![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
35 Cards in this Set
- Front
- Back
|
disease considerations
|
Common complaint:
Es6mated that 80% of people will experience at some stage Embarrassing problem for pa6ents Need to treat requests for advice sympathe6cally and privately Pa6ents will oHen use the term haemorrhoids to describe any anorectal complaint: e.g. anal fissure, polyps, anal warts, threadworm, gastric carcinoma, IBD |
|
|
Prevalence and Epidemiology
|
Can occur at any age but are rare in children and adults younger than 20
years Prevalence increases with age: Most common in pa6ents aged between 40 and 65 years Higher incidence in pregnant women |
|
|
physiology
|
Haemorrhoids are a normal part of the human anorectum
Arise from subepithelial connec6ve 6ssue cushions, which contain a rich network of blood vessels, within the anal area Normal haemorrhoidal 6ssue provides 15‐20% of res6ng anal pressure Provides important sensory informa6on to differen6ate between solid, liquid and gas Important for maintaining con6nence (coughing or straining) The vascular cushions increase in area and volume enabling the anal canal to remain closed and avoid the loss of stools |
|
|
aetiology
|
The degenera6ve effects of ageing may weaken or fragment the
suppor6ng 6ssues, and this along with the repeated passage of hard stool and straining produces a shearing force on the cushions, leading to their descent and prolapse The prolapsed cushions have impaired venous return, which results in engorgement that may be further exacerbated by straining, inadequate fibre intake, prolonged 6me on the lavatory, and condi6ons such as pregnancy that raise intra‐abdominal pressure Bleeding from the engorged prolapsed haemorrhoid occurs as a result of localised mucosal trauma or inflammation, which damages the underlying blood vessels |
|
|
pathophysiology
|
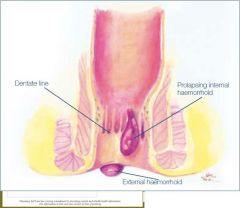
Haemorrhoids generally cause symptoms when they become enlarged,
inflamed, thrombosed or prolapsed May be internal or external: The transi6on between the upper and lower anal canal is called the dentate line Internal haemorrhoids develop above the dentate line Simple columnar epithelium, lacks sensory innerva6on External haemorrhoids develop below the dentate line Squamous epithelium, innervated |
|
|
internal and external heamorrhoid
|
|
|
|
stages of haemorroid
|

|
|
|
Pathophysiology - forming of hemorroid, strangulated?, role of connective tissue
|
Increased pressure, e.g. caused by prolonged straining with defeca6on,
interferes with venous return and causes engorgement of the haemorrhoids Easily trauma6sed, leading to rectal bleeding If the suppor6ng connec6ve 6ssue becomes weakened (age or persistent straining) the haemorrhoids are displaced down the anal canal and may eventually prolapse May become strangulated if prolapse below the anal sphincter |
|
|
Clinical Features
|
Bleeding, pain, perianal itching can all occur
OHen asymptoma6c un6l prolapse occurs AHer defeca6on, the haemorrhoids might return to their normal posi6on spontaneously or be reduced manually Associated bleeding results in bright red blood and most commonly seen as spoZng in the toilet or no6ced on toilet paper Internal haemorrhoids are painless, and bleeding alone may be the only symptom Severe pain is experienced when the pa6ent has external haemorrhoids that have become thrombosed OHen described as a dull ache, increasing in severity when the pa6ent defecates Pa6ents may then ignore the urge to defecate, leading to constipation |
|
|
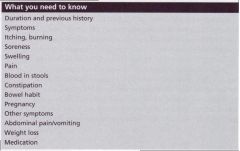
what needed to be known - history taking
|
|
|
|
Differential Diagnosis
|
Derma66s:
If pruri6s is the main complaint and the pa6ent does not complain of bleeding or prolapse, derma66s is a likely cause Condi6ons causing rectal bleeding: A number of condi6ons may present with rectal bleeding The presence of other symptoms may allow them to be excluded |
|
|
Differential Diagnosis
Conditions causing rectal bleeding |
Anal fissure:
Common and normally caused by straining Intense pain on defeca6on, bright red blood Referral (non‐urgent) may be required for diagnosis IBD (Crohn’s disease & ulcera6ve coli6s) Other symptoms normally present Diarrhoea with associated abdominal pain Pa6ents will generally appear unwell Upper GI Bleed: Erosion of the stomach wall or upper intes6ne OHen associated with NSAIDs, SSRIs, alcohol intake, an6thrombo6cs, prednisolone Tarry or black stools depending on the amount of blood loss Urgent referral Colorectal cancer: Generally affects pa6ents > 40 years of age Persistent change of bowel habit Rectal bleeding may be insidious Anaemia |
|
|
History Taking
|
Cons6pa6on:
Common causing or exacerba6ng factor Inadequate dietary fibre or fluid intake may be involved Medica6ons may also contribute Pregnancy: Higher incidence of haemorrhoids Increased pressure on the haemorrhoidal issue Prevention |
|
|
questions to ask and why
|

|
|
|
treametn related questions
|

|
|
|
medications that can diarrheoa or constipation
|

|
|
|
Treatment Related Questions-other medications, seen a doctor, recent childbirth
|
Other medica9ons?
An6platelets, an6coagulants may exacerbate bleeding ‐ referral may be appropriate Recent childbirth? May need to check wound healing ‐ suppositories may be more appropriate un6l would healing has occurred Seen a doctor before about these symptoms? A recent examina6on by a doctor may be required to exclude serious pathology before treatment can be recommended by the pharmacist |
|
|
Treatment Related Ques9ons
Constipation or altered bowel habit? |
Cons6pa6on is a common cause or contribu6ng factor in haemorrhoids
Insufficient fibre, lack of exercise or inadequate fluid intake may be involved Haemorrhoids associated with persistent changes in bowel habit may require inves6ga6on (leakage of faecal material through the anal sphincter may produce symptoms of itching and irrita6on and may be caused by the presence of a tumour Anal fissure or fistula can also lead to seepage |
|
|
Treatment Related Questions
Any unusual bleeding or pain? |
Blood may be evident in the toilet bowl, deposited onto the surface of the
stool or be seen on the toilet paper‐it will generally be bright red if it is due to haemorrhoids If it is mixed in with the stool it has come from higher up in the GIT and will be darker in colour Bleeding is an indica6on for referral to exclude more serious pathology such as polyps or a tumour‐bowel cancer may also cause bleeding Haemorrhoids are not always painful Sharp pain on defeca6on may indicate an anal fissure which may require referral Associated abdominal pain (not due to cons6pa6on), distention or vomi6ng requires referral |
|
|
Treatment Related Ques9ons
Recurring problem? |
If treatment does not sedle symptoms within one week, referral is required
Frequent relapses are also an indica6on for medical interven6on (e.g. injec6on or surgery for removal of haemorrhoid may be required) Persistent symptoms of haemorrhoids (e.g. itching and irrita6on) may be associated with rectal cancer and referral may be required |
|
|
flowchart of management
|

|
|
|
triggers for referral
|

|
|
|
treatment flow chart
|
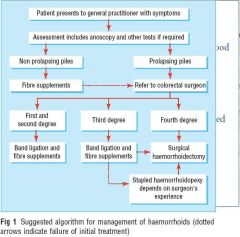
|
|
|
Management
Suppositories: |
zinc oxide 300 mg, balsam‐peru 50 mg, benzyl benzoate 33 mg, Anusol (NS, B2)
cinchocaine HCl 5 mg, hydrocor6sone 5 mg, Proctosedyl (S2, A) adrenaline 0.27 mg, benzocaine 150 mg, zinc oxide 250 mg, Rectinol (S2) |
|
|
management
Ointments: |
zinc oxide 10.75%, balsam‐peru 1.88%, benzyl benzoate 1.25%, Anusol (NS, B2)
lignocaine 1.5%, allantoin 0.9%, hamamelis liquid extract 0.5%, zinc oxide 7.5%, Hemocane (S2) cinchocaine HCl 0.5%, hydrocor6sone 0.5%, Proctosedyl (S2, A) cinchocaine HCl 0.5%, hydrocor6sone 0.5%, Rectinol HC (S2, A) adrenaline 0.01%, benzocaine 5%, zinc oxide 2%, Rectinol (S2) lignocaine base 5%, hydrocor6sone acetate 0.25%, aluminium acetate 3.5%, zinc oxide 18%, Xyloproct (S2, A) |
|
|
Management
Anaesthe9cs:- astringents |
Anaesthe9cs:
Lack of evidence for haemorrhoids, although effec6ve on other mucosal surfaces Short dura6on of ac6on, temporary relief of itching and pain Frequency of applica6on may cause sensi6sa6on; maximum of 2 weeks Astringents: Theore6cally useful as they provide a protec6ve coa6ng over haemorrhoids No evidence to support this theory, probably only provide a placebo effect |
|
|
Management
Hydrocortisone: protecterants |
Hydrocor9sone:
Effec6veness in reducing inflamma6on ‐ therefore useful in reducing haemorrhoidal swelling Protectorants: Claimed to provide protec6ve effects, providing relief from itching and pain Probably placebo effect |
|
|
Management
Other agents: |
An6sep6cs (e.g. chlorhexidine)
Vasocontrictors (adrenaline) Wound‐healing agents (yeast cell extract) Venotonics (e.g. flavonoids) have been used as dietary supplements; may improve venous tone, reduce hyperpermeability and have an6‐inflammatory effects Examples include horse chestnut (aesculus hippocastanum) and bilberry Hydroxyethylrutosides (Paroven, US) is used for varicose veins Lack of evidence suppor6ng use; may be beneficial |
|
|
Management Issues
Many proprietary prepara6ons also contain local anaesthe6c or a corticosteroid: |
Prolonged use should be avoided in favour of trea6ng the underlying
condi6on, as there may be adverse effects Short‐term use of cor6costeroids may provide symptoma6c relief but can also exacerbate candidiasis and other local infec6ons There is addi6onal risk that these prepara6ons may cause local skin sensi6sa6on or derma66s (derma66s medicamentosa) Steroids in par6cular can cause permanent damage or ulceration of the perianal skin |
|
|
Management Issues
Pregnancy and breastfeeding: |
Hydrocor6sone/LA combined products are ADEC Category A
Small amounts are secreted in breast milk Unlikely to be an issue |
|
|
Fibre
|
Soluble fibre (par6ally broken down) is found in oats, legumes, fruit and
vegetables, cereals and soy products Slows sugar absorp6on and may help to reduce cholesterol absorp6on Insoluble fibre (acts like a sponge) is found in wheat bran, wholegrain foods, skins of fruit and vegetables and in some legumes Bulk forming Need to ensure adequate fluid intake |
|
|
tips for non specialist
|

treatment is with rubber band ligation
|
|
|
Anal Fissure
Management |
Management of acute anal fissure is conserva6ve ‐ avoid hard stool, either
through use of stool soHeners or bulking agents, and use glyceryl trinitrate if needed Glyceryl trinitrate 0.2% ointment (Rectogesic, S3) 1 to 1.5 cm topically around the anus, 3 6mes daily, for up to 8‐weeks Topical glyceryl trinitrate should not be used if within the preceding 24 hours, the patient has taken one of the phosphodiesterase inhibitors (e.g. sildenafil) for erectile dysfunc6on |
|
|
anal fissure - management issues
|
Because of systemic absorp6on, glyceryl trinitrate ointment may cause
headache in some pa6ents If the above measures fail to achieve healing of the fissure, specialist referral is required ADEC Category B2, should be safe in breasmeeding |
|
|
Practical Points
|
Good hygiene:
Keep the area clean and dry Avoid soap products Use cleaning wipes instead of toilet paper Avoid nylon underwear A soak in a warm bath may relieve symptoms Barrier cream aHer a bowel movement |

