![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
148 Cards in this Set
- Front
- Back
|
what is the major glucogenic precursor? (which a.a.)
|
alanine: Ala released by muscle, kidneys and the gut ends up in the liver, (major site of gluconeogenesis and urea synthesis). Of all aa taken up by liver from circulation, >50% is Alanine.
|
|
|
what are the essential aa?
|
PVT TIM HALL
Phenylalanine-Valine-Tryptophane, Threonine-Isoleucine-Methionine, Histidine-Arginine-Lysine-Leucine Of the 10 essential amino acids: * The three basic amino acids are listed (Histidine-Arginine-Lysine) * The three branched chain amino acids are listed (Valine-Isoleucine-Leucine) The last two, Lysine and Leucine, are the only two purely ketogenic amino acids (His and Arg are only required in children and infants) |
|
|
what are omega 3 and 6 fatty acids?
|
6: linoleic acid in veg oil
3: alpha-linoleic acid in flaxeed oils, walnuts etc; eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) in fish oils, effective in lowering TG levels |
|
|
what is enriched carbs?
|
B vitamins added back (thiamin, riboflavin, niacin and folic acid)
these are present in bran (shell) and germ, which are removed in refined grains |
|
|
why is whole-grain food good?
|
Reduced hyperglycemia and insulin demand
reduced oxidative stress due to natural combo of B vitamins |
|
|
what happens during fasting?
|
-Use FFA, then ketone bodies
-Gradually allow brain to use ketone bodies instead of glucose -Brain transport of ketones is enhanced -Fasts of up to 60-70 days possible -Renal contributions to gluconeogenesis -reactions change to favor gluconeogenesis rather than glycolysis. |
|
|
what happens in the fed state (action of insulin)?
|
-Insulin rises
-Fatty acid oxidation inhibited -Ketogenesis suppressed -Free fatty acid levels drop as lipolysis stops -Lipogenesis resumes -Ketone bodies are metabolized to CO2 |
|
|
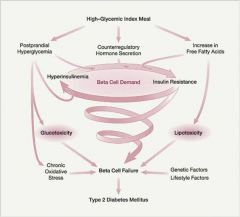
How do High Glycemic Loads Lead to Type 2 Diabetes Mellitus
|
|
|
|
what vitamins/minerals are not essential?
|
Vitamin D -- synthesized in skin
Niacin -- synthesized from tryptophan Vitamin K, Biotin, Folate -- synthesized by intestinal bacteria umm...i think this is wrong |
|
|
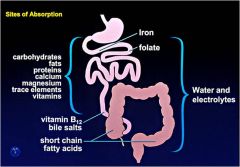
where is iron, folate, b12 and bile salts absorbed?
|
|
|
|
what are the most common causes of vit/min deficiencies in the US?
|
-chronic alcoholism
-malabsorption syndromes -poor or fad diets |
|
|
what is EAR, RDA, AI and UL when it comes to nutrient determination?
|

AI: adequate intake, when RDA cannot be determined (amt assumed to be adequate)
|
|
|
which vitamins are ligands for nuclear receptors?
|
A and D
|
|
|
which vitamins are antioxidants?
|
C and E
|
|
|
what's B1?
|
thiamin, cofactor for thiamine pyrophosphate (TPP), in:
- Pyruvate dehydrogenase complex (converts pyruvate into acetyl coA) - α-ketoglutarate dehydrogenase (converts α-ketoglutarate into succinyl coA...in TCA cycle) - transketolase reaction in pentose phosphate pathway to generate NADPH |
|
|
what happens with B1 deficiency?
|
B1 = thiamin
BeriBeri: Dry: peripheral neuropathy Wet: edema, tachycardia, cardiomegaly, congestive heart failure |
|
|
what is B2? what happens with def?
|

B2 = riboflavin -> FMN -> FAD (redox)
Def: mouth lesions (cheilosis, angular stomatitis) dermatitis glossitis (thick beefy tongue) |
|
|
what is B3? def?
|
B3 = niacin (can be made from trp) -> NAD/NADP
Def (alcoholics, trp def (e.g.Hartnup's)): Pellagra: Diarrhea Dermatitis Dementia |
|
|
pharmacological dose of which vitamin has anti-hyperlipidemia effect?
|
niacin
(niacin inhibits lipolysis in adipose cells-->dec free fatty acids-->liver has less free fatty acids to make TG-->dec TG production-->dec VLDL made by liver (VLDL made out of TG)-->dec LDL (LDL made out of VLDL in plasma...also, remember that LDL has a lot of cholesterol) okay so less VLDL and less LDL that means that there's less plasma TG (in the form of VLDL) and plasma cholesterol (in the form of LDL) kapish? |
|
|
what's B6? def?
|

pyridoxine -> makes PLP (pyridoxal phosphate...the active form)
-transamination -transsulfation -deamination -condensation Def: oculo-orogenital syndrome |
|
|
which vitamin is required for conversion of linoleic acid into arachidonic acid (prostaglandin precursor)
|
b6 = pyridoxine
|
|
|
what is B5?
|
pantothenate, makes CoA, Required for β-oxidation of fatty acids and oxidative degradation of amino acids
|
|
|
what is B9?
|
folate; active form THF; one-carbon transfer;
1. homocystein-methionine metab 2. thymidine synthesis (dUMP -> dTMP) 3. histidine metab |
|
|
what happens when B9 deficient?
|
1. megaloblastic anemia
2. inc. homocysteine (risk factor for CV diseases) 3. neural tube defects e.g. spina bifida |
|
|
what's B12?
|

cobalamin; methylation rxns:
Uracil to thymidine Homocysteine to methionine (methionine synthetase) Aminoethanol to choline |
|
|
what is B7?
|

biotin (cofactor for carboxylases)
|
|
|
what is vit C for?
|
Coenzyme in hydroxylation rxn:
1. Collagen syn: Pro/Lys -> OH-Pro / OH-Lys 2. Conversion cholesterol to bile acid 3. Catecholamine biosynthesis from tyrosine 4. Coenzyme in amidation of certain peptide hormones 5. reduce reactive oxidizing agents and free radicals |
|
|
what is vit K for?
|
post-txn modification of clotting factors
(e.g. syn of prothrombin) required for osteocalcin (in bone for mineralization/turnover) Anticoagulants interfere with Vitamin K action (eg. Warfarin) |
|
|
retinal vs retinol?
animal vs plant vitamin A? |
Retinol: storage and binding form
Retinal: active form in retina Retinyl esters- in animal fat beta-Carotene (provitamin A) - in plants (both converted to absorbed as retinol in gut) |
|
|
where is vitamin A stored?
|
Ito/Stellate cells in liver
(stored as retinyl palmitate) |
|
|
which vitamin, when in excess, is a teratogen?
|
vit A
|
|
|
what receptors does vitA bind to?
|
nuc receptors RAR/RXR -> txn
(vit A, along with vit D, bind to nuclear receptors) |
|
|
vision and vit A?
|
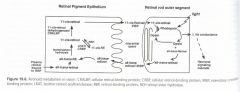
retinol -> retinal (required for opsin -> rhodopsin, light: rhodopsin -> opsin -> inc. Na conductance and firing of neuron)
rhodopsin (the visual pigment of rod and cone cells) has 11-cis retinal which is bound to OPSIN....when rhodopsin exposed to light-->release of trans retinal and opsin) |
|
|
which vitamin can help reduce blood pressure (HT)?
|
vitamin D ( ---| renin, which makes AngII, which inc. water retention and thus BP)
|
|
|
99% of body's Ca is in bone as what?
|
hydroxyapatite 3Ca3(PO4)2.Ca(OH)2
|
|
|
what are the functions of Ca?
|
0. bone! (99%)
1. second msger 2. neural conduction and mm contraction 3. cofactor for enz (eg PKC, panc lipase) 4. blood clotting 5. signal transduction |
|
|
contraction of hands (tetany) is often characteristic of deficiency of which mineral?
|
Ca (often following Mg def)
|
|
|
which mineral acts as a buffer for acid/base regulation
|
phosphorus
|
|
|
t/f
phosphorus is ingested as inorganic phosphate from food, and taken into cell as organic phosphate |
FALSE
dietary organic phosphorus -> (phosphatase) Pi |
|
|
t/f
most dietary Mg is absorbed in intestine |
false
only 40-45% abs'ed, others feces |
|
|
how is Mg excreted?
|
urine (40%) and perspiration (up to 25%)
|
|
|
what are the main functions of Mg?
|
1. involved in metab rxn (enz interactions, involved in ATP utilization)
2. important for function of some ion channels 3. structural modifications of nuc acids and membranes |
|
|
t/f
insulin facilitates net transport of K out of the cell |
FALSE
|
|
|
what mineral imbalance are these symptoms characteristic of:
ECG changes with potential arrhythmias Skeletal muscle necrosis Metabolic alkalosis |
hypokalemia
|
|
|
what mineral imbalance are these symptoms characteristic of:
Paralysis of skeletal muscle Mental confusion Abnormal cardiac rhythm leading to possible cardiac arrest (def of paralysis: Paralysis is caused by membrane depolarization triggering sodium channel inactivation, which renders the membrane inexcitable) |
hyperkalemia
|
|
|
what are the major functions of iron?
|
1. heme: hemoglobin, myoglobin, cytochrome oxidase in ETC
2. Component of peroxidase enzymes for protecting cells from oxidative injury 3. iron-regulated gene expression |
|
|
why is iron toxic to cells?
|
formation of hydroxyl radicals [Fenton reaction] (ferrous iron + hydrogen peroxide)
(1) Fe2+ + H2O2 → Fe3+ + OH· + OH− (2) Fe3+ + H2O2 → Fe2+ + OOH· + H+ |
|
|
describe iron homeostasis regulated by IRP-1 (iron regulatory protein)
|

low-iron: reduce syn of ferritin (iron storage protein); inc expression of transferrin receptor protein (brings iron into the cell)
(IRP= iron regulatory protein) |
|
|
what are the symptoms of iron deficiency?
|
anemia, pallor, fatigue, coldness, and susceptibility to infection
|
|
|
which mineral is required for the action of carbonic anhydrase?
|
zinc
|
|
|
what are zinc fingers?
|
binding domains (usually on txn factors for binding to DNA)
|
|
|
what inhibit the absorption of zinc?
|
high iron and phytate (IP6, storage-form phosphorus in plants e.g. bran and seeds)
|
|
|
what happens when zinc deficient?
|

dermatitis, lesions on pressure points.
|
|
|
what are the functions of Copper?
|
1. redox
2. cross-linking of collagen and elastin 3. iron metab and erythrogenesis 4. formation and maintanence of myelin 5. synthesis of melanin |
|
|
where is copper stored in the body?
|
mainly in liver associated with metallothioneins
(circulate in serum bound to albumin and ceruloplasmin) |
|
|
what's the main route of excretion for copper?
|
bile
|
|
|
t/f
high zinc inhibits copper absorption |
true
|
|
|
which mineral prevents Keshan disease (cardiomyopathy)?
|
selenium (needed for glutathione peroxidase and Iodothyronine deiodinases)
|
|
|
|
|
|
how can we assess nutrition/growth?
examples of direct measurements? indices? |
Direct Measurements: Weight, length/height, circumferences, skin-folds, extremity lengths etc
Indices: weight-for-length (age birth – 3-y); Body mass index, kg/m2 (age 2 – 20 Biochemical indices: Pre-albumin, Albumin, plasma/tissue micronutrient concentrations |
|
|
Malnutrition is the deviation from normal growth
give me some types |
FAILURE TO THRIVE (FTT); wasting:
Length, weight, weight-for-length, BMI: < 3rd percentile (<-2 SD) Weight or height drop > 2 major percentile channels STUNTING Length or height < 3rd percentile RISK FOR OVERWEIGHT: Weight-for-length or BMI: 85th - 95th percentile OVERWEIGHT Weight-for-length or BMI: >95th percentile (>2 SD) |
|
|
choose from
-Estimated Average Requirement (EAR) -Recommended Dietary Allowance (RDA) -Adequate Intake (AI) Level of intake for which the risk for inadequacy is 50% |
-Estimated Average Requirement (EAR)
|
|
|
Level of intake 2 SD above the EAR, covering 97% of the population
|
-Recommended Dietary Allowance (RDA)
|
|
|
choose from
-Estimated Average Requirement (EAR) -Recommended Dietary Allowance (RDA) -Adequate Intake (AI) Recommended intake where EAR cannot be established |
-Adequate Intake (AI)
|
|
|
The highest level of daily nutrient intake that is likely to pose NO risk of adverse health effects
These levels are available for several minerals and vitamins e.g., Fluoride, Iron & Fat soluble vitamins (A, D, E) |
tolerable upper limit (UL)
|
|
|
________ provides the amino acids required for synthesis of body proteins and other nitrogenous compounds with important functional roles e.g., glutathione, heme, creatinine, nucleotides and nuerotransmitters.
|
dietary proteins
|
|
|
what are the determinants of RDA for protein?
|
Lowest level of intake needed to replace losses (Average physiological requirement)
Digestibility and amino acid pattern in protein (protein quality) Individual variability in protein needs |
|

what's the true digestibility?
|
True Digestibility = [N intake – (Fecal N on test protein & non protein diet) x 100]/Nitrogen intake
|
|
|
define
E-Intake = Digestible-E = Metabolizable-E = |
E-Intake = E-Expenditure + E-storage + E-losses
Digestible-E = Gross E-intake – E-losses in feces Metabolizable-E = Gross E-Intake – (E-losses in feces + urine) Food labels = Metabolizable-E |
|
|
Food labels show which kind of energy?
|
Metabolizable-E
|
|
|
Colostrum is produced when?
|
birth to ~ 4th day of life
Colostrum (also known as beestings or first milk or "immune milk") is a form of milk produced by the mammary glands of mammals in late pregnancy and the few days after giving birth. Colostrum is high in carbohydrates, protein, and antibodies and low in fat (as human newborns may find fat difficult to digest). Newborns have very small digestive systems, and colostrum delivers its nutrients in a very concentrated low-volume form. It has a mild laxative effect, encouraging the passing of the baby's first stool, which is called meconium. This clears excess bilirubin, a waste product of dead red blood cells which is produced in large quantities at birth due to blood volume reduction, from the infant's body and helps prevent jaundice. In humans and mice, colostrum contains immunoglobulins such as IgA and IgM. IgA will be absorbed through the intestinal epithelial, travel through the blood and will be secreted onto other Type 1 mucosal surfaces. |
|
|
of mature milk, what's the:
proteins: CHO: fat: |
Mature Milk:
Protein is whey, casein, lactalbumin, lactoferrin, immunoglobulins, IgA CHO: Lactose, oligosaccharides Fat: Palmitic, linoleic & linolenic, arachidonic acid (AA) & docohexanoic (DHA) fatty acids |
|
|
Prolonged / exclusive breast feeding for first few months of life is associated with
|
Accelerated neuro-cognitive development
|
|
|
what are some guidelines for feeding babies?
|
Order of food introduction does not matter
One single-food (mashed or puréed’) per week Limit fruit juice to 4 – 6 oz/d (<250 mL/d) No added salt or sugar Avoid whole milk before age 12-months (bioavailability of Fe + GI occult blood loss) Avoid aspiration risk foods <4 y: Hot dogs, nuts, grapes, raisins, raw carrots, pop corn, round candy |
|
|
Peri-conceptional Folic acid deficiency increases risk for congenital _________
|
neural tube defects
|
|
|
what are some foods rich in folate?
|
Foods rich in folate: green vegetables, spinach, turnip greens, citrus fruits, dried beans & peas
|
|
|
Excessive consumption of cow milk in toddlers is associated with what? (2 things)
|
Fe++ def & dec albumin (hypoalbuminemia)
|
|
|
16 month old pale, edematous child with a microcytic anemia (Hgb 6 g/dl), hypoalbuminemia (1.8 g/dl), and excess milk intake
what's the problem? |
Excessive consumption of cow milk in toddlers is associated with Fe++ def & dec albumin
breast milk: low iron, but also high bioavailability cow milk: low iron AND low bioavailability |
|
|
what are the consequences of Fe deficiency?
|
Microcytic anemia
Fatigue, lethargy, cognitive and motor deficits, poor school performance inc risk for irreversible developmental delays Fe def results in increased absorption of lead |
|
|
to avoid Fe deficiency:
Breast fed infants should be supplemented with Fe fortified foods starting at 4 – 6 months Use only Fe fortified formulas during 1st year Screen (Hemoglobin) at 9-12 m, 15-18 m & adolescent females Avoid ____, ____, and ____milk before 1-yr Limit cow milk intake to ≤24 oz/day |
cow, goat, soy
|
|
|
how do we classify overweight and risk for overweight?
(Recommended CDC terminology is “overweight” not ‘obesity) |
Risk for overweight: BMI 85th – 95th percentile
Overweight: BMI >95th percentile BMI >95th percentile correlates with morbidity |
|
|
what are the critical Periods for Onset of persistent Overweight?
|
Fetal Life
Early age at Adiposity Rebound: <5 - 7 yr. Adolescence |
|
|
Infants of ________ mothers at highest risk to become overweight
|
diabetic
|
|
|
what's adiposity rebound?
|
Period of regaining body fat after loss of baby fat
|
|
|
t/f
late onset of adiposity rebound <5.5-yr, is associated with persistent overweight into adolescence and adulthood. |
false
early onset |
|
|
what's failure to thrive (FTT) and its types?
|
Most often in age ≤3-y; represents inadequate nutrition
Non-organic FTT: No disease: - limited parental skills, psycho-social circumstances Organic FTT: Primary disease induced poor growth Mixed FTT: disease & psycho-social factors another classification scheme: Primary (insufficient food intake): Environmental (care takers) vs. problem inherent to child e.g. neurological, behavioral, restricted diets Secondary (disease): Vomiting, fecal losses (maldigestion, malabsorption, pancreatic, hepatobiliary disorders) other disease Mixed: Disease and insufficient food intake |
|
|
in FTT, the ____ is more affected than ______ more affected than __________
|
Weight more affected than Length more affected than Head circumference
|
|
|
what are the risk factors for dental caries?
|
Risk factors:
Infants sleeping with milk bottle Toddler’s constantly drinking milk or sweet beverages from baby bottle |
|
|
how to treat dental caries?
|
Fluorinated toothpaste
Avoid frequent feeding sweet beverages Wean toddlers off the baby bottle |
|
|
t/f
pregnant women should eat lots of seafood |
false!
Pregnant women are advised to limit their intake of swordfish, shark, marlin, large tuna, king mackerel, and tilefish. |
|
|
Vitamin D toxicity can lead to infantile __________
|
hypercalcemia syndrome.
|
|
|
can pregnant women meet iron requirements by diet alone?
|
difficult...should take supplements
|
|
|
_____, craving for non-foods, is seen occasionally with iron-deficiency anemia.
When a patient is diagnosed with iron-deficiency anemia, screen for ______ |
pica
|
|
|
t/f
the less you weigh, the more you'll gain in pregnancy |
true
1st trimester 2-5 lbs total 2nd & 3rd trimesters: 1+lb week until delivery: underweight/teens/multiple gestation 1lb week until delivery: normal weight <1lb week until delivery: overweight/obese |
|
|
what are some tips to reduce morning sickness?
|
Dietary tips to help minimize symptoms:
eat frequent small meals avoid an empty stomach eat dry,starchy foods before getting out of bed drink liquids between meals avoid fried, greasy, and spicy foods |
|
|
what can cause constipation in the 2nd and 3rd trimesters?
|
caused by delayed gastric emptying, not enough fiber in diet or lack of exercise. Iron supplementation also may increase occurrence.
Eat high fiber foods:raw fruits&vegetables, enriched breads and grains. 8-10 glasses of fluid (water,juice,milk) Prune juice. |
|
|
what causes heartburn in the 2nd and 3rd trimesters?
|
general gastric pressure due to lack of normal space.
Avoid greasy or fatty foods Avoid highly spicy or acidic foods Eat several small meals instead of large ones Avoid lying flat for 1-2 hrs after eating |
|
|
what's hyperemesis?
|
Intractable vomiting in pregnancy that causes dehydration, electrolyte disturbances, nutritional deficiencies, and weight loss during the 1st trimester.
Occurs in 1/1000 pregnancies Treatment: IV Hydration, Antiemetic medication, Diet (NPO advancing to general diet as tolerated or Nutritional Support). |
|
|
for someone with hyperemesis, when is nutritional support indicated?
|
Nutrition Support is indicated:
inability to take adequate oral intake weight loss greater than 1kg/week for 4 weeks consecutively low prepregnancy weight/low weight gain Intrauterine growth retardation Nutritional biochemical marker abnormalities: negative nitrogen balance,persistent ketosis, hypoalbumenia, anemia, hypocholesterolemia |
|
|
when is enteral support indicated for someone with hyperemesis?
|
If no contraindications for enteral support are noted and if access can be obtained with minimal physical or psychological trauma.
Positive outcomes noted in patients. Small bore feeding tubes placed intragastrically or other nasogastric tubes placed post-pylorically under fluoroscopy. Iso-osmolar feeds infused continuously at a low rate via pump and advanced to goal rate. |
|
|
when is Peripheral Parenteral Nutrition indicated for someone with hyperemesis?
|
indicated when support needed for < 10days.
If >10days, increase risk for phlebitis. Total Parenteral Nutrition: indicated when support is long-term (>10 days). At risk for complications: infection or thrombosis at catheter site, sepsis, and metabolic imbalances. |
|
|
what's gestational diabetes?
|
Any degree of glucose intolerance with onset during pregnancy
Definition applies whether insulin or diet modification is used for treatment & whether or not the condition persists after pregnancy. 4% all pregnancies complicated with GDM |
|
|
how do we treat gestational diabetes?
|
Maintenance of near normal blood glucose level as possible by balancing food intake with insulin and exercise.
Provision of adequate calories to meet increased metabolic needs with pregnancy Prevention and treatment of acute complications of hypoglycemia, hyperglycemia, and short-term illness. |
|
|
Factors that predispose infant to IUGR (Intrauterine Growth Failure)
|
Chronic Hypertension
Preeclampsia Infections “TORCH” Maternal pregnancy wt and wt gain Maternal smoking Alcohol use in 2nd or 3rd trimesters Multiple gestation |
|
|
how is extrinsic IUGR cause?
|
Extrinsic IUGR is usually manifested by placentas that are reduced in size, which indicates they were incapable of supplying the fetus with adequate nutrition.
--severe protein restriction of mother’s diet to reduce supply of nutrients available for the synthesis of placental and fetal cells. |
|
|
consequences of malnutrition for the fetus depend on the timing, severity, & duration of the maternal dietary restriction.
These consequences may be reversible if the restriction primarily affects growth in _____, but a restriction in the number of cells may be permanent if the restriction is maintained throughout the entire period of hyerplastic growth. |
cell size
|
|
|
t/f
Teens who become pregnant < 4yrs after menarche are at high nutrition risk d/t meeting needs of their own growth as well as energy and nutrient demands of pregnancy. |
true
|
|
|
w/breastfeeding, there is a lower incidence of:
|
lower incidence of:
colic obesity coronary disease otitis media diabetes parasite infections food allergies respiratory infections obesity viral infections |
|
|
t/f
there's a correlation bw serum cholesterol level and CAD risk |

true
|
|
|
Dietary fat includes both
|
saturated and unsaturated fatty acids.
|
|
|
- A diet high in fat is generally high in _______
|
calories
Reduction of total fat to < 30% of total calories helps to control both calories and saturated fat intake. |
|
|
tell me how fats (different types) change LDL, HDL, and triglyceride levels
|
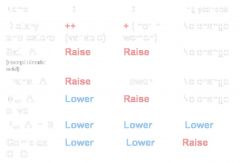
|
|
|
what are trans fatty acids?
|
Formed from the hydrogenation of liquid oils to fats. These are solid at room temperature.
Studies suggest that trans fatty acids raise total and LDL cholesterol levels. Current US intake in the U.S. diet is 2 to 4% of total calories. Found in processed foods-as hydrogenated vegetable oil Used by the food industry to increase shelf-life and flavor in produces such as snack foods, baked products, margarine, and french fries. so trans fat is CHEMICALLY unsaturated...but it basically behaves like saturated fats broken down into saturated and unsaturated unsaturated further broken into mono and poly unsaturated poly unsaturated further broken into n-3, n-6 fatty acids |
|
|
what are the pros/cons of a low-carb diet? (like the Atkins)
|

|
|
|
compare weight loss from low-carb and low-fat diets, at the 6 mnth and 1 yr mark
|
6 months
Greater weight loss in low-carbohydrate dieters 1 Year Mark No significant Difference in Weight Loss |
|
|
LOW-CARB diet:
Short term weight loss may be result of ______ Weight Loss also linked to initial baseline weight, age, and duration of diet Possibly increase HDL and decrease triglycerides May have beneficial effect on glucose levels (especially in diabetics) and short term effect on insulin sensitivity |
caloric restriction
|
|
|
what's the Mediterranean Diet?
|
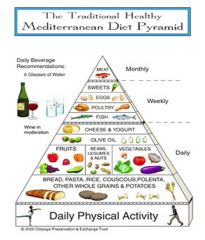
Abundance of Plant Food
Fruits, Vegetables, Nuts, Beans, Legumes Whole-Grain Cereal, Bread, Potatoes Olive Oil as Principle Fat Source Fish, Poultry, Dairy Products Low-Moderate Amounts Low Consumption of Red Meat Eggs consumed 0-4 times weekly Moderate Alcohol Consumption (Wine with Meals) |
|
|
what are Omega-3 Fatty Acids?
|
Eicosapentaenoic Acid (C20:5n-3), EPA
Docosahexaenoic Acid (C22:6n-3), DHA --Major Source is Fatty Fish Salmon, Mackerel, Herring, Trout alpha-linolenic acid (C18:3n-3), ALA -Major food sources are vegetable oils such as canola, flaxseed and soybean oil -Flaxseed, English walnuts, Mustard Oil |
|
|
does the Mediterranean Diet have
cardioprotective effects? |
yes
Early Separation of Survival Curves Protective against acute and fatal MI Consistent Basic Science and Clinical Trial Evidence |
|
|
Lower sodium intake requires food industry change
75% sodium intake comes from additions made in processing |
don't eat processed foods!!
|
|
|
Poverty -> malnutrition-> ___________
|
increases the risk and consequences of infectious diseases
|
|

|
poverty and malnutrition are related
|
|
|
Kwashiorkor – _______ malnutrition
Marasmus – _______ and _________ malnutrition |
Kwashiorkor – protein malnutrition
Marasmus – protein and calorie malnutrition In marasmus, energy and protein are deficient- occurs in a young child- 6 months to 1 year Kwashiorkor- occurs in an older child 1-5 years In Kwashiorkor, there is adequate energy intake but inadequate protein to meet the needs of growth and development This decreased protein intake leads to decreased visceral protein synthesis along with edema and fatty liver Marasmic infants show hunger, gross weight loss, wasting, loss of subcutaneous fat, flaky paint dermatosis and apathy Mortality varies between 15-40% CMI is impaired but humoral immunity is normal |
|
|
Kwashiorkor
Low protein intake relative to needs with adequate calories Appear well nourished, edema is common, hair is easily plucked Labs – low albumin, transferrin and lymphocytes High mortality, often due to _______ |
infection
|
|
|
marasmus
Low protein and calorie intake relative to needs Starved, wasted appearance Weight < 80% of ideal body weight Low serum creatinine...what about albumin levels in marasmus? |
albumin falsely normal due to dec blood volume
|
|
|
glucose is produced by the liver AND the _______
|
kidney
|
|
|
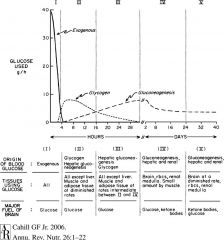
Five Metabolic stages between the post absorptive and prolonged starvation
|
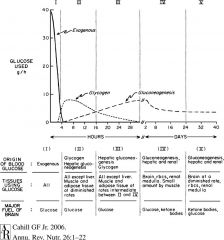
|
|
|
what does the brain use for fuel in starvation?
|
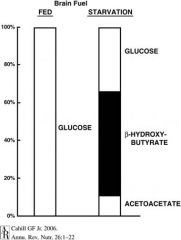
glucose + ketones
|
|
|
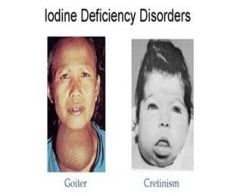
Iodine deficiency is associated with ______
|
cretinism
Cretinism is a condition of severely stunted physical and mental growth due to untreated congenital deficiency of thyroid hormones (hypothyroidism) or from prolonged nutritional deficiency of iodine |
|
|
most common cause of blindness in developing countries?
|
vitamin A deficiency
|
|
|
Most common anemia throughout the world. – 40% of worlds women have this anemia
|
microcytic anemia (most common form of anemia)
More common in infancy due to low iron levels in both human and cow milk Low meat intake and parasitic infections also contribute anemia= low Hg types: mcrocytic, normocytic, macrocytic based on size of RBC microcytic caused either by def in iron, coppor, pyridoxine |
|
|
how do you manage people with severe protein-energy malnutrition
|
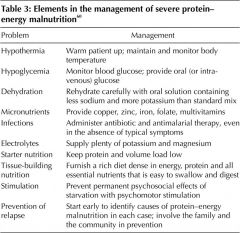
|
|
|
Food insecure households have_______rates of obesity and BMI’s > 30
|
higher
|
|
|
define anorexia
|
Anorexia is characterized by a refusal to maintain a minimally healthy body weight, most often by severely restricting what one eats.
|
|
|
define bulemia
|
bulimia is characterized by a pattern of binge eating followed by drastic attempts to avoid weight gain by engaging in self-induced vomiting, fasting, exercising, etc. With both disorders, the individual's primary means of self-evaluation is through shape and weight.
|
|
|
t/f
postmenarcheal females with anorexia may have amenorrhea for at least three cycles |
t
|
|
|
t/f
In 50% of cases, anorexia nervosa is prior to bulemia nervosa |
false
In ca. 50% of cases, BN is prior anorexia nervosa |
|
|
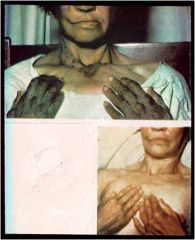
the dermatological effects below are of what disorder?
Dry skin Lanugo Acrocyanosis Brittle hair/nails Hypercarotenemia |
anorexia
|
|
|
the dermatological effects below are of what disorder?
Abrasions on dorsum of hand-Russell’s sign Dental caries Facial purpura |
bulimia
|
|
|
what's lanugo?
|
soft, downy, fine white hair that grows mainly on the arms and chests of female anorexics.
|
|

patients with which eating disorder would have parotid gland swelling?
|
both bulimia & anorexia
|
|
|
why is there low estrogen produced in anorexics?
|
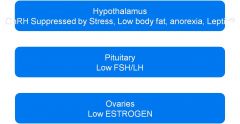
|
|
|
t/f all anorexic women with amenorrhea are infertile
|
false
in anorexia, infertility common, but fertility is possible even with amenorrhea. Long-term fertility is normal with weight recovery. Pregnancy complications-low birth weight, miscarriage, premature birth, prenatal death, Cesarean section, post-partum depression. Restriction associated with LBW. Outcomes generally good. |
|
|
what happens to bones of anorexic patients?
|
Osteopenia-Decreased bone mass in 90% of patients
Osteoporosis-Decreased bone mass with risk of fracture present in 40-50% of patients. May be seen in first six months of illness. Associated with increased resorption and decreased bone formation. |
|
|
t/f
after recovery from anorexia, patients no longer are at risk of fracture |
false
Lifelong risk of fracture even after recovery Monitor bone density every 12-24 months until improvement. Treatment Weight restoration Vitamin D 800-1000 IU/day Calcium 1500 mg/day Low impact exercise |
|
|
what are some neurological effects of anorexia?
|
peripheral neuropathy
seizures and cortical atrophy |
|
|
what are poor prognostic factors of eating disorders?
|
later age at onset of the disorder,
binge-purge behavior, and concurrent mood disorders |
|
|
what's the Russell's sign?
|

sign defined as scarring on the knuckles or back of the hand due to repeated self-induced vomiting over long periods of time. The condition generally arises from the afflicted's knuckles making contact with the incisor teeth during the act of inducing the gag reflex at the back of the throat with their finger(s).
This type of scarring is considered one of the physical indicators of a mental illness, and Russell's sign is primarily found in patients with an eating disorder such as bulimia nervosa or anorexia nervosa. However, it is not always a reliable indicator of an eating disorder. Russell's sign may be dermatologically treated with urea. |

