![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
Compare and Contrast angiocatheters and butterfly needles. When is each used appropriately?
|
Angiocatheters
- soft, pliable, move with person - less risk of infiltration Butterfly Needle - rigid, tiny gauge, more risk of infiltration - used in pediatrics to access foot and scalp veins - used by lab to draw blood. |
|
|
Local Complications of IV Therapy
Infiltration Describe it and what the nursing action is... |

Infiltration
* swelling * discomfort * burning * tightness * cool skin * blanching. Nursing -* Stop the infusion and remove the device (unless the medication is a vesicant; consult the health care provider and pharmacy). * Elevate the limb to increase patient comfort. * Check the patient's pulse and capillary refill time. * Counteract the effects of the drug as ordered. * Perform venipuncture in a different location and restart the infusion. * Check the site frequently. * Document |
|
|
Local Complications of IV Therapy
Phlebitiis Describe it and what the nursing action is... |

Phlebitis: nasty, ugly, red, widespread
* redness or tenderness at the tip of the catheter * puffy area over the vein * elevated temperature. Nursing: * At the first sign of redness or tenderness, stop the infusion. * To ease your patient's discomfort, apply warm packs. * Document your patient's condition and interventions. * If indicated, insert a new catheter at a different site, preferably on the opposite arm, using a larger vein or a smaller device and restart the infusion. |
|
|
Local Complications of IV Therapy
Extravasion Describe it and what the nursing action is.. |

Extravasation, the leaking of vesicant drugs (such as antineoplastics) into surrounding tissue, can cause severe local tissue damage, resulting in delayed healing, infection, tissue necrosis, disfigurement, loss of function, and even amputation.
S/S * blanching, burning, or discomfort at the I.V. site * cool skin around the I.V. site * swelling at or above the I.V. site. Nursing * Stop the I.V. flow: the catheter may need to remain in place to administer the antidote. * Estimate the amount of extravasated solution and notify the health care provider. * Instill the appropriate antidote according to your facility's protocol. * Elevate the extremity. * Record the extravasation site, your patient's symptoms, the estimated amount of extravasated solution, and the treatment. |
|
|
Systemic Complications of IV Therapy:
Speed Shock What is is and what are the nursing responsibilities? |
Speed Shock
a sudden adverse physiologic reaction to IV medications or drugs that are administered too quickly. S/S flushed face, headache, a tight feeling in the chest, irregular pulse, drop in BP, loss of consciousness, and cardiac arrest. (she said more common in peds) |
|
|
Systemic Complications of IV Therapy:
Embolus What is is and what are the nursing responsibilities? |
A blood clot or other solid mass, as well as an air bubble, can be delivered into the circulation through an IV and end up blocking a vessel.
"vascular collapse due to occlusion". - symptoms depend on where. - dyspnea, cyanosis, hypotension, weak, rapid pulse, loss of consciousness, shock, death. if AIR embolus: put on left side, trendelenburg. (air goes to right atrium - top of heart - will be trapped and dissipate. |
|
|
What are the functions (2) of the drip chamber in the IV tubing set up?
|
A drip chamber prevents air from entering the blood stream (air embolism), and allows an estimation of flow rate.
|
|
|
Why are IV's started in the veins instead of in the arteries?
|
One reason veins are preferred over arteries for intravascular administration is because the flow will pass through the lungs before passing through the body
|
|
|
What is a Push (or bolus) injection of a drug?
What are the potential problems and nursing responsibilities? |
Push (or bolus) injection of a drug into an appropriate-size vein is a fast, effective method to deliver medications.
- direct into bloodstream = dangerous Nursing: - If the drug has an antidote, know its location & dosage - If the drug has no antidote, know supportive measures you should initiate to minimize adverse reactions - pain or irritation at the site because drug may be irritating, or the increased pressure may cause pain - venous or arterial spasm: cramping & pain above the infusion site Nursing - dilute the medication and slow the push rate. Or, if possible, administer by infusion |
|
|
What is a buretrol and why is is used?
|

A buretrol is a type of infusion device that holds limited quantities of IV fluids or medications. It is generally used for pediatrics and often is designed to prevent free flow of fluids or air once the infusion is done (children are less able to handle large fluid influxes like adults can). The IV fluids are attached above the buretrol and refilled manually as the volume decreases.
|
|
|
Describe some nursing actions for Central Lines....
|
- post insertion: chest xray to confirm.
- use occlusive dressing - after insertion, assess breath sounds - incase MD injured lungs while inserting. - flush Q shift to maintain patency - monitor circulation; hematoma formation - change tubing per agency - document insertion site, flushing, dressing. - if port becomes clogged, can open with Urokinase |
|
|
What do you know about PICC lines?
Into what veins do PICC lines get inserted? (3) |
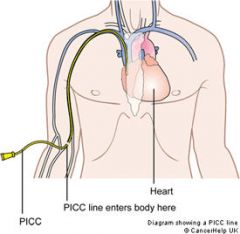
PICC Line: inserted through a peripheral vein, preferably in the upper arm, and advanced until the tip of the catheter reaches a large vein above the heart.
- can stay in place for as long as needed & up to one year if properly maintained. - median cephalic vein - basilic vein - cephalic vein |
|
|
What do you know about central catheters?
Into what veins do most central catheters get inserted? (3) |
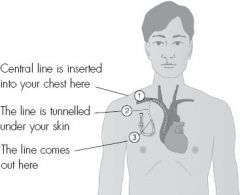
a catheter placed into a large vein in the neck (internal jugular vein or external jugular vein), chest (subclavian vein or axillary vein) or groin (femoral vein). It is used to administer medication or fluids, obtain blood tests (specifically the "mixed venous oxygen saturation"), and directly obtain cardiovascular measurements such as the central venous pressure.
|
|
|
How do you know which IV solution to choose?
|
The choice depends on its purpose:
1. to provide water, electrolytes, nutrients for daily needs 2. to replace water & correct electrolyte imbalances 3. to give meds & blood products |
|
|
Why would you NEVER give pure water intravenously?
|
- pure water would rapidly enter red blood cells and cause them to rupture.
|
|
|
What would you use to correct dehydration, sodium depletion, and GI losses?
|
Brunner: lactated ringers.
BECAUSE isotonic solutions expand the ECF. |
|
|
When NOT to give an isotonic solution?
|
Brunner: do NOT give isotonic solution
- heart failure - pulmonary edema - renal impairment - sodium retention BECAUSE isotonic solutions expand the ECF. |
|
|
What's the difference between a catheter and a cannula?
|
nothing. the terms are used interchangeably.
|
|
|
What are (4) reasons for placing a central catheter?
|
1. long term IV therapy
2. TPN 3. vasopressors 4. pt has no other good peripheral veins. |
|
|
What are some factors that effect flow rate? (4)
|
Brunner - flow rate
- height of liquid: raise to increase flow rate - diameter of tube: clamp on IV tubing regulates flow because it changes tube diameter. - length of tube: adding extension tubing decreases rate. - viscosity: eg. blood requires larger cannula than saline. |
|
|
What is the purpose of flushing "vascular devices"?
|
Brunner:
flushing ensures patency and prevents the mixing of incompatible medications. |
|
|
When removing an IV catheter - what are two possible dangers? What are the nursing actions to take to prevent/address these?
|
Brunner:
1. bleeding: put on dry sterile pressure dressing and 2. catheter embolism: if a piece of the catheter itself breaks off and travels to right ventricle, blocking blood flow. Nursing: compare expected length with actual length extracted. If catheter has been severed, nurse can apply tourniquet above the site to prevent catheter from entering central circulation until surgical removal is possible. Prevention: - avoid using scissors near catheter. - avoid withdrawing cath through insertion needle |
|
|
What's the difference between fluid overload and circulatory overload?
|
Brunner:
- circulatory overload is fluid overload in elderly with cardiac disease. - fluid overload: from rapid infusion or liver, kidney, heart disease. - treat: decrease rate, high Fowler's, call MD, monitor - avoid: use pump; monitor |
|
|
One more time:
What are the signs and symptoms of fluid overload? |
Brunner:
- 10 empty wine bottles. Just kddin' - increased BP - moist crackles - edema, weight gain - dyspnea, rapid shallow respirations |
|
|
Another systemic (or local) complication of IV therapy is infection. Give some S/S of systemic infection related to IV therapy (8)
|
Brunner
- abrupt high temp after starting IV - backache - headache - increased pulse, respirations - N/V/diarrhea - chills, shaking - general malaise could lead to vascular collapse, septic shock |
|
|
G's Q: why does a person take anticoagulants?
|
Because they have venous stasis.
due to surgery or mobility factors. Want to stretch out the process of clotting. |
|

Name this hernia!
|
Femoral Hernia
Most often in women. Area weakened b/c of pregnancies (or gymnastics) |
|
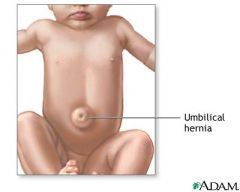
Name that Hernia!
|
Umbilical. Usu in babies - congenital. could also be from undue pressure or strain on area.
|
|

Name that Hernia!
|
Incisional hernia
|
|

Name that Hernia!
|
Inguinal Hernia - men mostly - canal where testes descends and sperm cord goes thru.
|
|
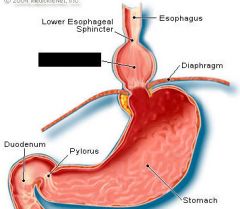
Name that Hernia!
|
Hiatal Hernia
|
|

no question, just a cool pix
|
:)
|
|
|
GERD is treated with three classes of meds. What are they? Can you give an example of a drug in each category?
|
- Antacids (neutralize the acid in the stomach so that there is no acid to reflux; action is brief: Milk of Magnesia, maalox, mylanta
- H2 Receptor Blockers (block acid production): tagament, prevacid, pepsin, zantac - Proton Pump Inhibitors (block acid AND heal): prilosec, protonix, purple pill nexium - Proton Pump Inhibitors |
|
|
In appendicitis, what is the name of the place where acute pain is felt in the RLQ?
|
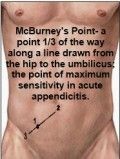
McBurney's Point
|
|
|
What's the difference between diverticulosis and diverticulitis?
|
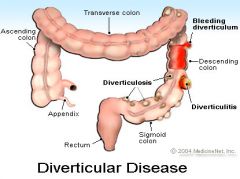
-osis = UNinflamed. outpouch. increasingly common in lower colon as we age.
- itis = inflammation & infection of the diverticulosis. caused by low fiber diet and/or weak intestinal wall. |
|
|
What class of drugs is used to treat diverticulitis, chron's disease and irritable bowel syndrome? Can you name an example?
|
Anti-cholinergics. Ex. Pro-Banthine (propantheline). will reduce secretions of certain organs, eg. stomach. Also Bentyl Dicyclomine for cholecystitis is an anit-cholinergic. It reduces muscle contractions in intestine.
|
|
|
Name a procedure that is done when there is perforation in diverticulitis.
|
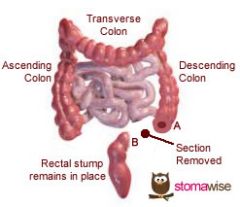
- Heartman's Procedure.
- resection of colon - closed distal stump - may be brought to surface. - can be temporary, depends on location and how widespread |
|
|
How much fiber do we need a day?
|
about 30 grams
|
|
|
What is Intussusception? Who gets it most?
|
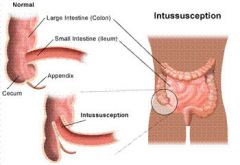
Intussusception is the most common cause of intestinal obstruction in children between ages three months and three years. Male babies are affected four times as often as female babies. Intussusception occurs when a portion of the intestine folds like a telescope, with one segment slipping inside another segment. This causes an obstruction, preventing the passage of food that is being digested through the intestine. The walls of the two "telescoped" sections of intestine press on each other, causing irritation and swelling. Eventually, the blood supply to that area is cut off, which can cause damage to the intestine.
|
|
|
What are adhesions?
|
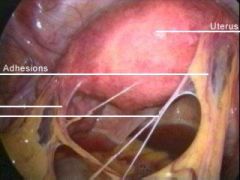
intestines (or other organs) tacked to each other by bands of fibrous glue. They lead to obstructions when they form circular bands around intestine. Acts like a tourniquet.
|
|
|
What is obstipation (yes, I spelled it right)
|
obstipation is Intestinal obstruction; severe constipation.
|
|
|
What is the standard sign of cholecystitis?
|

Murphy's sign:
This is the standard sign of cholecystitis worldwide. Pain is felt during inhalation or coughing when the physician palpates your RUQ due to the inflammation of the gallbladder. |
|
|
WHY oh why is the prothrombin (clotting time) increased with cholecystitis?
|
PT is increased (normal is 10-14 sec) because vitamin K is needed for clotting. Vitamin K isn't being absorbed because the bile is blocked and not getting to the intestine where Vitamin K is absorbed!
|
|
|
What class of drugs are used to treat cholecystitis? Can you name one?
|
Antispasmodics (anticholinergics). The one she gave us for gall bladder is Bentyl-Dicyclomine: used to reduce contraction of the muscles in the intestines. Another one she gave us (for diverticulitis) is Pro-Banthine.
|
|
|
She gave us four drugs for treating gallstones. What are they and how do they act?
|
Gallstones
1. Mono-octanoin: makes cholesterol soluble, so dissolves cholesterol stones 2. Chenodiol and 3. Ursodiol are made from bile acid: can take months or years to work. 4. MTBE: methyl tertbutyl ether: put directly into gall bladder - can dissolve in 1-3 days. |
|
|
A nonsurgical technique for removing gallstones is ERCP (Endoscopic retrograde cholangiopancreatography) Any ideas on what this is?
|
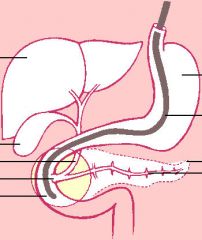
ERCP is used primarily to diagnose and treat conditions of the bile ducts, including gallstones, inflammatory strictures (scars), leaks (from trauma and surgery), and cancer. ERCP combines the use of x rays and an endoscope, which is a long, flexible, lighted tube. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject dyes into the ducts in the biliary tree and pancreas so they can be seen on x rays.
|
|
|
What is a T Tube?
|
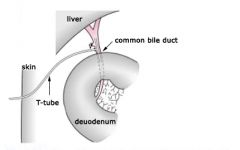
The T-tube allows bile to drain out of the patient's body into a small pouch, known as a bile bag. The amount of bile, which varies in color from deep gold to dark green, can then be measured. If a T-tube is put in place, it may remain attached to a bile bag for a week or possibly longer. When the bile bag is removed the T-tube will be tied or capped. It will remain in place for several months so that it can be used for special testing.
|
|
|
What is a "unique" or important problem with cholecystectomy?
|
Oxygenation - because is is a "high" incision site - patient will find deep breathing and coughing very painful.
|
|
|
One of the reasons hysterectomy is done is because of uterine prolapse. What is this?
|
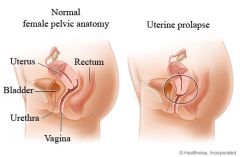
A uterine prolapse occurs when a woman's pelvic muscles and ligaments become weak, causing the uterus to drop from its usual position. This allows the neck of the uterus (cervix) to bulge down into the vagina.
|
|
|
What is a partial hysterectomy? What is left?
|
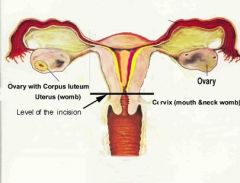
A full hysterectomy involves removing the entire uterus including the cervix, while in a partial hysterectomy the cervix is left intact. Sometimes the ovaries and fallopian tubes are removed at the same time as well, but this is considered a separate procedure.
|
|
|
What part of the body has to be moved in order to do a hysterectomy?
|
ureters. Ureteral injury is one of the most serious complications of gynecologic surgery. Less common than injuries to the bladder or rectum, ureteral injuries are far more serious and troublesome and are often associated with significant morbidity, the formation of ureterovaginal fistulas, and the potential loss of kidney function, especially when recognized postoperatively
|
|
|
What is "vasomotor instability"?
|
hot flashes. All vessels dilate at once.
|
|
|
Name some signs of menopause? (5)
|
- vasomotor instability
- night sweats - mood swings - neurogenital atrophy (lubrication in vagina minimal or nonexistent) - loss of estrogen - accelerated bone loss |

