![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
118 Cards in this Set
- Front
- Back
|
what are the effects of occlusal forces? what are its components?
|
teeth
periodontium tmj muscles of mastication |
|
|
injury resulting in tissue changes within the attachment apparatus as a result of occlusal forces
|
occlusal trauma
|
|
|
any contact that inhibits the remaining occluding surfaces from acheiving stable and harmonious contacts
|
occlusal interference
|
|
|
any contact of opposing teeth that occurs before the desirable intercuspation
|
occlusal prematurity
|
|
|
injury resulting from EXCESSIVE occlusal forces applied to a tooth or teeth with NORMAL support. (normal bone and attachment levels)
|
primary occlusal trauma
|
|
|
excessive occlusal force
tooth with normal support |
primary occlusal trauma
|
|
|
injury resulting from NORMAL or EXCESSIVE occlusal forces applied to a tooth or teeth with REDUCED support. (bone/ attachment loss present)
|
secondary occlusal trauma
|
|
|
normal or excessive occlusal force
tooth with reduced support |
secondary occlusal trauma
|
|
|
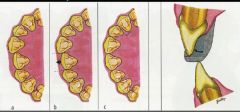
Stage of Occlusal Trauma: dependent on direction, degree and location of occlusal forces
|
stage 1: injury
|
|
|
Stage of Occlusal Trauma: a dynamic process of adaptive remodeling of the following:
1.pdl 2.bone 3.cementum |
stage 2: repair
|
|
|
what is the effect of occlusal trauma on the periodontium in the absence of periodontal inflammation
|
1. trauma to attachment apparatus
2. adaptive repair 3. widened PDL 4. possible radiographic vertical bone loss 5. no loss of periodontal attachment INCREASED MOBILITY WITHOUT AL AND INCREASED PD |
|
|
1. inflammation follows the course of blood vessels into the alveolar bone marrow spaces
2. defect morphology depends on location of blood vessels and thickness of bone 3. spread of inflammation into PDL is secondary in periodontititis |
Pathway of Inflammation:Weinmann
|
|
|
1. excessive occlusal forces alter the normal pathway of inflammation
2. inflammation enters PDL directly 3. development of angular bony defects with intrabony pockets |
Theory of Co-destruction: Glickman
|
|
|
evidence that vertical osseous defects are not caused by occlusal trauma
1. bony defects are result of apical plaque progression in areas of sufficient bony thickness 2. angular defects occur in both the presence and abscence of occlusal trauma |
Vertical Defect Formation: Waerhaug
|
|
|
Results of Animal Studies
|
1. excessive occlusal force on a healthy periodontium results in physiologic adaptation
2. includes increased mobility, PDL width and loss of bone 3. no loss of ct attachment 4. changes are reversible when force is removed |
|
|
Clinical Signs of Occlusal Trauma
|
1. increased mobility
2. fremitus 3. wear facets 4. tooth migration 5. tooth fracture 6. pulpal symptoms |
|
|
radiographic signs of occlusal trauma
|
1. widened pdl
2. thickening of lamina dura 3. vertical bone loss 4. furcation bone loss 5. root resorption 6. alveolar radiolucency and or condensation |
|
|
indications for occlusal therapy
|
1. parafunctional habits
2. occlusal interferences 3. tooth hypermobility 4. increased width of pdl 5. reduced alveolar bone support 6. inflammatory periodontal disease |
|
|
when should occlusal therapy begin and with what?
|
after resolution of periodontal inflammation?
1. SCRP 2. may reduce/resolve signs of trauma 3. if not then proceed to treat the occlusion |
|
|
when is it okay to bypass inflammation and immediately treat the pt with occlusal therapy?
|
gross interferences should be treated at onset of therapy
|
|
|
Methods of Occlusal therapy
|
1. limited occlusal adjustment
2. comprehensive occlusal adjustment 3. removable occlusal splint 4. fixed occlusal splint |
|
|
Occlusal adjustment Indications
|
increasing mobility or fremitus
discomfort during furnction parafunctional habits soft tissue injury food impaction occlusal interferences |
|
|
Occlusal Adjustment CI
|
as treatment for periodontal disease
without pretreatment diagnosis as primary therapy for bruxism severe extrusion or malposition when periodontal inflammation has not been controlled |
|
|
removeable splint indications
|
treat bruxism/parafunction
stabilize occlusion during periodontal treatment maintain occlusion after treatment |
|
|
fixed splint indications
|
mobility interferes with patient comfort
mobility interferes with patient function prevent tipping of drifting of teeth prevent extrusion of unopposed teeth following ortho therapy following acture trauma to teeth esthetic and prosthetic demands |
|
|
Miller Classification: Tooth can be moved less than 1mm in the buccolingual or mesiodistal direction
|
Class 1
|
|
|
Miller Classification:Tooth can be moved 1mm or more in the buccolingual or mesiodistal direction
No mobility in the occlusoapical direction (vertical mobility) |
Class 2
|
|
|
Miller Classification:Tooth can be moved 1mm or more in the buccolingual or mesiodistal direction
Mobility in the occlusoapical direction is also present |
Class 3
|
|
|
Miller Classification: Normal (physiologic) movement when force is applied.
|
Class 0
|
|
|
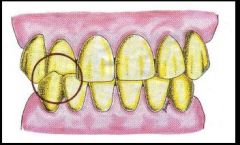
Signs of Occlusal Disease
|
1 .pathologic tooth wear
2. abfractions, notches between teeth and gum 3. fremitus which may cause fractured teeth or fillings 4. headaches and tmj pain 5. tooth sensitivity to cold and hot 6&7. bone loss and mobility with perio disease |
|
|
when the teeth are not in harmony with the joints and movements of the mandible
an underseriable occlusal contact that may produce mandibular deviation during closure to maximum intercuspation or may hinder smooth passage to and from MIP |
occlusal interference
|
|
|
occlusal contact that interrupts the harmonious closure of the teeth along the CR arc
|
occlusal prematurity
|
|
|
An interference between posterior teeth on the side of the dental arches to which the mandible is moving laterally in excursion, usually involving a stamp cusp against a shear cusp. Synonym: Laterotrusive Interference.
|
working interference
|
|
|
An interference between posterior teeth on the side of the dental arches away from which the mandible is moving laterally in excursion, usually involving stamp cusp against stamp cusp.
|
nonworking interference
|
|
|
An interference between posterior teeth on ether side of the dental arches caused by a protrusive movement of the mandible.
|
protrusive intereference
|
|
|
An interference involving exclusively a maxillary lateral incisor against its opponent during a lateral protrusive excursion of the mandible. This interference is observed as a "trip" by the lateral incisor during which the anterior guidance is momentarily borne by a lateral incisor without help from other maxillary anterior teeth.
|
Lateral protrusive interference.
|
|
|
An interference between posterior teeth when the mandible has translated laterally beyond the guidance of the cuspid. The incisors, not the posterior teeth, should provide anterior guidance after "crossover".
|
Crossover interference.
|
|
|
form of occlusal treatment in which the occlusal surfaces of one or more teeth are adjusted or modified by grinding with rotary dental instruments.
|
Occlusal Equilibration/adjustment
|
|
|
Forms of Occlusal Equilibration
|
1.Equilibration
2.Selective grinding 3.Limited adjustment 4.Coronaplasty 5.Coronal reshaping 6.Occlusal correction or recontouring 7.Spot grinding |
|
|
The Basic Principles of Occlusal Equilibration
|
•Primary Purpose: To eliminate deflective occlusal contacts that interfere with the physiologic function of the Tempromandibular Joint.
•Goal: A comfortable occlusion |
|
|
_______ __________is designed to eliminate all premature or deflective tooth contacts that prevent the condyle-disk assembly from complete seating in their respective fossa (centric relation) when the jaw closes to maximum intercuspation (MIP).
|
proper equilibration
|
|
|
Maximum distribution of occlusal stress in centric relation.
Forces of occlusion should be borne as much as possible by the long axis of the teeth. When there is surface to surface contact of flat cusps, it should be changed to a point to surface contact. Once centric occlusion is established, never take teeth out of centric occlusion. |
The Basic Principles of Occlusal Adjustment
|
|
|
Indications for occlusal adjustment
|
1. periodontal bone loss
fremitus, and mobility 2. restorative prosthetic 3. abfractions 4. implants 5. adjunct to ortho tx 6. orthognathic surgery 7.limited movement of the mandible 8.endodontics |
|
|
REMEMEBER THAT EQUILIBRATION IS NOT:
|
•REVERSIBLE
•BENIGN •A ROUTINE PROPHYLACTIC MEASURE •SURE FIX FOR BRUXISM |
|
|
CONTRAINDICATIONS FOR EQUILIBRATION
|
Patient is symptomatic
•Just because interferences exist •Just because a joint clicks •Lack of general physical and emotional stability of the patient •Lack of interest, concern, or compliance by the patient •Lack of maxillomandibular or dental stability of the patient |
|
|
Indications for equilibration of tmd patients
|
•ONLY FOLLOWING SUCCESSFUL OCCLUSAL APPLIANCE THERAPY AND AFTER OCCLUSION IS CLEARLY INDICATED IN THE ETIOLOGY OF THE TMD - muscle origin
•INTERFERENCES ARE PRESENT •DISCS ARE IN PLACE •SYMPTOMS ARE RESOLVED |
|
|
OCCLUSAL ADJUSTMENT IS NOT INDICATED FOR
|
AS A CURE FOR BRUXISM
TO PREVENT FUTURE TMD |
|
|
Goals of Occlusal Adjustment Technique
|
•Promote Masticatory Comfort and Efficiency
•Allow Proper Esthetics and Phonetics •Be Compatible With Periodontal Health •Provide Stable Contacts From CO to MIP •Provide Smooth Excursive Movements •Directs Occlusal Forces Axially |
|
|
Guidelines of the Occlusal Adjustment Technique:
1. Equilibrate Teeth After: |
•RESOLVING SYMPTOMS (Splint
•or minor adjustment). •PROVING FEASIBILITY ON DIAGNOSTIC CASTS •LOADING OF CONDYLES WITHOUT TENSION/TENDERNESS |
|
|
Guidelines of the Occlusal Adjustment Technique:
2. treatment planning |
CONSERVATION -- MINIMIZE ALTERATIONS TO THAT WHICH WILL MEET TX GOALS
•PERFORM ON DIAGNOSTIC CASTS FIRST! |
|
|
Guidelines of the Occlusal Adjustment Technique:
3. NEFF’S RULE OF THIRDS (CUSP TIP TO CENTRAL GROOVE) |

•NEAR GROOVE -- OKAY
•MIDDLE THIRD -- CAUTION •NEAR CUSP TIP – STOP •Clarifies if adjustment is doable or should you consider other tx options such as ortho, restorative or surgery. |
|
|
Guidelines of the Occlusal Adjustment Technique
4:Maintain ________ dimension of occlusion |
vertical
|
|
|
Principles of the Occlusal Adjustment Technique
5. ADJUST SHEAR CUSPS – SPARE STAMP CUSPS |

Don’t shorten stamp cusps! Narrow stamp cusps before reshaping fossae.
|
|
|
Guidelines of the Occlusal Adjustment Technique
6.MAINTAIN AT LEAST ONE _________STOP FOR EACH TOOTH |
stabilizing
|
|
|
Guidelines of the Occlusal Adjustment Technique
7. PROVIDE _____________STOPS - WHEN POSSIBLE |
anterior
|
|
|
Guidelines of the Occlusal Adjustment Technique
8. PRESERVE OR IMPROVE __________ |
esthetics
|
|
|
Guidelines of the Occlusal Adjustment Technique
9. LOAD THE MANDIBLE DURING EXCURSIONS WHEN MARKING ______________ (Bilateral manipulation) |
interferences
|
|
|
Principles of the Occlusal Adjustment Technique
10. A FULL __________MAY TAKE LONGER THAN ONE VISIT. |
equilibration
|
|
|
Where to Grind?
|
Adjust inclines, not stamp cusp tips.
|
|
|
The Three Golden Rules of Occlusion
|
1.The first Golden Rule is to have bilateral and even occlusal contact.
2.The second Golden Rule is posterior teeth disclusion, or anterior and canine guidance. 3.the third Golden Rule of Occlusion is an unobstructed envelope of function. |
|
|
any deviation from normal occlusion
|
malocclusion
|
|
|
Class 1 Malocclusion
|
crossbite
anterior crowding open bite midline deviation loss of posterior support bruxism |
|
crossbite anterior tx
|
selective grinding
limited ortho extensive rehab |
|
|
crossbite bilateral posterior tx
|
ortho
restorative -pallative -provide canine guidance orthognathic surgery |
|
|
open bite-anterior tx
|
provisional plateau on lingual surface of maxillary anterior teeth guidance
extraction of third molars can help occlusal reduction of lateral teeth create canine guidance , resin or porcelain on lingual invasive: vrown lengthening, endo, complex rehab |
|
|
Class 2-1 maloccclusion tx
|
alleviate/eliminate interferences, favor the anterior portion
restorative orthognathic surgery |
|
|
class 2-2 malocclusion tx
|
centric contact in anterior region
selective grinding or restorative |
|
|
class 3 malocclusion tx
|
stable occlusion posterior guidance
extraction of lower 3rd molars may help orthognathic surgery and or restorative possibly do nothing |
|
|
determinants of occlusion
|
1.two condyle/disc assemblies
2. teeth 3. neuromuscular system |
|
|
posterior/fixed determinates
produces axises for rotation, translation and other mandibular movements |
condyle/disc assembly
|
|
|
anterior determinate
Consist of the inter-occlusal contacting points and inclines of cusps of the opposing arches They are variable: (1) Modified by nature through Occlusal Wear, Drifting, Loss of Teeth, Extrusion (2) Modified by man: (a) Occlusal reshaping (b) Occlusal restoration |
teeth
|
|
|
Programmed by the teeth, more specifically the proprioceptive fibers in the PDL.
Conscious response: 1. Protective 2. Physiologic activity (chewing, swallowing, speech) Subconscious response: Pathologic 1.Bruxism 2.Other Parafunctional Habits |
neuromuscular system
|
|
|
1. The anterior determinant of mandibular movement.
2. It is the effect of tooth inclines on the envelope of motion and the envelope of function. 3. Can be defined as the dynamic relationship of the mandibular anterior teeth against the maxillary anterior teeth through all ranges of function 4. It is completely independent of condylar guidance, and is more important than condylar guidance as a determinant of posterior occlusal form. |
Anterior Guidance in the Natural Dentition
|
|
|
Function of Anterior Guidance: Anterior tooth position
|
incise food
aid in speech aid in esthetics protect the posterior teeth by directing the teeth together in MIP so that the closing forces will be verticall directed onto the posterior teeth |
|
|
anterior guidance is affected by:
|
posterior of the anterior teeth
patients arch relationship degree of overbite degree of overjet |
|
|
In patients with normal jaw relationships the vertical and horizontal overlap of anterior teeth and the lingual concavities of the maxillary incisors are highly significant during protrusive movements.
In lateral excursions the tooth contacts normally exists between the canines and those contacts usually dominant that movement. |
canine guidance and disclussion
|
|
|
Pronounced vertical overlap of the anterior teeth:
1. Permits posterior teeth to have _______cusps 2. Greater the degree of separation of the posterior teeth |
longer
|
|
|
Minimum anterior vertical overlap:
1. Require ______cusps 2. Lesser degree of separation of the posterior teeth |
shorter
|
|
|
Pronounced horizontal overlap of the anterior teeth:
Requires _____cusps of the posterior teeth Lesser degree of separation of the back teeth A minimum anterior horizontal overlap permits the posterior cusps to be ________. |
short
longer |
|
|
Customized Anterior Guide Table:
When preparation of anterior teeth is considered, the exact nature of the anterior contact should be _________ to the articulator. Where it can be _______and _________before these teeth are prepared. |
transferred
studied stored |
|
|
when is group function viable?
|
1- When it is already present and there are no adverse effects present
2- When Distribution of Excursive Stresses is advisable Such as: Presence of Bone Loss around Teeth Extensively Restored Teeth Loss of Bony Support around Canine Tooth Presence of Canine Wear |
|
|
steps in forming an anterior guide table
|
1. raise incisal guide pin 2mm
2. lubricate the pin and acrylic stop table and lingual max incisors with MRA 3. form ball of triad and place on the table. form triad over the sides of the table for stability 4. manipulate the articulator in a hinge and a range of lateral and protrusive movements. *note* make sure the anterior teeth are touching in all movements. make sure each movement include the entire incisal edge to edge 5. excess is trimmed, so table doesnt interfere with the hinge opening-closing arc of the articulator 6. incisal pin should contact the table in all excursive movements |
|
|
Difficulty breathing during sleep due to
obstructed nasal passages or collapsed oral airway |
sleep disordered breathing
|
|
|
Classified as the most moderate
manifestation of sleep disordered breathing Considered an indication of the existence or onset of a sleep breathing disorder |
snoring
|
|
|
Complete loss of airway patency
Patients demonstrate inspiration flow levels while asleep that are 50% less than when they are awake Defined by the National Heart Lung and Blood Institute as repeated episodes of no breathing for at least 10 seconds at a time called apneic events |
obstructive sleep apnea
|
|
|
Occurs when soft tissue in the upper
airway collapses causing a blockage Breathing stops for 10 seconds or longer Frequently happens hundreds of times per night |
Obstructive sleep apnea
|
|
|
2 types of Apnea
|
Central Sleep Apnea
Obstructive sleep apnea |
|
|
Neurological disorder
Occurs when the brain fails to send the appropriate signals to the muscles that initiate respiration |
Central Sleep Apnea
|
|
|
Obstructive Sleep Apnea is a ________ __________ condition. When left
untreated it takes an average of eight years off a person’s life! |
life threatening
|
|
|
Signs and Symptoms OSA
|
Excessive daytime tiredness
Snoring Hypertension Morning headaches Acid Reflux (GERD) Menopause (Hormone deficiency) in women Obesity Large neck circumference |
|
|
apnea hypopnea index
|
number of apneic and hypopneic
events that occur during the night (basically a count of all the times a patient stops breathing) |
|
|
AHI: 5-15 events is
|
mild
|
|
|
AHI: 15-30 events is
|
moderate
|
|
|
AHI: >30 events is
|
severe
|
|
|
SDB divided into three categories
|
snoring
upper airway resistance syndrome obstructive sleep apnea-most severe |
|
|
What Causes OSA in Children
|
Large tonsils and/or adenoids
Children with narrow maxillary arch development More common in overweight children Some children with enlarged tonsils/adenoids may be underweight Younger children with sleep apnea may have delayed growth because of disruptio |
|
|
High Risk for OSA in Children
|
Narrow facial bone structure
History of cleft palate Down Syndrome Children with allergies Asthma Reflux Frequent sinus infections Family history |
|
|
The pathology behind snoring and OSA is the ______.
|
same
|
|
|
An unstable airway causes both what?
|
snoring and osa
|
|
|
Not all _______have OSA. It is the most noticeable symptom.
|
snorers
|
|
|
How is Sleep Disordered Breathing treated?
|
CPAP
Surgery: 30-50% effective |
|
|
CPAP stands for?
|
Continuous Positive Air Pressure
|
|
|
Characteristics of CPAP
|
•The ‘Gold Standard’ for treatment of OSA.
•CPAP is prescribed to nearly 100% of the medically diagnosed OSA patients. •Efficacy is close to 100% if patient can stand the pressure. •CPAP delivers room air under pressure through a nasal mask. •Air pressure creates a pneumatic splint that holds the airway open. |
|
|
ESS score below what is considered normal?
|
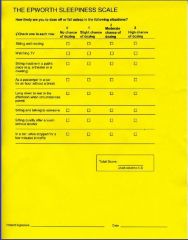
8
|
|
|
It is well documented there is considerable overlap of ________and _______ in patients with TMD’s and CSD’s , especially those patients with myogenous TMD’s
|
signs
symptoms |
|
|
Cervical Disorders are very _______associated with TM Disorders
|
often
|
|
|
Cervical and Central excitation of cervical sensory and motor neurons stimulates trigeminal motor neurons, causing an increase in _________ _________ activity
|
masticatory muscle
|
|
|
Reported to be the most common cervical nerve disorder.
|
Lesser Occipital Neuralgia
|
|
|
Commonly seen after trauma such as extension/flexion injuries.
|
Lesser Occipital Neuralgia-medications rarely provide any lasting relief
|
|
|
Lesser Occipital Neuralgia symptoms
|
1. Occipital pain which may or may not be unilateral.
2. Pain radiating from the occiput in and through the parietal and temporal regions to the anterior temporal, zygomatic and frontal portions of the head. 3. Pain and/or pressure behind the ipsalateral eye 4. Pronounced photophobia on the affected side 5. Nausea when the pain becomes severe 6. Pain radiating into the ipsalateral ear, shoulder, and at times, the arm |
|
|
The cervical sympathetic chain connects with this large nerve
|
Greater Occipital Neuralgia
|
|
|
The symptoms of greater occipital neuralgia are ______ yet ________ _________from those of lesser occipital neuralgia
|
similar
distcintly different |
|
|
As with lesser occipital neuralgia, neuralgia of the greater occipital nerve produces _____ and __________pain that radiates to the vertex, temporal, periorbital regions, and the mandible
|
occipital
suboccipital |
|
|
The pain is characterized as a _______, ________pain which, when severe, is perceived as driving pain on which shock like jabs may be superimposed
|
dull
constant |
|
|
Joint Vibration Analysis allows you to ....
|
view specific vibration patterns
-certain causative/dysfunctions have certain patters |
|
|
Diagnostics for TMD
|
clinical examination
imaging biometrics lab studies photographs |
|
|
biopak components for determining TMDs
|
joint vibration analysis
electrognathology electromyography mastication analysis |
|
|
imaging used to help diagnose TMDs
|
plane films
hypocycloidal tomography ct scans mri |

