![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
99 Cards in this Set
- Front
- Back
|
Problems associated with of body systems (including physiological and psychological functions |
Impairments in body function |
|
|
Problems with anatomical features of the body, such as significant deviation or loss, affecting all body systems |
Impairments in body structure |
|
|
Difficulties an individual may have in executing actios, task, activities |
Activity limitations |
|
|
Problems an individual may experience in involvement in life situations, including difficulties participating in self care, responsibilities in the home, workplace, or the community and recreatonal, leisure, and social activities |
Participation restrictions |
|
|
The entire background of an individual's life and living situation |
Contextual Factors |
|
|
Contextual Factors are composed of |
Environmental Factors Personal Factors |
|
|
Factors associated with the physical, social, and attitudinal environment in which people conduct their lives; factors may facilitate functioning or hinder functioning and contribute to disability |
Environmental Factors |
|
|
Features of the individual that are not part of the health condition or health state; includes age, gender, race, lifestyle habits, coping skills, character, affect, cultural, and social background, education, etc. |
Personal Factors |
|
|
Overstretching, overexertion, or overuse of soft tissue: tends to be less severe than a sprain, occurs from slight trauma or unaccustomed repeated trauma of a minor degree |
Strain |
|
|
This term is frequently used to refer specifically to some degree of disruption of the musculotendinous unit |
Strain |
|
|
Severe stress, stretch, or tear of soft tissues such as joint capsule, ligament, tendon, or muscle |
Sprain |
|
|
This term is frequently used to refer specifically to injury of a ligament and is graded as a first (mild), second (moderate), or third (severe) degree sprain |
Sprain |
|
|
Displacement of a part, usually the bony partners in a joint, resulting in loss of the anatomical relationship and leading to soft tissue damage, inflammation, pain, and muscle spasm |
Dislocation |
|
|
An incomplete or partial dislocation of the bony partners in a joint that often involves secondary trauma to surrounding soft tissue |
Subluxation |
|
|
If a rupture or tear is partial, pain is experienced in the region of the breach when the muscle is stretched or when it contracts against resistance |
Muscle/Tendon Rupture or Tear |
|
|
T/F If the rupture or tear is complete, pain is still present because the muscle pulls against the injury d/t stretching or contraction of the muscle |
F - the muscle does not pull against the injury anymore |
|
|
The general term that refers to tendon injury affected by mechanical loading |
Tendinopathy |
|
|
Inflammation of the synovial membrane covering a tendon |
Tenosynovitis |
|
|
Inflammation of a tendon |
Tendinitis |
|
|
Present when there is tendinitis |
Scarring or calcium |
|
|
Inflammation with thickening of a tendon sheath |
Tenovaginitis |
|
|
Degeneration of the tendon due to repetitive microtrauma |
Tendinosis |
|
|
Inflammation of a synovial membrane; an excess of normal synovial fluid in a joint or tendon sheath caused by trauma or disease |
Synovitis |
|
|
Bleeding into a joint, usually due to severe trauma |
Hemarthrosis |
|
|
Ballooning of the wall of a joint capsule or tendon sheath |
Ganglion |
|
|
May rise after trauma, and they somtimes occur with rheumatoid arthritis |
Ganglia |
|
|
Inflammation of a bursa |
Bursitis |
|
|
Bruising from a direct blow, resulting in capillary rupture, bleeding, edema, and an inflammatory response |
Contusion |
|
|
Repeated, submaximal overload and/or frictional wear to a muscle or tendon resulting in inflammation and pain |
Overuse syndromes, cumulative trauma, disorders, and repetitive strain injury |
|
|
Loss of normal function of a tissue or region |
Dysfunction |
|
|
May be caused by adaptive shortening of the soft tissues, adhesions, muscle weakness, or any condition resulting in loss of normal mobility |
Dysfunction |
|
|
Mechanical loss of normal joint play in synovial joint; commonly causes loss of function and pain |
Joint Dysfunction |
|
|
Precipitating factors of joint dysfunction may be what? |
Trauma Immobilization Disuse Aging Pathological conditions like rheumatoid arthritis |
|
|
Adaptove shortening of skin, fascia, muscle, or a joint capsule that prevents normal mobility or flexibility of that structure |
Contracture |
|
|
Abnormal adherence of collagen fibers to surrounding structures during immobilization after trauma, or as a complication of surgery, which restricts normal elasticity and gliding of the structures involved |
Adhesion |
|
|
Prolonged contraction of a muscle in response to a painful stimulus |
Reflex muscle guarding |
|
|
The primary pain causing lesion may located where? |
Nearby or underlying tissue, or a referred pain source |
|
|
T/F when the contracting muscle does not functionally splints the injured tissue against movement when the pain is not referred |
F - It does functionally splints |
|
|
Guarding ceases when the painful stimulus is what? |
Relieved |
|
|
Prolonged contraction of a muscle in response to the local circulatory and metabolic changes that occur when a muscle is in continued state of contraction |
Intrinsic Muscle Spasm |
|
|
May also be a response of muscle to viral infection, cold, prolonged periods of immobilization, emotional tension, or direct trauma to muscle |
Spasm |
|
|
Severity of tissue injury |
Grade 1 (First-degree) Grade 2 (Second-degree) Grade 3 (Third-Degree) |
|
|
Mild pain at the time of injury or within the first 24 hours |
Grade 1(First-Degree) |
|
|
Mild swelling, local tenderness, and pain occur when the tissue is stressed |
Grade 1(First-Degree) |
|
|
Moderate pain that requires stopping the activity. Stress and palpation of the tissue greatly increase the pain |
Grade 2 (Second-Degree) |
|
|
Near-complete or complete tear or avulsion of the tissue (tendon or ligament) with severe pain |
Grade 3 (Third-Degree) |
|
|
Stress to the tissue is usually painless; palpation may reveal the defect |
Grade 3 (Third-Degree) |
|
|
___ ligament results in instability of the joint |
Torn ligament |
|
|
During this stage, signs of inflammation are present |
Acute Stage |
|
|
Signs of inflammation |
Swelling Redness Heat Pain at rest Loss of function |
|
|
During this stage, ROM is painful, patient usually guards against the motion before completion of the range is possible |
Acute stage |
|
|
This stage usually lasts 4 - 6 days unless the insult is perpetuated |
Acute stage |
|
|
During this stage, the signs of inflammation progressively decrease and eventually are absent |
Subacute Stage |
|
|
During this stage, when testing ROM, patient may experience pain synchronous with encountering tissue resistance at the end of the available ROM |
Subacute Stage |
|
|
This stage usually lasts 10 - 17 days (14 to 21 days after the onset of injury) but may last up to 6 weeks in some tissues with limited circulation, such as tendons |
Subacute stage |
|
|
There are no signs of inflammation during this stage |
Chronic Stage |
|
|
During this stage, there may be contractures or adhesions limit range, and there may be muscle weakness that limit normal funtion |
Chronic Stage |
|
|
In this stage, connective tissue continues to strengthen and remodel in response to the stressed applied to it |
chronic stage |
|
|
This pain may be felt when testing tight structures at the end of their available range |
Stretch Pain |
|
|
During this stage, function may be limited by muscle weakness, poor endurance, or poor neuromuscular control. |
Chronic Stage |
|
|
This stage may last 6 months to 1 year depending on the tissue involved and amount of tissue damage |
Chronic stage |
|
|
also known as the inflammatory reaction stage |
Acute stage |
|
|
also known as the proliferation, repair, and healing stage |
subacute stage |
|
|
also known as the maturation and remodeling stage |
chronic stage |
|
|
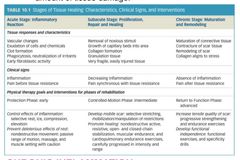
stages of tissue healing |
|
|
A state of prolonged inflmmation may occur if injured tissue is continually stressed beyong its ability to repair. There are symptoms of increased pain, swelling, and muscle guarding that last more than several hours after activity |
Chronic Inflammation |
|
|
A state that persists longer than 6 months. It includes pain that cannot be linked to a source of irritation or inflammation and functional limitations and disability that include physical, emotional, and psychosocial parameters |
Chronic pain syndrome |
|
|
The inflammatory stage involves theses responses in the tissue |
Cellular, vascular, and chemical responses in the tissue |
|
|
To minimize msk pain and promote healing, protection is provided via? |
Rest (splint, tape, cast) Cold (Ice) Compression Elevation |
|
|
should be directed to the structure involved to prevent abnormal adherence of the developing fibrils to surrounding tissue and thus avoid future disruption of the scar. |
Tissue-Specific movement |
|
|
The intensity (dosage) of movement should be gentle enough so the fibrils are not detached from the site of healing. |
Intensity of movement |
|
|
Active movement is appropriate in neighboring regions to maintain integrity in uninjured tissue and to aid in circulation and lymphatic flow |
General movement |
|
|
These should all be applied to prevent immobility |
Tissue-specific movement Intensity of movement General movement |
|
|
Specific interventions and dosages for the acute stage |
PROM Low dosage jt mobilization/manipulation techniques Muscle setting Massage |
|
|
Intervention for associated areas |
ROM Resistance exercise Functional Activities |
|
|
Occurs due to swelling and immobility during the acute stage |
Vascular Stasis |
|
|
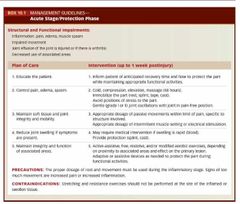
Acute stage/Protection phase |
|
|
Precautions taken during acute stage |
Proper dosage of rest and movement |
|
|
Contraindication for the acute stage |
Stretching and resistance exercises should not be performed at the site of the inflamed or swollen tissue |
|
|
During 2nd - 4th days, the inflammations begins to (inc, dec) |
inc |
|
|
The subacute stage usually lasts around how many days? |
10 to 17 days, or 14 to 21 days after the onset of injury
Can last up to 6 weeks |
|
|
T/F If the patient feels good about their wound, they may return to normal activity during the subacute stag |
False, the new tissue is fragile and easily damaged, returning to normal activity may cause exacerbation of symptoms |
|
|
Initiation of active exercises include? |
Multiple-angle, submaximal isometric exercises AROM |
|
|
Signs of excessive stress with exercise or activities |
Exercise or activity soreness that does not decrease after 4 hours and is not resolved ater 24 hours Exercise or activity that comes on earlier or is increased over the previous session Progressively increased feelings of stiffness and decreased ROM over several exercise sessions Swelling, redness, and warmth in the healing tissue Progressive weakness over several exercise sessions Decreaed functional usage of the involved part |
|
|
First to atrophy when there is joint swelling, trauma, or immobilization |
Slow-Twitch muscle fibers |
|
|
Exercises for _______ _____ are emphasized during the subacute phase, because slow twitch fibers atrophy first when there is joint swelling, trauma, or immobilization |
Muscular Endurance exercises |
|
|
T/F eccentric exercises can be used for non-muscuar injury if they do not reinjure the part |
T, as long as the resistance is low-intensity to avoid DOMS |
|
|
Intiation and progression of stretching |
Warm the tissues Muscle relaxation techniques Joint mobiliaztion/manipulation Stretching Techniques Massage Use of the new range |
|
|
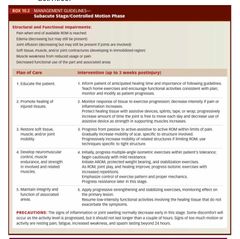
subacute stage |
|
|
Signs of too much motion |
Resting pain Fatigue Increased weakness Spasm lasting
all lasting beyond 24 hours |
|
|
Causes of chronic inflammation |
Overuse, cumulative trauma, repetitive strain Trauma Reinjury of an "old scar" Contractures or poor mobility |
|

|
Chronic inflammation |
|
|
If there is progressive loss of ROM as the result of stretching, (continue, do not continue) to stretch |
do not continue |
|
|
the factors that affect reflex muscle contraction are? |
Trauma Pain Inflammation Infection Emotional Tension Cold Immobilization |
|
|
The self-perpetuating cycle of muscle spasm are as follows |
Reflex muscle contraction Restricted movement Circulatory stasis Pain Muscle spasm repeat |
|
|
What are the signs of too much movement during the acute stage |
Increased pain or increased inflammation |
|
|
______ and _____-________ exercises may cause added trauma to muscle and are not used in the early subacute stage |
Eccentric and heavy-resistance exercises |
|
|
Precautions during subacute stage |
Signs of inflammation or joint swelling is decreased Some discomfort is present as activity level is progressed, but it should not last longer than a couple of hours. |
|
|
Contributing factors to chronic inflammation |
Imbalance b/t the length and strength of the muscles Rapid or excessive repeated eccentric demand Muscle weakness Bone malalignment or weak structural support Change in the usual intensity or demand Returning to an activity too soon after an injury Sustained awkward postures or motions Environmental factors Age-related factors Training errors A combination of several contributing symptoms |

