
What are the 5 Ps of of embolism?
|
1) Pain (constant, worse with any mvmt)
2) Pallor (followed by cyanosis) 3) Pulseless (with cold limb) 4) Parasthesis (periph nerve damage) 5) Paralysis (damage to muscle and motor nerves) |
|
|
Diagnosis of Embolism
|
Echo to eval for source of thrombus
Arteriogram to id location |
|
|
Complications of embolsim?
|
-Compartment syndrome
-Limb loss |
|
|
TX of embolism?
|
-Heparin immedately.
-Embolectomy-thrombectomy |
|
|
Chronic Arterial Occlusion?
|
-decrease in 50% of arterial lumen will produce clinical symptoms, ischemia, and necrosis
|
|
|
Most common cause of chronic arterial occlusion?
|
Atherosclerosis
|
|
|
Most common site of CAO?
|
Lower extremities
|
|
|
Clinical signs of CAO?
|
Pain
Calf pain area of occlusion is DISTAl to the site of claudication -decreased peripheral pulses, bruits,ischemic skin changes, and painful ischemic ulcers |
|
|
DX of CAO?
|
-Ankle/Brachial Index
>1.0 = normal 0.5-0.9=arterial claudication <0.4 = Severe arterial stenosis**** |
|
|
TX of CAO?
|
1) Pentoxifylline
2) Aspirin 3) Ticlopidine 4) Thromboendarterectomy 5) quit smoking 6) Heparin and warfarin no use here |
|
|
Giant Cell Arteritis?
|
-A granulomatous vasculitis that affects the temporal artery.
-Pts > 50 -May coexist with Polymyalgia Rheumatica |
|
|
What is the most common symptom of Giant cell arteritis?
|
-New onset of headache, located in the temporal region***
-Jaw claudication/visual disturbances -Transient vision loss/blindness |
|
|
PE of GCA?
|
-Enlargement, tenderness, and erythema may be noted of the artery
-Bruit may be present |
|
|
Labs of GCA?
|
-Elevated ESR
-Anemia -Leukocytosis |
|
|
Dx of GCA?
|
Biopsy
|
|
|
Tx of GCA?
|
-Start corticosteroids as soon as possible
|
|
|
What is the best screening tool for AAA?
|
Ultrasound for screening
|
|
|
Phlebitis/Thrombophlebitis?
|
-Inflammatory thrombosis involving the superficial veins of the lower extremity.
-Associated with varicose veins pregnancy, and catheter placement. Septic with IV drug users. |
|
|
TX of Phlebitis?
|
-Warm moist compress
-NSAIDS -Abx for staphylococci of septic |
|
|
II, III, AVF?
|
Inferior
|
|
|
V1-V3?
|
Anteroseptal
|
|
|
V2-V4?
|
Anterior
|
|
|
I,aVL, V4,V5,V6?
|
Lateral
|
|
|
V1-V2?
|
Posterior
|
|
|
What is the common cause of Endocarditis in the normal populaton?
|
Strep Viridans
|
|
|
What is the cause of Endocarditis in drug users?
|
Staph Aureus
|
|
|
Cause of Endocarditis with prosthetic valves?
|
S. Epidermidis
|
|
|
A development of clot in the deep veins of the extremities or pelvis is a?
|
DVT (Venous thrombosis)
|
|
|
Risk factors for DVT include?
|
-Venous stasis
-Activation of the coagulation system -Vascular damage and many others.... |
|
|
S/S of DVT?
|
Pain and swelling at the site and DISTAL from the clot
|
|
|
Homan's sign?
|
Pain with dorsiflexion of the foot, may be positive for DVT
|
|
|
DX of DVT?
|
-Compression ultrasound and venogram are diagnostic
-d-Dimer rules out thormbosis in pts with low proabability for DVT |
|
|
TX of DVT includes?
|
-LMWH
-Elastic stockings -Intermitt pneumatic leg compression -Heparin until warfarin levels are therapuetic -Invferior vena cava filter may me needed to prevent PE with pts contraind for anticoag tx. |
|
|
What are Varicose veins?
|
Incompetence of the Saphenous vein
-defective valves -often in the medial and anterior thigh, calf, and ankle. |
|
|
PE of Varicose Veins?
TX of? |
-Torturous veins that are easily compressed
-Support stockings -surgical -sclerosing agent |
|
|
Etiology: Rheumatic
Symptoms: Angina, Syncope Cardiac signs: Loud, rough systolic ejection murmur EKG: LVH Chest X-ray: Boot shaped heart |
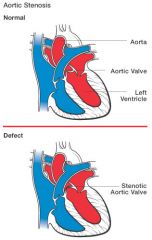
Aortic Stenosis?
|
|
|
DX and tx of Aortic Stenosis?
|
Dx: Cardiac Cath
TX: Tx CHF if present, No ACE, valve replacement, SBE abx prophalaxis is required |
|
|
Aortic Insufficiency?
|
E: Rheumatic
S: DOE, syncope, chest pain, CHF CS: Water hammer pulses, S3, Austin Flint Murmur, LVH |
|
|
DX and TX of AI?
|
DX: Cardiac cath confirms wide pulse pressure
TX: SBE antibiotic prophylaxis tx CHF, Surgical valve replacement |
|
|
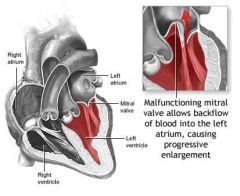
Mitral Stenosis?
|
Etiology: Rheumatic
Symptoms: Dyspnea, orthopnea, angina, hemoptysis Cardiac signs: Diastolic rumble, opening snap EKG: Chest x-ray: Straight left heart border. |
|
|
DX and TX of Mitral Stenosis?
|
DX: Echo and cardiac cath, with EKG of left atrial enlargment and A-fib
TX: Tx fib and CHF, SBE proph, valve replacement |
|
|
Mitral insufficiency
|
Holosystolic murmur at apex with radiation to the base or left axilla, may have S3
|
|
|
More common in young females
Crescendo mid to late systolic murmur |
MVP?
|
|
|
Tricuspid insuff?
|
Holosystolic murmur along left sternal border
|
|
|
Mitral Regurg murmur?
|
Holosystolic apical murmur
|
|
|
Aortic Stenosis Murmur?
|
Loud, rough, systolic diamond shaped murmur heard best a the base of heart with radiation to the neck.
|
|
|
Mitral Stenosis Murmur?
|
Soft, low pitched, diastolic rumble head best a the apex in the left decubitus position
|
|
|
Where do you hear a Austin Flint murmur?
|
With Aortic Insufficiency
|
|
|
Tx for Viridans Strep?
|
Pen G or ampicilln plus gentamycin or seftriazone plus gentamycin or Vancomycin
|
|
|
Acute/Subacute Bacterial Endocarditis (SBE)?
|
-Infection of the endothelial surface of the heart
-More common in Elderly people and males |
|
|
Predisposing factors of SBE?
|
-MVP
-Deg Vasc disease -IV Drug Use -Prosthetic Valves -Congenital abnormalities |
|
|
Most common community acquired SBE organism?
|
Viridans Streptococci
|
|
|
Nosocomial SBE?
|
Stpah epidermidis
|
|
|
Prosthetic valve SBE?
|
S epidermidis
S aureus Enterococci |
|
|
S/S of SBE?
|
Fever, fatigue, malais, weight loss, arthritis, and myalgias
|
|
|
PE or SBE reveals?
|
-Petechiae
-Olser's nodes -Janeway's lesions -Splinter Hemorrhages -Roth's spots of fundo exam -Cardiac murmur -Splenomegaly |
|
|
Labs to check for SBE?
|
ESR, CBC, Urinalysis(for hematuria)
|
|
|
What is the name of the criteria for dx of SBE?
|
Duke Criteria
|
|
|
TX of SBE?
|
Empiric tx depending on cultures
|
|
|
GIve abx prophalaxis for these procedures with pts at risk.
|
-dental
-tonsilectomy -surgery of resp mucosa -Sclerotherapy of esoph varices -Gallbladder surgery -Cytoscopy |
|
|
Acute Pericarditis?
|
Inflammation of the Pericardium
|
|
|
Clinical Manifestations of Pericarditis?
|
-Chest pain taht worsns with deep breathing, cough, or laying down.
--Pain with sitting or leaning forward -Pericardial friction rub -ST elevation -Pericardial effusion on ECHO |
|
|
TX of pericarditis?
|
-NSAIDS
-Steroids -Pericardiectomy for restrictive pericarditis |
|
|
Cardiac Tamponade?
|
-Accumulation of fluid that results in an increase in pericardial pressure and impairs ventricular filling, us a complication of pericardial effusion.
|
|
|
What do you see with Cardiac Tamponade?
|
-hypotension, bradycardia. DOE
-Distended neck veins, muffled heart sounds, narrow pp, and pulses paradoxus |
|
|
DX and tx of Cardiac Tamponade
|
DX: Echo
TX: Pericardiocentesis by echo guidance |
|
|
Pericardial effusion?
|
-Porlonged and severe inflammation leads to fluid accumulation around the heart can lead to cardiac tamponade
- May note diminished heart sounds and friction rub |
|
|
What does the heart look like with with pericardial effusion?
|
-Enlarged water bottle-shaped heart
|
|
|
TX of Pericardial effusion?
|
Pericardiocentesis confirms and treats
|

