![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
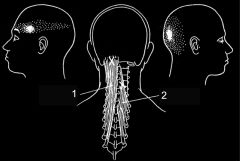
1. is?
2. is? |
1. Trigger point distribution for semispinalis capitis.
2. Trigger point distribution for semispinlalis cervicis. |
|
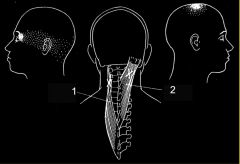
1. is?
2. is? |
1. Trigger point distribution for Splenius cervicis.
2. Trigger point distribution for Splenius capitis |
|

Pictured?
|
Trigger point distribution/referral pattern for Trapezius
|
|
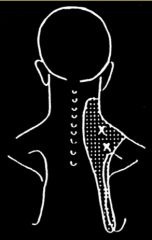
Pictured?
|
Trigger point referral pattern for Levator scapulae.
|
|

What is pictured? When would this occur?
|
Neurogenic Inflammation:
Activated microglia release several pro-inflammatory cytokines, chemokines, and other agents that modulate pain processing by affecting either presynaptic release of neurotransmitters and/or post-synaptic excitability Would occur post peripheral nerve injury. |
|
|
Examples of this type of pain are ACNES, meralgia, paresthetica, compressions (EtOH, cancer)
|
Peripheral neuropathic pain
|
|
|
Activated microglia release several pro-inflammatory cytokines, chemokines, and other agents that modulate pain processing by affecting either presynaptic release of neurotransmitters and/or post-synaptic excitability
|
Neurogenic inflammation (post-peripheral nerve injury)
|
|
|
What are the mechanisms of neuropathic pain?
|
• Spontaneous discharges or disregulated discharges
• Abnormal expression of ion channels • Localized demyelination • Disregulated cell bodies in DRG ***Each mechanism provides a different Tx approach*** |
|
|
This is an example of what type of pain:
Right shoulder pain post larparoscopic surgery (due to a sub-phrenic gas bubble) |
• Somatic-somatic
Diaphragm is a muscle - not hollow ∴ a somatic structure |
|
|
Visceral afferent nociceptors and afferent pain-projection neurons from a somatic structure synapse on the same neuron in the DRG. The brain projects the visceral sensation onto the somatic structure. This is the definition of?
|
Convergence-Projection Hypothesis.
|
|
|
What is the convergence-projection hypothesis?
|
• Visceral afferent nociceptors converge on the same pain projection neurons as the afferents from the somatic structures in which the pain is perceived. The brain projects the sensation on to the somatic structure.
• AKA referred pain |
|
|
Brain Freeze (cold stimulus on the vagus giving a headache) is an example of?
|
Referred pain (Convergence-Projection Hypothesis in action)
|
|
|
The thoracic parietal pleura, periphery of the diaphragmatic pleura, & upper 85% of the abdominal wall are all supplied by ____? Which means?
|
• All supplied by T6 & T7.
• This means that pain from any of these structures can feel the same. |
|
|
I'm used to the pain
|
Habituation
|
|
|
I have a lower pain threshold than before the accident
|
Sensitization
|
|
|
Intense, repeated, or prolonged stimuli applied to damaged or inflamed tissues reuslts in a ↓ of the threshold for activating 1º afferent nociceptors, and an ↑ in the frequency of firing for all stimuls intensities.
|
Neurogenic inflammation (Sensitization in the periphery)
|
|
|
_____ likely has a role in the pathogenesis of asthma, fibromyalgia, eczema, migraines, rosacea, dystonia, & psoriasis.
|
Neurogenic inflammation
|
|
|
Inflammatory mediators such as bradykinin, nerve growth factor, some prostaglandins, and leukotrienes contribute to this process ______. Silent nociceptors may also be involved.
|
Neurogenic inflammation
|
|
|
1. Pressure causes cell damage, ↓ pH, release of K+, syntehsis of prostaglandins & bradykinin, ↑ sensitivity to BK & other pain substances.
2. The Peripheral afferent nociceptor signals the spinal cord, but also induces the release of peptices that cause vasodilation and neurogenic edema (bogginess), w/ release of histamine from mast cells and serotonin from platelets. |
Neurogenic inflammation
|
|
|
If a mechanical stimulation (heel jar) causes abdominal pain, what can be inferred?
|
There is sensitization (the abdominal organs are sitting in an inflammatory soup caused by neurogenic inflammation)
|
|
|
What can be used to tx neurogenic inflammation?
|
• OMM - mobilizes extracellular fluid
• Botox |
|
|
An intiial noxious event causes centra hyperexcitation w/in the dorsal horn cells, w/ upregualtion of the pain response from further noxious stim.
|
Central Sensitization
|
|
|
1. Expansion of the receptive fields
2. Short term "wind-up" 3. Long term "amplification |
Central Sensitization
|
|
|
A, B, and C fibers have their cell bodies in the DRG. They sometimes respond to stim from receptor fields that are much wider than a single dermatome (so exam findings may deviate from expected dermatomal outlines). This is an example of?
|
• Expanding receptive fields (part of Central Sensitization)
|
|
|
What two neurotransmitters are used by inhibitory neurons?
What two NT are used by excitatory neurons? |
• GABA or glycine
• Glutamate and aspartate |
|
|
How is GABA synthesized?
|
GABA is synthesized from glutamate by glutamate decarboxylase which uses pyridoxal phosphate (B6)
|
|
|
Mediated by NT in and neurotrophic factors such as: glutamate, sub. P, neurokinins, calcitonin gene-related peptige G-protein coupled receptors, ligand gated ion channels, Trk receptors, NO, and prostanoids
• Glutamate excites wide-dynamic range neurons. The more they fire, the lower the threshold of the C fibers --> less input generates more pain ª Opioid and glutamate-R antatgonists (tramadol, methadone, dextromethorphan), can help prevent this effect. |
Wind-up (part of Central Sensitization)
|
|
|
What drugs are useful for preventing wind-up? Why?
|
• Tramadol, methadone, dextromethorphan
• They are opioids and glutamate-R antagonists |
|
|
Regulatory interneurons wind down, w/ less inhiitory messaging.
• Vg-Ca++ channel blockers, NMDA-R antagonists, NO syntease inhibitors, and agents that increase inhibition can block this ___. • This can also be worsened by what? |
Amplification (part of Central Sensitization)
• Sympathetically maintained activity can generate loss of inhibitor effect of GABA |
|
|
What drugs are effective against amplification? Why?
|
• Gabapentin
• Pregabalin • They are Vg-C++ channel blockers |
|
|
Stimulation of large afferents activate the release of inhibitory glycine (rubbing vigorously on the area of an injury. This is ______?
|
• Gate Control theory
|
|
|
Electircal stim devices which stimulate fine-diameter interneurons are employing what method of pain modulation?
|
• Gate Control theory
|
|
|
• Inflammatory signaling molecules trigger Na+ channel phosphorylation
• Gene transcription altered at the DRG and dorsal horn neurons • Lower activation threshold and larger current when activated |
Peripheral sensitization (a Neuropathic pain mechanism)
|
|
|
• Peripheral nociceptor inpts trigger molecular ∆s in central neruons
• Less GABA and glycine inhibition • More MNDA and AMPA activation • Death of inhibitor interneurons |
Central senstization (a Neuropathic pain mechanism)
|
|
|
• Constant activation of the polymodal (wide dynamic range) fibers w/ ongoing release of neuropeptides (sub. P, calcitonin-gene-related peptide) causing ongoing neurogenic inflammation in the periphery, central wind up
• What drugs help here? |
• Persistent inflammatory pain model
• NSAIDs are effective here |
|
|
• Collateral sprouting after peripheral nerve injury and axonal degeneration w/ ectopic discharges
• What drugs help here? |
• Persistent neuropathic pain model
• Local anesthetics effective here |
|
|
• Loss of inhibtory fxn of GABAergic dorsal cells leads to excessive glutamate/aspartate
• What drugs help here? |
• Persistent neuropathic pain model
• Anti-epileptic drugs help here. |
|
|
Spontaneous pain & sympathetic dysfxn following injury
|
Complex Regional Pain syndrome
|
|
|
Spontaneous pain & sympathetic dysfxn following injury + identifiable nerve injury
|
Complex Regional Pain syndrome I (or Post-traumatic neuralgia)
|
|
|
Spontaneous pain & sympathetic dysfxn following injury + NO identifiable nerve injury
|
Complex Regional Pain syndrome II (Reflex sympathetic dystrophy)
|
|
|
What potentially catastrophic ddxs should come to mind w/r/t pain?
|
• Cancer
• Infection • Fractue • Ongoing tissue damage (nerve compression) |
|
|
Lumbalgia + Hx of longstanding steroid use = possible ____
|
Osteoporotic fracture
|
|
|
Lumbalgia + unexplained fracture = ______
|
Malignant involvement of the bone
|
|
|
Pelvic pain + increasing abdominal girth = possible ____
|
Ovarian cancer
|
|
|
What are some red flags w/r/t pain?
|
• Children, age > 5.
• Fevers, chills, night sweats, penetrating wound • Unrelenting night pain or pain at rest • Progressive motor/sensory deficit • Unexplained distribution * Unexplained weight loss • Hx of cancer • Hx of steroid use, immunosuppression, IV drug use • Failure to improve after 6 wks conservative Tx. |
|
|
Depression occurs in up to ___ of chronic pain pts. Anxiety in ____ of chronic pain patients. What other psych things may be seen?
|
• 80%
• 30% • Substance abuse and PTSD often seen. |
|
|
What are Waddell's signs?
|
• Help to determine if a patient is faking their pain.
|
|
|
A stellate ganglion block often terminates this kind of pain
|
Sympathetically mediated pain
|
|
|
Peripheral nerve damage without autonomic change (post-herpetic neuralgia, neuroma formation) is referred to as ___ type of pain.
|
Non-sympathetically mediated.
|
|
|
• disturbance of function or pathologic changes in a nerve. vs.
• disturbance of function or pathologic changes in one or more nerve roots. |
• Neuropathy vs. Radiculopathy
|
|
|
Term for undertreating pain.
|
Oligoanalgesia
|
|
|
Polymyositis, dermatomyositis, polymyalgia rhematica, spacticity, & thalamic pain are all examples of _____
Leavator ani syndrome, Proctalgia guhax, DeQuervain, Meralgia paresthetica, & Burning mouth syndrome are all examples of _________ |
Generalized Chronic Pain syndromes
(also includes Fibromyalgia & Sickle Cell) Localized Chronic Pain syndromes |
|
|
• Mild pain: non-opiod +/- adjuvant
• Moderate pain: opioid and non opioid +/- adjuvant • Severe pain: opioid +/- adjuvant, and non-opioid The above describes |
Analgesic stepladder
|
|
|
Lidoderm/EMLA and Capsaicin are examples of?
|
Topical analgesics
|
|
|
Examples of these type of pain-management drugs are: sodium channel blockers (Anticonvulsants and antiarrhythmics), mood stabilizers, antidepressants, muscle relaxers, marijuana, antihistamines
|
Co-analgesics
|
|
|
What co-analgesic is especially useful for neuropathic pain?
|
Anti-convulsants
|
|
|
Carbamazepine, gabapenting, pregabalin, phenytoin & vaproic acid are often used as co-analgesics for what type of pain?
|
Neuropathic pain
|
|
|
How are TCAs useful as co-analgesics? SNRIs?
|
• TCAs inhibit Na+ channels and block NMDA receptors
• SNRIs inhibit the reuptaek of biogenic amines (NEP, 5-HT) ↑ [ ] & duration of action at the synapse |
|
|
What co-analgesics are useful for chronic pain and MS?
|
Antispastics (skeletal muscle relaxants) Baclofen & dantrolene
|
|
|
What co-analgesics are usefulf for musculoskeletal conditions?
|
Atispasmodics (skeletal muscle relaxants) Carisoprodol, cyclobenzaprine, metaxalone, methocarbamol.
|
|
|
Prazoin, terazosin, phenoxyenzamine (are ___?) and clonidine ( ___?) are used for what?
|
• Prazosin, terazosin, phenoxybenzamine are all alpha-1 antagonists
• Clonidine (alpha-2 agonists) • All used as sympathetic nervous system blockers |
|
|
Helpful for opioid-induced nausea, and especially useful because it potentiates the analgesic effects, possibly by blocking histamine mediated activation of C fibers.
|
Hydroxyzine
|
|
|
What drug inhibits release of NEP from the postganglionic adrenergic neurons, producing a chemical sympathectomy?
|
Lidocaine
|
|
|
Babes exposed to opioids close to delivery may have ____
|
Respiratory depression
|
|
|
Babes exposed to COT during pregnancy may ___
|
WILL go through excrutiating w/drawal
|
|
|
Babes exposed to NSAIDS late in pregnancy may have ____
|
Constriction of the ductus arteriosus
|
|
|
What are some key side-effects of NSAIDs?
|
• GI upset, gastritis, upper GI bleed
• Elevated BP • Derm RXNs • Exacerbation of bronchospasms • Nephrotoxicity |
|
|
What are some of the risk factors to consider when prescribing opiods?
|
• Age < 45, ♀, family Hx of abuse, smoker
• Psych: substance abuse, Hx of sexual abuse, major psych ddx • Social: legal probs, MVAs, poor support |
|
|
What should be included in the medication contract/policy agreement?
|
• Definiition of Tx goals • Informed consent • Clinic policies and procedures • Exit strategy |
|
|
What are the four A's? What are they used for?
|
• Analgesia
• Adverse effects • Activities of daily living • Aberrant behaviors Used during Chronic Opioid Therapy |
|
|
Primary chronic neurobiological disease with genetic, psychosocial, and environmental factors influencing its manifestation.
|
• Addiction
• Continued use despite harm |
|
|
What can help allay the nausea and vomiting sometimes caused by opioids?
|
• Antidopaminergic, antiserotonergics, anticholinergics
|
|
|
What opiod can cause a prolonged QT?
|
Methdone
|
|
|
Classic neuropathic pain (intense burning pain, hyperalgesia, allodynia)
• Autonomic features (altered sweating, skin color, skin temp) • Trophic changes to skin, hair, nails • Altered motor function (loss of strength, decreased ROM, tremor |
Chronic Regional Pain Syndrome (CRPS)
|
|
|
How will the skin around an area of CRPS appear?
|
• ↑ sweating, heat, hair growth
|

