![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
What is ZD6474?
|
This is also known as Vandetinib and is a VEGF and EGFR inhibitor. This is why Ram was comparing this in the lab to Avastin/Tarceva, which is a VEGF and EGFR inhibitor.
6474 = Vandetanib. So you can remember that it is a VEGF inhibitor for the V, then the next letters spell out and, and the next letter is an E for EGFR inhibitor. |
|
|
Are there skin side effects of the ZD6474?
|
Yes they tend to get a skin rash that Ram says is self-limiting. With sun exposure the rash is worse or more of a copper appearance.
|
|
|
What is the pheo predominant type of VHL?
|
*This is type 2 VHL.
If you go to the VHL family alliance website there is only type 2a and type 2b 2a - pheo predominant, they don't get kidney cancer or pancreatic cysts 2b - get kidney cancer, and pancreatic cysts. 2c is pheo only, but not on VHL family alliance website. These patients are called pheo predominant and not pheo only because we don't know for sure that they won't get renal lesions but they do get predominantly pheos. Type 2c is known as pheo only. Oh No Pheo is the neumonic...with N representing the memory device for 2. |
|
|
What mutation type in VHL is more likely to be associated with pheos?
|
What generally goes with Pheo is a missense mutation. In a partial deletion family they don’t tend to get Pheo, you could try and argue that you need a missense to get Pheo, but he said that is not really true. So if you have a germiline mutation that completely deletes VHL and then you have a second mutation that is a complete deletion then that is too much for the cell and the cell dies it doesn’t get cancer. But if you have a complete deletion that is the germline mutation but then the sporadic mutation that you get is a intra-genic missense mutation well then you have a missense mutation and you can get a Pheo. This is much harder to happen then a sporadic deletion mutation, but it is possible.
|
|
|
What does it mean when we say something Choykeized? If a cyst Choykeizes does that mean it is benign?
|
Dr. Linehan described a phenomenon wheras, and said that Choyke wrote a paper about it, that showed were sometimes these cysts will decrease in size, they call it Choykeize, and then they have seen occasionally where these cysts have then come back and sometimes with solid component and sometimes with increased growth rate. There is no understanding at this point as to why that happens.
|
|
|
What other cancer syndromes besides VHL get renal cysts?
|
Cancer syndromes that get cysts are HLRCC, BHD, and VHL obviously. BHD cysts are usually not macroscopic they are microscopic, but in animal models you will see larger cysts.
|
|
|
What is type II VHL?
|
This is where the predominant visceral manifestation is pheo.
Oh No Pheo ----no starts with N my neumonic for 2. conf notes |
|
|
What is a worse phenotype with VHL a complete or partial deletion?
|
So if you have a germiline mutation that completely deletes VHL and then you have a second mutation that is a complete deletion then that is too much for the cell and the cell dies it doesn’t get cancer so the answer is partial deletion. These patients get kidney cancer.
-Conf Notes 8.11 |
|
|
How long between the second hit with VHL and tumor formation?
|
VHL – they estimate that the time to second hit with vhl till the appearance of tumor is something like 25 years.
-conf notes 8.11 |
|
|
What type of genetic mutation is associatd with adrenal lesions in VHL?
|
In general these are missense mutations. We really usually don't see adrenal lesions with complete deletions.
|
|
|
If we have a patient with type 2 VHL and an asymptomatic adrenal mass less than 2 cm, what makes us pull the trigger for surgery?
|
So our typical plan for type 2 VHL patients that get adrenal lesions smaller than 2cm are that we move based on the cats in general.
-Linehan |
|
|
What is the most common fragile site in chromosome 3?
|
The most fragile site of chromosome 3 is 3p4.21
|
|
|
Where have we seen pheos in VHL patients?
|
adrenal
extra-adrenal: obviously along the sympathetic chain, lung,, neck, also have seen both inside the bladder as well as on the extraperitoneal side of the bladder. |
|
|
Does deletion length correlate with phenotype severity in patients with VHL?
|
Thus, we were
intrigued to find that patients with complete germline deletion of VHL tended to have the least severe clinical disease, as defined by necessity for surgical intervention. In this study there were 13 patients, 11 of these patients had the attenuated phenotype, however 2 of the families had an aggressive phenotype requiring multiple surgeries. The gene that was codeleted in the FISH studies was HSPC300 which had no known function at the time of the study. Maranchie 2004 |
|
|
Tumor size guideline for VHL patients to indicate surgery necessary?
|
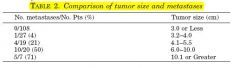
JUrology paper 2004 last author Mac Walther looking at our series of VHL patients and met risk.
|
|
|
What is the inheritence pattern for VHL?
|
Autosomal dominant
|
|
|
What are the clinical manifestations of VHL?
|
Affected individuals
are predisposed to central nervous system hemangioblastomas,renal cysts and cancers, retinal angiomas, endolymphatic sac tumors, pheochromocytomas, pancreatic cysts and neuroendocrine tumors, and epididymal cystadenomas., broad ligament cystadenomas |
|
|
What percentage of patients with VHL get kidney cancer?
|
Estimates range from 25-45%.
Source: J Urol 2004 Mac Walther. |
|
|
The patient has bilateral renal tumors as well as multiple cysts on imaging. The patient on image screening also has pancreatic cysts, an enhancing pancreatic lesion at the head of the pancreas and a CNS lesion conssitent with HMB. No family history of any of these signs of disease and is a great historian. What gives?
|
Approximately 20% of VHL disease patients result from a de novo mutation and do not have a family history.
|
|
|
A patient with an apparently sporadic pheochromocytoma is referred to your clnic for evaluation and treatment. Is there a chance that you should be looking for VHL? What percentage would have it?
|
VHL disease is suggested to account for approximately
a third of patients with a CNS haemangioblastoma,450% of patients with a retinal angioma, 1% of patients with RCC, 50% of patients with apparently isolated familial phaeochromocytoma and 11% of patients with an apparently sporadic phaeochromocytoma5,8,13 Source: Maher 2011 European journal of genetics |
|
|
You are seeing a patient in your clinic with a known family history of VHL with a renal lesion that has been followed for some time by his GP with imaging of the abdomen. The tumor has reached around 3cm in size and he knows that you trained at the NIH and so referred the patient to you so that you could remove the tumor. You are seeing the patient in clinic and what other imaging studies should you consider doing before surgery?
|
CT head and MRI of the spine. Catecholamines as well to make sure that there are no extra-adrenal pheos hiding out.
Overall CNS haemangioblastomas occur in 60–80% of VHL patients1,15,16 and most commonly occur in the cerebellum, spinal cord and brain stem with supratentorial lesions being rare. Patients with cerebellar haemangioblastomas typically present with symptoms of increased intracranial pressure and limb or truncal ataxia (depending on the precise location of the tumour) and the clinical presentation of CNS haemangioblastomas reflects their mass effect. Haemangioblastomas with an associated cyst tend to become symptomatic sooner.16 Source: Maher 2011 |
|
|
What are the common symptoms seen with ELST in patients with VHL?
|
Endolymphatic sac tumours (ELST) can be detected by MRI or CT imaging in up to 11% of patients.36 Bilateral ELSTs are considered pathognomonic for VHL disease. Although often asymptomatic, the most frequent clinical presentation is hearing loss (mean age 22 years),
but tinnitus and vertigo also occur in many cases |
|
|
What is a possible screening schedule for VHL patients?
|
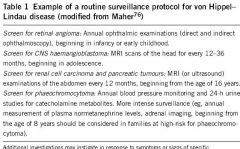
|

