![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
17 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
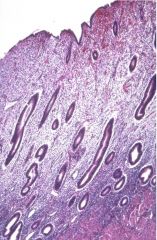
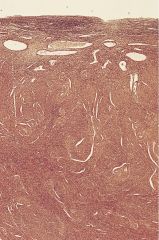
normal proliferative phase
|
endometrium under the influence of estrogen. glands have straight tubular appearance, dense and mitotically active stroma
|
|
|
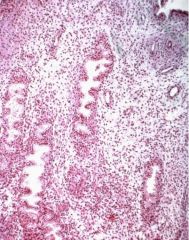
normal secretory phase
|
endometrium post ovulation, under the influence of progesterone. increasingly complex glands w/ edematous stroma, vascular changes, & pseudodecidual rxn
|
|
|
normal menstrual phase
|
glands degenerate, stroma invaded by neutrophils
|
|
|
post implantation endometrium
|
hobnailing of endometrium following implantation (hCG) w/ hypersecretory glands (Aria-Steele)
|
|
|
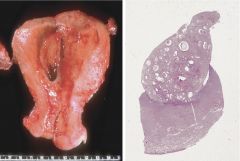
post menopausal endometrium (mostly myometrium)
|
inactive endometrium w/ atrophic glandular epithelium resulting from estrogen withdrawal
|
|
|
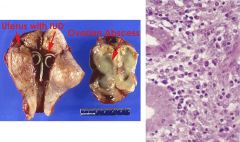
endometritis
|
acute: s/p ascending cervical infection, PMN infiltrate
chronic: s/p IUD, PID, retained POC, plasma cell & lymphocyte infiltrate symptoms: abnormal bleeding, pelvic pain, pyometra w/ endocervical canal blockage (increased squamous endometrial carcinoma risk) |
|
|
adenomyosis
|
hormonally responsive endometrial glands and stroma present in myometrium
enlarged uterus w/ reddish myometrium w/ cyst foci (not to be confused w/ adenocarcinoma) symptoms: pelvic pain, abnormal bleeding, dysmenorrhea, dyspareunia, regression w/ menopause tx: hysterectomy, or tx symptoms |
|
|
endometriosis
|
endometrial glands/stroma outside the uterus, 5-10% young women
endometrial reflux through fallopian tube during menopause (most widely accepted theory) reddish hemorrhagic lesions become cystic --> chocolate cysts --> cyclic bleeding additional symptoms: dysmenorrhea, pelvic pain, dyspaneuria, 1-2% develop adenocarcinoma |
|
|
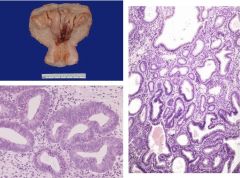
endometrial polyp
|
benign proliferative lesions, typically in perimenopausal women. result from focal hypersensitivity of endometrial glands to estrogen. may show cystic of hyperplastic changes. may be associated w/ bleeding, 0.5% develop to adenocarcinomas
|
|
|
endometrial hyperplasia
|
pre neoplastic process occuring as a result of unopposed estrogen stimulation (PCOS, granulosa cell tumor, obesity, exogenous estrogen therapy)
simple - mild glandular complexity w/out atypia (1% progress to adenocarcinoma) complex hyperplasia - marked glandular complexity w/out atypia (3%) atypical hyperplasia - marked glandular complexity w/ atypia (25%) symptoms: abnormal uterine bleeding tx: reduce estrogen stimulation, hysterectomy |
|
|
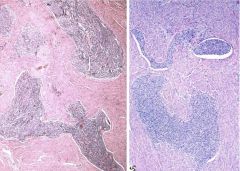
endometrial adenocarcinoma
|
typically post-menopausal, endometroid differentiation following effects of increased or unopposed estrogen. increased risk w/ breast or ovarian cancer.
papillary growth invading the myometrium endometrioid (60%) - glandular structures, nuclear atypia secretory - well differentiated serous - well differentiated, non-estrogen dependent, poor prognosis clear cell - non-estrogen dependent, poor prognosis post menopausal bleeding metastasizes to paraortic lymph nodes |
|
|
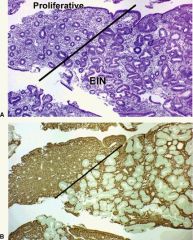
Endometrial Intraepithelial Neoplasia
|
alternative method to dx proliferative endometrial lesions. loss of PTEN (tumor suppressor) function. pre neoplastic lesion
|
|

|
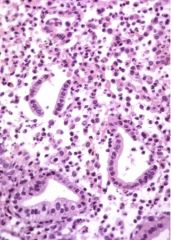
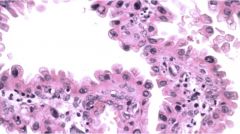
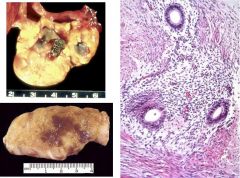
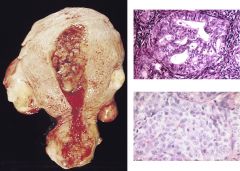
endometrial adenocarcinoma
Serous (top R) clear cell (bottom R) |
typically post-menopausal, endometroid differentiation following effects of increased or unopposed estrogen. increased risk w/ breast or ovarian cancer.
papillary growth invading the myometrium endometrioid (60%) - glandular structures, nuclear atypia secretory - well differentiated serous - well differentiated, non-estrogen dependent, poor prognosis clear cell - non-estrogen dependent, poor prognosis post menopausal bleeding metastasizes to paraortic lymph nodes |
|
|
endometrial stromal sarcoma
|
polypoid growth, derived from stromal cellls, invades myometrium & uterine vessels. resembles proliferative phase stroma, recurrence common
|
|
|
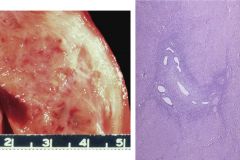
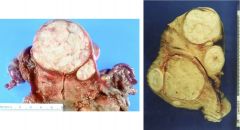
leiomyomas
|
benign tumor of myometrial origin, 75% of women, regression w/ menopause. uniform spindle cells in interlacing bundles, low mitotic rate, lack nuclear atypia & extensive necrosis
symptoms: bleeding, discomfort, compression of adjacent structures tx: myomectomy, hysterectomy, ablation |
|
|
leiomyoma
|
benign tumor of myometrial origin, 75% of women, regression w/ menopause. uniform spindle cells in interlacing bundles, low mitotic rate, lack nuclear atypia & extensive necrosis
symptoms: bleeding, discomfort, compression of adjacent structures tx: myomectomy, hysterectomy, ablation |
|

|
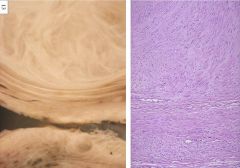
leiomyosarcoma
|
malignant neoplasm arising from myometrium. large areas of necrosis, high mitotic rate, nuclear atypia, 5 yr survival < 20%
|

