![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
180 Cards in this Set
- Front
- Back
|
Umbilical vessels
|
2 Arteries
1 Vein 1/3 of babies with a single uterine artery will have another anomaly. |
|
|
What is the placenta
|
Discoid mass composed of fetal (chorion frondosum) and maternal (decidua basalis) tissues divided by fissures into cotelydones (lobules) on the uterine side.
|
|
|
Pregnancy history of a woman (acronym)
|
GTPAL (GTPAV in french)
G : gravidity (twins = 1 pregnancy) T : Term infants A : Abortions P : Premature infants L : number of living infants |
|
|
Trimesters
|
T1 : 0-12 weeks
T2 : 12-28 weeks T3 : 28-40 weeks |
|
|
Physical signs of pregnancy
|
Goodell's sign : softening of the cervix (4-6 weeks)
Chadwick's sign : bluish discoloration of the cervix and vagina due to pelvic vasculature engorgement (6 weeks) Hegar's sign : softening of the cervical isthmus (6-8 weeks) Uterine enlargment |
|
|
Goodell's sign
|
softening of the cervix (4-6 weeks)
|
|
|
Chadwick's sign
|
bluish discoloration of the cervix and vagina due to pelvic vasculature engorgement (6 weeks)
|
|
|
Hegar's sign
|
softening of the cervical isthmus (6-8 weeks)
|
|
|
Investigations for pregnancy
|
B-HCG
- Peptide hormone composed of alpha and beta subunits produced by placental trophoblastic cells (maintains the corpus luteum during pregnancy) - Positive in serum 9 days post-conception, positive in urine 28 days after last menstrual period - Plasma levels double every 1-2 days, peak at 8-10 weeks, then fall to a plateau until delivery + Levels less than expected by dates suggest ectopic pregnancy, abortion or wrong date + Levels higher than expected suggest multiple gestation, mole, trisomy 21 or wrong dates U/S - Transvaginal 5 weeks : gestational sac visible (b-hcg >1200-1500) 6 weeks : fetal pole seen 7-8 weeks : fetal heart tones visible - Transabdominal 6-8 weeks : intrauterine pregnancy visible (b-hcg > 6500) |
|
|
B-Hcg rule of 10's
|
10 IU at time of misses menses
100 000 IU at 10 weeks 10 000 IU at term |
|
|
Physiologic skin changes in pregnancy
|
- Increased pigmentation of perineum and areola
- Chloasma : pigmentation under eyes and on bridge of nose - Linea nigra : midline abdominal pigmentation - Hyperestrogenism : spider angioma, palmar erythema - Striae gravidarum due to connective tissue changes |
|
|
Physiologic cardiovascular changes in pregnancy
|
- Hyperdynamic circulation
- Increased CO, HR and blood volume - Decreased BP due to decreased PVR - Enlarging uterus compresses IVC and pelvic veins - Decreased venous return leads to risk of hypotension - Increased venous pressure leads to risk of varicose veins, hemorrhoids leg edema |
|
|
Physiologic hematologic changes in pregnancy
|
- Hemodilution causes physiologic anemia and apparent decrease in Hb and Hte
- Increased leucocyte count but impaired function leads to improvement in autoimmune disease - Gestational thrombocytopenia : mild and asymptomatic (platelets > 70 000), normalizes within 2-12 weeks following delivery - Hypercoagulable state : increased risk of DVT and PE but also decreased bleeding at delivery - Resetting of the osmostat under the influence of beta-hcg leads to non pathological hyponatremia in pregnancy |
|
|
Physiologic respiratory changes in pregnancy
|
- Increased incidence of nasal congestion and epistaxis
- Increased O2 consumption to meet increased metabolic requirements - Elevated diaphragm i.e. patient appears more "barrel-chested" - Increased minute ventilation leads to decreased CO2 with a resulting mild respiratory alkalosis that helps CO2 diffuse across the placenta and be eliminated from the fetus - No change in VC and FEV1 - Decreased TLC, FRC and RV |
|
|
Physiologic GI changes in pregnancy
|
- GERD due to increased intra-abdominal pressure and progesterone (causing decreased sphincter tone and delayed gastric emptying)
- Increased gallstones due to progesterone causing inreased gallbladder stasis - Constipation and hemorrhoids due to progesterone causing decreased GI motility - Atypical appendicitis presentation due to displacement of appendix |
|
|
Physiologic GU changes in pregnancy
|
- Increased urinary frequency due to increased total urinary output
- Increased incidence of UTI and pyelonephritis due to urinary stasis - Glycosuria can be physiologic, must test for gestational diabetes mellitus - Ureters and renal pelvis dilation due to progesterone induced smooth muscle relaxation and uterine enlargement - Increased CO and thus increased GFR leads to decreased creatinine (normal in pregnancy : 35-44 mmol/L), uric acid and BUN. |
|
|
Physiologic neurologic changes in pregnancy
|
Increased incidence of carpal tunnel syndrome and Bell's palsy
|
|
|
Physiologic endocrine changes in pregnancy
|
Thyroid : moderate enlargement and increased basal metabolism
- increased total thyroxine and TBG - free thyroxine index and TSH levels are normal Adrenal : maternal cortisol rises throughout pregnancy (total and free) Calcium : decreased total maternal Ca due to decreased albumin - free ionized calcium proportion remains the same due to PTH - increased bone turnover but no loss of bone density because estrogen inhibits resorption |
|
|
Foods rich in folic acid
|
Spinach
Lentils Chick peas, asparagus, broccoli, peas, Brussels sprouts, corn and oranges |
|
|
Folic acid supplementation
|
Encourage acid folic supplementation 8-12 weeks preconception to prevent neural tube defects
- 0.4 to 1 mg in all women - 5 mg if past neural tube defect, anti-epileptic medication, diabetes mellitus or BMI > 35 Continue for first trimester of pregnancy |
|
|
When to give 5 mg of folic acid supplementation
|
8-12 weeks preconception to women with :
- past NTD - anti-epileptic medication - diabetes mellitus - BMI > 35 |
|
|
Neagle's Rule
|
1st day of LMP + 7 days - 3 months
|
|
|
Initial prenatal visit
- when - what |
Physical exam
- complete exam to obtain baseline - BP and weight important for interpreting subsequent changes - Pelvic exam Investigations - bloodwork : CBC, blood group and type, Rh antibodies, infection screening as per preconception counselling - Urine R&M, C&S : bacteriuria and proteinuria - Pelvic exam + Pap smear, culture for N. gonorrhea and C. Trachomatis + Bacterial vaginosis swab Verify in gynecology book or uptodate |
|
|
Contraindications to exercise in pregnancy (absolute and relative)
|
Absolute contraindications
- ruptured membranes - preterm labour - hypertensive disorders of pregnancy - incompetent cervix - IUGR - multiple gestation (>3) - Placenta previa after 28th week - Persistsent 2nd or 3rd trimester bleeding - Unontrolled type I diabetes - Thyroid disease - Other serious disease Relative contraindications - previous spontaneous abortion - previous preterm birth - mild/moderate cardiovascular or respiratory disorder - anemia <100 - malnutrition or eating disorders - |
|
|
Increase in caloric intake during each trimester
|
T1 : 100 cal/day
T2 : 300 cal/day T4 : 450 cal/day |
|
|
Nutritional advice during pregnancy
|
3-4 servings of milk products daily
daily caloric intake increase of 100 cal/d (T1) 300 cal/d (T2) 450 cal/d (T3) Daily multivitamins should be continued in T2 for women who do not consume an adequate diet - Iron is the only supplement for which requirements during pregnancy cannot be met by diet alone Nutrients important during pregnancy - Folate : 0.4-5mg per day - Calcium : 1200-1500 mg per day - Vitamin D : 200 IU per day - Iron : 0.8 mg/d in T1 4-5 mg/d in T2 and > 6 mg/d in T3 - Essential fatty acids |
|
|
Weight gain in pregnancy
|
Optimal gain depends on pre-pregnancy weight
- BMI < 19 : 13-18 kgs - BMI 19-25 : 11-16 Kgs - BMI > 25 : 7 to 11 Kgs General rule : - 1-3.5 kg in T1, then 0.45 KG/week until delivery |
|
|
Sexual intercourse in pregnancy
|
May continue except in patients at risk for for abortion, preterm labour or placenta previa.
Breast stimulation may induce uterine activity and is discouraged in high risk patients near term. |
|
|
Uterine heights in pregnancy
|
12 weeks : pubic symphysis
16 weeks : mid-way umbilicus 20 weeks : umbilicus 1 cm each week afterwards |
|
|
Timing for prenatal visits
|
Q4-6 weeks until 28 weeks, Q2 weeks from 28 to 36 weeks and q weekly from 36 weeks until delivery
|
|
|
Leopold's maneuvers
|
First maneuver : to determine which fetal part is lying furthest away from the pelvic inlet
- palpate upper abdomen with both hands; the consistency, mobility and shape of the form palpated is noted - head : moves independently of the trunk, is round and firm - buttocks : moves with the trunk , is softer has bony processes Second maneuver : to determine the location of the fetal back - one hand remains steady on a side of the abdomen while the other hand palpates the other side - the fetal back will feel smooth, while the limbs will feel like protrusions Third maneuver (Pawlick's Grip) : to determine which fetal part is lying above the pelvic inlet - palpate the lower abdomen with thumb and fingers - should validate findings from the first maneuver Fourth maneuver : to locate the fetal brow - examiner faces patient's feet - brow is located on the side when there is greatest resistance when fingers are moved down the side of the uterus towards the symphysis pubis - fetal head flexed : brow and back on opposite side - fetal head extended : brow and back on the same side |
|
|
Differential diagnosis of decreased fetal movements
|
Death of fetus
Amniotic fluid decreased Sleep cycle of fetus Hunger / thirst Decreased fetal movements = <6 movements / 2 hours |
|
|
When are fetal movements first noticed?
|
18-20 weeks in primigravidas. Can occur 1-2 weeks earlier in multigravidas.
|
|
|
What is a non stress test?
|
Fetal heart rate tracing using an external Doppler to assess FHR and its relationship to fetal movement
|
|
|
Indication of non stress test
|
Any suggestion of uteroplacental insuffisiency or suspected fetal disease
|
|
|
Interpretation of non stress test
|
- Reassuring NST : at least 2 accelerations of FHR >15 BPM from the baseline lasting >15 s. in 20 min
- Non reassuring NST : < 2 accelerations in 40 min + If no observed accelerations or fetal movement in the first 20 minutes, stimulate fetus (fundal pressure, acoustic/vibratory stimulation) and continue monitoring for 30 minutes + if NST non reactive, then perform biophysical profile |
|
|
What is a biophysical profile?
- Indications - Interpretation - Soring |
It consists of a 30 minutes U/S assessment of the fetus +/- NST
BPP is the best choice for : - non reassuring NST - post-term pregnancy - decreased fetal movement - any other suggestion of fetal distress or uteroplacental insuffisiency Scoring of BPP 1) Amniotic fluid volume + fluid pocket of 2 cm in 2 axes : 2 points + oligohydramnios : 0 points 2) Breathing + at least one episode of breathing lasting at least 30 seconds : 2 points + no breathing : 0 points 3) Limb movement + Three discrete movements : 2 points + two or less : 0 points 4) Fetal tone + At least one episode of limb extension followed by flexion : 2 points + no movement : 0 points Interpretation - 8 points : perinatal mortality rate 1:1000, repeat BPP as clinically indicated - 6 points : perinatal mortality rate 31:1000, repeat BPP in 24 hours - 0-4 points : perinatal mortality rate 200:1000; deliver fetus if benefits of delivery > risks |
|
|
Differential diagnosis of increased maternal serum AFP
|
Incorrect GA
> 1 fetus Fetal demise oNTD Abdominal wall defects (e.g. omphalocele) |
|
|
Differential diagnosis of decreased maternal serum AFP
|
Incorrect GA
Gestational trophoblastic neoplasia Missed abortion Chromosomal anomalies Maternal DMI/DMII |
|
|
First trimester screening (FTS)
|
11-14 weeks
Measures - Nuchal translucency on U/S - Beta-Hcg - Pregnancy associated plasma protein A (PAPP-A) Risk estimate for : - Down syndrome : increased NT, increased AFP, decreased PAPP-A Useful where patient wants results within the first trimester More accurate estimate of Down syndrome risk than MSS, (Sn 85%) 5% false positive rate Patients with positive screen should be offered CVS or amniocentesis |
|
|
Maternal serum screening (MSS)
|
15-18 weeks
Measures - Maternal serum AFP - Beta-Hcg - Unconjugated estrogen (estriol or uE3) Risk estimate for : - Open neural tube defect (oNTD) : increased MSAFP - Trisomy 21 : decreased MSAFP, increased B-HCG, decreased uE3 - Trisomy 18 : decreased MSAFP, decreased B-HCG, decreased uE3 Only offered alone if patient missed the time window for IPS or FTS 8% of baseline false positive rate for t21, lower for oNTD and t18 Patients with positive screen should be offered U/S or amniocentesis. |
|
|
Integrated Prenatal Screenin (IPS)
|
Nuchal translucency on 12 week U/S
FTS at 11-14 weeks MSS + inhibin A at 15-18 weeks Risk estimate for oNTD, T21, T18 Sn 85-90% 2% False positive rate Patients with positive screen should be offered U/S and/or amniocentesis |
|
|
Sensitization routes for Rh negative mothers
|
- Incompatible blood transfusions
- Previous fetal-maternal transplacental hemorrhage - Invasive procedures in pregnancy - Any type of abortion - Labour and delivery |
|
|
Overall risk of isoimmunization of an Rh negative mother
|
16% in total
- 2% antepartum - 7% within 6 months of delivery - 7% in the second pregnancy |
|
|
Investigations for Rh isoimmunization
|
Routine screening at first visit for blood group, Rh status and antibodies are measured by the indirect Coombs test.
If Rh Positive with antibodies present, the severity of fetal anemia is determined primarily by antibody concentration - Ab titres <1:16 considered benign - Ab titres >1:16 necessitates amniocentesis to determine severity of fetal anemia (which correlates with the amount of biliary pigment in amniotic fluid from 27 weeks +) ** A positive titre means that the fetus is at risk of hemolytic anemia, not that it has occured or will developp **** Kleihauer-Betke test used to determine extent of fetomaternal hemorrhage Detailed U/S for hydrops fetalis |
|
|
Rh negative mother prophylaxis
|
Exogenous Rh IgG (RhoGam or WinRho) binds to Rh Ag of fetal cells and prevents it from contacting maternal immune system.
RhoGam given to all Rh negative women in the following scenarios : - routinely at 28 weeks GA (provides protection for 12 weeks) - within 72 hours of the birth of an Rh positive fetus - with a positive Kleihauer-Betke test - with any invasive procedure in pregnancy - in ectopic pregnancy - with miscarriage or therapeutic abortion (only 50 ug requried) - with an antepartum hemorrhage) If mother Rh negative and Ab screen positive, follow mother monthly Ab titres throughout pregnancy +/- serial amniocentesis as needed (RhoGam has no benefits) |
|
|
Risk factors for neural tube defects
|
Genetics
- family history of NTD - cosanguinity - chromosomal (t13, t18, t21) Race - Caucasians > africans Insufficient vitamins : zinc and folate Maternal chronic disease : diabetes Maternal use of antiepileptic drugs |
|
|
Hydrops fetalis definition and classification
|
Abnormal edema in 2 or more fetal compartments
- ascites - pericardial effusion Classified as immune (isoimmunization) or non immune (caused by many different end-stage fetal diseases) |
|
|
Complications of isoimmunization
|
Hemolytic anemia
Erythroblastosis fetalis Hydrops fetalis |
|
|
Group B streptococcus screen
- risk factors - clinical features - investigations - treatment |
15-40% vaginal carrier state
Risk factors - GBS bacteriuria during current pregnancy - previous infant with invasive GBS infection ++++++++ - preterm labour < 37 weeks - amniotic membrane rupture > 18 hours - intrapartum maternal termperature > 38 ++++++++++ - positive GBS screen during current pregnancy Clinical features - not harmful to mother - danger of vertical transmission (neonatal sepsis, meningitis or pneumonia) Investigations - screening of all women at 35-37 weeks with vaginal and anorectal swabs for C&S Treatment - Indications for ATB prophylaxis : positive GBS screen or GBS status unknown + 1 RF - ATB for GBS prophylaxis (at least 4 hours pre delivery) + Penicillin G 5 million U IV then 2.5 million U IV Q4H until delivery + PCN allergic but not at risk of anaphylaxis - cefazolin 2 g IV then 1 g Q8H + PCN allergic and at risk of anaphylaxis - Clindamycine 900 mg IV Q8H or erythromycin 500 mg IV Q6H - If fever, broad spectrum ATB indicated |
|
|
Indications for chromosomal screening
|
Maternal age > 35
Risk factors in current pregnancy - teratogen exposure - abnormal U/S - abnormal prenatal screen (FTS, MSS, IPS) Past history / family history of : - previous pregnancy with chromosomal anomaly or genetic disease - either parent a know carrier of genetic disorder or balanced translocation - family history of chromosomal anomaly, genetic disorder, birth defect or undiagnosed mental retardation - cosanguinity - three or more spontaneous abortions |
|
|
Indications for amniocentesis
|
Identification of genetic anomalies (as per chromosomal screening indications)
Assessment of fetal lung maturity (T3) via the L/S ratio (Lecithin:sphingomyelin ratio) + if >2:1, respiratory distress syndrome is less likely to occur Assessment of amniotic fluid bilirubin concentration in Rh isoimmunized pregnancies |
|
|
Advantages and disadvantages of amniocentesis
|
Advantages
- also screens for oNTD (acetylcholinesterase and amniotic AFP) 96% accurate - in women > 35 years old, the risk of chromosomal anomaly (1:180) is greater than the increased risk of miscarriage from the procedure - more accurate genetic testing than CVS Disadvantages - 0.5% risk of spontaneous abortion and risk of fetal limb injury - results take up to 14-28 days |
|
|
Chorionic Villus Sampling
- Procedure - Advantages - Disadvantages |
Biopsy of fetal derived chorion using a trans-abdominal needle or trans-cervical catheter at 10-12 weeks
Advantages - enables pregnancy to be terminated earlier than with amniocentesis - rapid karyotyping and biochemical assay within 48 hours, including FISH analysis - high sensitivity and specificity Disadvantages - 1-2% risk of spontaneous abortion and risk of fetal limb injury - does not screen for neural tube defects - 1-2% incidence of genetic mosaicism (false negative rates) |
|
|
How much iron is needed during pregnancy?
|
Mother needs 1 g of elemental iron per fetus, this amount exceeds normal stores + dietary intake
|
|
|
Etiology of iron deficient anemia in pregnancy
|
Inadequate iron intake
Decreased iron absorption (malabsorption syndrome, antacid use) Increased losses (vaginal bleeding, other source of bleeding) Increased requirement (fetal growth, multiple gestation) |
|
|
Complications of iron deficient anemia in pregnancy
|
Mother : angina, CHF, infection, slower recuperation, preterm labour
Fetal : decreased oxygen carrying capacity leading to fetal distress, IUGR, low birth weight and hydrops fetalis |
|
|
Management of iron deficient anemia in pregnancy
|
Prevention
- 150 mg ferrous sulfate OD for all pregnant women in T2 and T3 If anemic - 1 g ferrous sulfate OD |
|
|
Complications of low folate during pregnancy
|
Neural tube defects
|
|
|
Epidemiology of folate deficiency anemia
|
Often associated with iron deficiency anemia.
Incidence varies with 0.5-2.5% depending on region, population, diet. |
|
|
Prevention of folate deficiency anemia
|
Prevention
- 0.4-1 mg folic acid PO daily for 1-3 months preconceptually and throughout T1 - 5 mg folic acid per day with past history of oNTD |
|
|
Screening for gestational diabetes
|
28 weeks with O'Sullivan test
|
|
|
Risk factors for developing gestational diabetes
|
Age > 25
Obesity Family history of DM Previous history of GDM Previous child with birthweight >4.0 kg Certain ethnicities (aboriginal, hispanic, asian, african) |
|
|
Management of pre-existing diabetes in pregnancy
1. Pre-counselling 2. Pregnancy 3. Labour 4. Post-partum |
1. Preconception
- Pre-plan and refer to high risk clinic - Optimize glycemic control - Counsel patient : potential risks and complications - Evaluate for diabetic retinopathy, neuropathy, coronary artery disease 2. Pregnancy - If already on medication, generally switch to insulin therapy; continuing glyburide or metformin controverial + Other oral hypoglycemiants are not studied - Tight glycemic control + Diet management first line therapy + If blood glucose not well controlled, initiate insulin therapy + Insulin dosage may need to be adjusted in T2 due to increased demand and increased insulin resistance - Monitor as for normal pregnancy plus initial 24 hour urine protein and creatinine clearance, retinal exam, HbA1C + if HbA1C > 140% of prepregnancy value associated with increased risk of spontaneous abortion and congenital malformations - Increased fetal surveillance 3. Labour - must consider size of baby for time of delivery - can wait for spontaneous labour if glucose well controlled and BPP normal - Induce by 40 weeks - Type of delivery + increased risk of cephalopelvic disproportion (CPD) and shoulder dystocia with babies > 4000 g + elective C/S for predicted birth weight > 4500 g (controversial) - Monitoring + during labour, monitor blood sugars Q1H with patient on insulin and dextrose drip + aim for blood sugar between 3.5 to 6.5 mmol/L to reduce the risk of neonatal hypoglycemia 4. Postpartum - Insulin requirements dramatically drop with the expulsion of placenta - No insulin is required for 48-72 hours postpartum in most type I DM - Monitor glucose Q6H, restart insulin at 2/3 prepregnancy dosage when glucose > 8 mmol/L |
|
|
Target blood values in pregnancy
|
Fasting blood glucose <5.3
1 hour post-prandial blood glucose <7.8 2 hour post-prandial blood glucose <6.7 |
|
|
Screening for gestational diabetes mellitus
|
- At 24-28 weeks
- Pregnant females age > 25 or age <25 with 1 risk factor - 1 hour, 50 g OGTT + Plasma glucose < 7.8 mmol/L = no GDM + PG >7.8 and <10.3 = 2 hours OGTT + PG > 10.3 = GDM established - Impaired glucose tolerance if + FPG >5.3 mmol/L + PG 1 hour, 75 g OGTT >10.6 + PG 2 hour, 75 OGTT > 8.9 |
|
|
Management of gestational diabetes
|
- Treat both GDM and IGT
- Tight glycemic control optimal as in type 1 and type 2 DM - Monitoring and timing for delivery as for type 1 and type 2 DM - Stop insulin and diabetic diet postpartum - Follow-up with 2 hour, 75 g OGTT 6 weeks-6months postpartum |
|
|
Maternal complications of DM in pregnancy
|
Obstetric
- HTN/Pre-eclampsia (insulin resistance is implicated in etiology of HTN) - Polyhydramnios (maternal hyperglycemia leads to fetal hyperglycemia which leads to fetal polyuria) Diabetic emergencies - Hypoglycemia - DKA - Diabetic coma End organ involvement (DM1&2 not GDM) - Retinopathy - Nephropathy Other - Pyelonephritis/UTI (glycosuria provides a culture medium for E. Coli) - Increased incidence of spontaneous abortions (in DM1, DM2 not GDM) |
|
|
Fetal complications of DM in pregnancy
|
Growth
- Macrosomia (hyperinsulinism) - IUGR (due to placental vascular insufficiency) Delayed organ maturity - Fetal lung immaturity (hyperglycemia interferes with surfactant synthesis RDS) Congenital anomalies (DM1, DM2 not GDM) - 2-7x increased risk of cardiac, NTD, GU(cystic kidneys), GI (anal atresia) and MSK ***** Pregnancies complicated by GDM do not manifest an increased risk of congenital anomalies because GDM develops after the critical period of organogenesis ****** Labour and delivery - Preterm labour (mostly in patient associated with HTN/Pre-eclampsia) - Birth trauma (due to macrosomia) - Increased incidence of stillbirth Neonatal - Hypoglycemia (due to pancreatic hyperplasia and excess insulin secretion in the neonate) - Hyperbilirubinemia and jaundice - Hypocalcemia - Polycythemia |
|
|
Classification of hypertensive disorders of pregnancy
- Pre-existing hypertension - Gestational hypertension - Pre-existing hypertension + Pre-eclampsia - Severe pre-eclmapisa |
1. Pre-existing HTN
- diastolic hypertension that predates pregnancy or is diagnosed before 20 weelks gestation. In most cases HTN persists >42 d postpartum. It may be associated with proteinuria 2. Gestational hypertension - Diastolic hypertension develops after 20 weeks gestation. In most cases it resolves < 42 days postpartum A. Without pre-eclampsia : < 0.3g/d B. With pre-eclampsia i. with new onset proteinuria ii. with one or more adverse conditions 3. Pre-existing HTN + pre-eclampsia : HTN associated with one of the following after 20 weeks: - Resistant hypertension - New or worsening proteinuria - One or more adverse conditions 4. Severe Pre-Eclampsia - Onset before 34 weeks gestation - Heavy proteinuria (3-5 g/d in 24 hr urine) Or with one or more adverse conditions |
|
|
Adverse conditions in pregnancy
|
1. Convlusions (eclampsia)
2. Very high diastolic pressure (>100 mm Hg) 3. Thrombocytopenia (<100 000) = bleeding, petechiae 4. Oliguria (<500 mL/d) 5. Pulmonary edema 6. Elefated liver function tests 7. Severe nausea and vomiting 8. Frontal headache 9. Visual disturbance (blurring, scotoma) 10. Persistent abdominal pain in RUQ 11. Chest pain or shortness of breath 12. Suspected placenta abruptio 13. HELLP syndrome 14. IUGR 15. Oligohydramnios 16. Absent or reversed umbilical artery end diastolic flow as determined by doppler velocitometer 17. CNS = hyperreflexia, somnolence, irritability, tremulousness |
|
|
Definition of pre-existing HTN in pregnancy
|
HTN (>140/90) prior to 20 weeks GA (unless a gestational trophoblastic neoplasia), persisting postpartum
|
|
|
Management of pre-existing HTN in pregnant women
|
Alpha Methyldopa 250-500 mg PO tid/qid or labetalol 100-300 mg PO bid/tid
NO ACEI, DIURETICS or PROPRANOLOL Monitor progress with serial U/S |
|
|
Etiology and pathophysiology of gestational hypertension
|
- Imbalance of thromboxane (vasoconstrictor) and prostaglandin (vasodilator), arteriolar constriction, capillary damage, protein extravasation and hemorrhage.
- In patients with trophoblastic diseases (mole, hydrops, choriocarcinoma), occurs earlier than 20 GA, otherwise occurs after 20 weeks |
|
|
Risk factors for gestational hypertension
|
Maternal factors
- Primigravida - First conception with a new partner - PMHx or FHx of gestational HTN - DM, chronic HTN or renal insuffisiency - Antiphospholipd antibody syndrome - Extremes of maternal age (<18 and >35) Fetal factors - IUGR or oligohydramnios, GTN, multiple gestation, fetal hydrops |
|
|
Pre-eclampsia investigations
|
CBC
Creatinine, Electrolytes, Urinalysis or urine dipstick AST/ALT LDH INR, aTTP |
|
|
HELLP syndrome
|
Hemolysis
Elevated liver enzymes Low platelets |
|
|
Management of gestational hypertension
|
Without Pre-eclampsia
- Bed rest + left lateral decubitus position, normal salt and protein intake - Avoid diuretics and anti-hypertensives - Monitor for progression - If > 37 weeks With Pre-eclampsia - Verify if HELLP present - Stabilize and deliver : only cure is delivery - Increased maternal monitoring to hourly input and output, urine dip Q12H and neurological vitals Q1H - Increased fetal evaluation - Anticonvulsant therapy + Mg Sulfate : 4 g IV bolus over 20 minutes followed by 2-4 g/hour + Monitor for signs of Mg toxicity (give calcium gluconate = antagonist) - Anti-hypertensive therapy + Hydralazine 5-10 mg IV bolus over 5 minutes Q15-30 minutes as necessary + Labetolol 20-50 mg IV Q10 minutes 2nd line : nifedipine 10-20 mg PO Q20-60 minutes - Post-partum management + Risk of seizure highest in first 24 hours postpartum, thus continue Mg Sulfate for 12-24 hours + Vitals Q1H + Consider HELLP syndrome in toxic patients + Must return to a normotensive BP within 2 weeks |
|
|
Signs of Mg toxicity
|
Depressed deep tendon reflexes
Decreased RR Anuria Hypotonia CNS or cardiac depression |
|
|
Complications of gestational hypertension
|
Maternal
- Hemorrhagic stroke (50% of deaths) - Left ventricular failure / pulmonary edema - Liver and renal dysfunction - Abruption - Seizure - DIC (release of placental thromboplastin = consumptive coagulopathy) - HELLP syndrome + treat with FFP infusion or plasma exchange Fetal - Fetal loss - IUGR - Prematurity - Placenta abruptio |
|
|
Definition of hyperemesis gravidarum
|
Intractable nausea and vomiting, severe enough to cause weight loss, dehydration, ketonuria, electrolyte imbalance, acid-base disturbances and if severe, hepatic and renal damage.
Usually presents in T1 then diminishes; persists throughout pregnancy in a minority 1% of pregnancies |
|
|
Etiology of hyperemesus gravidarum
|
Rapidly rising B-HCG and estrogen levels
|
|
|
Investigations for hyperemesis gravidarum
|
Diagnosis of exclusion : r/o GI inflammation, pyelonephritis, thyrotoxicosis
Multiple gestation, GTN, HELLP syndrome CBC, electrolytes, BUN, creatinine, LFTs, Urinalysis U/S |
|
|
Management of Hyperemesis gravidarum
|
Supportive
- if severe, admit - NPO initially, then small frequent meals of appealing foods - Correct hypovolemia, electrolye imbalances and ketosis - Thiamine supplementation may be indicated - TPN if severe to reverse catabolic state Pharmacological Options - Diclectin (10 mg doxylamine succinate with vitamin B6) can be started at 2 tablets QHS + 1 tablet Qam + 1 tablet qPM; dosage can be increased up to 8 tablets per day - Gravol can be safely used as an adjunct to Diclectin (1 suppository bid or 25 mg PO qid) Non pharmacological options - rest - avoid triggers - acupressure - ginger |
|
|
Complications of hyperemesis gravidarum
|
Maternal
- dehydration, electrolyte and acid-base imbalance - Mallory-Weiss tear - Wernicke's encephalopathy - Death Fetal - usually none - IUGR (15x more common in women losing >5% of pre-pregnancy weight) |
|
|
Differential diagnosis of jaundice in pregnancy
|
- Viral hepatitis
- Unique to pregnancy + Cholestatic jaundice of pregnancy + HELLP + Hepatic rupture, hematoma and infarct + Acute fatty liver of pregnancy (AFLP) + Hyperemesis gravidarum - Pre-existing conditions + chronic hepatitis, cirrhosis, familial hyperbilirubinemia, Budd-Chiari syndrome, Wilson's disease, hepatic tumours, intrahepatic cholestasis, biliary obstruction, PBC, PSC. |
|
|
Causes of jaundice unique to pregnancy
|
Cholestatic jaundice of pregnancy
Acute fatty liver of pregnancy HELLP Acutre hepatic rupture, hematoma and infarct Hyperemesis gravidarum |
|
|
Presentation of HELLP syndrome
|
Epigastric, RUQ or chest pain, N/V, symptoms of pre-eclampsia (headahce, blurred vision, thirst) with or without jaundice
Atypical presentation : asymptomatic reduction in platelet count, "flu-like symptoms" |
|
|
Laboratory findings and investigations for HELLP syndrome
|
High AST
Hyperbilirubinemia Thrombocytopenia Elevated LDH Liver biopsy : rarely done = periportal hemorrhage and fibrin deposition with periportal necrosis DDX : ITP, PTT, APLA, AFLP |
|
|
Management of HELLP
|
Supportive (ICU) and prompt delivery
|
|
|
Complications of HELLP
|
Sepsis
Multi-system organ failure Hepatic failure DIC Death |
|
|
Definition of cholestatic jaundice of pregnancy
|
Clinical syndrome characterized by intense pruritus that precedes jaundice by 7-14 days
|
|
|
Risk associated with cholestatic jaundice of pregnancy
|
Risk of reduced vitamin K absorption = increased risk of newborn hemorrhagic disease
|
|
|
Epidemiology of cholestatic jaundice of pregnancy
|
17-29 weeks GA
High incidence in Chile and Scandinavia Selenium may be preventive against cholestasis Strong familial predisposition Correlates with oral contraceptive sensitivity Episode predisposes to cholestasis on subsequent gestation |
|
|
Presentation of cholestatic jaundice of pregnancy
|
Intense pruritus (classically worst on palms and soles of feet) +/- icterus (1-2 weeks later)
ALT <500, ALP and GGT markedly elevated Steatorrhea unusual |
|
|
Management of cholestatic jaundice of pregnancy
|
- Ursodeoxycholic acid (20-25 mg/kg/day)
- Pruritus : cholestyramine - Prophylactic vitamin K before delivery - Consider induction of labour |
|
|
Hepatic infarct, hematoma and rupture
- Presentation - Diagnosis - Management - Complications |
A rare consequence of pre-eclampsia typically occuring in T3
- Vasospasm induced hepatic infarction can lead to hematoma formation - Hematoma can rupture Presentation - Hepatic rupture : RUQ pain, abdominal distention, N/V and HTN followed by shock Diagnosis - Hemoperitoneum (paracentesis, U/S, CT, MRI showing ruptured liver) Complications - Death if untreated |
|
|
Etiology and epidemiology of UTI in pregnancy
|
Etiology
- Increased urinary stasis from mechanical and hormonal (progesterone) factors - Organisms include + GBS + Common organisms in UTI in non pregnant women Epidemiology - Most common medical complication of pregnancy - Asymptomatic bacteriuria in 2-7% of pregnant women depending on parity and socioeconomic factors N.B. Asymptomatic bacteriuria to be treated in pregnancy because of increased risk of progression to cystitis, pyelonephritis and probable increase risk of preterm labour. |
|
|
Features and investigations of UTI in pregnant women
|
Features
- may be asymptomatic - dysuria, urgency and frequency in cystitis - fever, flank pain, CVA tenderness in pyelonephritis Investigations - Urinalysis, Urine cultures - VCUG, cystoscope and renal function tests in recurrent infections |
|
|
Management of UTI in pregnancy
|
Uncomplicated UTI
- 1st line : Amoxicillin 250-500 mg PO Q8H x 7 days - alternatives : TMP-SMX (Septra) or nitrofurantoin - avoid sulfa drugs during last 6 weeks of pregnancy due to displacement of biliribun from albumin and increased kernicterus in newborn - follow with monthly urine cultures Pyelonephritis - hospitalization and IV antibiotics Prognosis - complications : acute cystitis, pyelonephritis and possible premature rupture of membranes - recurrence common |
|
|
Which antibiotic to avoid in last 6 weeks of pregnancy? and why?
|
Avoid sulfa drugs during last 6 weeks of pregnancy due to displacement of biliribun from albumin and increased kernicterus in newborn
|
|
|
Definition of acute fatty liver of pregnancy
|
A form of hepatic failure with coagulopathy and encephalopathy that is characterized by microvesicular fatty infiltrates in liver parenchyma
Usually in 3rd trimester |
|
|
Risk factors for acute fatty liver of pregnancy
|
Primigravidas
Male gestations (2.7x higher) Long chain acyl-CoA dehydrogenase deficiency with at least one allele for the G1528 mutation in either mother or fetus No recurrence with subsequent pregnancies |
|
|
Clinical features of acute fatty liver of pregnancy
|
Acute N/V + severe upper abdominal pain preceding jaundice
Confusion Pre-Eclampsia Pruritus Range in presentation - mild - fulminant : GI bleed, hepatic coma, renal failure and true hepatic failure |
|
|
Diagnosis of acute fatty liver of pregnancy
|
- Elevated PTT and low serum fibrinogen
- AST>ALT - Hypoglycemia - Pre-Eclampsia and HELLP features frequently present - Liver biopsy to establish diagnosis + microvesicular fatty infiltrates of the central zone hepatocytes + Oil Red O stain on frozen tissue + Electron microscopy - U/S, MRI, CT : not useful, but try if liver biopsy is not possible (CT is most helpful) |
|
|
Management and prognosis of acute fatty liver of pregnancy
|
Management
- Early diagnosis with prompt delivery followed by maximal supportive care + ABC, mechanical ventilation, transfusion of blood products + Hepatic encephalopathy treatment - Lactulose, catharsis + Treat hypoglycemia Prognosis - recovery begins with delivery - persistent or increasing hyperbilirubinemia and complications |
|
|
Risk factors for venous thromboembolism in pregnancy
|
Previous VTE
Hypercoagulability (Antiphospholipid, Protein C/S deficiency, V leiden...) Immobilization Age >35 Obesity Infection Shock / dehydration Vascular damage at delivery Stasis (compression by uterus) |
|
|
Management of VTE in pregnancy
|
- Warfarin is contraindicated in pregnancy due to its potential teratogenic effects
- Unfractionned heparin + bolus of 5000 IU followed by an infusion of 30 000 IU/24 hrs + measure the aPTT six hours after the bolus + maintain the aPTT at a therapeutic level (1.5-2 times normal) + repeat Q24H once therapeutic + HIT uncommon (3%) but serious complications - Compression stockings - Prophylaxis + women on long term anticoagulation : full therapeutic anticoagulation throughout pregnancy and for 6-12 weeks postpartum + women with a non-active PMHx of VTE : unfractionned heparin regimens suggested - Routine prophylaxis + insufficient evidence in pregnancy to recommend routine use of LMWH + current prophylaxis regimens for acquired thrombophilias, such as APLA syndrome, include the use of low dose ASA in conjunction with prophylactic heparin. |
|
|
Etiology of recurrent pregnancy loss
|
Mechanical : uterine anatomy, cervical incompetence
Autoimmune : antiphospholipid antibody syndrome, lupus anticoagulant Karyotype : both parents Endocrine : hypothyroidism, diabetes mellitus Maternal infection Environment : smoking, alcohol, drugs, radiation |
|
|
Differential diagnosis of first and second trimester bleeding
|
Physiological bleeding : spotting (due to implantation of placenta - reassure and check serial beta-hcg)
Spontaneous abortion Coagulopathy Abnormal pregnancy (ectopic, molar) Trauma Genital lesion (cervical polyp, neoplasms) Post-coital Investigations - B-HCG - U/S - CBC - Blood group and screen |
|
|
Types of spontaneous abortions and characteristics
|
1) Threatened
- Vaginal bleeding with or without cramping - Cervix closed and soft - U/S shows viable fetus - Tx : watch and wait, <5% go on to abort 2) Inevitable - Increased bleeding and cramps with or without rupture of membranes - Cervix closed until products start to expel, then external os opens - Tx : watch and wait; misoprostol (PGE1); D&C with or without oxytocin 3) Incomplete - Extremely heavy bleeding and cramps with or without passage of tissue - Cervix open - Tx : watch and wait; misoprostol; D&C +/- oxytocin 4) Complete - Bleeding and complete passage of sac and plancenta - Cervix open - Tx : no D&C - expectant management 5) Missed - No bleeding (fetal death in utero) - Cervix closed - U/S may show SGA - Tx : watch and wait; misoprostol; D&C +/- oxytocin 6) Septic - Contents of uterus infected (infrequent) - Tx : D&C + IV broad spectrum antibiotics |
|
|
Definition of recurrent abortions
|
3 or more consecutive spontaneous abortions
|
|
|
Definition of antepartum hemorrhage
|
Vaginal bleeding from 20 weeks to term
|
|
|
Differential diagnosis of antepartum hemorrhage
|
Bloody show (shedding of cervical mucous plug)
Placenta previa Abruptio placenta (most common pathological etiology in T3) Vasa previa Marginal sinus bleeding Cervical lesions (cervicitis, polyp, ectropion, cervical cancer) Post coital Trauma Uterine rupture Bleeding from bowel or bladder Placenta accreta Abnormal coagulation |
|
|
Definition of placenta previa
|
Abnormal location of the placenta near, partially or completely over the cervical os
Etiology : idiopathic |
|
|
Presentation of placenta previa
|
History
- Painless bright red vaginal bleeding (recurrent), may be minimized and cease spontaneously, but can become catastrophic - Mean onset of bleeding is 30 weeks, but onset depends on degrees of previa P/E - Uterus soft and non tender - Presenting part high or displaced Do NOT perform a vaginal exam until placenta previa has been ruled out by U/S |
|
|
Risk factors for placenta previa
|
History of placenta previa
Multiparity Increased maternal age Multiple gestation Uterine tumour Uterine scar due to previous abortion, C/S, D&C, myomectomy |
|
|
Classification of placenta previa
|
Total : placenta completely covers the internal os
Partial : placenta partially covers the internal os Marginal : within 2 cm of os but does not cover any part of os (causes potential risk of hemorrhage during cervical effacement and dilatation) Low lying placenta (not a previa) : placenta in lower segment but clear of os (can also bleed but usually in labour) |
|
|
Complications of placenta previa (Fetal, maternal
|
Fetal
- perinatal mortality low but still higher than with a normal pregnancy - permaturity (bleeding often dictates early C/S) - intra uterine hypoxia - fetal malpresentation - PPROM - risk of fetal blood loss from placenta, especially if incised during C/S Maternal - <1% maternal mortality - Hemorrhage and hypovolemic shock, anemia, ARF, pituitary necrosis (Sheehan) - Placenta Accreta - Hysterectomy |
|
|
Definition of placenta accreta
|
Placental tissue invades superficially into myometrium
|
|
|
Definition of placenta increta
|
Placental tissue invades deeply into myometrium
|
|
|
Definition of placenta pecreta
|
Placental tissue invades through the myometrium
|
|
|
Main diagnosis for placenta previa
|
U/S
REPEAT U/S throughout pregnancy |
|
|
Management of placenta previa
|
Goal : keep pregnancy intrauterine until the risk of delivery < risk of not delivering
- Stabilize and monitor + blood work - U/S assessment - RhoGam if mother Rh negative x Kleihauer-Betke test to determine extent of fetomaternal transfusion so that appropriate dose of rhogam can be given - GA < 37 weeks and minimal bleeding (expectant management) x admit to hospital x limited physical activity, no douches, enemas or sexual intercourse x consider corticosteroids for fetal lung maturity x delivery when fetus is mature or hemorrhage dictates - GA > 36 weeks, profuse bleeding or L/S ratio is >2:1 - deliver by C/S |
|
|
Clinical features of Abruptio Placentae
|
PAINFUL vaginal bleeding (sudden onset, constant, localized to lower back and uterus)
Uterine tenderness and contractions +/- fetal distress +/- fetal demise +/- bloody amniotic fluid |
|
|
Definition of abruptio placentae
|
Premature separation of a normally implanted placenta after 20 weeks gestation
|
|
|
Risk factors for abruptio placentae
|
Previous abruption
Maternal hypertension Cigarette smoking Multiparity Maternal age > 35 PPROM Rapid decompression of a distended uterus (polyhydramnios, multiple gestation) Uterine anomaly Trauma |
|
|
Complications of abruptio placenta
|
Fetal
- Perinatal mortality 25-60% - Prematurity - Intrauterine hypoxia Maternal - < 1% maternal mortality - DIC - ARF - Anemia - Hemorrhagic shock - Sheehan syndrome - Amniotic fluid embolus |
|
|
Classification of abruptio placenta
|
Total vs partial
- external / revealed / apparent : blood dissects downward toward cervix - internal / concealed : blood dissects upward toward fetus - most are mixed |
|
|
Grades of abruptio placenta
|
Graded according to :
- uterine irritability - maternal hemodynamics - maternal fibrinogen - fetal heart rate |
|
|
Investigations for placenta abruption
|
U/S not sensitive
Blood work and fetal heart rate |
|
|
Management of placenta abruptio
|
- Maternal stabilization (hemodynamically...)
- Electronic fetal monitoring - Maternal monitoring (vitals, urine output, blood loss, bloodwork (Hte, CB, PTT/PT, platelets, fibrinogen, FDP, type and cross match) - Blood products on hand - RhoGam if Rh negative x Kleihauer-Betke test may confirm abruption If GA > 36 weeks : stabilize and deliver If GA < 36 weeks - if mild, deliver when fetus is mature - otherwise deliver by C/S for any beginning in complications |
|
|
Definition of vasa previa
|
Unprotected fetal vessels pass over the cervical os; associated with velamentous insertion of cord into membranes of placenta or succenturiate lobe.
|
|
|
Presentation of VASA previa
|
PAINLESS vaginal bleeding and fetal distress (tachy and bradyarrhythmia)
50% perinatal mortality, increasing to 75% if membranes rupture (most infants die of exsanguination) |
|
|
Investigations for vasa previa
|
Apt test : NaOH mixed with the blood, can be done immediately to detemine the source
- fetal : supernatant turns pink - maternal : supernatant turns yellow Wright stain on blood smear and look for nucleated RBC (in cord, not maternal blood) |
|
|
Management of vasa previa
|
Emergency C/S
|
|
|
Definition of ectopic pregnancy
|
Embryo implants outside of the endometrial cavity
|
|
|
Common locations of ectopic pregnancies
|
Ampullary 78%
Isthmic 12% Fimbrial 5% Interstitial 2% Abdominal 2% Intramural Cervical Infundibular |
|
|
Etiology of ectopic pregnancy
|
50% due to damage of fallopian tube cilia from PID
Intrinsic abnormality of the fertilized ovum Conception late in cycle Transmigration of fertilized ovum to contralateral tube |
|
|
Risk factors of ectopic pregnancy
|
50% idiopathic
Older women of african descent Smoking Endometriosis IUD use (although decreased pregnancy rate, if pregnancy occurs there is increased risk of ectopic) History of PID (especially with C. Trachomatis) Salpingitis Infertility Clomiphene citrate use (for induction of ovulation) Previous procedures - any surgery on fallopian tube - abdominal surgery for ruptured appendix - IVF pregnancies following ovulation induction Structural - uterine leiomyomas - adhesions - abnormal uterine anatomy (T-shaped uterus) |
|
|
Presentation of ectopic pregnancy
|
Temperature > 38 degrees
Abdominal tenderness (90%) +/- rebound Bimanual examination - cervical motion and adnexal tenderness - palpable adnexal mass Other signs of pregnancy : Chadwick, Hegar, Goodell If ectopic pregnancy ruptures - acute abdomen with increasing pain - abdominal distention - symptoms of shock |
|
|
Investigations for ectopic pregnancy
|
BHCG
U/S Laparoscopy |
|
|
Treatment of ectopic pregnancy
|
Goals of treatment : be conservative (preserve tube if possible)
Surgical - Linear salpingostomy if tube salvageable - Salpingectomy if tube damaged or ectopic is ipsilateral recurrence - 15% risk od persistent trophoblast - is patient is Rh negative give WinRho - may require laparotomy Medical (MTX) - use 50 mg/m2 body surface area; given in single IM dose - this is 1/6 chemotherapy dose, therefore minimal side effects - follow B-HCG levels weekly until B-HCG is non detectable - success 67%, as many as 25% will require a 2nd dose - tubal patency following MTX treatment approaches 80% |
|
|
Prognosis of ectopic pregnancy
|
9% of maternal deaths
40-60% of patients will become pregnant again after surgery 10-20% will have subsequent ectopic gestation |
|
|
Treatment algorithm of ectopic pregnancy
|
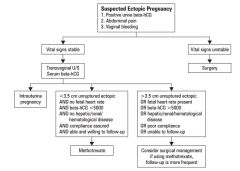
|
|
|
Complications associated with maternal gestation
|
Maternal
- Hyperemesis gravidarum - GDM - Gestational HTN - Anemia - Increased physiological stress on all systems - Increased compressive symptoms - C/S Utero-placental - Increased PROM/PTL - Polyhydramnios - Placenta Previa - Placental abruption - PPH (uterine atony) - Umbilical cord prolapse - Cord anomalies (velamentous insertion, 2 vessel cord) Fetal - Prematurity - IUGR - Malpresentation - Congenital anomalies - Twin-twin anomalies - Increased perinatal morbidity and mortality - Twin interlocking (twin A breech, twin B vertex) - Single fetal demise |
|
|
Management of twin pregnancies
|
- U/S determination of chorionicity must be done within the first trimester (ideally 8-12 weeks GA)
- Increased antenatal surveillance + NST weekly from 24 weeks GA + Serial U/S Q 2-3 weeks from 28 weeks GA to assess growth + Doppler flow studies weekly if discordant fetal growth + BPP as needed - Vaginal examination in 3rd trimester to check for cervical dilatation - May attempt vaginal delivery if twin A delivered vaginally and twin B delivered by C/S - Mode of delivery depends on fetal weight, GA, presentation |
|
|
Twin Twin transfusion syndrome
|
10% of monochorionic twins
Etiology - arterial blood from donor twin passes through placenta into vein of recipient twin Clinical features - donor twin : IUGR, hypovolemia, hypotension, anemia, oligohydramnios - recipient twin : hypervolemia, hypertension, CHF, polycythemia, edema, polyhydramnios, kernicterus in neonatal period |
|
|
Management of twin twin transfusion
|
Therapeutic serial amniocentesis to decompress polyhydramnios of recipient twin and decrease pressure in cavity and on placenta
Intrauterine blood transfusion to donor twin if necessary Laparoscopic occlusion of placental vessels |
|
|
Definition of IUGR
|
Infant weight <10th percentile for a particular GA
Weight not associated with any constitutional or familial causes |
|
|
Risk factors for IUGR
|
Maternal
- malnutrition - smoking - drug abuse - alcoholism - heart disease - type 1 DM - SLE - pulmonary insufficiency - previous IUGR Maternal-fetal - any disease causing placental insufficiency (GHTN, chronic HTN, CRF, gross placental morphological abnormalities) Fetal - TORCH - Multiple gestation - Congenital anomalies |
|
|
Classification and features of IUGR
|
Symmetric (type I(
- occurs early in pregnancy - inadequate growth of head and body - head : abdomen ratio may be normal - usually associated with congenital anomalies or TORCH infections Asymmetric (type II) - occurs late in pregnancy - brain is spared, therefore head:abdomen ratio increased - usually associated with placental insufficiency - more favorable prognosis than type I |
|
|
Complications of IUGR
|
Prone to meconium aspiration, asphyxia, polycythemia, hypoglycemia and mental retardation
Greater risk of perinatal morbidity and mortality |
|
|
Investigations for IUGR
|
- Symphysis-fundus height (SFH) measurements at every antepartum visit
- if mother at high risk or SFH lags >2cm behind GA + anatomy U/S exam should include assessment of biparietal diameter (BPD), head and abdomen circumference, femur length and fetal weight, amniotic fluid - BPP - Doppler analysis of umbilical cord blood flow as needed |
|
|
Differential diagnosis of incorrect uterine size for dates
|
Inaccurate dates
Maternal diabetes mellitus Polyhydramnios, oligohydramnios Multiple gestations Abnormal karyotype IUGR Fetal anomaly Abnormal lie |
|
|
Definition of macrosomia
|
Infant weight > 90th percentile for a particular GA or > 4000 g
|
|
|
Risk factors of macrosomia
|
Maternal diabetes
Maternal obesity Constitutional Past history of macrosomic infant |
|
|
U/S predictors of macrosomia
|
Polyhydramnios
Third trimester abdominal circumference (AC) >1.5 cm/week Head circumference (HC)/AC ratio <10th percentile Femur length (FL)/AC ratio <20th percentile |
|
|
Definition of polyhydramnios
|
Amniotic fluid volume (AFV) >2000 cc at any stage in pregnancy
U/S criteria L >8x8 cm pocket of amniotic fluid volume |
|
|
Etiology of polyhydramnios
|
Idiopathic
Maternal type 1 DM Maternal-fetal - chorioangiomas - multiple gestation - fetal hydrops Fetal - chromosomal anomaly (up to 2/3 of fetuses with severe polyhydramnios) - respiratory : cystic adenamatoid malformed lung) - CNS : anencephaly, hydrocephalus, meningocele - GI : TE fistula, duodenal atresia, facial clefts (interfere with swallowing) |
|
|
Features of polyhydramnios
|
Pressure symptoms from overdistended uterus (dyspnea, edema, hydronephrosis)
Uterus large for dates, difficulty palpating fetal parts and hearing fetal heart tones Complications - cord prolapse - placenta abruptio - malpresentation - preterm labour - uterine dysfunction - postpartum hemorrhage - increased perinatal mortality rate |
|
|
Management of polyhydramnios
|
1- determine underlying cause
+ screen for maternal disease / infection + complete fetal U/S evaluation 2- depends on severity + mild to moderate cases require no treatment + if severe, hospitalize and consider therapeutic amniocentesis |
|
|
Definition of oligohydramnios
|
Amniotic fluid index of 5 cm or less
An important sign of chronic placental insufficiency |
|
|
Etiology of oligohydramnios
|
Early onset oligohydramnios
- Decreased production : renal agenesis or dysplasia, urinary obstruction, posterior urethral valves (male), chronic hypoxemia leading to IUGR results in shunting away from the kidneys to ensure profusion of the brain - Increased loss : prolonged amniotic fluid leak (although most often labour ensues) Late onset oligohydramnios - amniotic fluid normally decreases after 35 weeks - common in post-term pregnancies - U/S Doppler studies (umbilical cord and uterine artery Dopplers) |
|
|
Clinical features of oligohydramnios
|
Cord compression
Increased risk of fetal adverse outcomes Early onset - 15-25% have fetal anomalies - Amniotic fluid bands (T1) can leat to Potter's facies, limb deformities, abdominal wall defects Late onset - pulmonary hypoplasia - marker for infants who may not tolerate labour well |
|
|
Management of oligohydramnios
|
- Maternal hydration with oral or IV fluids to help increase amniotic fluid
- Vesicoamniotic shunt : if etiology is related to fetal obstructive uropathy, however, pulmonary function may not be restored with restoration of amniotic fluid. - Injection of fluid via amniocentesis will improve condition for 1 week - Consider delivery if at term - Amnio infusion may be considered during labour via intra-uterine catheter, evidence to show improved fetal outcomes is equivocal |
|
|
Definition of puerperium
|
6 week period of adjustment after pregnancy when pregnancy induced changes are reversed
|
|
|
Definition of postpartum hemorrhage
|
Loss of > 500 ml of blood at the time of vaginal delivery or > 1000 ml with C/S
Early : within first 24 hours postpartum Late : after 24 hours but within 6 weeks |
|
|
Etiology of postpartum hemorrhage
|
4 Ts
1. Tone - Uterine atony, due to: + labour (prolonged, precipitous, induced, augmented) + uterus (infection, over-distention) + placenta (abruption, previa) + maternal factors (grand multiparity, gestational HTN) + halothan anesthesia 2. Tissue - Retained placenta - Retained blood clots in atonis uterus - Gestational trophoblastic neoplasia 3. Trauma - Laceration - Episiotomy - Hematoma (vaginal, vulvar, retroperitoneal) - Uterine rupture - Uterine inversion 4. Thrombin - coagulopathy + most identified prior to delivery (low platelets inreases risk) + includes hemophilia, DIC, aspirin use, ITP, TTP, vWD + do not forget therapeutic anti-coagulation |
|
|
Uterine atony
|
Most common cause of PPH
Avoid by giving oxytocin with delivery of the anterior shoulder Occurs within first 24 hours |
|
|
Management of postpartum hemorrhage
|
Medical therapy
- Oxytocin 20 U/L NS or RL IV continuous IV - in addition can give 10 U intramyometrial after delivery of the placenta - Ergotamine 0.25 mg IM/IMM Q5min up to 1.25 mg; can be given as IV bolus - Carboprost (PGF-2 alpha analog) 0.25 mg IM/IMM Q15min to max 2 mg (major prostaglandin effect side effects and contraindicated in CN, pulmonary, renal and hepatic dysfunction) Local control - Bimanual compressions - Uterine packing (mesh with antibiotic treatment) - Intrauterine Senstake-Blakemore catheter for balloon tamponad - may slow hemorrage Surgical therapy - D&C (beware of vigorous scraping which may cause Asherman's syndrome) - Laparotomy with bilateral ligation of uterine artery,ovarian artery or hypogastric artery - Hysterectomy (last option) with angiographic embolization if post-hysterectomy bleeding |
|
|
Definition of retained placenta
|
Placenta undelivered after 30 minutes postpartum
|
|
|
Etiology of retained placenta
|
Placenta separated but not delivered
Abnormal placental implantation i.e. placenta accreta, placenta increta, placenta percreta |
|
|
Risk factors for retained placenta
|
Placenta previa
Prior C/S Post-pregnancy curettage Prior manual placental removal Uterine infection |
|
|
Management of retained placenta
|
2 large bore IVs, type and screen
Brant maneuver (firm traction on umbilical cord with one hand applying suprapubic pressure to hold uterus in place) Oxytocin 10 IU in 20 mL NS into umbilical vein Manual removal if above fails D&C if required |
|
|
Etiology of uterine inversion
|
Often iatrogenic (excess cord traction with fundal placenta)
Excessive use of uterine tocolytics More common in grand multiparous (lax uterine ligaments) |
|
|
Features of uterine inversion
|
Can cause profound vasovagal response with vasodilation and hypovolemic shock
Shock may be disproportionate to maternal blood loss |
|
|
Management of uterine inversion
|
Urgent management essentials, call anesthesia
ABCs - initiate IV crystalloids Can use tocolytic drug or nitroglycerin IV to relax uterus and aid replacement Replace uterus without removing placenta Remove placenta manually and withdraw slowly IV oxytocin infusion (only after uterus replaced) Re-explore uterus May require GA +/- laparotomy |
|
|
Definition of postpartum pyrexia
|
Fever > 38 on any 2 of the first 10 days postpartum, except the first day
|
|
|
Etiology of postpartum pyrexia
|
B-5W
Breast : engorgement, mastitis Wind : atelectasis, pneumonia, PE Water : UTI Wound : C/S incision or episiotomy site Walking : pelvic thrombophlebitis, DVT Womb : endomtritis |

