|
|
Palliative care is an approach which improves
quality of life of patients and their families
facing life-threatening illness, through the
prevention and relief of suffering by means of
early identification and impeccable
assessment and treatment of pain and other
problems, physical, psychosocial and
spiritual (WHO 2002).
|
|
|
|
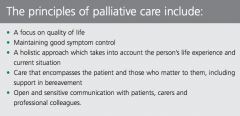
DOMAIN 1 PRINCIPLES OF PALLIATIVE CARE Palliative care aims to improve the QOL of people with life-limiting conditions and their
families, not only by treating their physical symptoms but also by attending to their psychological, social and spiritual needs. Palliative care is applicable for people of any age and may be integrated at any point in the disease trajectory from diagnosis through the continuum of care to bereavement.
|
Domain 1 Indicators
As a health care professional you should:
• Understand and be able to describe the meaning of the term ‘life-limiting condition’
• Understand and be able to apply the principles of palliative care that affirm life, offer people
with life-limiting conditions a support system to help them live as actively as possible until
death with optimal quality of life and help families cope during illness
• Understand the significance of the physical, psychological, social and spiritual issues that affect
people with life-limiting conditions and their families throughout the continuum of care
• Demonstrate the ability to use the palliative care approach as early as is appropriate in order
to facilitate person-centred practice that recognises the concerns, goals, beliefs and culture of
the person and her/his family
• Provide empathetic care to individuals with life-limiting conditions and their families, with clear
regard to the individuality of each person
• Show a commitment to one’s own continued professional development and learning and
facilitate the learning and development of others, in order to improve care for those with lifelimiting
conditions and their families
• Show a commitment to developing self-care strategies and to attending to any impact that
working with people facing life-limiting conditions and their families may have on you.
|
|
|
Domain 1 ALL NURSES
As a registered nurse caring for people with life-limiting conditions you should:
• Understand and recognise common trajectories of life-limiting conditions
• Understand the impact that psychological responses, social stressors and spiritual
dimensions to loss may have on the mental health and decision making of the
person with a life-limiting condition and their family and take this into account
when planning care
• Understand, recognise and address pathological responses to loss which may
impact on the mental health and decision-making of individuals and families
• Provide education to people with life-limiting conditions, their carers and
colleagues in the context of your role and at an appropriate level
• Take cognisance of the potential role of specialist palliative care services in
supporting staff in other agencies to provide a palliative care approach to persons
with a life-limiting condition.
|
DOMAIN 2 COMMUNICATION Effective communication is essential to the application of palliative care principles and to the
delivery of palliative care. Communication is particularly important where bad news has to be
relayed, when difficult decisions regarding treatment continuance and/or cessation are to be made
and where the communication needs of the person with a life-limiting condition and their family
differ. Communication is also important where circumstances are ambiguous or uncertain and
when strong emotions and distress arise. Specific consideration should be given to communication
as a method of:
• Supporting and enabling therapeutic relationships with a person with a life-limiting condition
and her/his family
• Ensuring that the person and her/his family understand and participate in decision-making
regarding care to the extent that she/he is able to and wishes to be involved
• Enabling inter-professional teamwork.
|
|
|
Domain 2 Indicators
As a health care professional you should:
• Understand the essential role communication plays in palliative care
• Understand the different types of communication e.g. verbal, non-verbal, visual, written, and
interpersonal interaction (either one-to-one or with a group or team)
• Demonstrate the ability to communicate effectively with the person with a life-limiting
condition, their family and the interdisciplinary team in order to establish, maintain and
conclude a therapeutic relationship
• Demonstrate the ability to communicate effectively with individuals and families from diverse
cultures and different backgrounds, using professional interpreters (Appendix 1) where
necessary and/or assistive communication technology where necessary
• Be able to modify your own communication style to facilitate communication with individuals
with a range of communication impairments or seek facilitation in this area if required.
• Understand the importance of using strategies that empower effective communication e.g.
active listening, plain language, appropriate tone, clarifying statements, inviting questions
• Demonstrate an ability to be attentive to the person through careful listening to help the person
and their families feel they have been heard
• Support individuals (or parents in the case of children and minors) to make informed decisions
regarding the level of information they wish to receive and want to share with their family
• Act as an advocate for the person and their family to ensure appropriate and timely palliative
care intervention.
|
Domain 2 ALL NURSES
As a registered nurse caring for people with life-limiting conditions you should:
• Be able to assess the person’s current understanding of their health status
• Be able to address questions regarding diagnosis and likely prognosis in an accurate
and empathetic manner, taking account of the person’s needs and wishes, and
referring where appropriate
• Understand that the communication of information which fundamentally changes
the person’s understanding of their situation and/or influences their decisionmaking
or planning is an on-going process and not a single event
• Recognise and contribute to the management of potential conflict in decisionmaking
in the context of palliative care.
|
|
|
DOMAIN 3 OPTIMISING COMFORT AND QUALITY OF LIFE
Individuals with life-limiting conditions and their families can be affected not only in physical, but
also in psychological, social and spiritual ways. Optimising comfort and quality of life for the person
with a life-limiting condition and her/his family is a dynamic process that involves anticipating,
acknowledging, assessing and responding to a range of symptoms and needs in a proactive and
timely manner in order to prevent and relieve suffering.
|
Domain 3 Indicators
As a health care professional you should:
• Understand the significance of anticipating and responding to the needs of people with lifelimiting
conditions and their families (e.g. physical, psychological, social and spiritual) in a
proactive and timely manner
• Understand how the palliative care approach can enhance the assessment and management
of symptoms
• Exhibit an ability to apply a range of assessment tools to gather information
• Be able to evaluate non-complex interventions and propose alternative actions if deemed
necessary
• Recognise the importance and benefit of multidisciplinary working in optimising comfort and
enhancing the quality of life of the person with a life-limiting condition and her/his family
• Recognise the ways in which people with life-limiting conditions and their families can be
engaged in self-management of their condition.
• Demonstrate professional awareness of the scope of, and benefits of, timely and appropriate
access to specialist palliative care services
• Be aware of the uniqueness of a good death and facilitate the achievement of this as much as
possible
|
|
|
Domain 3ALL NURSES
As a registered nurse caring for people with life-limiting conditions you should:
• Be able to assess a person with a life-limiting condition and recognise the role of
palliative care in enhancing that person’s care
• Be able to describe common chronic illnesses, the expected natural course and
trajectories, common treatments and complications
• Be able to assess and manage uncomplicated symptoms associated with lifelimiting
conditions using guidelines and standard protocols of care and in the
context of current scope of practice
• Demonstrate and ability to assess and manage common symptoms associated
with life-limiting conditions (Appendix 2)
• Be able to recognise, plan and implement the care and management of potentially
reversible causes of clinical deterioration
• Be able to recognise and assist in the provision of immediate care of emergencies
that may arise in the palliative care setting (e.g. spinal cord compression,
hypercalcaemia, major haemorrhage), and know when to escalate
• Be able to anticipate (where possible) and recognise a need for change in the
focus of care and treatment goals at critical decision points in the course of a lifelimiting
condition
• Be able to help the person with a life-limiting condition and their family adapt to a
transition from life prolonging treatment to a focus on palliative care
• Be able to anticipate, recognise and respond effectively to signs and symptoms of
imminent death
• Take a lead in providing guidance and support to the individual and their family,
preparing them for what to expect during the normal dying process
• Ensure last offices are attended to in the context of the individuals beliefs, culture
and religious practice
• Understand the process for verifying and pronouncing death
• Be aware of circumstances where a coroner’s examination is required.
|
DOMAIN 4
CARE PLANNING AND COLLABORATIVE PRACTICE
Care planning in palliative care is characterised by coordinating and integrating person-centred
care in order to promote quality of life for people with life-limiting conditions and their families. It
involves assessing need, promoting and preserving choice, predicting likely problems and planning
for the future in the context of a changing and deteriorating disease trajectory. Care planning
ensures that multiple disciplines and agencies can be accessed and referred to as required in a
timely manner. People with life-limiting conditions should be helped to engage with care planning
to the extent that they are able to and wish to be involved. The concerns of families and carers
should be taken into account as part of this process.
|
|
|
Domain 4 Indicators
As a health care professional you should:
• Recognise the impact of a life-limiting condition on the person and her/his family and be able
to provide support in order to help the individual to adapt to the changes in her/his condition
• Recognise the impact of a life-limiting condition on the person and her/his family’s mental
health and coping mechanisms and be able to provide support in order to help the individual
to adapt to the bereavement and loss
• Appreciate the roles, responsibilities and professional boundaries of individual members of the
interdisciplinary team
• Understand the collaborative relationship between the person with life-limiting conditions, the
health care professional, the family and all the other agents of care involved with the person
and the family in order to develop an individualised and coherent plan of care to assist the
person and the family to attain realistic goals and outcomes in all care settings
• Collaborate effectively with others as a member or leader of multidisciplinary team
• Be able to identify priorities or concerns for the individual with a life-limiting condition and
their carers, taking account of the individual’s coping strategies and how the person perceives
their diagnosis
• In the context of professional scope of practice be able to critically evaluate outcomes of
interventions against established standards and guidelines
• Demonstrate an understanding of advance care planning and an appreciation of the appropriate
time(s) to engage in discussions about preferences for care with the person with a life-limiting
condition and her/his family
• Demonstrate an ability to communicate sensitively and clearly about advance care planning
with the person, the family and the range of professionals and agencies involved.
|
Domain 4 ALL NURSES
As a registered nurse caring for people with life-limiting conditions you should:
• Be able to facilitate and participate in key events in the care of the person with a
life-limiting condition, such as family meetings and advance care planning
• Demonstrate ability to recognise that the person with a life-limiting condition may
lose capacity to make decisions at end-of-life
• Understand that in situations where a person lacks capacity to make decisions,
the nurse acts as an advocate to ensure decisions made are in the best interests
of the person and follow the current Code of Conduct for each Nurse and Midwife
• Be able to address questions regarding issues of organ donation or post mortem
• Understand the importance of timely referral to primary care and palliative care
teams in the management of the person with palliative care needs
• Demonstrate an awareness of the need for communicating with primary care
teams and other teams that may impact on the delivery of care to people with
life-limiting conditions and their families.
|
|
|
DOMAIN 5
LOSS, GRIEF AND BEREAVEMENT
Dealing with loss, grief and bereavement for the person themselves, their family and the
professionals who care for them is intrinsic to palliative care provision. Most people manage their
loss by combining their own resources with support from family and friends. However, a minority
of people are at risk of developing complications or difficulties in their grieving. Professionals
using the palliative care approach have an important role to play in supporting bereaved people
by providing information and support to all and by identifying those who require bereavement
therapy or counselling.
|
Domain 5 Indicators
As a health care professional you should:
• Understand that grief is a normal and appropriate response to loss which has physical,
psychological, spiritual, emotional and social aspects that affect how it is experienced
• Recognise the range of individual physical, psychological, spiritual, emotional and social
responses to loss and grief
• Recognise the factors which may put a person at risk of encountering difficulties in their grief,
whilst also remaining aware of the resources and resiliencies that are particular to each person
and family
• Demonstrate an ability to engage with a person who is experiencing loss in the context of
professional scope of practice and/or role
• Assist the family to access bereavement information and support at a level that is appropriate
to their needs
• Understand the personal impact of loss, grief and bereavement and recognise your own loss
responses and engage in activities that maintain your resilience on an on-going basis
• Possess a level of self-awareness that prevents your own experiences of loss from negatively
impacting on the person with a life-limiting condition or their family.
|
|
|
Domain 5 ALL NURSES
As a registered nurse caring for people with life-limiting conditions you should:
• Demonstrate an understanding of normal and pathological responses to the
diagnosis/prognosis of a life-limiting condition and an ability to address the
immediate management of such issues or make appropriate referral.
|
DOMAIN 6
PROFESSIONAL AND ETHICAL PRACTICE IN THE CONTEXT OF PALLIATIVE CARE
The goal of health care is to help people sustain health that is essential to their well-being. However,
there comes a time when specific treatments or interventions may be futile or overly burdensome.
Integrity in palliative care practice refers to the importance of respecting the person’s values, needs
and wishes in the context of a life-limiting condition. It guides all health care professionals to reflect
on the relationship between their contribution to a person’s care and the necessary contributions
of other professionals. Professional and ethical practice is about considering how best to provide
continuing and integrated care to people as their health care needs change in the course of lifelimiting
conditions.
|
|
|
Domain 6 Indicators
As a health care professional you should:
• Work within your current Code of Professional Conduct and engage ethically, knowledgably
and respectfully with other disciplines
• Recognise and respect your professional responsibility to care for people with life-limiting
conditions and their families to ensure their comfort and dignity
• In the context of your current professional role establish collegial partnerships and in the
context of palliative care contribute to the professional development of students, peers,
colleagues and others through consultation, education, leadership, mentorship and coaching
• Use the resources available in the context of providing appropriate care to the person with a
life-limiting condition
• In the context of professional scope of practice and/or role anticipate and demonstrate the
ability to address potential ethical issues that may be encountered when caring for the person
with a life-limiting condition and her/his family such as: Do Not Attempt Resuscitation Orders,
withdrawal and withholding of treatment, use of artificial hydration and feeding, palliative
sedation and requests for euthanasia
• Be able to establish and respect people’s wishes about their care and options/ preferences.
This includes:
• Recognising peoples right to make informed decisions to refuse additional treatment(s)
• Seeking, responding to and implementing people’s preferences about where they are
cared for (e.g. in their own homes) if this is practicable
• Respecting advance care plans made by people where the decision is an informed choice
and relates to the situation that has arisen (Medical Council, 2009)
• Demonstrate a commitment to engage in anti-discriminatory practice in relation to end of
life care and service delivery
|
Domain 6 ALL NURSES
As a registered nurse caring for people with life-limiting conditions you should:
• Be aware of and act according to the current code of professional conduct for
Nurses and Midwives, as it applies to the care of people with life-limiting conditions
• Demonstrate an understanding of the difference between managing a life-limiting
condition and providing end-of-life care.
(HSE 2014)
|
![]()
![]()
![]()