![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
439 Cards in this Set
- Front
- Back
|
Amount of blood that mom can afford to lose during pregnancy? |
1000 cc |
|
|
Uterine blood flow at term? |
750 cc/min (12% of CO) |
|
|
D dimers & fibrinogen level during pregnancy? |
D-dimers=> Inc=> never use during pregnancy Fibrinogen => inc => if “normal “ it’s pathological |
|
|
Resp system changes in pregnancy? |
Dec FRC=> Inc TV => inc minute ventilation |
|
|
Resp system changes in pregnancy? |
Dec FRC=> Inc TV => inc minute ventilation |
|
|
Cr changes in pregnancy? Normal value during pregnancy? |
Dec due to Inc blood flow to kidney => inc GFR 0.4- 0.8 mg/dl |
|
|
Obstructive uropathy In pregnancy? |
Enlarged uterus compresses on ureters at pelvic brim esp on R side |
|
|
Weight gain according to BMI in pregnancy? |
<18.5 => 1Ib/wk 18.5-24.9 => 0.75 Ib/wk 25-29.9 => 0.5 Ib/wk >30 => 0.25 Ib/wk |
|
|
Weight gain according to BMI in pregnancy? |
<18.5 => 1Ib/wk 18.5-24.9 => 0.75 Ib/wk 25-29.9 => 0.5 Ib/wk >30 => 0.25 Ib/wk |
|
|
1st trimester screening? |
Done between wk 10-0/7 & 13-6/7 PUB US=> nuchal translucency (normal is <3mm) b-HCG=> inc in downs PAPP-A=> dec in all |
|
|
2nd trimester screening? |
Best time=> between 16-18 weeks IBEA Inhibin A ,B-hCG=> inc in downs Estriol, AFP => inc in neural tube defects |
|
|
2nd trimester screening? |
Best time=> between 16-18 weeks IBEA Inhibin A ,B-hCG=> inc in downs Estriol AFP=> inc in neural tube defects |
|
|
Goals for 1st trimester US? |
Dates+ no of gestations + aneuploidy |
|
|
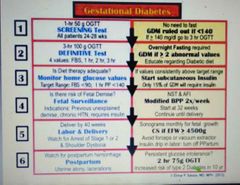
W/U of gestational DM? |
1 hr glucose tolerance test (screening test) => 3 hr glucose tolerance test (confirmatory test) |
|
|
1 hr glucose tolerance test procedure? |
50 gm of glucose => glucose level after 1 hr If <140 => stop screening If >140=> 3 hr glucose tolerance test |
|
|
W/U of gestational DM? |
1 hr glucose tolerance test (screening test) => 3 hr glucose tolerance test (confirmatory test) |
|
|
1 hr glucose tolerance test procedure? |
50 gm of glucose => glucose level after 1 hr If <140 => stop screening If >140=> 3 hr glucose tolerance test |
|
|
W/U of gestational DM? |
1 hr glucose tolerance test (screening test) => 3 hr glucose tolerance test (confirmatory test) |
|
|
1 hr glucose tolerance test procedure? |
50 gm of glucose => glucose level after 1 hr If <140 => stop screening If >140=> 3 hr glucose tolerance test |
|
|
Protocols of 3 hr glucose tolerance test? |
Fasting level=> 100 gm of glucose => glucose levels hourly for 3 hours |
|
|
W/U of gestational DM? |
1 hr glucose tolerance test (screening test) => 3 hr glucose tolerance test (confirmatory test) |
|
|
1 hr glucose tolerance test procedure? |
50 gm of glucose => glucose level after 1 hr If <140 => stop screening If >140=> 3 hr glucose tolerance test |
|
|
Protocols of 3 hr glucose tolerance test? |
Fasting level=> 100 gm of glucose => glucose levels hourly for 3 hours |
|
|
Positive 3 hr glucose tolerance test criteria? |
Any 2 of following 4: Fasting=> _>95 1 hour=> _> 180 2 hour=> _>155 3 hour=> _> 140 |
|
|
Condition associated with hypothyroidism ? |
Infertility due to anovulation |
|
|
Condition associated with hypothyroidism ? |
Infertility due to anovulation |
|
|
Rx of hypothyroidism in pregnancy? |
1- frequent TSH monitoring every 4-6 wks 2- adjust dose of levothyroxine based on TSH levels |
|
|
Rx of hyperthyroidism? |
1- surgery in 2nd trimester 2- PTU in pregnancy |
|
|
Rx of epilepsy in pregnancy? |
Levetiracetam Lamotrigine Folic acid supplement |
|
|
Rx of HTN in pregnancy? |
H LMN Hydralazine Labetalol Methyl dopa (DOC) Nifedipine |
|
|
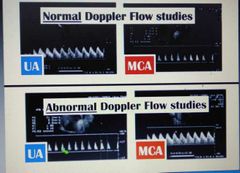
Umbilical A doppler use? |
To monitor growth restriction Normal => inc End Diastolic volume If absence/reversed flow=> inc risk of mortality Inc Systolic/Diastolic ratio is abnormal |
|
|
MCA doppler? |
Inc blood flow in fetal anemia |
|
|
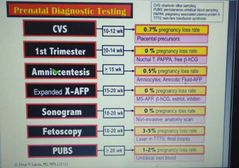
Amniocentesis vs CVS? |
Both => genetic testing CVS=> done at 10-13 wks Amniocentesis => done at 15-20 wks |
|
|
Amniocentesis vs CVS? |
Both => genetic testing CVS=> done at 10-13 wks Amniocentesis => done at 15-20 wks |
|
|
PUBS AKA? Done during which time? |
Cordocentesis 20-32 wks=> if >32 , just deliver |
|
|
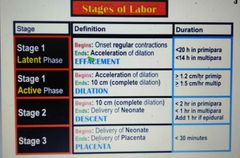
Stages of labour? |
Stage 1: Latent=> upto 6cm dilation, 20 hrs in nullipar, 14 hr in multipar Active+> upto 10cm dilation Stage 2: delivery of baby,3 hr for N & 2 hr for M Stage 3=> delivery of placenta, usually w/i 30 min of delivery |
|
|
Amniocentesis vs CVS? |
Both => genetic testing CVS=> done at 10-13 wks Amniocentesis => done at 15-20 wks |
|
|
PUBS AKA? Done during which time? |
Cordocentesis 20-32 wks=> if >32 , just deliver |
|
|
Stages of labour? |
Stage 1: Latent=> upto 6cm dilation, 20 hrs in nullipar, 14 hr in multipar Active+> upto 10cm dilation Stage 2: delivery of baby,3 hr for N & 2 hr for M Stage 3=> delivery of placenta, usually w/i 30 min of delivery |
|
|
Cervical change for labour? |
AKA cervical ripening => due to breakage of S-S bonds b/w collagen & infusion of water => effacement of cervix |
|
|
Amniocentesis vs CVS? |
Both => genetic testing CVS=> done at 10-13 wks Amniocentesis => done at 15-20 wks |
|
|
PUBS AKA? Done during which time? |
Cordocentesis 20-32 wks=> if >32 , just deliver |
|
|
Stages of labour? |
Stage 1: Latent=> upto 6cm dilation, 20 hrs in nullipar, 14 hr in multipar Active+> upto 10cm dilation Stage 2: delivery of baby,3 hr for N & 2 hr for M Stage 3=> delivery of placenta, usually w/i 30 min of delivery |
|
|
Cervical change for labour? |
AKA cervical ripening => due to breakage of S-S bonds b/w collagen & infusion of water => effacement of cervix |
|
|
Breech types? |
1- Frank=> hip flexed, knee extended 2- Complete=> hip flexed,knee flexed 3- Footling=> hip EXTENDED , knee any |
|
|
Pelvic inlet? |
From pubic symphysis to sacral prominence |
|
|
Adequate contraction? |
1- 3 in 10 minutes (averaged over 30 minutes) 2- Montevideo units >200 in 10 min (averaged over 30 min) |
|
|
How to Augment labour? |
1- balloon to stimulate engagement 2- misoprostol, dinoprostone 3- Oxytocin 4- amniotomy |
|
|
Cervical change during active phase of labor? |
1- 1.2 cm/hr in nulliparous 2- 1.5 cm/hr in multiparous |
|
|
How to Augment labour? |
1- balloon to stimulate engagement 2- misoprostol, dinoprostone 3- Oxytocin 4- amniotomy |
|
|
Cervical change during active phase of labor? |
1- 1.2 cm/hr in nulliparous 2- 1.5 cm/hr in multiparous |
|
|
Criteria for arrest of active phase? |
No cervical change: 1- after 4 hrs of adequate contractions 2- after 6 hrs of inadequate contractions |
|
|
Causes of arrest of active phase? |
1- Passenger=> baby too big(C/S) 2- Pelvis => mom’s anatomy (C/S) 3- Power=> dec strength of contractions => augment with oxytocin & amniotomy |
|
|
Px of ROM? P/E? Dx? |
1- rush of fluid 2- speculum exam=> pooling in posterior vagina 3- nitrazine test=> paper/swab turns blue Ferning on slide U/S=> oligohydramnios |
|
|
Preterm? Premature? |
1- before 37 weeks 2- no contractions |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
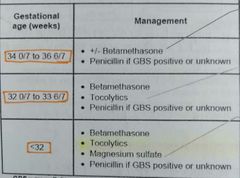
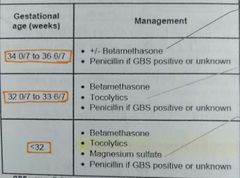
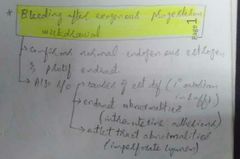
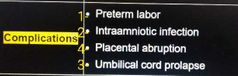
Preterm labour? Rx? |
1- contractions + cervical change before 37 wks 2- >34 => deliver <20 => abortion 20-34 => steroids + tocolytics |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
Preterm labour? Rx? |
1- contractions + cervical change before 37 wks |
|
|
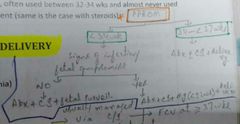
Tocolytics? |
BC PM 1- Beta agonist => rarely used 2- CCB=> nifedipine 3- PGE-i => indomethacin (avoid in >32 wks ) 4- magnesium => <32 weeks for neuroprotection |
|
|
Post dates? |
>40 wks by conception OR >42 wks by LMP |
|
|
Pre eclampsia def? Rx? |
_>140/ _>90 + _>300 mg/dl proteinuria after 20 wks Continue preg until 37 wks then deliver |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Magnesium used in? Schedule? |
1-Pre eclampsia with severe features & eclampsia 2- during labour & 24 hrs after delivery |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
Preterm labour? Rx? |
1- contractions + cervical change before 37 wks 2- >34 => deliver <20 => abortion 20-34 => steroids + tocolytics |
|
|
Tocolytics? |
BC PM 1- Beta agonist => rarely used 2- CCB=> nifedipine 3- PGE-i => indomethacin (avoid in >32 wks ) 4- magnesium => <32 weeks for neuroprotection |
|
|
Post dates? |
>40 wks by conception OR >42 wks by LMP |
|
|
Pre eclampsia def? Rx? |
_>140/ _>90 + _>300 mg/dl proteinuria after 20 wks Continue preg until 37 wks then deliver |
|
|
Pre eclampsia with severe features? |
1- _>160/_>110 2- Cr _>1.1 or 2* baseline 3- platelets <100000 4- AST/ALT 2* ULN 5- pul edema 6- RUQ or epigastric pain 7- headache or visual disturbance |
|
|
Rx of Pre eclampsia with severe features? |
Magnesium & urgent delivery |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks 2- <24 wks=> abortion 24-34 => steroids for lung maturity >34=> deliver |
|
|
Magnesium used in? Schedule? |
1-Pre eclampsia with severe features & eclampsia & HELLP 2- during labour & 24 hrs after delivery |
|
|
Earliest sign of Mg toxicity? Antidote? Preventive measures? |
1- dec resp rate + loss of DTRs 2- Ca 3- Mg checks |
|
|
Alarm sx that eclampsia is around the corner? |
1- capsular stretch 2- inc LFTs 3- dec platelets |
|
|
Added risk for di-zygotic twins? |
1- Breech 2- CS 3- PPH 4- preterm |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
Preterm labour? Rx? |
1- contractions + cervical change before 37 wks 2- >34 => deliver <20 => abortion 20-34 => steroids + tocolytics |
|
|
Tocolytics? |
BC PM 1- Beta agonist => rarely used 2- CCB=> nifedipine 3- PGE-i => indomethacin (avoid in >32 wks ) 4- magnesium => <32 weeks for neuroprotection |
|
|
Post dates? |
>40 wks by conception OR >42 wks by LMP |
|
|
Pre eclampsia def? Rx? |
_>140/ _>90 + _>300 mg/dl proteinuria after 20 wks Continue preg until 37 wks then deliver |
|
|
Pre eclampsia with severe features? |
1- _>160/_>110 2- Cr _>1.1 or 2* baseline 3- platelets <100000 4- AST/ALT 2* ULN 5- pul edema 6- RUQ or epigastric pain 7- headache or visual disturbance |
|
|
Rx of Pre eclampsia with severe features? |
Magnesium & urgent delivery |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks |
|
|
Magnesium used in? Schedule? |
1-Pre eclampsia with severe features & eclampsia & HELLP 2- during labour & 24 hrs after delivery |
|
|
Earliest sign of Mg toxicity? Antidote? Preventive measures? |
1- dec resp rate + loss of DTRs 2- Ca 3- Mg checks |
|
|
Alarm sx that eclampsia is around the corner? |
1- capsular stretch 2- inc LFTs 3- dec platelets |
|
|
Added risk for di-zygotic twins? |
1- Breech 2- CS 3- PPH 4- preterm |
|
|
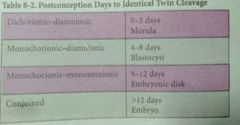
Timing of separation of embryos & type of twins? |
1- day 0-3=> tubal phase, di-ch di-amn 2- day 4-8=> blastocyst stage , mono ch & di amn 3- day 9-12=> non-conjoint with mono ch & mono amn 4- >12 days=> conjoint with mono ch & mono amn |
|
|
All multiple gestations at risk of? |
BC PPP 1- breech birth 2- pre term delivery (due date 4 wks less per fetus) 3- placenta previa 4- PPH 5- CS |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
Preterm labour? Rx? |
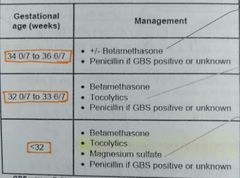
1- contractions + cervical change before 37 wks
|
|
|
Tocolytics? |
BC PM 1- Beta agonist => rarely used 2- CCB=> nifedipine 3- PGE-i => indomethacin (avoid in >32 wks ) 4- magnesium => <32 weeks for neuroprotection |
|
|
Post dates? |
>40 wks by conception OR >42 wks by LMP |
|
|
Pre eclampsia def? Rx? |
_>140/ _>90 + _>300 mg/dl proteinuria after 20 wks Continue preg until 37 wks then deliver |
|
|
Pre eclampsia with severe features? |
1- _>160/_>110 2- Cr _>1.1 or 2* baseline 3- platelets <100000 4- AST/ALT 2* ULN 5- pul edema 6- RUQ or epigastric pain 7- headache or visual disturbance |
|
|
Rx of Pre eclampsia with severe features? |
Magnesium & urgent delivery |
|
|
P PROM? Rx? |
1- ROM without contractions before 37 wks |
|
|
Magnesium used in? Schedule? |
1-Pre eclampsia with severe features & eclampsia & HELLP 2- during labour & 24 hrs after delivery |
|
|
Earliest sign of Mg toxicity? Antidote? Preventive measures? |
1- dec resp rate + loss of DTRs 2- Ca 3- Mg checks |
|
|
Alarm sx that eclampsia is around the corner? |
1- capsular stretch 2- inc LFTs 3- dec platelets |
|
|
Added risk for di-zygotic twins? |
1- Breech 2- CS 3- PPH 4- preterm |
|
|
Timing of separation of embryos & type of twins? |
1- day 0-3=> tubal phase, di-ch di-amn 2- day 4-8=> blastocyst stage , mono ch & di amn 3- day 9-12=> non-conjoint with mono ch & mono amn 4- >12 days=> conjoint with mono ch & mono amn |
|
|
All multiple gestations at risk of? |
BC PPP 1- breech birth 2- pre term delivery (due date 4 wks less per fetus) 3- placenta previa 4- PPH 5- CS |
|
|
Delivery decision in multiple gestations? |
1- cephalic-cephalic=> vaginal 2- cephalic-breech=> clinical decision 3- breech-breech => CS |
|
|
PPH def? |
1000 cc for c section 500 cc for vaginal delivery |
|
|
Uterine atony px? Rx? |
1- boggy uterus 2- MUTS uterus massage=> uterotonics => mechanical tamponade with Bakri balloon/packing => surgery |
|
|
Prolonged ROM? Association? |
1->18 hrs between ROM & delivery of placenta 2- inc risk of Gp B strep infections => chorioamnio, endometritis |
|
|
Chorioamnionitis vs endometritis? Px? |
1-baby out=> endomet baby in=> chorioamnio 2- maternal fever, tachy ,fundal (uterine)tenderness, purulent amniotic fluid |
|
|
Chorioamnionitis & endometritis rx? |
IV Clindamycin + amp + gent |
|
|
Preterm labour? Rx? |
1- contractions + cervical change before 37 wks |
|
|
Tocolytics? |
BC PM 1- Beta agonist => rarely used 2- CCB=> nifedipine 3- PGE-i => indomethacin (avoid in >32 wks ) 4- magnesium => <32 weeks for neuroprotection |
|
|
Post dates? |
>40 wks by conception OR >42 wks by LMP |
|
|
Pre eclampsia def? Rx? |
_>140/ _>90 + _>300 mg/dl proteinuria after 20 wks Continue preg until 37 wks then deliver |
|
|
Pre eclampsia with severe features? |
1- _>160/_>110 2- Cr _>1.1 or 2* baseline 3- platelets <100000 4- AST/ALT 2* ULN 5- pul edema 6- RUQ or epigastric pain 7- headache or visual disturbance |
|
|
Rx of Pre eclampsia with severe features? |
Magnesium & urgent delivery |
|
|
R/f for percreta/increta/acreta? Rx? |
1- inc risk with increasing pregnancies 2- D&C then hysterectomy |
|
|
Normal fetal HR? |
110-160 |
|
|
R/f for percreta/increta/acreta? Rx? |
1- inc risk with increasing pregnancies 2- D&C then hysterectomy |
|
|
Normal fetal HR? |
110-160 |
|
|
Non stress test evaluates? |
Accelerations & variability |
|
|
Non stress test evaluates? |
Accelerations & variability |
|
|
Adequate accelerations? |
>32 wks=> 15*15, 2 in 20 <32 wks=> 10*10, 2 in 20 |
|
|
Non stress test evaluates? |
Accelerations & variability |
|
|
Adequate accelerations? |
>32 wks=> 15*15, 2 in 20 <32 wks=> 10*10, 2 in 20 |
|
|
15*15, 2 in 20 interpretation? |
15 bpm rise in HR sustained for 15 seconds occurring twice in 20 minutes |
|
|
NST employed when? |
Dec fetal movements felt by mom |
|
|
NST employed when? |
Dec fetal movements felt by mom |
|
|
Biophysical profile determinants? |
NAB MT 1- NST 2- Amniotic fluid index 3- Breathing 4- movement 5- tone Each given 2 points |
|
|
Amniotic fluid index ? Interpretation? |
Sum of max depths of amiotic fluid pockets in each 4 quadrants Oligo<5 Normal >5 Reassuring 8-25 Polyhydramnios >25 |
|
|
NBSIM according to BPP? |
0-2 => fetal demise imminent 8-10=> reassuring 4-6=> >36 wks=> deliver oxytocin,CS <36 wks=> contraction stress test |
|
|
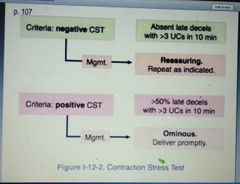
Contraction stress test interpretation? |
EH LU VC Early deceleration => head compression Variable deceleration => cord compression Late deceleration => uteroplacental insufficiency |
|
|
Variability stratification? |
Absent => no variation-smooth line Minimal=> <5 bpm variation Moderate=> 6-25 bpm variation Marked=> >25 bpm variation |
|
|
Findings suggestive of placenta previa remaining until end of pregnancy? |
1- lack of resolution by 3rd trimester 2- extension over Os by more than 25 mm |
|
|
Findings suggestive of placenta previa remaining until end of pregnancy? |
1- lack of resolution by 3rd trimester 2- extension over Os by more than 25 mm |
|
|
Vasa previa triad? |
ROM Bleeding Fetal bradycardia |
|
|
Uterine rupture px? |
Contractions + sudden fetal distress => loss of contractions + loss of fetal station |
|
|
Fetal R/F for erythroblastosis fetalis ? |
1- Mom Rh neg 2- Father Rh positive/unknown 3- Mom Rh antibody positive 4- Antibodies cause anemia ie Kell,D, Duffy antibodies 5- Antibody titers >1:8 to 1:32 |
|
|
Fetal R/F for erythroblastosis fetalis ? |
1- Mom Rh neg 2- Father Rh positive/unknown 3- Mom Rh antibody positive 4- Antibodies cause anemia ie Kell,D, Duffy antibodies 5- Antibody titers >1:8 to 1:32 |
|
|
NBSIM in erythroblastosis fetalis if paternity in question? |
Amniotic fluid PCR to determine genotype of baby |
|
|
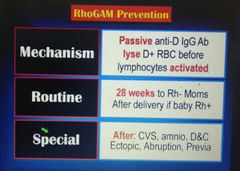
Ppx of alloimmunization? |
Rhogam-D IMIG at 28 wks & w/i 72 hrs of delivery |
|
|
Intrapartum abx choice in Gp B strep? |
1- Ampicillin => DOC 2- Cefazolin=> PCN allergic but not anaphylactic 3- clindamycin => PCN allergic and anaphylactic , if sensitive to both clinda & erythro 4- vancomycin => PCN allergic and anaphylactic , resistant to either clinda OR erythro |
|
|
Intrapartum abx choice in Gp B strep? |
1- Ampicillin => DOC 2- Cefazolin=> PCN allergic but not anaphylactic 3- clindamycin => PCN allergic and anaphylactic , if sensitive to both clinda & erythro 4- vancomycin => PCN allergic and anaphylactic , resistant to either clinda OR erythro |
|
|
Baby born to a hep B positive mom. NBSIM? |
CS=> IVIG hep B & Hep B vaccine on the day of delivery Breastfeeding is Ok |
|
|
Route of delivery in HIV mom? |
If viral load <1000 copies/ml=> ARVT + vaginally >1000 copies/ml or not on HAART=> AZT+ ARVT +C/S |
|
|
Intrapartum abx choice in Gp B strep? |
1- Ampicillin => DOC 2- Cefazolin=> PCN allergic but not anaphylactic 3- clindamycin => PCN allergic and anaphylactic , if sensitive to both clinda & erythro 4- vancomycin => PCN allergic and anaphylactic , resistant to either clinda OR erythro |
|
|
Baby born to a hep B positive mom. NBSIM? |
CS=> IVIG hep B & Hep B vaccine on the day of delivery Breastfeeding is Ok |
|
|
Route of delivery in HIV mom? |
If viral load <1000 copies/ml=> ARVT + vaginally >1000 copies/ml or not on HAART=> AZT+ ARVT +C/S |
|
|
HIV status positive at time of delivery. NBSIM? |
Zidovudine |
|
|
Intrapartum abx choice in Gp B strep? |
1- Ampicillin => DOC 2- Cefazolin=> PCN allergic but not anaphylactic 3- clindamycin => PCN allergic and anaphylactic , if sensitive to both clinda & erythro 4- vancomycin => PCN allergic and anaphylactic , resistant to either clinda OR erythro |
|
|
Baby born to a hep B positive mom. NBSIM? |
CS=> IVIG hep B & Hep B vaccine on the day of delivery Breastfeeding is Ok |
|
|
Route of delivery in HIV mom? |
If viral load <1000 copies/ml=> vaginally >1000 copies/ml or not on HAART=> CS |
|
|
HIV status positive at time of delivery. NBSIM? |
Zidovudine |
|
|
Breastfeeding in HIV? |
Not recommended |
|
|
Factors for successful VBAC? |
<_2 CS Low transverse cut |
|
|
Conditions under which vacuum & forceps are applied? |
Mom fully dilated & effaced Fetal station 2+ |
|
|
Grades of episiotomy? |
1=> involves vagina 2 => involves perineum 3 => involves anal sphincter 4 => involves anal mucosa |
|
|
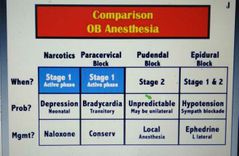
Pain of stage 1 & 2 spinal levels? |
Stage 1=> T10-T12 (visceral pain) Stage 2=> S2-S4 (somatic pain) |
|
|
Narcotics analgesia toxicity? Rx? |
1- resp depression 2- naloxone |
|
|
Narcotics analgesia toxicity? Rx? |
1- resp depression 2- naloxone |
|
|
Labour stage respective nerve blocks? Toxicity? |
Stage 1=> para cervical block with local lidocaine, fetal bradycardia Stage 2=> by palpating ischial tuberosity & injecting towards pudendal N near sacrospinous ligament |
|
|
Anesthesia of choice in labour? Toxicity? |
1-Epidural 2- if introduced in subdural space=> vasodilation & hypotension If too high=> paralysis of diaphragm |
|
|
Signs of placental separation? |
1- gush of blood 2- lengthening of cord 3- globular ,firm shape of uterus 4- uterus rises up to ant abd wall |
|
|
Low fetal birth wt? |
<2.5 kg OR <5.5 Ib |
|
|
Polyhydramnios def? Associations? |
1- AFI _>24 or single deepest pocket _>8cm 2- cong fetal malformation + maternal DM |
|
|
Fetal alcohol syndrome px? |
Microcephaly Mid face hypoplasia (small palpebral fissure, smooth philtrum, thin vermillon border) |
|
|
Def of infertility? |
Inability to conceive after 1- >6 mon of unprotected sex in >35 yr 2- >12 mon of unprotected sex in <35 yr |
|
|
Umbilical cord prolapse px? FHR tracing ? |
UC delivers ahead of fetal part , fetus is unengaged FHR tracings => persistent variable decelerations or severe bradycardia |
|
|
Uterine inversion vs vaginal/cervical inversion? |
Uterine=> shaggy appearance Cervix/vagina=> smooth |
|
|
Prolonged 3rd stage? Rx? |
>30 min Manual extraction of placenta |
|
|
Condition associated with uterine inversion? |
Hemorrhage |
|
|
Best initial therapy for non reducible uterus ie cervix tightly contracted in uterine atony? |
Uterine relaxing agent=> halothane, terbutaline, Mgso4 |
|
|
Steps to take with fetal bradycardia? |
1- confirm fetal HR 2- vaginal exam to assess for cord prolapse 3- positional changes 4- o2 5- IVF +/- pressors 6- discontinue oxytocin |
|
|
Mc finding in uterine rupture? |
Fetal HR abnormality |
|
|
Uterine hyper stimulation def? Association? |
>5 contractions in 10 min Misoprostol |
|
|
Type of Px associated with cord prolapse? |
Footling breech Transverse lie |
|
|
Polyhydramnios def? |
Single deepest pocket _> 8cm AFI => _>24 |
|
|
Sources of progesterone? |
Before 7 weeks=> corpus luteum Between 7& 9=> both After 9 wks=> placenta |
|
|
Functions of progesterone? |
Early=> endometrial changes for blastocyst implantation Late=> immune tolerance & prevent myometrial contraction |
|
|
Striae gravidarum AKA? |
Stretch marks |
|
|
Chadwick sign? |
Bluish discoloration of vagina & cervix as a result of increased vascularity |
|
|
Cloasma? |
Blotchy pigmentation of nose & face |
|
|
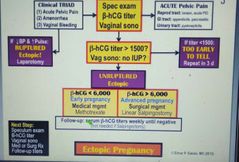
Criteria for MTX use in ectopic pregnancy? |
1- no fetal heart sounds 2- hcg<6000 3- pregnancy mass diameter <3.5 4- no hx of folic acid supplementation |
|
|
Different methods for abortion? |
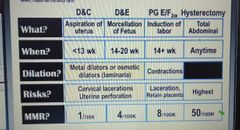
|
|
|
Different types of abortion? |

|
|
|
Wu of fetal demise? |
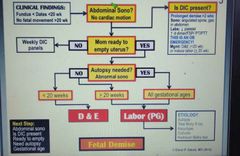
S DEA G |
|
|
Management of fetal demise? |
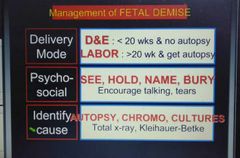
|
|
|
Most common location if ectopic pregnancy? |
Ampulla of fallopian tube |
|
|
Wu of ectopic pregnancy? |
Spec B V |
|
|
Dd of ectopic pregnancy? Further Wu with? |
A-TIME 1- Threatened abortion 2- incomplete abortion 3- molar preg 4- ectopic pregnancy B- US |
|
|
Prenatal diagnostic tests? |
|
|
|
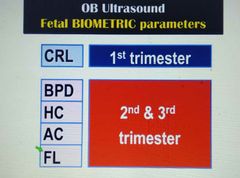
Obs US? and when they are done? What can they assess? |

|
|
|
Nuchal translucency dd? |
1- aneuploidy 2- congenital heart dz |
|
|
Tasks for 1st prenatal visit? |

|
|
|
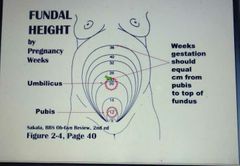
Clinical landmars of gestation with their associated gestational age? |

|
|
|
Fundal height in pregnancy? |
|
|
|
Fetal biometric parameters & when they are measured? |
|
|
|
Common findings with preg by trimester? 1- sx 2- signs 3- wt gain 4- complications |
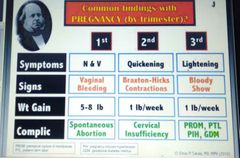
|
|
|
Routine prenatal tests by trimester? |
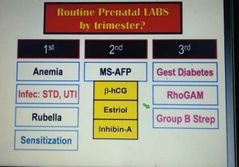
|
|
|
Tasks of first prenatal visit? |
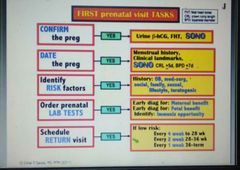
|
|
|
Signs of pregnancy? |

|
|
|
Establishing due date? |
1- conception dating=> 266 days or 38 wks 2- menstrual dating=> 280 days or 40 wks 3- Naegele's rule=> +7days/-3mon/+1year |
|
|
STDs screened during initial prenatal visit? |
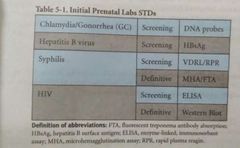
|
|
|
Causes of Inc AFP? NBSIM? |
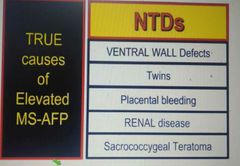
2- abd US |
|
|
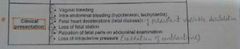
Initial approach to late trimester bleeding? |
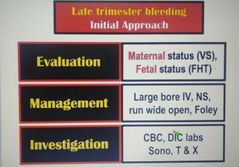
|
|
|
MCC of: 1- late preg bleeding 2- late preg painful bleeding 3- Obstetric DIC |
All=> apruptio placenta |
|
|
Perinatal infections? Rx? Mode of delivery? |
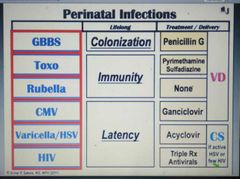
|
|
|
Perinatal infections with characteristic findings? |
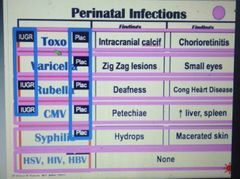
|
|
|
Perinatal infections that cause IUGR? |
CTR Rubella Toxo CMV
|
|
|
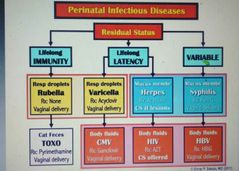
Perinatal infections that are transferred via placenta? |
CTR VS CMV Toxo Rubella Varicella Syphilis |
|
|
Perinatal infections that are transferred via vaginal fluids? |
HSV HBV HIV |
|
|
Px of GBS sepsis in neonates? Rx? |
1- bilat diffuse PNA & sepsis w/I hrs of birth 2- Pen G Alt=> clindamycin, erythromycin |
|
|
Toxo infection 1- lethal during 2- most occur during 3- prevention |
1- 1st trimester 2- 3rd trimester 3- avoid contact with cat feces |
|
|
Varicella mode of transmission? Residual effects of 1 infection? Risk of fetal infection highest? |
1- resp droplets 2- lifelong latency 3- 5 day AP to 2nd day PP |
|
|
MCC of congenital deafness? |
CMV |
|
|
Mc congenital viral infection? |
CMV |
|
|
Ppx of HIV? |
Triple therapy starting at 14 wks regardless of viral load |
|
|
Px of congenital syphilis? Delivery mode? |
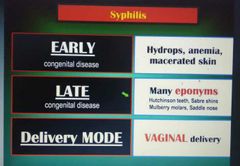
|
|
|
Residual status of perinatal infections? |
|
|
|
Mode of transmission of perinatal infections to mother? |
1-Resp droplets=> Rubella + varicella 2-Mucous membranes=> herpes+ syphilis 3-Cat feces=>toxo 4-Body fluids=>CMV+ HIV+ HBV |
|
|
Cervical insufficiency triad? |
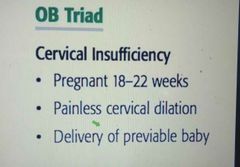
|
|
|
Wu of alloimmunization? |
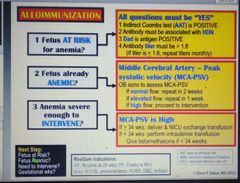
RAIG |
|
|
Alloimmunization ppx? |
|
|
|
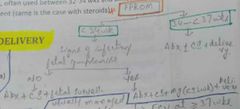
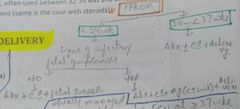
Preterm labor dx criteria? Management? Screening? |
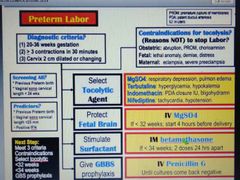
CT 32 34 G |
|
|
CI to tocolytics? |
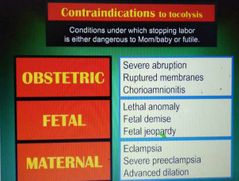
|
|
|
SE of tocolytics? |
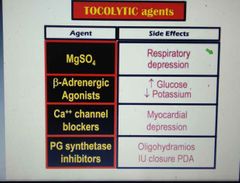
|
|
|
Reasons not to prolong preg in PROM? |
1- labor 2- distress 3- chorioamnionitis |
|
|
Management of post term pregnancy? |
DCS |
|
|
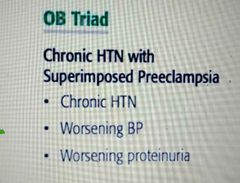
Cf suggesting superimposed preeclampsia on chronic HTN? |
|
|
|
Anti hypertensives never used in preg? |
1- ACE/ARBs 2- diuretics |
|
|
Cervical cerclage is considered in cervical insufficiency if? |
1- cervical length <25mm before 24 wks by vag US & 2- Prior preterm birth at <34 wks |
|
|
Management of cervical insufficiency? |
1- elective cerclage placement at 13-14 wks 2- emergency cerclage placement, but first ro labor, chorioamnionitis 3- cerclage removal at 36-37 wks to allow vag delivery if McDonald procedure performed 4- C/S if shirodkar |
|
|
Post conception embryos' separation day & associated type of twin? |
|
|
|
CI to mgso4? |
1-Renal insufficiency 2-Myasthenia gravis |
|
|
Prerequisite for fetal fibronectin test? |
1- gestation 22-35 wks 2- cervical dilation <3 cm 3- membranes intact |
|
|
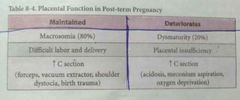
Two different syndromes of post term pregnancy? |
|
|
|
Management of meconium aspiration? |
1- amnioinfusion 2- laryngoscopic visualization=> only if fetus is depressed |
|
|
Preg with Multiple gestations px with preterm labor. NBSIM? |
Observation |
|
|
Rx of rheumatic MS? |
1- activity limitation 2- avoid anemia 3- balloon valvuloplasty |
|
|
Rx of eisenmenger syn? |
Avoid hypotension |
|
|
Do we need Abx ppx with congenital heart defects during delivery? |
No as s viridans aren't associated with genital tract |
|
|
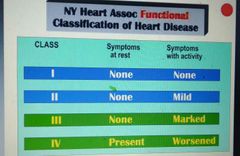
NYHA classification? And associated delivery place? |
1 & 2=> deliver in L&D, No invasive monitoring 3 & 4=> deliver in ICU, invasive monitoring |
|
|
Rx of hyperthyroidism? |
1st trimester=> PTU 2nd/3rd=> methimazole |
|
|
Fetal demise Rfs with GDM? Monitoring? |
1- need insulin or glyburide HTN Prev demise 2- NST & AFI 2/wk starting at 32 week |
|
|
Wu of gestational DM? |
|
|
|
Antepartum maternal assessment of overt DM? |
1- HbA1c 2- 24 hr urine 3- retinal exam 4- home glucose monitoring |
|
|
Fetal anomalies associated with DM? |
Only with overt DM . Not with true GDM (as hpl Inc in later half of preg ) 1- NTDs 2- congenital heart defects 3- sacral agenesis/caudal regression syn 200* Inc in overt DM |
|
|
Electrolyte Dec due to DM in preg? |
Ca |
|
|
Px of cholestasis of preg? Rx? |
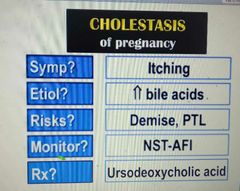
|
|
|
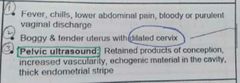
Px of acute fatty liver of preg? Rx? |
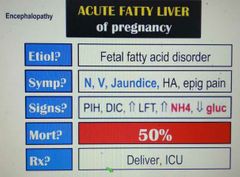
|
|
|
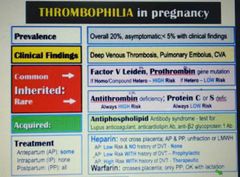
Thrombophilia in preg px? MCCs? Rx? |
AP=> LMWH is stopped at 36 wk & UFH is continued from there as it can be reversed with protamine sulfate in case of C/S PP=> anticoagulation can be started 6 hrs after vag delivery & 12 hrs after C/S. |
|
|
Highest risk of preg associated thrombophilia at what time? |
1st week postpartum |
|
|
Obs complications if; 1- hypothyroidism left untreated 2-hyperthyroidism left untreated |
1- anovulation, spontaneous abortion 2- thyroid storm, IUGR |
|
|
Rx of hypothyroidism in preg? |
Inc throxine dose by 30% above prepreg dose |
|
|
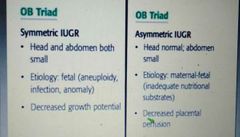
Symmetrical vs asymmetrical IUGR? |
|
|
|
Macrosomia definition? Management? |
1- >90% percentile, >4000 gm 2- scheduled C/S if: a- fetal wt >4500 gm in DM b- >5000 gm if no DM |
|
|
Uterus < or > dates. NBSIM? Causes? |

|
|
|
MCC of non reactive NST? |
Sleeping baby |
|
|
NBSIM If 1- negative CST 2- Positive CST |
|
|
|
Doppler flow studies in MCA & UA in normal & IUGR? |
|
|
|
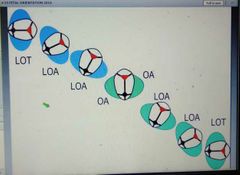
Position of fetal head during 1- start of labor 2-when comes out, 3-after coming out? |
|
|
|
Stages of labor? |
|
|
|
Wu of abnormal 1st stage of labor? |
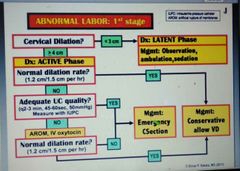
|
|
|
Comparison of OB anesthesia? |
|
|
|
Maternal meds that can cause 1- fetal Brady 2- fetal tachy |
1- beta blockers+ local anesthesics 2- beta agonists+ parasympatholytics |
|
|
UC prolapse px? |
Malpresentation/ unengaged fetal px part=> UC delivers thru cervix ahead of px fetal part=> persistent variable deceleration & severe brady |
|
|
Delay in Rx of acute cervicitis can result in? |
1- ascending infections 2- preg complications eg preterm birth |
|
|
Uterine size-date discrepancy? |
1->2 cm diff in fundal height measurement from gestational age |
|
|
Urinary protein excretion that is considered abnormal in preg? |
1->300 2- 2+ on urine dipstick |
|
|
Anemia def in preg? |
1st & 3rd trimester=> <11 2nd trimester=> <10.5 |
|
|
Pao2 & paco² in preg? |
PaO2=> 100-110 Paco2=> 27-32 |
|
|
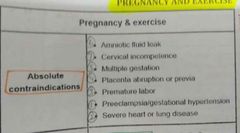
CI to exercise in preg? |
|
|
|
Exercise recommendation in preg? |
Low-mod intensity exercise for >30 min , 5-7 days/wk |
|
|
Antepartum fetal assessment of overt DM? |
1- quad screen at 16-18 2- US at 18-20 3- fetal echo at 22-24 4- monthly sonogram for fetal wt monitoring 5- if Inc risk of fetal demise=> weekly NST & AFI starting at 32 wks |
|
|
Rx of hyperemesis gravidarum? |
1- dietary changes 2- hydration 3- ginger 4- pyridoxine± doxylamine |
|
|
MCCs of Wernicke encephalopathy? |
1- chronic alcoholism 2- malnutrition (AN) 3- Hyperemesis gravidarum |
|
|
Thiamine def in preg associated with? |
1- Wernicke encephalopathy 2- spontaneous abortion |
|
|
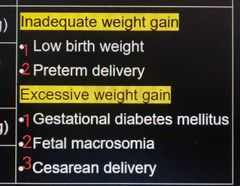
Complications of 1- excessive weight gain 2- inadequate weight gain |
1- fetal macrosomia+ GDM+ C/S 2- FGR+ preterm delivery |
|
|
R/fs for molar preg? |
1- extremes of maternal age 2- hx of hydatidiform mole 3- complete mole associated with Vit A deficiency |
|
|
Mc genotype of molar preg? |
46 XX |
|
|
Management of molar pregm |
1- D&C 2- Histopath confirmation 3- serial b-hcg levels 4- contraception for 6 mon |
|
|
Confirmation of malignant gestational trophoblastic dz? Rxm |
1- quantitative b-hcg 2- MTX & hysterectomy |
|
|
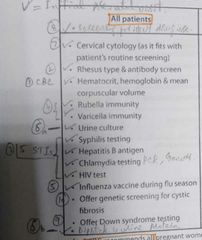
1st Prenatal visit tests? |
|
|
|
HIV positive mom's should be screened for which vaginal pathogen additionally? |
Trichomonas vaginalis |
|
|
Rx of asymptomatic bacteriuria? |
1- cephalexin 2- amox clav 3- nitrofurantoin 4- fosfomycin |
|
|
Routine vaccines during preg? |
1- TDaP 2- inactivated influenza 3- Rho(D) immunoglobulin |
|
|
Vaccines recommended for special circumstances in pregm |
Hep A & B SHiN Post expo varicella zoster |
|
|
Vaccines not recommended in pregm |
1- HPV 2- MMR 3- Varicella 4- live influenza 5- small pox |
|
|
Rx of syphilis in preg? |
IM benzathine pen G 1 dose weekly for 3 weeks |
|
|
Unvaccinated preg women with confirmed Rubella expo. NBSIM? |
Offer termination of preg If not wishing to do=> IVIG |
|
|
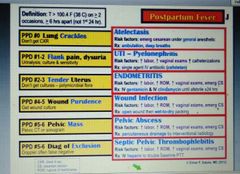
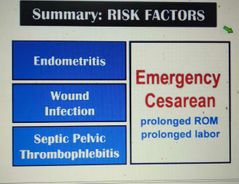
Rfs for septic pelvic thrombophlebitis? |
1- preg 2- C/S 3- Endometritis 4- ca 5- PID 6- Pelvic surg |
|
|
Px of septic Pelvic thrombophlebitis? |
1- fever unresponsive to abx 2- no localising signs 3- neg infectious diagnostic evaluation |
|
|
Rx of septic pelvic thrombophlebitis? |
1- anticoagulation 2- broad spectrum Abx |
|
|
2nd trimester quad screen in 1- trisomy 18 2- NTD 3- abd wall defect |
1- normal inhibin A 2- Inc AFP 3- Inc AFP |
|
|
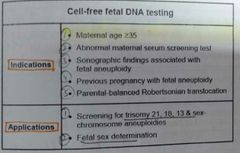
Cell free fetal DNA indications? Applications? |
|
|
|
Inc AFP associated with which renal conditions? |
1- fetal congenital nephrosis 2- benign obstructive uropathy |
|
|
Complications of chorioamnionitis? |
1-Maternal=> uterine atony+ PPH+ Endometritis 2-Fetal=> Premature birth+ infection+ enceph+ cerebral palsy+ death |
|
|
Px of malignant gestational trophoblastic dz? |
1- irregular postpartum bleeding 2- enlarged uterus 3- pelvic pain |
|
|
Sinusoidal FHR tracing characteristics? Association? |
1-Category 3 FHR tracing Fixed amplitude of 5-15/min & frequency 3-5 cycle/min 2- severe fetal anemia |
|
|
Fetal position when early deceleration occurs? |
Ant fontanel in close contact with cervix (ie cervix ≥5cm dilated & station 0) |
|
|
Late deceleration associated with? Causes? |
1- uterplacental insufficiency 2- labor stress(tachysystole) Abruptio placenta Placental calcification |
|
|
Causes of variable deceleration? |
1- cord compression 2- cord prolapse 3- nuchal cord 4- oligohydramnios |
|
|
Characteristics of variable deceleration? |
1- abrupt <30 sec from start to Nadir 2- decrease ≥15/min; duration ≥15 sec but <2 min 3- have variable depth & duration with each deceleration 4- not necessarily associated with contraction |
|
|
NBSIM if 1- intermittent variable deceleration 2- recurrent variable deceleration |
1- close obs without intervention 2- A- maternal repositioning (L lateral position, all fours) B- Amnioinfusion C- instrumental delivery if fully dialted D- Don't use oxytocin |
|
|
Category 1 FHR tracing pattern? |
1- FHR 110-160 2- Moderate variability => 6-25 3- ± acceleration 4- ± early deceleration 5- no late/variable deceleration |
|
|
Category 3 FHR tracing? |
≥1 of following 1- absent variability + Brady 2- absent variability + recurrent late deceleration 3- absent variability + recurrent variable deceleration 4- sinusoidal pattern |
|
|
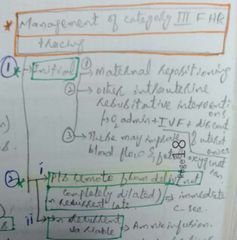
Management of category 3 FHR? |
|
|
|
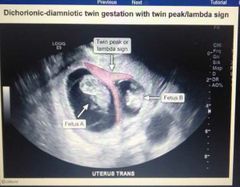
How to differentiate between monochorionic vs dichorionic on imaging? |
Differentiated by base shape of intertwin membrane T sign=> monochorionic lamDa sign=> Dichorionic |
|
|
FHR Tracing on abruptio placentae? |
1- no acceleration 2- late deceleration 3- minimal variability |
|
|
Management of placenta previa? |
1- speculum exam: TAUS followed by TVUS 2- C/S at 36-37 weeks 3- digital vaginal/cervical exam & sex CI |
|
|
R/fs for placenta previa? |
1- Prev hx of placenta previa 2- prior c/s or other uterine surg 3- multiparity 4- Inc maternal age >35 5- smoking |
|
|
FHR tracing in placenta previa? |
Early in dz=> normal ie reactive Continued bleeding=> fetal compromise |
|
|
Rfs for abruptio placentae? |
1- maternal HTN, preeclampsia, eclampsia trauma 2- abd trauma 3- cocaine, smoking 4- prior hx of abruptio placentae |
|
|
Rfs for uterine rupture? |
1- prior uterine surg 2- induction of labor/prolonged labor 3- fetal macrosomia 4- congenital uterine anomalies |
|
|
Cfs of uterine rupture? |
|
|
|
Pt with Prev hx of classical uterine incision/ myomectomy with entry to uterine cavity. NBSIM if 1- pt px b4 labor 2- at labor |
1- elective c/s at 36-37 wks 2- A- unruptured=> laparotomy followed by hysterotomy B- ruptured=> deliver thru rupture site followed by uterine repair |
|
|
Placenta accreta Rfs? |
1- hx of c/s 2- myomectomy 3- D&C 4- maternal age >35 |
|
|
Antenatal US findings in placenta accreta? |
Irregular or absent myometrial -placental interface & intraplacental villous lakes |
|
|
Management of placenta accreta? |
Antenatally diagnosed=> planned cesarean hysterectomy Undiagnosed=> usually results in cord avulsion & needs manual extraction |
|
|
Vasa previa rf? |
2nd trimester US=> Placenta previa 3rd trimester=> resolves without involution of associated blood vessels |
|
|
FHR Tracing in Vasa previa? |
Tachy=> Brady=> sinusoidal wave pattern |
|
|
Dx of Vasa previa? |
Antenatal abd & TV Doppler US |
|
|
Management of Vasa previa? |
If dx before labor=> C/S Dx during labor=> emergency C/S |
|
|
Intrauterine adhesions rf? Evaluation? |
1- intrauterine infection intrauterine surg 2- hysteroscopy
|
|
|
Intrauterine adhesions result in? |
Lack of endomet (Asherman syn) 1- light menses 2- 2 amen 3- infertility 4- neg progesterone withdrawal test 5- cyclic pelvic pain 6- recurrent preg loss |
|
|
Rx of intrauterine adhesions? |
Lysis of adhesions |
|
|
Progesterone withdrawal test? |
|
|
|
Rfs for ectopic pregnancy? |
1- prior hx of ectopic pregnancy 2- Prev Pelvic/tubal surg 3- PID |
|
|
Rx of ectopic pregnancy? |
1- MTX=> CI in ruptured 2- Surg |
|
|
Specific Rfs for cornual/ interstitial ectopic pregnancy? |
1- uterine anomalies eg bicornuate 2- in vitro fertilization |
|
|
Inadequate contractions? |
<3 in 10 min Soft to palpate |
|
|
1-Def of arrest of labor in 1st stage ? 2-Rx? |
1-Dilation ≥6cm with ROM & 1 of following: A- no cervical change for ≥4 hrs despite adequate contractions B- no cervical change for ≥6 hrs with inadequate contractions 2- C/S |
|
|
MCC of arrest of 2nd stage? |
Fetal malposition |
|
|
Precipitous labor? Most significant r/f? |
1- spontaneous fetal delivery that occurs within 3 hrs of initiation of contractions. Not caused by oxytocin. 2- multiparity |
|
|
Indications of oxytocin? SEs? |
A- 1- induction & augmentation of labor 2-PPH B- 1- SIADH=>Hyponatremia 2-Hypotension 3-Tachysystole=> FHR tracing abnormalities 4-rupture of unscarred uterus |
|
|
SEs of epidural analgesia? |
1- hypotension 2- high spinal 3- leakage of CSF |
|
|
Preterm labor def? |
Regular painful contractions at <37 wks that cause cervical Dilation ≥3 cm &/or effacement length <2 cm |
|
|
Mgso4 given with? Not given with? |
1- indomethacin 2- nifedipine |
|
|
Fetal fibronectin low during? Useful during? |
22-33 wks for predicting preterm labor |
|
|
Prevention of preterm birth? |
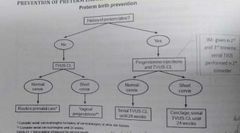
|
|
|
Rfs for preterm labor? |
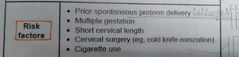
6- PPROM 7- Age >40 8- IVF |
|
|
Rfs for PROM? |
1-Genital tract infection 2- hx of prior PPROM 3- Tobacco use |
|
|
Management of PPROM? |
|
|
|
Indications for operative vaginal delivery? |
1- protracted 2nd stage of labor 2- FHR abnormalities 3- maternal CI to pushing |
|
|
Fetal complications of operative vaginal delivery? |
1- laceration 2- cephalohematoma 3- facial N palsy 4- intracranial hemorrhage 5- shoulder dystocia |
|
|
Maternal complications of operative vaginal delivery? |
1- GUT injury 2-urinary retention 3- rectal sphincter involvement 4- hemorrhage |
|
|
Maternal CI to pushing? |
1-NM dz 2-If valsalva is CI=> cerebrovascular dz + cardiovascular dz |
|
|
CI to ECV? |
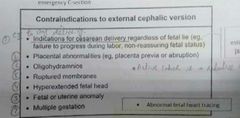
|
|
|
Internal podalic version used in? |
In twin delivery to convert second twin from oblique/transverse px to breech px for subsequent delivery |
|
|
Septic abortion often follows? Cfs? |
1- induced abortions 2- fever + malaise + signs of sepsis + foul smelling vaginal discharge + cervical & uterine motion tenderness |
|
|
Products of conception? |
A solid or sac like bloody white mass |
|
|
Wu of recurrent preg loss? |

|
|
|
Management of spontaneous abortion? |

|
|
|
What is Lochia ? Types? |
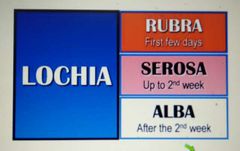
Shedding of endometrial layer of decidua basalis |
|
|
Lower abd pain 6hrs after a spontaneous vaginal delivery. Dx? Rx? |
1- uterine contractions 2- analgesics |
|
|
Postpartum contraception? |
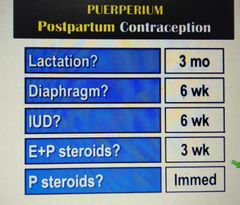
|
|
|
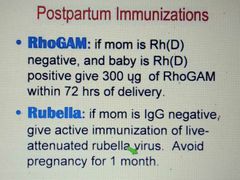
Postpartum immunizations? |
|
|
|
Causes of postpartum hemorrhage? Management? |

|
|
|
Placental inspection components |
1- maternal side=> check for all cotyledons 2- fetal side=> blood vessels usually don't go close to boundary of placenta but if they do think missing accessory lobe |
|
|
Dd of postpartum fever? Rx? |
Wind=> water=> womb=> wound=> walk |
|
|
Sequel if Endometritis isn't treated? |
Endomet=> endo myo met=> Endo myo para met=> Pelvic abscess |
|
|
Rfs for Endometritis, wound infection, septic pelvic thrombophlebitis? |
Inc vaginal exams |
|
|
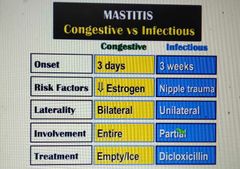
Congestive mastitis vs infectious mastitis? |
|
|
|
Thin & thick Endomet stripe ? |
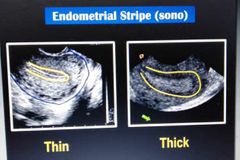
|
|
|
Non-mets vs good prognosis vs poor prognosis gestational trophoblastic neoplasia? |
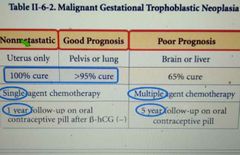
|
|
|
Ulcer vs no ulcer STD? |
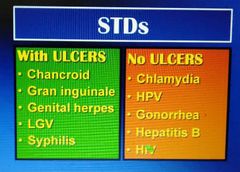
LGS CH |
|
|
STDs with painful ulcers? |
1- genital herpes 2- chancroid |
|
|
LGV associated groove sign? |
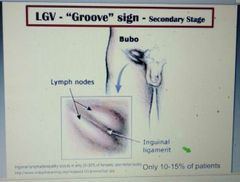
|
|
|
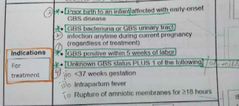
Indications for GBS Rx? |
|
|
|
1- Definition of FGR? 2- CFs? |
1- <10% percentile wt for gestational age 2- loose peeling skin Minimal sub-cut fat Thin umbilical cord Large ant fontanel Meconium stained amniotic fluid |
|
|
Wu of FGR? |
1- placenta histopath 2- looks syndrome associated=> karyotype 3- urine tox 4- serology |
|
|
Neonatal Complications of FGR? |
1- polycythemia 2- hypoglycemia 3- hypocalcemia 4- poor thermoregulation |
|
|
FGR Rfs? |
1- maternal htn 2- pregestational DM 3- Genetic abnormalities 4- congenital inf |
|
|
Wu of antepartum bleeding? |
1- speculum exam 2- TV US |
|
|
Normal uterine contraction characteristics? |
1- occurs every 2-3 min 2- lasts for 45-55 sec 3- intrauterine pressure of 55 mmhg |
|
|
ECV performed at? |
Between >37 wks & labor |
|
|
Mechanism of abortion mcly leading up to septic abortion? |
Induced abortions |
|
|
Uterotonic used in spontaneous abortion? |
Misoprostol Not oxytocin as it's receptors are fewer in 1st & 2nd trimester |
|
|
Px of septic abortion? |
|
|
|
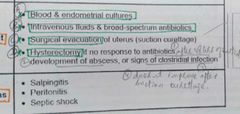
Rx of septic abortion? Complications? |
|
|
|
Evaluation of IUFD? |
|
|
|
Management of late term preg? |
1- frequent fetal monitoring=> NST + US for amniotic fluid vol 2- delivery prior to 43 weeks gestation |
|
|
1- Beta 3 agonist used to treat which type of urinary incontinence ? 2- Eg? |
1- urgency incontinence 2- mirabegron |
|
|
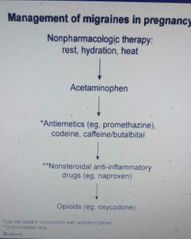
Rx of migraine in preg? |
NAANO |
|
|
Postpartum management of GDM? |

|
|
|
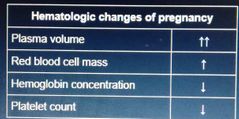
Heme changes in preg? |
|
|
|
Complications of acute pyelo in preg? |
1- ARDS 2- preterm labor 3- LBW |
|
|
Rx of UTI in preg. NBSIM? |
Test of cure ie a repeat urine culture to check if infection has been eradicated |
|
|
Fetal fibronectin test use? |
Used to diff between true preterm labor & false labor in pts with preterm contractions |
|
|
Inc AFP value? |
≥2.5 MoM |
|
|
Normal causes of Inc AFP? |
1- MCC=> incorrect gestational age dating 2- multiple gestations |
|
|
Rfs for pyelo in preg? |
1- asymptomatic bacteriuria 2- dm 3- age <20 |
|
|
Mc presenting sx of preeclampsia with severe features? |
Bilat occipital /frontal HA that doesn't improve with acetaminophen & NSAIDs |
|
|
Mc rf for pelvic organ prolapse? |
Multiparity |
|
|
Degrees of Perineal lacerations? |

|
|
|
1- Round ligament pain pathophys? 2- Px? |
1- ligament stretched by gravid uterus 2- sharp pain that radiates to vagina |
|

Findings? |
|
|
|
Mc type of twin preg? |
Dichor diamniotic |
|
|
US appearance of a uterine fibroid? |
Hypoechoic mass with shadowing |
|
|
Complications of Dec wt gain in preg? Excessive gain in preg? |
|
|
|
Pre-preg wt & Ideal preg wt gain for that category? |
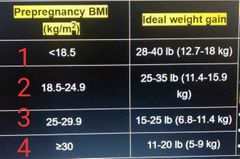
|
|
|
How much extra caloreies needed in 2nd & 3rd trimester? |
350-450 kcal/day |
|
|
Doppler flow to adnexa during ectopic pregnancy findings? |
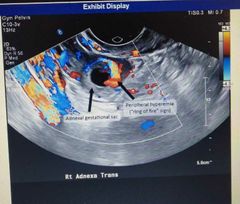
Ring of fire sign=> Inc Doppler flow |
|
|
Short interpreg interval def? It's complications? |
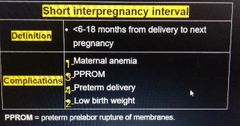
|
|

Sign? |
Amniotic fluid Ferning |
|
|
Complications of PPROM? |
|
|
|
Pathophys of placental abruption in PPROM? |
Dec amniotic fluid=> uterine decompression=> maternal decidual vessels shear=> bleeding & placental separation |
|

Dx? |

Double bubble sign of Duodenal atresia + associated polyhydramnios |
|

Dx? |
Rocker bottom feet |
|

Dx? |
Clenched hands with overlapping fingers |
|

Cystic mass is? Probable dx? |
1- cystic hygromas 2- Turner syn |
|

Dx? |
Ectopic pregnancy |
|

Dx? |
Uterine leiomyoma |
|
|
Px of retained placenta? |
1- persistent vaginal bleeding 2- malodorous lochia |
|
|
Total fetal blood volume? |
~250 ml or 1 cup |
|
|
Dx criteria of cervical insufficiency? |
|
|
|
Rx of cervical insufficiency? |
Prophylactic Cerclage placement at 12-14 wks |

