![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
135 Cards in this Set
- Front
- Back
|
Risk factors for amniotic fluid embolism |
maternal: - incr age - multiparity - strong frequent titanic contractions - Hx allergy/ atopy fetal: - mec stain liquor - IUFD - polyhydramnios - chorioamnioitis - microsomia - uterine rupture/ placenta accreta |
|
|
Biphasic response to AFE |
1. Pulmonary HTN - ~30min - AFE --> biochemical mediator --> pul a vasospasm --> pul HTN and RVF - mechanical obstruction to pulmonary vessel 2. LVF, pulmonary oedema, DIC, neurological impairment |
|
|
distinguish AFE from fat embolism |
fat embolism has petechial rash! |
|
|
diagnosis for AFE |
Dx of exclusion more specific tests 1. pulmonary blood sample - fetal debris 2. Zinc - incr 3. Sialyl Tn antigen incr |
|
|
AFE and future pregnancy |
no increased rise of reoccurrence |
|
|
Classification of drugs in pregnancy |
A - large # pt, no prob - paracetamol B -->B1 - limited # w/o prob, no animal evidence of prob -->B2 - limited # w/o prob, inadequate animal studies -->B3 - limited # w/o prob, animal studies increase fetal damage C - harmful (?reversible) effect on fetus, no malformation. e.g. opioid D - caused/ suspected to cause fetal malformation X - cause permanent fetal Dx/ not to be used in preg |
|
|
Drugs to incr utrine tone |
oxytocics 1. oxytocin - 5IU bolus - uterine contraction, peripheral vasodilation - SE: decr coronary artery perfusion (vascular relaxant), decr PVR --> incr HR, mild ADH activity 2. ergometrine - 0.5mg IM, 0.125mg IV slowly - uterine constriction - SE N/V (CTZ), headache (incr BP). relative C/I PET, heart disease, cerebral aneurysm 3.Misoprostol - 1mg PR - uterine constriction - SE: N/V/ D, bronchospasm, shunting 4. PGF-2 alpha - carbiprost - 0.25mg intramyometrial or IM 10-15min max 2mg - uterine contraction - SE: N/V/D, bronchospasm, shunt + hypoxia 5. alpha-agonist - e.g. clonidine |
|
|
Drugs to decrease uterine tone |
1. smooth muscle relaxation - VA - Mg - CCB - nitrates 2. B-agonists e.g. salbutamol 3. NSAIDs NB- N2O and thiopentone do not affect uterine tone |
|
|
Guidelines for DVT prophylaxis in pregnancy |
UK guidelines - Royal college of obstetrician and gynaecologist 1. assess risk - prv VTE, Hx thromboembolic disorder, cancer, >35BMI, parity >3, smoker, immobility, pre-eclampsia 2. categorise as high, intermediate or low risk High risk: antenatal prophylaxis, postpartum 6weeks prophylaxis intermediate risk: consider antenatal prophylaxis, postpartum 7 days prophylaxis low risk: pre and post mobilise, avoid dehydration |
|
|
cause of early decels on CTG |
fetal head compression |
|
|
cause of late decels |
fetal asphyxia (decr O2 --> vasocontrict --> reflex brady) |
|
|
Transmission of pain in first stage of labour |
first stage - uterine contraction and cervical dilatation 1. pelvic plexus 2. superior, middle and inferior hypogastric plexuses 3. lumbar sympathetic chain 4. white rami of spinal nerves T10-L1 |
|
|
Secondary stage of labour pain transmission |
second stage - stretch birth canal and perineum pudendal nerve S2-4 anterior root = efferent motor root |
|
|
analgesic options in labour |
1. Non-Pharm - emotional support - massage - TENS - hydrotherapy 2. Pharm - N2O - IV morphine - Remifentanly PCA - 20-40mcg Q3min, resp Depression) - neuroaxial: epidural/ CSE |
|
|
How does Mx of collapse in obstetric population differ from normal population |
1. difficult - ventilation, rapid hypoxia and acidosis, rapid blood loss, reduce O2 carry capacity 2. Left lat tilt 15degree - aortocaval compression 3. intubate early + difficult (aspiration, oxygenation) 4. volume replace aggressive (care with preeclampsia). haemorrhage may be concealed 5 Perimortal CS within 5min 6. chest compression higher on sternum (enlarged breast, incr AP diameter of thorax) |
|
|
Confidential enquiry into maternal deaths UK 2011-2013 |
leading cause of death - direct: thrombosis/ TE - indirect: cardiac disease (overall aswell) - 6week - 1yr: mental health Top 3 overall causes of death 1. cardiac disease 2. sepsis 3. thrombosis |
|
|
at what gestation do you worry about aortocaval compression |
20weeks + |
|
|
CVS changes in pregnancy |
1. Incr SV 25% 2. incr CO 40% (reduce PVR, incr HR) 3. aortocaval compression after 20weeks |
|
|
Respiratory changes in pregnancy |
physiological: 1. decr ETCO2 (30) 2. incr MV 3. decr FRC anatomical 1. failed intubation 7x more likely |
|
|
Haematological changes in preg |
1. dilutional anaemia 2. Thrombocytopenia 3. increase clotting factors 4. decr alb 5. decr pseudocholinesterase |
|
|
GIT changes in pregnancy |
NO change in rate of gastric emptying and basal gastric acid production GORD due to decreased oesophageal sphincter tone (progesterone) but delayed gastric emptying in labour |
|
|
how long does sodium citrate last how long does it take to work |
1hr take 10-15min to work |
|
|
ranitidine - how long to work IV |
45min |
|
|
Causes of postpartum haemorrhage PPH |
primary PPH (24hr delivery - 4 T: --> Tone --> TISSUE - retained (placenta accrete (endomedium), intreat (myometrium), percreta (other organs) --> TRAUMA --> THROMBIN (coag prob) 2. Secondary PPH (24hr - 6weeks postpartum) - infection e.g. endometritis |
|
|
RF for PPH |
Maternal - advanced age - antepartum haemorrahge - anaemia - Uterus: fibroid, clot Labour - long - induced Fetal - twins - polyhydramnios - placenta: praaevia, increta, percreta, accreta |
|
|
Prevention of PPH |
1. prophylactic oxytocics in 3rd stage- decr by 50%
2. early cord clamp 3. controlled cord traction |
|
|
Transexamic acid and PPH |
- meta analysis - reduced need for blood transfusion by a third WHO guidelines recommend if bleeding despite uterotonics. UK guidelines say no role |
|
|
Define preeclampsia |
pregnancy induced hypertension (SBP>140mmHg, DBP > 90mmhg) develop after 20week gestation or up to 3months postpartum + assoc with 1+ of: - renal impairment - liver disease - neurological disease - haematological disturbance - FGR |
|
|
severe pre-eclampsia |
HTN SBP > 160, SBP>110 + 1or more of: - IUGR or decr fetal blood flow/ abnormal CTG - platelet <100 + DIC or haemolysis - CNS Sx - liver Sx - severe proteinuria (>5g/24hr) |
|
|
Risk factors for pre-eclampsia |
1. primip 2. 1st pre with new partner 3. pre-existing HTN 4. DM 5. FHx 6. multiple pregnancy 7. obesity 8. incr maternal age |
|
|
Patholophysiology of pre-eclampsia |
placental ischamia deficient placental implantation vasoactive substances --> 1. endothelial damage + vasospasm 2. PG metabolism --> incr TXA and decr prostacyclin |
|
|
HELLP |
haemolysis elevated liver enzymes, low platelet - microangiopathic haemolytic anaemia |
|
|
Mx of pre-eclampsia goals |
1. decrease BP 2. method/timing delivery 3. prevention of eclampsia |
|
|
how much to drop the BP by in Rx of preeclampsia |
rate of 10-20mmHg every 10-20min use labetalol (50IV Q20min), hydrazine, nifedipine |
|
|
prevention of eclampsia |
MgSO4 - decr risk by 50% NNT 50 |
|
|
which b-blocker can't be used in pregnancy |
atenolol - FGR |
|
|
Ca-channel blocks 2 types |
1. verapamil - heart action mainly - decr contractility and AV node conduction 2. dihydropyridines e.g. nifedipine - act on vascular smooth muscle relaxation diltiazen in b/w verapamil and nifedipine verapamil and diltizem c/i in b-blocker |
|
|
ACEI in pregnancy |
NO - renal agenesis of fetes |
|
|
Snip in pregnancy |
avoid - methaemoglobinaemia |
|
|
MgSO4 interaction in anaesthesia |
1. prolong NMBD - depolarising and non-depolarising 2. potentate hypotension with nifedipine 3. tocolytic -> PPH risk |
|
|
timing of eclampsia |
antepartum 40% intrapartum 20% postpartum 40% |
|
|
therapeutic Mg level |
2-3.5mmol/L |
|
|
toxicity Mg |
>3.5mmol/L - monitor by loss if patellar reflexes >5--> resp paralysis >12 --> cardiac arrest |
|
|
Rx of Mg toxicity |
calcium glutinate 10ml 10% over 10min |
|
|
Meta-analysis in 2011 of pregnancy women undergoing GA |
1. mortality 1:10,000 2. no increase risk major birth defect 3. surgery and GA not major risk factors for spontaneous aboration 4. acute appendicitis with peritonitis --> risk for fetal loss |
|
|
when to do in pregnancy - RSI - lat tilt |
RSI 18+ lat tilt 20+ |
|
|
Drug in pregnant patient non-obstetric surgery |
- Midazolam - considered safe -Propofol class B (decr bone ossification in rats), thiopentone class A -N2O - safe but affect DNA synthesis + teratogenic in rats -Ketamine - uterine contractions (avoid) -NSAIDs - avoid in 1st tri (miscarriage) and 3rd (closure PDA) -VA - class B, decrease uterine contractions - LA - incr risk toxicity (use lower doses) - NBNMD - class B - sux - class A |
|
|
Mx of difference types of placenta prevaeia |
1. placenta praaevia - GA or regional 2. placenta percreta - GA 3. placenta accrete - GA with balloons in situ by radiology |
|
|
grades of placenta praaevia |
Grade 1 - lower edge NOT each internal os (<4cm) Grade 2 - lower edge reach internal os but not covered Grade 3 - partially cover internal os Grade 4 - completely cover internal os increase risk wiht increased number of LSCS |
|
|
Risk index in pregnancy and cardiac disease |
CARPREG risk index (cardiac disease in pregnancy) - quantify cardiac risk factors with indigence of cardiac complications and mortality - based on - Hx of Sx, NYHA SOB, LVEF, valve lesion |
|
|
adenosine in pregnancy |
safe usual dose CTG monitor --> fetal brady |
|
|
Mx of AF in pregnancy |
1. Dig, B-block or non-dihydropyridine CCB 2. DC cardioversion (if unstable) 3. anticoagulation |
|
|
neuroaxial and platelet cut off in pregnancy - normal - PET - ITP |
normal: >80 and not falling PET - <100 - check coag - >75 + coag normal --> regional ITP platelet >100 (as platelet dysfunction present) |
|
|
Types of vWD |
type 1 - deficit vWF (common - 70%) Type 2 - abnormal wWF type 3 - absence of vWF (rare) |
|
|
vWD and pregnancy and neuroaxial |
type 1 - increased production in preg, check coagulation and vWF level Type 2 and 3 - no EDB |
|
|
Regional anaesthesia in MS |
demyelinating inflammatory disease regional - theoretical concern can incr LL sx demyelinating SC exposed to neurotoxic effects of LA therefore epidural may be better than spinal |
|
|
GA and MS (multiple sclerosis) |
Sux - reduce dose, incr sensitivity NDMR - resistance - use normal dose temperature Mx important irrespective of method of delivery, relapse likely postpartum |
|
|
Scoliosis and regional |
1. increase dural puncture 2. partial block 3. difficult insertion |
|
|
raised ICP and regional in pregnancy |
NO spinal or epidural |
|
|
spinal bifida defn |
developmental congenital disorder due to incomplete closing of neural tube |
|
|
Spina bifida and regional |
spina bifida occulta - ok for regional (epidural>spinal) - check level --> incomplete formation of lamina --> check for cord teetering - external cutaneous - tuff hair, birthmark, lipoma Spinal bifida cystica and myelomeningocele - CI regional syrinx - in all types of spina bifida - out pouching of spinal cord |
|
|
myasthenia gravis and mortality in pregnancy |
inversely proportional to duration of disease 1st year diagnosis - highest risk >7yrs since diagnosis - minimal risk |
|
|
MG and regional |
preferred |
|
|
MG and muscle relaxation |
Sux - resistance - need increased dose NDMR - sensitivity and prolonged effect - reduce dose. reversal can --> cholinergic crisis MgSO4 - relatively c/i --> myasthenia crisis |
|
|
spinal cord injury level of injury don't feel contractions |
T5 - may present with autonomic dysreflexia |
|
|
Causes of failed spinal |
Patient factors - - disease: --> scoliosis, spina bifida --> dural ectasia in Marfan - anatomical variants: --> subarachnoid trabeculae --> subdural block --> septae Technical factors - - incorrect placement (pencil point needle) - dural flap LA factors: --> maldistribution - failure to spread or too much CSF --> resistance --> chemical failure - bad batch |
|
|
Spinal needle less likely to cause dural puncture headache |
sproute (pencil point) < quinke |
|
|
PHPD symptoms |
- typically 24-48hr, can occur immediately - frontooccipital headache - CN involvement - abducens n (traction when CSF vol low), rarely oculomotor, trigeminal |
|
|
Mx of dural puncture |
1. intrathecal catheter - reduce incidence from 60 --> 30%. leave in 24hr. ?role of intrathecal morphine 2. bed rest - does not help 3. Caffeine - controversial 4. blood patch - 60% success after first, 80% success after second experimental techniques 1. epidural fluids - short term relief only 2. epidural morphine - emerging evidence of success in reducing need for blood patch |
|
|
normal clinical course of PDPH |
70% resolve by 1 week 95% resolve by 6weeks |
|
|
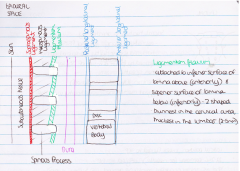
extension of epidural space |
foramen magnum to sacrococcygeal membrane b/w dura and ligamentum flavum |
|
|
width of epidural space |
increase cranial --> caudal C - 2mm T - 3mm L - 5mm due to this shape spread of LA affected, lower thoracic epidural spread more cranial, higher thoracic epidural spread more caudal T4/5 insertion --> T2-8 block T8/9 insertion --> T4/12 block |
|
|
draw epidural space |
|
|
|
Minimum monitoring for neuroaxial block (ANZCA document) |
1. BP - regular 2. RR 3. conscious state evaluation 4. ECG and sats - available 5. monitored for 30min until vital signs stable |
|
|
sympathetic block in neuroaxial block |
2-3 level above sensory block |
|
|
Motor bock in neuroaxial block |
2 level below sensory block |
|
|
NICE Guidelines height of block |
- T6 light touch - T4 cold touch |
|
|
Bromage score |
I - complete - NO movement feet or knees II - almost complete - only move feet III - partial - partial knees IV - none - full flexion of knee and foot Aim bromage I or II in LSCS |
|
|
recovery of fibres post spinal |
1. first to recover - touch and pressure A-beta 2. second to recover - pinprick A-delta 3 last to recover - cold C-fibre therefore as epidural wear off will feel pain even tho block to ice adequate therefore touch more sensitive measure |
|
|
performing EPB evidence based - continuous vs resistance - LORS - predistention - catheter length in epidural space |
Continuous vs resistance - continuous reduce incidence dural puncture LORS - reduce dural tap - reduce VAE - reduce pneumocephalus (dural puncture with air) Pre distension epidural space with saline --> reduce epidural vein cannulation and unblocked segments length in epidural space - 4-5cm reduce missed segments and risk of catheter knott |
|
|
Advantages of PCEA in epidural (c/w continuous infusion) |
1. incr material satisfaction 2. lower LA total dose 3. lower motor block |
|
|
Why use low dose formula (0.2% or 1%) |
lower dose --> inc NVD |
|
|
why use ropivacine vs lignocaine vs bupivacine |
bupivacine - avoid inc cardiotoxicity lignocaine - repeat doses --> tachyphylaxis |
|
|
Why use opioid in epidural |
synergistic with ropivacine - incr analgesia - incr maternal satisfaction |
|
|
argument against lignocaine 2% + adrenaline |
neurotoxicity - can't give intrathecally (sodium metabisulphite --> arachnoiditis) alternative Naropin 0.75% --> much much longer block |
|
|
peak plasma lignocaine dose post epidural lignocaine 2% + adrenaline |
30min |
|
|
C/I to epidural/ neuroaxial - absolute - relative |
Absolute: pt refusal Relative - sepsis - coagulation - platelet <80 - anticoagulation use - neurological dx - spina bifida, raise ICP - CVS: severe valvular stenosis |
|
|
Mx of epidural disconnection |
reconnection safe if: 1. <8hr disconnection 2. fluid inside catheter static (<12.5cm moved and does not move when lifted above patient) |
|
|
How to reconnect epidural catheter |
soak in 10% povidone iodine solution for 3min dry cut 20cm from end with sterile instrument --> if not remove catheter |
|
|
epidural in sepsis |
limited evidence, may indicate no increased risk sepsis relative C/I to neuroaxial block risk vs benefit analysis for patient pre-procedure Abx |
|
|
Distinguish post part foot drop causes |
1. lumbosarcral vs common perineal nerve (rarer) Lumbosacral trunk - compressed by fetal head or forceps - unilateral foot drop - sensation loss lateral CALF + FOOT common perineal - improper positioning in lithotomy - unilateral foot drop - sensory DORSUM FOOT ONLY |
|
|
femoral neuropathy |
cause: fetal head or forceps or retractor in LSCS sensory: anterior thigh, medial leg motor: hip flexion, knee extension reflex - REDUCE/ ABSENT KNEE JERK |
|
|
Obturator nerve palsy |
Cause: forceps delivery Sensory: medial thigh motor: aDDuction hip NB: may be combined with femoral n damage |
|
|
Nerve root damage L2, 3,4,5, S1 |
L2: anterior thigh, hip flexion L3 - medial thigh, hip aDDuction L4 - lat thigh, knee, leg extension L5 - lat leg, dorum foot, ankle dorsi flexion S1 - lateral foot, ankle plantar flexion |
|
|
most common organism in epidural abscess |
staph aureus (gram +ve cocci) |
|
|
Cause of meningitis post neuroaxial |
strep viridans |
|
|
cessation of clopidorel and ticlopidine pre neuroaxial |
clopidogrel - 7days (less time do P2Y12 assay) ticlopidine - 10-14days |
|
|
heparin preneuroaxial - IV - SC |
IV -4hr after last dose - check APTT 1hr before next dose SC - 6hr after last dose (ESRA + ANZCA) - 2hrs before next dose (ESRA + ANZCA) |
|
|
Clexane (LMWH) - pre block - catheter removal |
Pre block - prophylactic - 12hr post dose - therapeutic - 24hr - after block next dose given 4hr later Removal of EDB catheter - prophylactic 12hr post dose - therapeutic - 24hr post dose - next dose 4hr later |
|
|
Warfarin in neuroaxial |
INR <1.5 perform or remove catheter |
|
|
Fondaparinux |
neuroaxial CI remove EDB catheter >36hr after last dose, wait 12 hr before next dose |
|
|
Bloody epidural tap in elective surgery |
ANZCA pain guidelines - incr risk haemoatoma in patient receiving intraop heparin - insufficient data to support cancellation of a case ESRA 2010 - delay operative to next day |
|
|
Anticoagulation and peripheral nerve block |
should follow same principle as neuroaxial block esp deep plexus, non-compressible and near vascular structures some risk vs benefit for peripheral nerve |
|
|
Risk factors for total spinal |
Drug factors - drug dose (not volume) - basicity - less with hyperbaric - prior drug epidural LA Patient Factors - incr intra-abdo pressure - BMI pregnancy - spinal canal abnormality Technique - higher lumbar - immediate supine position - finer spinal needle |
|
|
In PPH, what measures are available to reduce degree of blood loss on the table? |
SURGICAL - bimanual uterine compression and packing - aortic compression - uterine or internal iliac artery ligation - hysterectomy RADIOLOGICAL - arterial embolisiation - balloon occlusion of iliac vessels (needs to stable enough for potentially long XR procedure) MEDICAL - keep anaesthetic vapour concentration down - ergometrine - oxytocin - carboprost (PGF2-alpha) HAEMATOLOGICAL - correct coagulopathy - Factor VIIa - Transeamic acid - cell salvage |
|
|
What do you tell the obstetricians in the case of a dural tap |
normal delivery providing the second stage in not prolonged (previously used to avoid active second stage and deliver with forceps, but this does not reduce incidence of headache) |
|
|
When to give left lat tilt in pregnant lady |
20week |
|
|
When does reflux become an issue in pregnancy |
14-16 week |
|
|
When does epidural abscess develop? |
>4days |
|
|
Risk factors for epidural abscess? |
1. Immunocompromised - DM, immunosuppressant, HIV
2. Source of infection - distant source, haematological spread
3. Disrupted spinal column - spinal surgery
4. Difficult insertion
5. Disordered clotting - anti-platelet or coagulants
6. Prolonged insertion of catheter |
|
|
Cause of neurological deficit in epidural haematoma |
1. Direct compression 2. Leptomeningeal thrombosis 3. Spinal artery compression |
|
|
When to declare major obstetric haemorrhage |
1. Haemorrhagic shock 2. EBL >1.5 L 3. Coagulapathy on bloods/ clinical 4. 4u RBC transfused and more expected
AND patient still bleeding |
|
|
MAGPIE trial |
magnesium effective in reducing risk of seizures. should be continue 24hr post-delivery or 24hr after last seizure whichever is later |
|
|
Magnesium in preeclampsia |
- first live Rx of prophylactic seizure prevention and treatment. - 4g over 5-10 min then infusion 1-2g/hr (2g bolus if already on Mg infusion) - collaborative eclampsia trial showed Mg superior to phenytoin or diazepam - therapeutic level 2-3.5 mmol/L - 1g Mg = 4mmol |
|
|
symptoms and sings of hypermagnesimia |
> 5mmol/L --> decr patella reflex (first sign) > 6mmol/L --> resp depression 6.3-7.1 --> resp arrest 12+ --> cardiac arrest other symptoms: N/V, flushing, slurred speech |
|
|
Defn of anaemia in pregnancy |
<10.5 g/dL |
|
|
Painless vs painful APH obs |
Painless - placenta preveia Painful - placental abruption |
|
|
what are the causes and how do you stop major causes of obstetric bleeding |
1. TONE - pharm: oxytocin, ergometrine, misoprostol, prostaglandin F2-alpha - physical: uterine compression 2. TISSUE: - retained products of conception 3. TRAUMA - examination under anaesthesia and repair 4. THROMBIN - coagulopathy Mx 5. THEATRE - intrauterine tamponade - Bakeri balloon - arterial ligation - B-lynch suture - arterial embolism - hysterectomy 6. GENERAL: - warm - IV Fluid/ RBC/ FFP - avoid excess colloid - cell salvage |
|
|
What are the stages of labour |
1. first stage - cervical dilatation to 10cm 2. second stage - cervical dilatation to 10cm to delivery of baby 3. Third stage - after delivery of baby to delivery of placenta |
|
|
incidence of placenta accreta in those with placenta previa + prv LSCS |
1x LSCS = 1:200 2x LSCS 50% 2/3 with accreta need hysterectomy |
|
|
effect of epidural on labour outcomes |
1. superior analgesia (but NOT greater maternal satisfaction) 2. NO - incr LSCS, instrumental delivery, change fetal outcomes 3. Incr: - labour duration - oxytocin use - pyrexia --> Ix and Rx of mum and bub |
|
|
what is chorioamnioitis |
Defn: bacterial infection fetal amniotic chorion membrane Dx require 2+ of: 1. fever > 37.8 2. WCC >18 3. mum tachycardia >120 4. fetal tachycardia >160-180 5. purulent/ smelly amniotic fluid/ vaginal discharge 6. uterine tenderness |
|
|
Normal fetal HR variablity |
5-15bpm |
|
|
fetal accelerations |
normal and reassuring |
|
|
abnormal features of CTG |
1. baseline FHR outside 110-160 2. baseline variability <5bpm 3. reduce/ absent acceleration 4. deceleration |
|
|
causes of baseline fetal brady |
1. cord compression and acute fetal hypoxia 2. post maturity >40week gestation 3. congenital heart abnormality |
|
|
causes of fetal tachy |
1. excess fetal movement/ uterine stimulation 2. Maternal stress/ anxiety 3. material pyrexia 4. fetal infection 5. chronic hypoxia 6. prematurity <32week gestation |
|
|
causes of early deceleration |
fetal head compression - not pathological decal start with contraction and improve to baseline by end of contraction "mirror image of uterine trace" |
|
|
late deceleration defn |
start with peak of contraction and peak after uterine contraction. defined when peak occur > 15 sec after peak in uterine contraction |
|
|
causes of late deceleration |
1. hypoxia 2. placental abruption 3. cord compression/ prolapse 4. excess uterine activity 5. maternal hypotension/ hypovolaemia |
|
|
variable deceleration definition |
variable FHR decal in time and size may be accompanied by incr variability of fetal HR |
|
|
cause of variable decal |
1. compression of umbilical cord. ?fetal hypoxia |
|
|
prolonged decal/ brady |
decr FHR >30bpm for >2min |
|
|
cause of prolonged decel/ brady |
1. maternal hypotension 2. umbilical cord compression 3. uterine hypertonia |
|
|
mnemonic for improving intra-uterine fetal oxygenation before delivery |
SPOILT Syntocinon off Position full left lateral Oxygen IV infusion of crystalloid Low BP - if present IV vasopressor Tocolysis - terbutaline 250mcg (B2-agonist) or GTN (2x 400mcg puffs sublingual) |

