![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
Definition of a wound
|
any anatomical or functional interruption in the continuity of the tissue that is accompanied with cellular damage and death
|
|
|
Etiology of Wounds
|
Traumatic Injuries
Chemical Physical Pathologic Cause disruption of tissues such as carcinomas and non healing ulcers(TB and Sarcodiosis) |
|
|
Physical Injury-*
|
Crushing-rubber dam clamp
Extreme Temperatures Irradiation-cancer patients Dessication Obstruction of arterial inflow or venous outflow-espeically in toes and fingers w/ diabetes and peripheral vascular disease Denture irritaiton |
|
|
Chemical Injury-*
|
-unphysiologic pH-very acidic or basic
-disrupt of protein integriy -ischemia -aspirin -phenol -arsenic and acids(ill-advised chemical consumption) |
|
|
Healing definition
|
-Series of coordinated processes initated by injury and directed toward restoring structural and functional integrity
|
|
|
Types of Wound Healing
|
Primary-edges are put together-for soft and hard tissue healing(suturing)
Secondary-granulation tissue forms and epithelium migrates across to close up wound ex. avulsed piece of tissue with too much tissue loss to close the wound-->formation of 2ndary healing Tertiary Healing-delayed primary closure ex. if wound is dirty, clean it out and then LATER freshen margins and close it to avoid sealing bacteria in |
|
|
Primary Intention
-tissue? -how to start it? -scarring? -how fast does it feal? -used for? |
-minimal tissue loss
-wound edges brought into contact with sutures -minimal scarring -rapid healing -well repaired incisions and well reduced bony fractures |
|
|
Secondary Intention
-wound edges? -size of defect? filled with? -scarring? -healing? -used for? |
-Wound edges widely separated from surgery or tissue loss
-defect is large and filled with blood clot(starts healing process) -scar formation, slow healing -extraction sockets, avulsive injuries, poorly reduced bony fractures - dont undermine gingiva and close via unattached mucosa |
|
|
Tertiary Intention
|
Wound left open for period of time then closed with a tissue graft
|
|
|
Healing of Extraction Socket
-type of intention -what happens inititally? for what reason? what occurs during the first week? what happens in the wound? -epithelium? -sequence of events |
-2ndary intention
-blood clot forms wihtin 24 hrs, coagulates and seals off from oral cavity 1st week: inflammatory phase + fibroplasia -WBCs debride bacteria, bone, osteoclasts along wound margin -epithelium migrates along socket wall until it reaches the other side -2nd week: granulation tissue and new trabecular bone by osteoblasts-delay in pts with osteoporosis or bone problems -4th week: epithelialization complete-may cause concerns in the anterior region -4th week: new bone formation though poorly calcified-(refracture of bone is easy so must wait 6-8 weeks before physical activity) -4-6 weeks: complete healing |
|
|
Stages of Wound Healing
|
Inflammatory Stage-blood clot, inflammatory cells
Fibroblastic Stage(granulation tissue)-fibroblast come in, growth factor release, lattice network of soft/hard tissue laid down Remodeling Stage-tissue becomes stronger or bone turns over to become lamellar rather than woven(which is initially formed during wound healing) |
|
|
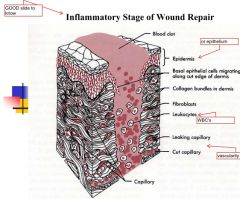
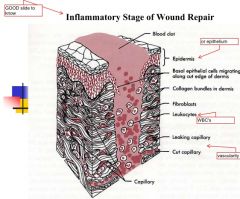
Inflammatory Stage
begins? how long? signs? wound strength? role of Fibrin? |
-when tissue injury occurs
-3-5 days -eat soft foods only and gentle brushing -erythema, edema, warmth, pain, loss of fxn -no gain in wound strength -fibrin holds wound together-gets stronger in later stages |
|
|
|
|
|
Inflammatory Stage-Vascularity
-immediate reaction? -initiates? -releases? -vasoeffects? -leukocytes -max swelling occurs? |
-vasconstriction immediate(maynot be possible with anticoagulants)
-clotting cascade from veseel disruption -Mediators: Serotonin, Histamine, Prostaglandin -Vasodilation and increased vascualr permeability -leukocytes(debride) adhere to endothelial cell wall, migrate to interstitial tissues-->edema(max swelling48-72 hrs post procedure...1 week for large surgery) |
|
|
Cardinal Signs of Inflammation
|
Warmth and erythema-->vasodilation
Swelling-->leakage of fluid Pain and loss of fxn--> release vasoactive amines and pressure from edema note: vicodin may not be as effective as antiinflammatories if inflammation is the reason for pain |
|
|
Cellular Componenet
-triggered by? componenets |
-activation of complement
-C3, C5 chemotactic factors -neutrophils-initial -macrophages-debride + growth factors for healing -lymphocytes |
|
|
Neutrophils
-how soon do they appear? -mechansim -fxn |
-first cells that appear
-6-12 hours -release lysosomal enzymes(proteases) -digest necrotic debris and bacteria |
|
|
Macrophages
-type of cells -fxn? -attracted by? -release? |
-phagocytic cells
-continue debridement -chemoattractants, fragments of collagen, TGF-B1, thrombin(lattice of fibrin to strengthen wound) -release biologically active substances like pgs, lks, gfs |
|
|
Growth Factors
-necessary for? -secreted by? -examples |
-necessary for inititiation and propagation of granulation tissue
-secreted by macrophages -PDGF, TGF-a, TGF-b, EGF, FGF |
|
|
Lymphocytes
-mostly found in? -tcell function? |
-T and B cells are found in chronic inflammation
-can cause serious dammage in PA lesion or endodontics -T-cells secrete lymphokines, chemotactic for fibroblast proliferation |
|
|
ECM
-how much? -what holds the wound together? |
-little ECM present
-only fibrin holds wound together at this stage -fibrin scaffold for fibroblasts to lay down ECM in granulation tissue phase |
|
|
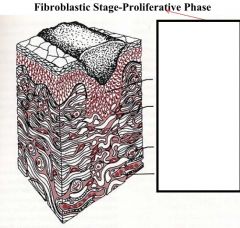
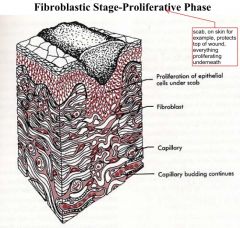
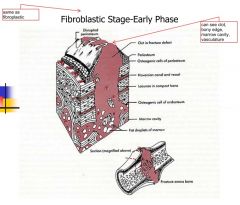
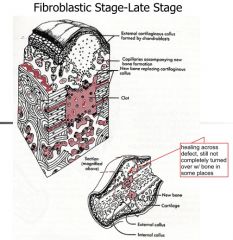
Fibroblastic Stage(Granulation Tissue)
-timing -what forms -vascularity? -type of wound healing -what do you see? |
-2-3 weeks-wound starts to strengthen
-Fibrin scaffold -Collagen deposition -revascularization -haphazard wound healing -macrophages, fibroblast ingrowth, loose connective tissue, angiogenesis |
|
|
|
|
|
|
|
|
Wound Contraction
-occurs at? -presents significant amounts of? -what happens to fibroblasts -how to reduce this? -what happens to the wound? |
-movable wound edges
-granulation tissue -fibroblast phenotypic changes during wound contraction -inhibit granulation tissue reduces contraction such as skin grafts -reepithelialization and contraction close wound |
|
|
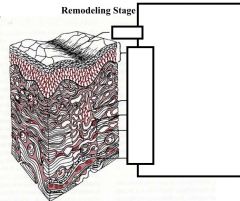
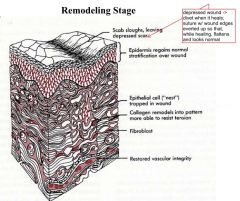
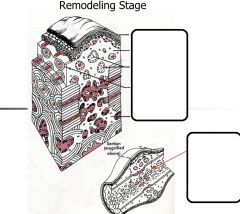
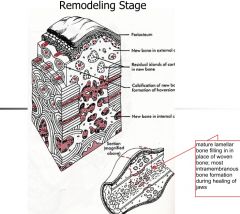
Remodeling Stage(maturation)
-timing? -begins with? -physical changes? -scar changes? |
->3 weeks
-begins with remodeling -increase in tensile strength -not really possible to tear up wound after this -reorganization of collagen-not as haphhazard -scar softens and contracts -can massage |
|
|
|
|
|
Abnormal Scar Formation
-Hypertrophic scar -scars usualy present as -HT presents as -Keloid -presents as -common in -occurs in people -how to prevent this? neither happen intraorally |
-Hypertrophic
-scar is usually flat w/ less pigment than tissues surrounding area -raised and pink-ish Keloid -extra piece of tissue that proliferates and grows out -common in asian/african americans -often shows up in the past-some people more prone -try intraoral approach to prevent this |
|
|
Surgeon's goal
|
to produce a scar that minimizes loss of fxn and looks as inconspicous as possible
|
|
|
Factors that impair wound healing
|
-foreign material
-necrotic tissue -ischemia -tension-causes tissues to become ischemic(decreased vascularity and thus healing) |
|
|
Bone Healing and Repair types
|
Direct
Indirect |
|
|
Direct Bone Healing
-contact? -distance? -kind of healing -relies on what type of fixation -type of bone deposition -extent of callus? -what is found in the area? |
-edge to edge contact
-< 1mm -cellular healing -rigid bone fixation -Direct lamellar bone deposition -minimal callus formation -osteoblasts, haversion canal, osteoclasts |
|
|
Indirect Bone Healing:
-type of callus -pathway -what forms? -effect mobility has on healing |
-collagenous bridging(callus)
- hematoma-->inflammatory phase-->granulation tissue--?fibrous tissue--?fibrocartilage callus-->cartilage-->osteoid tissue - woven bone forms by endochondral ossifcation - poor bone formation-->mal-union of bone-->negatively affects occlusion in jaws |
|
|
Adequate Bone Healing needs?
|
-vascular supply-nourishment and oxygen supply
-immoblization-slight tension to sitmulate continued osteoblastic proliferation and ossification |
|
|
|
|
|
|
|
|
|
|
|
Complications of Bone healing
|
-nonunion(not immobilized, not enough vascularity, segment too long)
-failure of fracture to heal -infection -osteomyelitis(hard to tx b/c hard for antibiotics to penetrate into bone) |
|
|
Implant Osseointegration
-effect on epithelium -what must happen on implant surface? how long does it take for full integration? |
-bone-implant interface inhibits lateral growth of epithelium without contact inhibition
- bone healing onto implant surface must occur before soft tissue forms -want bone surrounding entire implant -6 months needed for full integration -but now can put crown immediatley on and load it |
|
|
implant OI
-distance between bone and implant -need what kind of bone near the implant -why do you need a nightguard/splint -surface needs to be free of? |
-short distance b/w bone and implant
-viable bone at or near surface of bone along the implant -can do bone graft or put implant deeper -no movemment of implant while bone is attaching to its surface -implant surface free of contamination by organic/inorganic materials |
|
|
IO be careful of
|
excessive loading
|
|
|
Factors Affecting Healing
|
IF DINAR
- Infection -Foreign Material -Diabetes -Ischemia(hypoxia) -Nutrition(protein and vitamin deficiency) -Age -Radiation |
|
|
Bacterial Infection
-role in healing? -what does it do? -sxs? -releases? |
-major cause of impaired healing
-colonization with inflammation leads to further tissue damage -redness, heat, edema, pain, leukocytosis, fever -release of proteases and oxygen free radicals, cell lysis, destruction ECM, impaired healing |
|
|
Ischemia(hypoxia)
-how does it impair healing? -what leads to ischemia -causes? |
-decreased O2 impairs healing
-constricting sutures, tissue edema, necrotic tissue -anemia(not as much blood to tissues), malnutrition, sepsis lowers tissue oxygen -cell death-->release proteases and glycosidases -tissue breakdown and impaired healing |
|
|
Radiation
-dependent on? -type of effects? -how is it damaging? |
-dose depdendent
-acute and chronic effects -Acute-->mucositis, erythema, desquamation -Chronic-->irreversible, in vessel walls, skin connective tissues and mucosa -osteoradionecrosis of bone radiation effects do not get better with time but get worst due to lessening of blood supply |
|
|
Age
|
-more susceptible to wound healing problems
-decline in general health |
|
|
Therapeutic Agents
detrimental? what stimulates healing? what do chemotherapeutics do? can possbily arrest? |
- detrimental effects on health
-steroids, anticoags, antineoplastics -growth hormone, Vitamin A and C stimulate healing -chemotherapeutics inhbit wound repair -decrease tensile strength Arrest inflammatory phase -suppress protein synthesis and cell proliferation |
|
|
malnutrition
-role in wound healing -good nutrtion does what? |
-greatest contributor to poor wound healing, esepcially in elderly
-enhance immune response -stimulate hormone secretion |

