![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
368 Cards in this Set
- Front
- Back
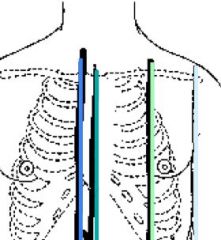
Name the landmark lines for the anterior chest
|
Sternal border, midsternal line, midclavicular line, anterior axillary line
|
|
|
The top of the heart is called __
|
The base
|
|
|
Allen test
|
Determining the patency of the radial and ulnar arteries by compressing one artery site and observing return of skin colors as evidence of patency of the other artery
|
|
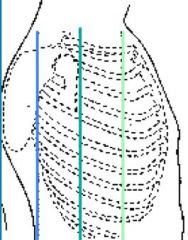
Name the landmark lines for the lateral chest
|
Posterior axillary line, midaxillary line, anterior axillary line
|
|
|
The bottom of the heart is called __
|
The apex
|
|
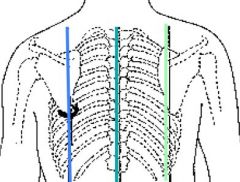
Name the landmark lines for the posterior chest
|
Left scapular line, vertebral line, right vertebral line
|
|
|
What is beating against the chest wall that produces an apical pulse?
|
Apex of the heart
|
|
|
What are the borders of the thoracic cage?
|
The thoracic cage is defined by the sternum, 12 pairs of ribs, and 12 thoracic vertebrae. The diaphragm forms the floor of the thoracic cavity. The intercostal space is named for the rib above it.
|
|
|
What are the great vessels that return unoxygenated blood to the heart?
|
Inferior and superior vena cava
|
|
|
The __ leaves the right ventricle and carries venous blood to the lungs.
|
Pulmonary artery
|
|
|
The __ leaves the lungs and returns freshly oxygenated blood to the heart.
|
Pulmonary vein
|
|
|
The great vessels are comprised of __
|
Inferior and superior vena cava; pulmonary artery and vein; aorta
|
|
|
What is the tough fibrous sac that surrounds and protects the heart?
|
Pericardium
|
|
|
What is cyanosis? What does it look like?
|
Dusky blue mottling of the skin and mucous membranes due to excessive amt of reduced hemoglobin in the blood
|
|
|
The __ is the muscular wall of the heart.
|
Myocardium
|
|
|
The __ is the thin layer of endothelial tissue that lines the inner surface of the heart chambers and valves.
|
Endocardium
|
|
|
Homan's sign
|
Calf pain that occurs when the foot is sharply dorsiflexed (pushed up toward the knee); may occur with deep vein thrombosis, phlebitis, Achilles tendinitis, or muscle injury
|
|
|
The AV valves of the heart separate ___
|
The atria from the ventricles
|
|
|
What is Hypercapnia, Hypoxemia, and Surfactant?
|
• Hypercapnia is the increase of CO2 that stimulates us to breathe
• Hypoxemia is a decrease in O2 in the blood that can stimulate us to breathe, but is less effective than hypercapnia • Surfactant is the complex lipid substance neeed to sustained inflation of the alveoli |
|
|
The right AV valve is called the __ valve
|
Tricuspid
|
|
|
The left AV valve is called the __ valve
|
Mitral
|
|
|
The AV valves open during ___
|
Diastole (filling phase of ventricles)
|
|
|
The right AV valve is called the __ valve
|
Tricuspid
|
|
|
What are three normal breath sounds in their expected region?
|
• Bronchial – Normal over the trachea; loud with harsh sounds, tubular; I<E (inspiration is shorter than expiration)
• Bronchovesicular – Normal over major airways; quieter sound heard over sternum and scapulae; I=E • Vesicular – Normal in peripheral lung fields; I>E |
|
|
The AV valves close during ___
|
Systole (pumping phase)
|
|
|
The left AV valve is called the __ valve
|
Mitral
|
|
|
What are four adventitious sounds that are always abnormal?
|
Crackles (rales): Discontinuous sounds due to fluid in alveoli or alveoli popping open after being compressed; always allow a person to move around/cough, etc. after waking up first thing – some alveoli may have closed while client was sleeping, but will clear up after some deeper breathing – could lead to a false diagnosis
Wheezes: Continuous, high pitched sounds d/t obstructed air flow; typically heard with asthma Rhonchi: Continuous, low pitch type of wheeze; snoring sound; from mucous or fluid in the airway Stridor: From an upper airway obstruction; indicates a medical emergency will soon be happening; ex. Choking on foreign body |
|
|
Where are the semilunar valves located?
|
Between ventricles and arteries
|
|
|
The AV valves open during ___
|
Diastole (filling phase of ventricles)
|
|
|
Pulsus pardoxus
|
Beats have weaker amplitude with respiratory inspiration, stronger with expiration
|
|
|
What are the two semilunar valves and what do they connect?
|
Pulmonic valve - right side of heart (to lungs); aortic valve - left side of heart (to body)
|
|
|
The AV valves close during ___
|
Systole (pumping phase)
|
|
|
Semilunar valves open during __
|
Systole
|
|
|
What six things do we check upon inspection of the thorax?
|
• Perform identification of landmarks, structures, and reference lines
• Include a description of skin including the lips and nails • Include the thoracic configuration and ratio (ex. AP=1:2) • Look at the angle of rib insertion anteriorly an posteriorly (ex. Anterior – horizontal, Posterior – sloped) • Assess the ICS – note any bulging or retractions) • Give a description of the spine |
|
|
Where are the semilunar valves located?
|
Between ventricles and arteries
|
|
|
True or false - there are no valves between the vena cava and the right atrium or between the pulmonary vein and the left atrium.
|
True
|
|
|
What are three general guidelines when percussing the thorax?
|
• Be specific as to sound elicited and location heard. Describe lung borders, techniques, and findings
• Use percussed resonance starting at the apicies and comparing side to side as you work down • Abnormal findings must be at least 2-3 cm wide |
|
|
What are the two semilunar valves and what do they connect?
|
Pulmonic valve - right side of heart (to lungs); aortic valve - left side of heart (to body)
|
|
|
In this phase, the ventricles relax and fill with blood.
|
Diastole
|
|
|
Semilunar valves open during __
|
Systole
|
|
|
True or false - there are no valves between the vena cava and the right atrium or between the pulmonary vein and the left atrium.
|
True
|
|
|
In this phase, the ventricles relax and fill with blood.
|
Diastole
|
|
|
The heart contracts during what phase?
|
Systole
|
|
|
True or false - the atria do not contract.
|
False - the atria have higher pressure at the beginning of diastole, which forces blood into the ventricles; however, towards the end of diastole, the atria contract and push the last amount of blood into the ventricles (atrial kick); so, atrial systole occurs during ventricular diastole.
|
|
|
What causes the first heart sound?
|
When the AV valves shut (end of diastole when pressure of ventricle is finally higher than the atria due to the filling of blood; signals beginning of systole) to prevent regurgitation of blood back into the atria
|
|
|
What causes the second heart sound?
|
When the ventricles are emptied after contraction, its pressure falls; when pressure falls below the pressure of the aorta, some blood flows back to the left ventricle; the aortic valve shuts to prevent regurgitation; this shutting causes the 2nd heart sound.
|
|
|
What is isometric contraction?
|
When all valves of the heart are briefly closed, and the ventricles contract to build pressure to a high level
|
|
|
What is isometric relaxation?
|
After ventricular contraction and ejection of blood, all valves are temporarily closed while the ventricles relax
|
|
|
True or false - the first heart sound only represents the closing of the mitral valve.
|
False - this usually comprises both the closing of the mitral valve and the tricuspid valve (though sometimes you can hear them separately)
|
|
|
True or false - the second heart sound only represents the closing of the aortic valve.
|
False - the second heart sound is usually comprised of the closing of the aortic valve and the pulmonic valve (though sometimes they can be heard separately).
|
|
|
The __ heart sound can be heard loudest at the apex.
|
S1 (first heart sound - closing of AV mitral valve)
|
|
|
The __ heart sound can be heard loudest at the base.
|
S2 (second heart sound - closing of the semilunar aortic valve)
|
|
|
What causes a split S2 heart sound?
|
When the aortic valve closes significantly earlier than the pulmonic valve, causing two distinct sounds.
|
|
|
What causes a third heart sound (S3)?
|
When ventricular filling creates audible vibrations; cause - ventricles are resistant to filling during the early rapid filing phase right after S2 (when AV valves are open and atrial blood first pours into the ventricles)
|
|
|
What causes a fourth heart sound (S4)?
|
Occurs at end of diastole, at presystole, when ventricle is resistant to filling; atria contract and push blood into a noncompliant ventricle, causing vibrations. Occurs just before S1
|
|
|
This extra heart sound occurs right after S2 and sounds like distant thunder
|
S3
|
|
|
This extra heart sound is heart immediately before S1 and is best heard at the apex with patient in left lateral position.
|
S4
|
|
|
This extra heart sound is known as a ventricular gallop.
|
S3
|
|
|
This extra heart sound is known as an atrial gallop.
|
S4
|
|
|
True or false - having a third heart sound is always abnormal.
|
False - it is usually abnormal in adults, but it is common in children and young adults. Normally, it disappears upon standing.
|
|
|
This condition gives rise to an auscultable "friction rub" (best heard with the diaphragm at the apex of the heart).
|
Perdicarditis
|
|
|
A __ is often heard/felt in the second and third left interspaces and occurs with pulmonic stenosis and pulmonic HTN.
|
Thrill
|
|
|
A __ occurs with right ventricular hypertrophy; one can palpate a diffuse lifting impulse during systole.
|
Lift or heave
|
|
|
This is a gentle, blowing, swooshing sound that can be heard on the chest wall.
|
Murmur
|
|
|
What can cause murmurs?
|
1. Faster blood flow (ex. during exercise)
2. Viscosity of blood decreases (ex. anemia) 3. Structural valve defects or unusual openings in chambers |
|
|
All heart sounds are described by what four characteristics?
|
1. Frequency (pitch) - high or low
2. Intensity (loudness) 3. Duration 4. Timing (systole or diastole) |
|
|
What is the heart's one unique ability?
|
Automaticity - it can contract by itself, independent of any signals or stimulation from the body.
|
|
|
The __ wave on an ECG represents the depolarization of the atria
|
P
|
|
|
The __ on an ECG represents the time necessary for atrial depolarization plus time for the impulse to travel through the AV node to the ventricles
|
PR Interval
|
|
|
The __ on an ECG represents depolarization of the ventricles
|
QRS complex
|
|
|
In the resting adult, the heart normally pumps __ of blood per minute. This is called __
|
4 - 6 L; cardiac output
|
|
|
Cardiac Output =
|
Stroke volume x heart rate (bpm)
|
|
|
__ is the venous return that builds during diastole, stretching the ventricles just before contraction.
|
Preload
|
|
|
According to __, the greater the stretch of the ventricles during preload, the greater the contraction.
|
Frank-Starling Law
|
|
|
__ is the opposing pressure the ventricle must generate to open the aortic valve against the higher aortic pressure - i.e., it is the resistance against which the ventricle must pump its blood.
|
Afterload
|
|
|
What are the main vascular structures in the neck?
|
Carotid artery and the jugular veins
|
|
|
True or false - the pulse of the carotid artery closely coincides with the apical pulse.
|
True
|
|
|
True or false - the jugular veins empty unoxygenated blood into the superior vena cava, and because no valve separates the vena cava from the right atrium, the jugular veins give information about the right side of the heart.
|
True
|
|
|
Which jugular vein is more visible? Where is it?
|
External; lateral to the sternomastoid muscle, above the clavicle
|
|
|
The components of the jugular venous pulse occur because of events in the __ side of the heart
|
Right
|
|
|
In the resting adult, the heart normally pumps __ of blood per minute. This is called __
|
4 - 6 L; cardiac output
|
|
|
Cardiac Output =
|
Stroke volume x heart rate (bpm)
|
|
|
__ is the venous return that builds during diastole, stretching the ventricles just before contraction.
|
Preload
|
|
|
According to __, the greater the stretch of the ventricles during preload, the greater the contraction.
|
Frank-Starling Law
|
|
|
__ is the opposing pressure the ventricle must generate to open the aortic valve against the higher aortic pressure - i.e., it is the resistance against which the ventricle must pump its blood.
|
Afterload
|
|
|
What are the main vascular structures in the neck?
|
Carotid artery and the jugular veins
|
|
|
True or false - the pulse of the carotid artery closely coincides with the apical pulse.
|
True
|
|
|
True or false - the jugular veins empty unoxygenated blood into the superior vena cava, and because no valve separates the vena cava from the right atrium, the jugular veins give information about the right side of the heart.
|
True
|
|
|
Which jugular vein is more visible? Where is it?
|
External; lateral to the sternomastoid muscle, above the clavicle
|
|
|
The components of the jugular venous pulse occur because of events in the __ side of the heart
|
Right
|
|
|
How does the fetal heart differ from all others?
|
Since the lungs are non-functional, the blood is rerouted in two ways:
1. Foramen Ovale - shunt between right and left atria (since blood does not need to go to right ventricle and then pulmonary artery) 2. Ductus Arteriosis - shunts blood from pulmonary artery to aorta Since they are both pumping into systemic circulation, right and left ventricles are equal in weight and muscle thickness |
|
|
How does the heart position of an infant differ from an adult's?
|
More horizontal in infant; apex is higher; changes to adult position by age 7
|
|
|
What are some expected findings for blood pressure and pulse for pregnant clients?
|
Decreased BP due to peripheral dilation; increased pulse rate of 10 - 15 beats per minute
|
|
|
What are some expected findings for BP and cardiac output for elderly clients?
|
Increased systolic BP due to stiffening of large arteries; left ventricular wall increases in thickness; decreased cardica output with activity
|
|
|
What are some expected changes on ECGs of elderly clients?
|
Longer PR interval (AV block) and longer Q-T interval but unchanged QRS
|
|
|
HTN is a systolic BP of __ and a diastolic BP of __
|
140 or greater; 90 or greater
|
|
|
__ is when the heart's blood supply can't keep up with demand.
|
Angina
|
|
|
A feeling of a squeezing "clenched fist" in the chest, along with sweating and cold sweats, may indicate what condition?
|
Angina
|
|
|
This type of dyspnea occurs with heart failure and happens when the patient is lying down.
|
Paroxysmal nocturnal dyspnea
|
|
|
What is orthopnea?
|
Needing to stand up to breathe
|
|
|
What is hemoptysis?
|
Coughing up blood
|
|
|
Edema is dependent when caused by ___
|
Heart failure
|
|
|
__ edema is worse at evening and better in morning after elevating the legs all night
|
Cardiac
|
|
|
What is nocturia?
|
Needing to urinate frequently at night
|
|
|
What is the only pulse that should not be palpated bilaterally?
|
Carotid artery
|
|
|
What does a normal carotid pulse feel like?
|
Smooth, with rapid upstroke, strength of 2+ or moderate; bilateral symmetry
|
|
|
For middle-aged to older persons, one should auscultate the carotid arteries for the presence of ___
|
Bruits
|
|
|
What part of the stethoscope should be used to auscultate for bruits?
|
Bell
|
|
|
True or false -- when listening for bruits at the carotid artery, you should ask the patient to hold their breath briefly so you can remove any possible conflicting sounds from the trachea.
|
True
|
|
|
An auscultated ___ indicates turbulence due to a local vascular cause, such as atherosclerosis.
|
Bruit
|
|
|
From the __ you can assess the central venous pressure (CVP) and thus judge the heart's efficiency as a pump.
|
Jugular veins
|
|
|
On what side of the client should you stand to inspect the jugular veins?
|
Right
|
|
|
True or false - the jugular pulse is generally not palpable.
|
True
|
|
|
When reading the CVP using the jugular vein, what should be used as the arbitrary point of reference?
|
Angle of Louis (sternal angle)
|
|
|
What would signify an elevated CVP when *****sing the jugular veins?
|
Level of pulsation that is more than 3 cm above the sternal angle while at 45 degrees (as with heart failure).
|
|
|
True or false - one cannot see the apical pulse.
|
False -- it can been seen, especially in children and those with thinner chest walls
|
|
|
True or false - everyone has a palpable apical pulse.
|
False -- only half of clients will have a palpable apical pulse
|
|
|
If you cannot find the apical pulse on a supine client, what alternative can be taken?
|
Asking them to roll midway to the left, which will also displace the apical pulse farther to the left
|
|
|
How does one palpate across the precordium?
|
Using palm of hand -- palpate apex, left sternal border, and base, searching for any pulsations; there should be no vibrations
|
|
|
What does a thrill feel like? How would you palpate for it?
|
Holding palm against apex, left sternal border, and base; feels like a purring cat
|
|
|
When auscultating for heart sounds, what direction will you move the bell/diaphragm of the stethoscope?
|
Z pattern
|
|
|
In what order should you ascultate for heart sounds?
|
Aortic valve area (2nd right interspace); pulmonic valve area (2nd left interspace); Erb's point (near center); triscuspid valve area (left lower sternal border); mitral valve area (5th interspace around left midclavicular line)
|
|
|
How do you check for a pulse deficit?
|
Auscultating the apical beat while simultaneously palpating the radial pulse - the two counts should be identical
|
|
|
What might cause a pulse deficit?
|
Weak contraction of the ventricles, as with A-Fib
|
|
|
True or false - sinus arrhythmias are common in children and young adults.
|
True
|
|
|
S1 is louder than S2 at the __
|
Apex
|
|
|
S2 is louder than S1 at the __
|
Base
|
|
|
True or false - S1 coincides with the carotid pulse.
|
True
|
|
|
S1 corresponds with what wave on an ECG?
|
R wave
|
|
|
When listening for heart sounds, you hear a consistent lub - T-DUP, this indicates ___
|
A split 2nd heart sound
|
|
|
What is the most common extra heart sound, usually associated with mitral valve prolapse?
|
Midsystolic Click
|
|
|
How are murmurs graded?
|
i - vi
i = barely there vi = loudest, even when stethoscope just lifted off the chest |
|
|
What is an innocent murmur?
|
Not pathologic - not valvular
|
|
|
What is a functional murmur?
|
Due to increased blood flow in heart; pathologic
|
|
|
True or false - some extra heart sounds and murmurs can only be heard while the patient is laying on the left side
|
True
|
|
|
True or false - murmurs are common with newborns
|
True, due to fetal shunt closure
|
|
|
Why should the nurse avoid pressure in the carotid sinus area of an elderly adult?
|
May cause reflex slowing of HR; also may compromise circulation if artery is narrowed due to atherosclerosis
|
|
|
What is a venous hum?
|
Common in healthy children; not pathologic; continuous low-pitched soft hum that is heart throughout heart cycle.
|
|
|
What is mammary souffle?
|
Murmur that may occur in pregnant women due to increased blood flow to internal mammary artery
|
|
|
What are all the palpable pulses of the body?
|
Carotid, brachial, radial, ulnar, femoral, popliteal, posterior tibial, dorsalis pedalis, temporal
|
|
|
What is ischemia?
|
Deficient supply of oxygenated blood to a tissue caused by obstruction of a blood vessel
|
|
|
What is the role of the lymphatic system?
|
Retrieves excess fluid from tissue spaces and returns it to the bloodstream; conserve fluid and plasma proteins that leak out of capillaries; major part of immune system; absorbs lipids from intestinal tract
|
|
|
What is the role of the right lymphatic duct?
|
Drains the right side of the head and neck, right arm, right thorax, right lung, right side of heart, and right upper liver
|
|
|
Mitral valve stenosis is common with what disease?
|
Rheumatic Fever
|
|
|
What are lymph nodes?
|
Small, oval clumps of lymphatic tissue located at intervals along vessels; nodes filter the fluid before it is returned to the blood-stream and filter out microorganisms that can be harmful to the body
|
|
|
What organs aid the lymphatic system?
|
Spleen, tonsils, and thymus
|
|
|
What is the role of the spleen?
|
Destroy old RBCs; produce antibodies; store RBCs; filter microorganisms from blood
|
|
|
True or false - lymph nodes in children are relatively small.
|
False -- they are relatively large and even superficial ones are often palpable
|
|
|
What sort of vascular changes are expected in the PVS of pregnant women?
|
Dependent edema; varicosities in the legs; hemorrhoids
|
|
|
What sort of vascular and lymphatic changes are expected in older adults?
|
Arteriosclerosis - hardening of the arteries
Also, progressive enlargement of the intramuscular calf veins (possible DVTs) Fewer lymph nodes |
|
|
What is claudication distance?
|
Number of blocks walked or stairs climbed to produce pain
|
|
|
Edema is __ when the cause is generalized (as in heart failure) or __ when it is the result of local obstruction or inflammation.
|
Bilateral; unilateral
|
|
|
Clubbing and flattening of the angle of nails occur with what cardiovascular conditions and respiratory conditions?
|
Cyanotic heart disease and cor pulmonale
|
|
|
True or false - capillary refill tests are an index of peripheral perfusion and cardiac output
|
True
|
|
|
Normal capillary refill occurs within __ seconds
|
1 - 2
|
|
|
How is the force of a pulse graded?
|
0 - 3
0 = absent 1 = weak 2 = normal 3 = bounding |
|
|
How are the epitrochlear lymph nodes palpated?
|
The shaking hands technique (reach other hand under person's elbow and palpate between the groove of the biceps and triceps muscles, above the medial epicondyle)
|
|
|
How is the adequacy of collateral circulation before cannulating the radial artery tested?
|
Modified Allen Test
|
|
|
What is the modified Allen test?
|
Tests the adequacy of circulation via the radial arteries; the ulnar and radial pulse of each hand is occluded while the person makes a fist several times, causing the hand to blanch; the person then opens the hand and the examiner releases pressure on the ulnar artery; a palmar blush should return in 2 - 5 seconds; occlude with about 11 lbs of pressure
|
|
|
What are the limitations of the Allen test?
|
Purely subjective and requires patient cooperation that may not be possible in emergency situations
|
|
|
Malnutrition to the legs due to poor arterial sufficiency or perfusion is manifested by what symptoms?
|
Thin, shiny, atrophic skin; thick-ridged nails; loss of hair; ulcers; gangrene
|
|
|
What should the venous pattern of the legs appear like upon inspection?
|
Flat and barely visible
|
|
|
Chronic venous stasis can manifest itself with what sort of coloring in the legs?
|
Brownish discoloration
|
|
|
What is a Homan sign?
|
Homans' sign is a sign of deep vein thrombosis (DVT). A positive sign is present when there is pain in the calf on dorsiflexion of the patient's foot at the ankle while the knee is fully extended.
|
|
|
Where can the popliteal pulse be found?
|
Behind the knee, in the popliteal fossa
|
|
|
If pretibial edema is found, how should it be graded?
|
1 - 4
1 = mild pitting, slight indentation 4 = Very deep pitting, indentation lasts a long time, leg is grossly swollen |
|
|
Unilateral edema usually occurs with ___
|
Occlusion of a deep vein
|
|
|
Varicosities occur in the __ veins
|
Saphenous
|
|
|
What is the manual compression test?
|
Test for varicose veins; test the length of the varicosity while the patient is standing; one hand is placed over a lower part of the vein, and the other hand compresses the vein about 15 - 20 cm higher; competent valves will produce wave; a palpable wave transmission occurs when waves are incompetent
|
|
|
A nurse suspects an arterial deficit in a patient's legs, so he raises the legs about 30 cm above the table and has the patient wag the feet for about 30 seconds; then the patient is instructed to sit up and let the legs dangle. Why?
|
Raising the feet and wagging them drains off arterial blood; skin color will only reflect contribution of arterial blood. Feet should look pale but pink; elevational pallor indicates insufficiency; when dangling the feet, color should return in about 10 - 15 seconds.
|
|
|
What is dependent rubor?
|
Deep blue-red color in lower extremeties as a result of arterial insufficiency.
|
|
|
What is a doppler ultrasonic stethoscope used for?
|
Detecting a weak pulse
|
|
|
True or false - nearly 80% of pregnant women have some peripheral edema and varicose veins are common during the third trimester.
|
True
|
|
|
Abrupt progressive tricolor changes of the fingers due to cold, vibration, and stress, usually from white pallor to blue to red in the heel is probably __
|
Raynaud's Phenomenon
|
|
|
This is a high-protein swelling of the limb, most commonly due to breast cancer treatment.
|
Lymphedema
|
|
|
Who are at risk for chronic venous symptoms and pain?
|
Jobs with prolonged sitting or standing; obesity; pregnancy; prolonged bedrest; history of heart failure, varicosities, or thrombophlebitis; veins crushed by trauma
|
|
|
What are some signs and symptoms of arterial-ischemic ulcer?
|
Ulcers on toes, metatarsal heads, heels, with pale ishemic base, well-defined edges, and no bleeding
|
|
|
How does a venous (stasis) ulcer differ from an arterial (ischemic) ulcer?
|
Venous (stasis) ulcer = bleeding, uneven edges
Arterial (ischemic) ulcer = well-defined edges with no bleeding |
|
|
What is a DVT?
|
Deep vein thrombophlebitis -- deep vein is occluded by a thrombus, causing inflammation, blocked venous return, and edema; patient will complain of intense, sharp, deep muscle pain; you will notice warmth, swelling, redness; possible positive Homan sign
|
|
|
True or false - over age 45, occurrence of superficial varicose veins is three times more common in women than in men
|
True
|
|
|
Dilated, torturous veins is a sign of __
|
Varicose veins
|
|
|
The sternal angle is often called __
|
The Angle of Louis
|
|
|
Orthopnea is difficulty breathing when __
|
Supine
|
|
|
What is paroxysmal nocturnal dyspnea?
|
Awakening from sleep with shortness of breath and needing to be upright to achieve comfort
|
|
|
Barrel chest is presented for clients with __
|
Chronic emphysema
|
|
|
What position do clients with COPD often sit?
|
Tripod; this gives them leverage so that their abdominals, intercostal, and accessory neck muscles can aid in expiration
|
|
|
Why are neck muscles hypertrophied with someone who has COPD?
|
Neck muscles larger from continually aiding in forced respirations
|
|
|
What are the three expected types of breath sounds in the adult and older child?
|
Bronchial (high and loud; trachea and larynx)
Bronchovesicular (moderate; over major bronchi) Vesicular (low; over peripheral lung) |
|
|
What are adven***ious sounds?
|
Added breath sounds that are not normally heard in the lungs (ex. crackles or wheezing); caused by air colliding with excretions or by the popping open of previously deflated airways
|
|
|
Wheezing is also known as __
|
Rhonchi
|
|
|
Crackles are also known as __
|
Rales
|
|
|
This thoracic condition has horizontal ribs and costal angle of >90 degrees
|
Barrel Chest
|
|
|
What are atelectatic crackles?
|
Non-pathologic crackles - short popping sounds but do not last beyond a few breaths; occurs when alveoli are not fully aerated, and crackles are heard when they are expanded by a few deep breaths
|
|
|
A person with __ may purse lips in a whistling position while breathing
|
COPD
|
|
|
Chronic ___ (lung condition) may cause hypertrophied abdominals from forced expirations
|
Emphysema
|
|
|
What is forced expiration time? What is considered normal?
|
Number of seconds it takes for a person to exhale from total lung capacity to residual volume; 4 seconds or less
|
|
|
Abnormal sunken sternum and adjacent cartilages
|
Pectus Excavatum
|
|
|
Abnormal thoracic configuration where there is an S-shaped curvature of the thoracic and lumbar spine, often with vertebrae rotation
|
Scoliosis
|
|
|
What is kyphosis?
|
An exaggerated posterior curvature of the thoracic spine (humpback) that causes pain and limited mobility; associated with aging and familiar "dowager's hump" of postmenopausal osteoporotic women; related to physical fitness
|
|
|
This heart valve is also called the bicuspid
|
Mitral
|
|
|
The Sinoatrial Node (SA) impulse begins __
|
In the right atrium
|
|
|
Where is the ATRIOVENTRICULAR NODE (AV) found?
|
Atrial septum
|
|
|
This extra heart sound is low pitched, like “Ken-tuck-y”
|
S3 - ventricular gallop
|
|
|
This extra heart sound is low pitched, like “Ten-nes-see”
|
S4 - atrial gallop
|
|
|
What is a possible cause of a 3rd heart sound?
|
Heart failure
|
|
|
What are possible causes of a 4th heart sound?
|
MI, HTN, AS
|
|
|
Murmurs can be heard all over the __
|
Precordium
|
|
|
What is the sequence in which the cardiovascular system is examined?
|
Sequence:
Inspect Palpate Auscultate |
|
|
These are lifts along sternal border or apex.
|
Heaves
|
|
|
What is "APE to MaN" used for?
|
Remembering sequence of listening to heart sounds:
Aortic- RSB @ 2nd ICS Pulmonic- LSB @ 2nd ICS Erbs- LSB @ 3rd ICS Tricuspid- LLSB @ 5th ICS Mitral(apical)-L MCL @ 5th ICS |
|
|
At these two positions (while listening for heart sounds), S2 will be louder
|
Pulmonic and aortic (base of the heart)
|
|
|
At these two positions (while listening for heart sounds), S1 will be louder
|
Tricuspid and mitral (apex of the heart)
|
|
|
At this position (while listening for heart sounds), S1 = S2
|
Erb's Point
|
|
|
At this position (while listening for heart sounds), S1 = the R wave on an ECG
|
Mitral (apex of the heart - point of maximal impulse)
|
|
|
What is cardiac tamponade?
|
Excess fluid in pericardium, crushes heart; pericarditis and aortic dissection cause
|
|
|
What is cor pulmonale?
|
RVH from COPD, pulmonary HTN (loud S2, LSB lift)
|
|
|
What is myocarditis?
|
Inflammation from autoimmune disease or virus
|
|
|
__ is a fairly common heart defect that can occur soon after birth. In this congenital defect, abnormal blood flow occurs between the aorta and the pulmonary artery.
|
Patent ductus arteriosis
|
|
|
What is the most common cyanotic congenital heart defect?
|
Tetralogy of Fallot
|
|
|
__ is multisystem inflammatory response; with lesions affecting the heart, joints, subcutaneous tissue and CNS; warning signs include streptococcal exposure and sore throat
|
Rheumatic Fever
|
|
|
What are the axillary lines used for *****sment of the chest?
|
Axillary lines:
Anterior, Posterior, Midaxillary |
|
|
What are the four functions of the respiratory system?
|
1. Changing chest size during respiration
2. Inspiration 3. Expiration 4. Control of respiration |
|
|
In what sequence should the lungs and thoracic region be examined?
|
Sequence:
Inspect Palpate Percuss Auscultate |
|
|
How can symmetrical expansion of the chest and thoracic region be palpated?
|
Two thumbs - deep breath - thumbs should move apart
|
|
|
What are two common phrases that patients are asked to utter when vocal fremitus is being *****sed?
|
Ninety-nine or blue moon
|
|
|
What is bronchophony, egophony, and whispered pectoriloquy?
|
Bronchophony - aksed patient to repeat "99" while listening with stethoscope
Egophony - Auscultate chest while person phonates a long "ee-ee-ee-ee" sound Whispered pectoriloquy - ask the person to whisper a phrase like "1 - 2 - 3" as you listen |
|
|
What is the normal finding of the bronchophony test?
|
Normal voice transmission is soft, muffled, and indistinct -- can't make out the words
|
|
|
What is the normal finding of the egophony test?
|
You should hear "eeeee" through stethoscope
|
|
|
What is the normal finding of the whispered pectoriloquy test?
|
Normal response is faint, muffled, and almost inaudible
|
|
|
What are the types of wheezes?
|
Sibilant= high-pitched, musical squeaking
Sonorous= low-pitched, snoring, moaning Stridor= high-pitched, crowing |
|
|
What are the types of crackles?
|
Fine= high-pitched
Coarse= loud, low-pitched, bubbling or gurgling Atelectatic crackles= short-lived, popping crackles |
|
|
What is an abnormal finding of bronchophony?
|
The words will be distinct
|
|
|
The Angle of Louis lines up with what rib(s)?
|
2nd
|
|
|
What two sites does the Angle of Louis indicate?
|
1. Lines up with the 2nd ribs on either side
2. Indicates site of bifurcation of the trachea into the right and left bronchi |
|
|
The trachea is __ (posterior/anterior) to the esophagus.
|
Anterior
|
|
|
Can the trachea be auscultated from the posterior position?
|
No, since it is in front of the esophagus.
|
|
|
What three lines help examiners landmark the front of the thorax?
|
Midsternal line, midclavicular line, anterior axillary line
|
|
|
Increased tactile fremitus would be evident in an individual who has which of the following conditions?
A) Emphysema B) Pneumonia C) Pleural Effusion D) Pneumothorax |
B) Pneumonia
Decreased fremitus occurs when anything obstructs transmission of vibrations (e.g., obstructed bronchus, pleural effusion or thickening, pneumothorax, or emphysema). Increased fremitus occurs when the density of the lungs increase, making it a better conductor for vibrations. |
|
|
What is an appropriate intervention if a nasoenteral tube is misplaced in the respiratory tract?
|
Remove the tube and report to the health care provider
|
|
|
A clinical manifestation common in an individual with chronic obstructive pulmonary disease (COPD) is:
A) periodic breathing patterns. B) pursed-lip breathing. C) unequal chest expansion. D) hyperventilation. |
B) pursed-lip breathing.
Feedback: CORRECT An individual with COPD may purse the lips in a whistling position. By exhaling slowly and against a narrow opening, the pressure in the bronchial tree remains positive, and fewer airways collapse. |
|
|
Routine irrigation of feeding tubes maintains its ___
|
Patency
|
|
|
The thoracic cage is defined by all of the following except the:
A) sternum. B) ribs. C) costochondral junction. D) diaphragm. |
C) costochondral junction.
Feedback: CORRECT The thoracic cage is defined by the sternum, ribs, vertebrae, and diaphragm. |
|
|
A lipid emulsion is administered via __ or __
|
Primary IV or IV piggyback
|
|
|
Inspiration is primarily facilitated by which of the following muscles?
A) Diaphragm and abdominus rectus B) Trapezia and sternomastoids C) Internal intercostals and abdominal D) Diaphragm and intercostals |
D) Diaphragm and intercostals
Feedback: CORRECT The major muscle responsible for inspiration is the diaphragm. Intercostal muscles lift the sternum and elevate the ribs, making them more horizontal; this increases the anteroposterior diameter. |
|
|
Why do researchers believe that parenteral nutrition is associated with a significant increase of catheter-related infections?
|
Pathogens can easily access the blood stream via venous access device; increased risk is due in part to poor blood glucose control and resulting hyperglycemia, creating an environment for pathogen growth
|
|
|
Which of the following voice sounds would be a normal finding?
A) The voice transmission is distinct and sounds close to the ear. B) The "eeeee" sound is clear and sounds like "eeeee". C) The whispered sound is transmitted clearly. D) Whispered “1-2-3” is audible and distinct. |
B) The "eeeee" sound is clear and sounds like "eeeee".
Feedback: CORRECT A normal finding from voice sounds is egophony; “eeeee” heard through the stethoscope clearly. |
|
|
When administering parenteral nutrition, special care should be taken to monitor and maintain __ levels in the normal range.
Why? |
Blood glucose
Higher levels are associated with hyperglycemia and resulting cardiovascular events, general infection, sepsis, acute renal failure, even death |
|
|
The function of the trachea and bronchi is to:
A) transport gases between the environment and the lung parenchyma. B) condense inspired air for better gas exchange. C) moisturize air for optimum respiration. D) increase air turbulence and velocity for maximum gas transport. |
A) transport gases between the environment and the lung parenchyma.
Feedback: CORRECT The trachea and bronchi transport gases between the environment and the lung parenchyma. |
|
|
What is the most common type of enteral nutrition?
|
Gastric feedings
|
|
|
Stridor is a high-pitched, inspiratory crowing sound commonly associated with:
A) upper airway obstruction. B) atelectasis. C) congestive heart failure. D) pneumothorax. |
A) upper airway obstruction.
Feedback: CORRECT Stridor is associated with upper airway obstruction from swollen, inflamed tissues or a lodged foreign body. |
|
|
Percussion of the chest is:
A) a useful technique for identifying small lesions in lung tissue. B) helpful only in identifying surface alterations of lung tissue. C) is not influenced by the overlying chest muscle and fat tissue. D) normal if a dull note is elicited. |
B) helpful only in identifying surface alterations of lung tissue.
Feedback: CORRECT Percussion detects only the outer 5 to 7 cm of tissue; it will not penetrate to reveal any change in density deeper than that. |
|
|
Which of the following correctly expresses the relationship to the lobes of the lungs and their anatomic position?
A) Upper lobes—lateral chest B) Upper lobes—posterior chest C) Lower lobes—posterior chest D) Lower lobes—anterior chest |
C) Lower lobes—posterior chest
Feedback: CORRECT The posterior chest is almost all lower lobe. |
|
|
An increase in the transverse diameter of the chest cage in a pregnant female is due to a(n):
A) compensatory increase in respiratory parenchyma. B) increase in estrogen. C) increase in surfactant. D) increase in tidal volume. |
B) increase in estrogen.
Feedback: CORRECT The increase in estrogen level during pregnancy relaxes the chest cage ligaments. This allows an increase in the transverse diameter of the chest cage by 2 cm, and the costal angle widens. |
|
|
The first heart sound is produced by the:
A) closure of the semilunar valves. B) closure of the AV valves. C) opening of the semilunar valves. D) opening of the AV valves. |
B) closure of the AV valves.
Feedback: CORRECT The first heart sound (S1) occurs with closure of the AV valves. |
|
|
Which of the following guidelines may be used to identify which heart sound is S1?
A) S1 is louder than S2 at the base of the heart. B) S1 coincides with the A wave of the jugular venous pulse wave. C) S1 coincides with the carotid artery pulse. D) S1 coincides with the Q wave of the QRS electrocardiogram complex. |
C) S1 coincides with the carotid artery pulse.
Feedback: CORRECT S1 coincides with the carotid artery pulse. |
|
|
Which of the following cardiac alterations occurs during pregnancy?
A) An increase in cardiac output and blood pressure B) An increase in cardiac volume and a decrease in blood pressure C) An increased heart rate and increased blood pressure D) An increased stroke volume with decreased cardiac output |
B) An increase in cardiac volume and a decrease in blood pressure
Feedback: CORRECT During pregnancy the blood volume increases by 30% to 40%; this creates an increase in stroke volume and cardiac output and an increased pulse rate of 10 to 15 beats per minute. The arterial blood pressure decreases in pregnancy as a result of peripheral vasodilation. |
|
|
Which of the following is an appropriate position to have the patient assume when auscultating for extra heart sounds or murmurs?
A) Roll toward the left side B) Roll toward the right side C) Trendelenburg position D) Re***bent position |
A) Roll toward the left side
Feedback: CORRECT After auscultation in the supine position, the nurse should have the patient roll onto the left side; the examiner should listen at the apex with the bell for the presence of any diastolic filling sounds (i.e., S3 or S4) or murmurs that may be heard only in this position. The examiner should have the patient sit up and lean forward; the examiner should auscultate at the base with the diaphragm for a soft, high-pitched, early diastolic murmur of aortic or pulmonic regurgitation. |
|
|
The ability of the heart to contract independently of any signals or stimulation is due to:
A) depolarization. B) automaticity. C) conduction. D) repolarization. |
B) automaticity.
Feedback: CORRECT The heart can contract by itself, independent of any signals or stimulation from the body; this property is termed automaticity. |
|
|
When auscultating the heart of a newborn within 24 hours after birth, the examiner hears a continuous sound that mimics the sound of a machine. This finding most likely indicates:
A) the presence of congenital heart disease. B) a normal sound because of the thinner chest wall of the newborn. C) an expected sound caused by nonclosure of the ductus arteriosus. D) pathology only when accompanied by an increased heart rate. |
C) an expected sound caused by nonclosure of the ductus arteriosus.
Feedback: CORRECT The murmur of a patent ductus arteriosus is a continuous machinery murmur, which disappears by 2 to 3 days. |
|
|
A bruit heard while auscultating the carotid artery of a 65-year-old patient is caused by:
A) decreased velocity of blood flow through the carotid artery. B) turbulent blood flow through the carotid artery. C) rapid blood flow through the carotid artery. D) increased viscosity of blood. |
B) turbulent blood flow through the carotid artery.
Feedback: CORRECT A carotid bruit is a blowing, swishing sound indicating blood flow turbulence. A bruit indicates atherosclerotic narrowing of the vessel. |
|
|
The jugular venous pressure is an indirect reflection of the:
A) heart's efficiency as a pump. B) cardiac cycle. C) conduction effectiveness. D) synchronization of mechanical activity. |
A) heart's efficiency as a pump.
Feedback: CORRECT Jugular venous pressure is a reflection of the heart’s ability to pump blood. If the pressure is elevated, heart failure is suspected. |
|
|
The semilunar valves separate the:
A) atria from the ventricles. B) right atria from the left atria. C) ventricles from the arteries. D) atria from the veins. |
C) ventricles from the arteries.
Feedback: CORRECT The semilunar valves separate the ventricles from the arteries. The atrioventricular valves separate the atria and ventricles. |
|
|
One of the leg's deep veins is the:
A) great saphenous. B) small saphenous. C) tibial. D) popliteal |
D) popliteal.
Feedback: CORRECT The femoral and popliteal veins are the deep veins in the leg. |
|
|
Arteriosclerosis refers to:
A) a variation from the heart's normal rhythm. B) a sac formed by dilation in the arterial wall. C) thickening and loss of elasticity of the arterial walls. D) deposition of fatty plaques along the intima of the arteries. |
C) thickening and loss of elasticity of the arterial walls.
Feedback: CORRECT Arteriosclerosis is the thickening and loss of elasticity of the arterial walls. |
|
|
Palpable inguinal lymph nodes are:
A) normal if small (less than 1 cm), movable, and nontender. B) abnormal in adults but common in children and infants. C) normal if fixed and tender. D) abnormal and indicate the presence of malignant disease. |
A) normal if small (less than 1 cm), movable, and nontender.
Feedback: CORRECT Inguinal lymph nodes may be palpable. This is a normal finding if the nodes are small (1 cm or less), movable, and nontender. |
|
|
Lymphedema is:
A) the indentation left after the examiner depresses the skin over swollen edematous tissue. B) a thickening and loss of elasticity of the arterial walls. C) an inflammation of the vein associated with thrombus formation. D) the swelling of an extremity caused by an obstructed lymph channel. |
D) the swelling of an extremity caused by an obstructed lymph channel.
Feedback: CORRECT Lymphedema is swelling of the limb caused by surgical removal of lymph nodes or damage to lymph nodes and vessels. |
|
|
The cervical nodes drain the:
A) upper arm and breast. B) hand and lower arm. C) external genitalia. D) head and neck. |
D) head and neck.
Feedback: CORRECT The cervical nodes drain the head and neck. |
|
|
Claudication is caused by:
A) venous insufficiency. B) arterial insufficiency. C) varicose veins. D) stasis ulcerations. |
B) arterial insufficiency.
Feedback: CORRECT Claudication is caused by arterial insufficiency. |
|
|
The patient has severe bilateral lower extremity edema. The most likely cause is:
A) an infection of the right great toe. B) Raynaud phenomenon. C) heart failure. D) an aortic aneurysm. |
c) heart failure.
Feedback: CORRECT Bilateral lower extremity edema is a result of a generalized disorder such as heart failure. |
|
|
A client has been admitted to the hospital with acute bronchitis. The nurse *****ses that the client has a barrel chest and is less than the desired weight, and that he reports experiencing severe dyspnea when she tries to perform any physical activity. The nurse recognizes that the client is most likely to have the underlying lung disease of:
a. emphysema. b. tuberculosis. c. empyemia. d. lung cancer. |
a. emphysema
|
|
|
This lung condition involves a collapsed shrunken section of alveoli or entire lung as a result of 1) airway obstruction 2)compression of lung 3) lack of surfactant
|
Atelectasis
|
|
|
A child has a chronic cough and diffuse wheezing during the expiratory phase of respiration. The nurse is aware that this child may have which of the following?
a. Bronchitis b. Foreign body in trachea c. Asthma d. Pneumonia |
c. asthma
|
|
|
The heart contains four chambers: two upper chambers and two lower chambers. The wall that divides the left and right sides of the heart is known as the:
a. septum. b. pericardium. c. atria. d. ventricle. |
a. septum
|
|
|
True or false - pleural friction rub can be palpable
|
True
|
|
|
A client admitted for evaluation of cardiac distress says to you, "The doctor was here today and said that my ejection fraction was low. I'm not sure what that means. Can you explain it to me?" Your best response would be:
a. "It is the percentage of blood in the ventricle that is ejected with each contraction, and it is affected by preload, afterload, and contractibility." b. "It is the force required for the ventricles to push blood out of the heart and into circulation. The left ventricle has to work harder than the right ventricle to circulate the blood through the body." c. "When the heart rate increases, it causes increased cardiac output. If the rate is very rapid, the ventricles cannot fill completely, so cardiac output falls, as does the stroke volume. When the heart rate is slow (<60), cardiac output decreases because the heart contracts less often." d. "It is the amount of blood in the ventricles before contraction. When ventricles are full, they stretch and then contract more forcefully. When the blood volume is low, due to conditions such as hemorrhage or dehydration, preload decreases." |
a. "It is the percentage of blood in the ventricle that is ejected with each contraction, and it is affected by preload, afterload, and contractibility."
|
|
|
When does decreased tactile fremitus occur?
|
When something is obstructing the transmission of vibrations in the lungs
|
|
|
As a nurse, you understand that most deaths related to heart disease are caused by:
a. atherosclerosis. b. myocardial infarction. c. coronary artery disease. d. atrial fibrillation. |
c. coronary artery disease
|
|
|
This type of crackles presents with aging adults, bedridden persons, or in persons who were just aroused from sleep
|
Atelectatic crackles
|
|
|
When caring for clients with peripheral vascular diseases, your focus needs to be on:
a. teaching clients how to monitor their own blood pressures. b. identifying the risk factors associated with cigarette smoking. c. maintaining the telemetry unit at all times and the client's response to exertion and activity. d. maintaining circulation to the affected area, decreasing edema, and managing pain. |
d. maintaining circulation to the affected area, decreasing edema, and managing pain.
|
|
|
Pleural friction rub is present in patients with __, and is accompanied by pain with breathing
|
Pleuritis
|
|
|
A 40-year-old female client reports that she is experiencing pain, numbness, and discoloration in her hands and feet. It worsens when she is exposed to cold conditions. She has a history of smoking cigarettes and works in a high stress job. From this collected *****sment data, you determine the client may have which of the following conditions?
a. Thrombophlebitis b. Buerger's disease c. Arteriosclerosis obliterans d. Raynaud's disease |
d. Raynaud's disease
|
|
|
A high-pitched wheeze is often present in patients with ___
|
Acute asthma or chronic emphysema
|
|
|
Your client is experiencing severe lymphedema in her left arm post-mastectomy. You have placed a sign at the head of her bed that alerts other nurses and phlebotomists to avoid needle sticks in the affected extremity. You understand the rationale for this to be:
a. no particular reason; it just seems logical. b. the client will experience more pain in that arm. c. the blood vessels are compromised and collapsed. d. the puncture site may become a focus for infection. |
d. the puncture site may become a focus for infection.
It is important to avoid any needle sticks in the affected extremity of someone with lymphedema. This may become a focus for infection. Venipunctures are also avoided because the tourniquet needed to expand the vein may damage the tissue. The nurse should place a sign above the bed of a client with lymphedema to alert other staff to avoid using the affected extremity. |
|
|
Low pitched wheezes is often present in this lung abnormality or with airway tumors
|
Bronchitis
|
|
|
Stridor is often present in clients with croup or children with epiglot***is; also presents when there is a foreign object obstruction in the airway
|
Stridor
|
|
|
When inspecting the anterior chest, if you notice retraction or bulging of the interspaces, what does this mean?
|
Obstruction of the respiratory tract or increased inspiratory effort is needed, as with atelectasis; bulging can mean forced expiration as with emphysema or asthma
|
|
|
Coarse crackles are often associated with what lung abnormalities?
|
Pulmonary edema, pneumonia, pulmonary fibrosis, and the terminally ill who have depressed cough reflex
|
|
|
Stridor has what type of sound?
|
High pitched inspiratory crowing sound
|
|
|
This abnormality involves a forward protruding sternum, with ribs sloping back (Pidgeon Chest)
|
Pectus Carinatum
|
|
|
Atelectatic crackles are often associated with what populations?
|
Aging adults, bedridden persons, people just aroused from sleep
|
|
|
This abnormality involves a forward protruding sternum, with ribs sloping back (Pidgeon Chest)
|
Pectus Carinatum
|
|
|
Pleural friction rub is often heard in clients with what condition?
|
Pleuritis
|
|
|
This is a lower-pitched booming sound found when too much air is present, such as in emphysema and pneumothorax
|
Hyperresonance
|
|
|
High-pitched wheezing is often a symptom of what conditions?
|
Acute asthma and chronic emphysema
|
|
|
This is a lower-pitched booming sound found when too much air is present, such as in emphysema and pneumothorax
|
Hyperresonance
|
|
|
Low-pitched wheezing is often present in clients with what conditions?
|
Bronchitis or single bronchus obstruction
|
|
|
A __ note sound when percussing signals abnormal density in the lungs, as with pneumonia, pleural effusion, atelectasis, or tumor
|
Dull
|
|
|
Stridor is often present in what clients?
|
Clients with croup, children with acute epiglottitis, person who has inhaled foreign object or has an obstructed airway
|
|
|
A __ note sound when percussing signals abnormal density in the lungs, as with pneumonia, pleural effusion, atelectasis, or tumor
|
Dull
|
|
|
What does stridor sound like?
|
High-pitched inspiratory crowing sound, louder in neck
|
|
|
Bronchial (tracheal) sounds are __ pitched, while vesicular sounds are __ pitched
|
High; low
|
|
|
This condition involves a collapsed shrunken section of an alveoli or an entire lung as a result of airway obstruction, compression of the lung, or lack of surfactant
|
Atelectasis
|
|
|
Bronchial (tracheal) sounds are __ pitched, while vesicular sounds are __ pitched
|
High; low
|
|
|
This is a lower-pitched booming sound found when too much air is in the lungs, as in emphysema or pneumothorax.
|
Hyperresonance
|
|
|
True or false - atelectatic sounds are non pathologic
|
True
|
|
|
Clients with this lung condition may purse their lips in a whistling fashion in order to exhale more slowly.
|
COPD
|
|
|
True or false - atelectatic sounds are non pathologic
|
True
|
|
|
Crackles only in the upper lung fields occur with ___; crackles only in the lower lung fields occur with ___
|
Cystic fibrosis; CHF
|
|
|
The person with __ may purse the lips in a whistling fashion to breathe.
|
COPD
|
|
|
This abnormal configuration of the thorax presents with a forward protrusion of the sternum, with ribs sloping back at either side (pigeon breast)
|
Pectus Carinatum
|
|
|
The person with __ may purse the lips in a whistling fashion to breathe.
|
COPD
|
|
|
What will pleural friction fremitus feel like when palpated?
|
Two pieces of leather rubbing together
|
|
|
This abnormal lung condition involves a collapsed shrunken section of the alveoli or an entire lung due to 1) airway obstruction 2) compression of the lung 3) lack of surfactant
|
Atelectasis
|
|
|
When will decreased tactile fremitus occur?
|
When anything is obstructing transmission of vibrations (eg. obstructed bronchus, pleural effusion or thickening, pneumothorax, and emphysema)
|
|
|
This abnormal lung condition involves a collapsed shrunken section of the alveoli or an entire lung due to 1) airway obstruction 2) compression of the lung 3) lack of surfactant
|
Atelectasis
|
|
|
Patient one has an increased respiratory rate with guarding and lag on one side of the chest; patient two has a very productive cough, producing thick sputum and having a hard time breathing. Who has bronchitis and who has pneumonia?
|
Patient one has pneumonia; patient two has bronchitis
|
|
|
Excess mucuos secretion, crackles over deflated areas, dyspnea, fatigue, possible cyanosis and clubbing of fingers, all which can be caused by cigarette smoking, is often indicative of what lung abnormality?
|
Bronchitis
|
|
|
What will palpation reveal of a client with pleural effusion?
|
Decreased or absent tactile fremitus; decreased chest expansion on affected side
|
|
|
Excess mucuos secretion, crackles over deflated areas, dyspnea, fatigue, possible cyanosis and clubbing of fingers, all which can be caused by cigarette smoking, is often indicative of what lung abnormality?
|
Bronchitis
|
|
|
This condition is typified by free air in pleural space that causes partial or complete lung collapse. Percussion is hyperresonant and tactile fremitus, decreased or absent.
|
Pneumothorax
|
|
|
True or false - asthma involves unilateral wheezing
|
False - bilateral wheezing
|
|
|
This lung condition involves undissolved materials originating in the legs detaching and traveling via venous system to the right lung to become lodged in vessels, occluding them.
|
Pulmonary Embolism
|
|
|
True or false - asthma involves unilateral wheezing
|
False - bilateral wheezing
|
|
|
A 35 yr old recent immigrant is being seen in clinic for complaints of cough that's associated w/rust-colored sputum, low-grade afternoon fevers, & night sweats for past 2 months. Nurse's preliminary analysis is that this patient may be suffering from:
|
Tuberculosis
|
|
|
True or false - TB and Pulmonary embolism may present blood with coughing
|
True
|
|
|
The nurse is aware that tactile fremitus is produced by:
|
Sounds generated from the larynx
|
|
|
True or false - TB and Pulmonary embolism may present blood with coughing
|
True
|
|
|
During auscultation of the lungs, the nurse knows that decreased breath sounds would most likely be heard:
|
when the bronchial tree is obstructed
|
|
|
True or false - TB is initially asymptomatic
|
True (only positive skin test or chest x-ray)
|
|
|
Upon examination of a patient, you note a coarse, low-pitched sound during both inspiration and expiration. This patient complains of pain with breathing. These findings are consistent with:
|
pleural friction rub
|
|
|
True or false - TB is initially asymptomatic
|
True (only positive skin test or chest x-ray)
|
|
|
During palpation of the anterior chest wall, the nurse notes a coarse, crackling sensation over the skin surface. On the basis of these findings, the nurse suspects:
|
Crepitus
|
|
|
This lung abnormality involves a thrombus making its way into the lung and occluding a blood vessel
|
Pulmonary embolism
|
|
|
Your patient has a long history of chronic obstructive pulmonary disease (COPD). You are most likely to observe:
|
an anteroposterior: transverse diameter ratio of 1:1
|
|
|
This lung abnormality involves a thrombus making its way into the lung and occluding a blood vessel
|
Pulmonary embolism
|
|
|
The nurse has noted unequal chest expansion and recognizes that this occurs when:
|
part of the lung is obstructed or collapsed
|
|
|
True or false - crackles are not common in patients with TB and Pulmonary Embolism
|
False - they are fairly common to both
|
|
|
A 65 year old patient with a history of heart failure comes to the clinic with complaints of "being awakened suddenly from sleep, with shortness of breath." You:
|
suspect that the patient is experiencing paroxysmal nocturnal dyspnea
|
|
|
True or false - crackles are not common in patients with TB and Pulmonary Embolism
|
False - they are fairly common to both
|
|
|
The most important technique when progressing from one ausculatory site on the chest wall to another is:
|
side to side comparison
|
|
|
This lung condition involves a buildup of excess fluid in the intrapleural space, with compression of overlying lung tissue; this subdues all lung sounds (no tactile fremitus)
|
Pleural effusion or thickening
|
|
|
During an examination of the anterior thorax, the nurse recalls that the trachea bifurcates anteriorly at the:
|
angle of Louis
|
|
|
This lung condition involves a buildup of excess fluid in the intrapleural space, with compression of overlying lung tissue; this subdues all lung sounds (no tactile fremitus)
|
Pleural effusion or thickening
|
|
|
True or false - percussing cardiac borders is just as accurate as performing an xray to determine true cardiac borders.
|
False - It is only of moderate usefulness but not very accurate.
|
|
|
This is a palpable vibration when examining the lungs.
|
Fremitus
|
|
|
When palpating for fremitus, where should you start?
|
Lung apices (top of chest)
|
|
|
When will increased fremitus be palpated?
|
In cases of lung compression or consolidation, as in lobar pneumonia.
|
|
|
This is a coarse, crackling sensation palpable over the skin surface of the chest.
|
Crepitus
|
|
|
How is crepitus assessed -- inspecting, palpating, percussing, or auscultating?
|
Palpating
|
|
|
In what order should the lungs and thorax be examined?
(choose from inspecting, auscultating, percussing, palpating) |
Inspect, palpate, percuss, auscultate
|
|
|
How should healthy lung tissue sound when percussed?
|
Clear, low-pitched, hollow
|
|
|
What do dull sounds from percussed lung tissue mean?
|
Abnormal density in lungs, as with pneumonia, pleural effusion, etc.
|
|
|
How long should an examiner listen for lung sounds at each location?
|
One full respiration at each location
|
|
|
When do decreased or absent lung sounds occur?
|
1. When bronchial tree is obstructed by secretions, mucus plug, or foreign body
2. In emphysema as result of loss of elasticity in lung fibers and decreased force of inspired air 3. When anything obstructs transmission of sound between lung and stethoscope, such as pleural thickening or air (as in pneumothorax) |
|
|
A person with COPD will have what sort of facial expression?
|
Tired, tense, strained faces with possible pursed lips
|
|
|
A normal thorax has (horizontal / downward sloping) ribs about 45 degrees relative to the spine.
|
Downward sloping
|
|
|
True or false - the normal thorax should have a ratio of anteroposterior to transverse diameter of 1:1.
|
False - ratio should be 1:2 to 5:7
A 1:1 ratio is more indicative of COPD (esp. chronic emphysema) |
|
|
Where are the upper borders of the lungs when inspecting the anterior chest?
|
About 3 to 4 cm above the inner third of the clavicles.
|
|
|
Which lung is narrower? Why?
|
Left lung due to the heart
|
|
|
What is the hollow U-shaped depression just above the sternum (between the clavicles)?
|
Suprasternal Notch
|
|
|
What is the costal margin?
|
Anterior chest landmark -- where the right and left costal margins meet at the xiphoid process (bottom of the sternum)
|
|
|
Which heart sound provides the "lub" of the heart beat?
|
S1
|
|
|
Which heart sound provides the "dub" of the heart beat?
|
S2
|
|
|
The heart sound S1 is comprised of what two sounds? Which comes first?
|
M1 and T1 (mitral valve closing and tricuspid valve closing) -- M1 comes slightly ahead of T1 but usually you can't distinguish them
|
|
|
The heart sound S2 is comprised of what two sounds? Which comes first?
|
A2 and P2 (aortic valve closing and pulmonic valve closing) -- A2 comes slightly ahead of P2, though you usually hear them together as one sound (sometimes you can hear them separately as a split heart sound, esp. with inspiration).
|
|
|
How can someone tell between pneumonia and bronchitis?
|
Both have some similar symptoms; however, bronchitis involves an inflammation of the bronchi, resulting in excess mucuous, whereas pneumonia involves an infection of one or both lungs. Unlike bronchitis, pneumonia is often associated with shaking chills, chattering teeth and fevers that exceed 102 degrees. If someone has pneumonia, he may also cough up blood in addition to mucus. Bronchitis does not usually require hospitalization, as symptoms pass over time or are quelled through antibiotics. Pneumonia on the other hand will often require hospitalization as respiratory infections begin to interfere with breathing. These infections can also enter the bloodstream and spread to other organs.
Pneumonia more often results in extreme lung complications. Lung abscesses and pleural effusion are two of these. Lung abscesses are pus-filled cavities that form in the infected lobes of the lungs. Pleural effusion occurs when internal fluid builds between the lungs and chest wall, interfering with breathing. |
|
|
What is the main symptomatic difference between asthma and emphysema?
|
The biggest difference between asthma and COPD with regard to symptoms is that asthma fluctuates daily (one day can be symptom free while another symptoms flare on another). COPD does not fluctuate. Symptoms progress with age and exposure to external environmental factors, such as smoke and dust.
|
|
|
True or false - TB is associated with night sweats and purulent sputum.
|
True
|

