![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
147 Cards in this Set
- Front
- Back
|
What are the unique features of the brain/spinal cord?
|
- Blood brain barrier
- Rigid skull / vertebral canal |
|
|
What is the function of the blood brain barrier?
|
Protects from organisms, but also restricts immune system access
|
|
|
What are the implications of the rigid skull / vertebral canal on infection of the nervous system?
|
With inflammation that leads to swelling it can lead to neurologic damage
|
|
|
What are the types of infection of the nervous system?
|
- Leptomeningeal inflammation
- Parenchymal inflammation - Subdural or epidural inflammation |
|
|
What are the type(s) of leptomeningeal inflammation?
|
Meningitis
|
|
|
What are the type(s) of parenchymal inflammation?
|
- Encephalitis / cerebritis (brain) / myelitis (spinal cord)
- Brain abscess |
|
|
What is the term for when the meninges and the brain tissue are infected?
|
Meningoencephalitis
|
|
|
What are the type(s) for subdural or epidural inflammation?
|
Subdural / epidural epmyemas (external to the brain)
|
|
|
How does infection manifest / spread to the brain?
|
- Hematogenous spread (arterial or retrograde venous spread)
- Local extension (air sinuses, infected tooth) - Neural route (extension from PNS to CNS) - Direct implantation (trauma, iatrogenic like in OR) |
|
|
Specifically how does an infection spread via retrograde venous spread?
|
- Anastomotic connections between face veins and cerebral circulation
- Paravertebral venous plexus, Batson |
|
|
What does "neurotropism" mean?
|
A special affinity for nervous tissue (eg, infections predisposed for the brain)
|
|
|
What are the mechanisms of neurotropism by infections?
|
- Viral specific receptors on brain cells
- Capsule proteins that adhere to meninges that possess anti-phagocytic properties - Viral spread along nerves |
|
|
Which infections exhibit neurotropism via viral specific receptors on the brain cells? What tissues?
|
- Poliovirus: for motor neurons of anterior horns of spinal cord
- Mumps virus: for ependymal cells lining ventricles |
|
|
Which infections exhibit neurotropism via capsule proteins that adhere to meninges and possess antiphagocytic properties? What tissues?
|
- Group B Streptococci
- E. coli subtypes |
|
|
Which infections exhibit neurotropism via viral spread along nerves? What tissues?
|
- Herpes simplex virus
- Rabies - Varicella zoster virus |
|
|
What are the clinical signs/symptoms of meningitis?
|
- Headache
- Photophobia - Stiff neck (nuchal rigidity) - Clouded consciousness - Fever |
|
|
What are the clinical types of meningitis? Time line?
|
- Hyperacute (<24 hours)
- Acute (2-7 days) - Subacute / chronic (>1 week) - Aseptic |
|
|
What is the cause of "hyperacute" meningitis? Timeline? Characteristics?
|
- Meningococcal meningitis
- < 24 hours - Sparse inflammation, numerous organisms, congestion |
|
|
What is the cause of "acute" meningitis? Timeline? Characteristics?
|
- Usually bacterial
- 2-7 days - Usually results from hematogenous spread |
|
|
What is the cause of "subacute/chronic" meningitis? Timeline? Characteristics?
|
- Tuberculosis or syphilis (often brain parenchyma is also affected)
- > 1 week - Lymphocytes, plasma cells, macrophages appear in the exudate |
|
|
What is the cause of "aseptic" meningitis? Characteristics?
|
- Usually viral (arboviruses, enteroviruses - echovirus and coxsackie)
- Much less fulminant than bacterial meningitis - Less severe symptoms - More common in summer and early fall - Lymphocytic infiltrate in meninges |
|
|
What type of meningitis has an exudate that contains lymphocytes, plasma cells, and macrophages? Cause? Timeline?
|
- Subacute / Chronic (>1 week)
- Tuberculosis an syphilis - Often brain parenchyma is also affected |
|
|
What type of meningitis is associated with sparse inflammation, numerous organisms, and congestion? Cause? Timeline?
|
- Hyperacute (<24 hours)
- Meningococcal meningitis |
|
|
What type of meningitis is much less fulminant than bacterial meningitis and has less severe symptoms? Cause? Other characteristics?
|
- Aseptic
- Usually viral (arboviruses, enteroviruses - echovirus and coxsackie) - Summer and early fall - Lymphocytic infiltrate in meninges |
|
|
What type of meningitis is the most common infection in the CNS? Cause? Timeline?
|
- Acute (2-7 days)
- Usually bacterial cause - Usually results from hematogenous spread |
|
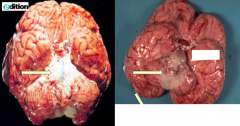
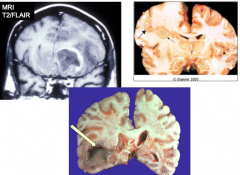
What do these images show?
|
Meningitis
- Thick white exudate overlying the pons - On the rest of the brain you can see how the meninges should look (clear) - Some have a predilection for the base of the brain |
|

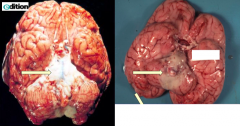
What does this image show?
|

Thick meninges (gray tissue is acute inflammatory cells and fibrin)
|
|
|
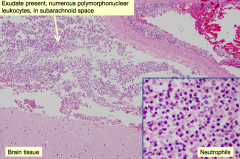
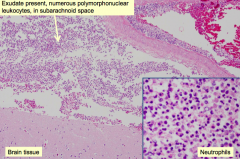
What is the histologic appearance of acute bacterial meningitis?
|
- Exudate in subarachnoid space contains numerous polymorphonuclear leukocytes
- Margination of neutrophils (PMNs) |
|
|
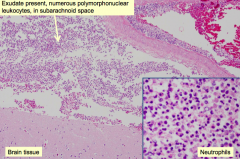
What are the complications of bacterial meningitis?
|
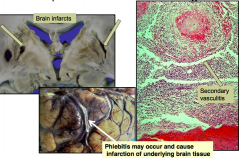
- Severe inflammatory response can cause a secondary vasculitis, may lead to a brain infarct
- Phlebitis may occur and cause infarction of underlying brain tissue |
|
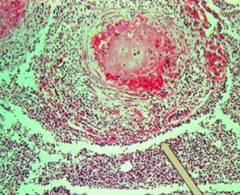
What does this image show?
|
Secondary vasculitis due to the meningitis
|
|
|
What are the causative organisms of Aseptic Meningitis? Most common?
|
- Arbovirus
- Enterovirus (most common): echovirus and coxsackie |
|
|
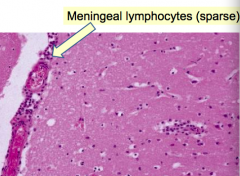
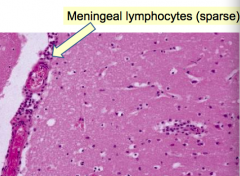
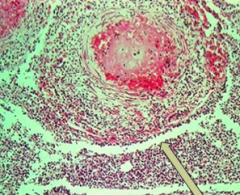
What kind of infiltrate is associated with aseptic meningitis?
|
Meningeal lymphocytes (sparse)
|
|
|
How can parenchymal infections manifest themselves?
|

Brain abscesses - circumscribed focus of infection
- Fibroblastic response leads to a capsule wall - Inside contains the pathogen - Outside contains reactive astrocytes |
|
|
What are the clinical symptoms of parenchymal infections / brain abscesses?
|
- Focal deficits
- Raised intracranial pressure |
|

What is usually the cause of a brain abscess in the parenchyma?
|
Usually bacterial or fungal
Immunocompetent host: - Strep and Staph Immunocompromised host: - Toxoplasma - Nocardia - Listeria - Gram negative bacilli - Mycoacteria - Fungi |
|
What do these images show?
|
Brain abscesses
- Tend to move towards the ventricles - Abscess may burst into the ventricle and fill it with purulent material |
|
|
What is the histological appearance of a brain abscess?
|
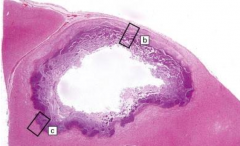
- Center is necrotic
- Edges contain inflammatory cells and fibrous capsule - Presence of giant cells (in non-bacterial infections) |
|
|
What is the term for inflammation of the CNS?
|
- Brain parenchyma: encephalitis
- Spinal cord: myelitis - Meninges and brain parenchyma: meningoencephalitis |
|
|
What are the causes of meningoencephalitis?
|
Bacterial
- Tuberculosis - Syphilis - Lyme disease Viral Fungal |
|
|
What is the causative agent of tuberculosis? How often does infection involve the CNS? Risk factor?
|
- Mycobacterium tuberculosis
- 10-15% of cases involve the CNS: meningoencephalitis (most common form) - HIV infection is a risk factor |
|
|
What kind of infections can tuberculosis cause in the CNS?
|
- Meningoencephalitis (most common)
- Tuberculoma - Osteomyelitis (spinal cord) |
|
|
What is the most common form of TB in the CNS? Impact on CSF? Symptoms?
|
Meningoencephalitis
- CSF: elevated pressure and protein, decreased glucose, lymphocytic pleocytosis (lots of lymphocytes in CSF) - Non-focal symptoms: headache, lethargy, confusion, vomiting |
|
|
How do you diagnose meningoencephalitis caused by TB?
|
- Cultures for Acid Fast Bacilli (AFB) in CSF are positive in 50%
- PCR for TB now always performed on CSF |
|
|
What happens to the CSF during meningoencephalitis caused by TB?
|
- Elevated pressure
- Elevated protein - Decreased glucose - Lymphocytic pleocytosis (lots of lymphocytes in CSF) |
|
|
What happens to the meninges during meningoencephalitis caused by TB?
|
- Contains lymphocytes and macrophages
- Granulomas may extend into underlying brain |
|
|
What is the gross appearance of TB meningitis?
|
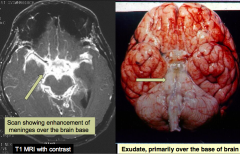
Appearance is not specific for TB meningitis
- Basilar meningitis contains exudate - Increased brightness on MRI |
|
|
What is the histologic appearance of TB meningitis?
|
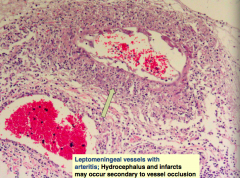
- Secondary vasculitis (in particular occurs with TB)
- Can cause infarcts or occlude CSF in the ventricular system leading to hydrocephalus - Vein is being pointed at, contains leukocytes |
|
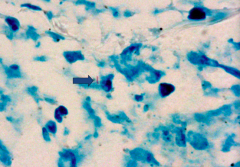
What does this image show?
|
Acid Fast Bacilli (AFB) stain showing positive bacillus (sign of TB infection)
|
|
|
Besides a meningoencephalitis, what other form can tuberculosis infection take?
|

Tuberculoma
- Mass lesion with central necrotic core of caseation - Surrounded by fibroblasts, epithelioid histiocytes, giant cells, and lymphocytes - Acid Fast Bacilli (AFB) are present in the necrosis |
|
|
What is the histologic appearance of a tuberculoma?
|
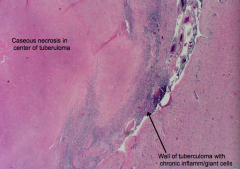
- CASEOUS necrosis in center of tuberculoma
- Wall of tuberculoma contains CHRONIC inflammatory cells: giant cells and mononuclear cells |
|
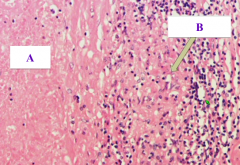
What does this image show?
|
Tuberculoma
- A = Caseous Necrosis - B = Granulomatous inflammation in the wall with mononuclear cells (should also show giant cells, but none pictured here) |
|
|
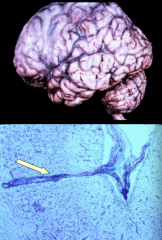
What happens when tuberculosis infects the spinal column (osteomyelitis)?
|

Causes Spondylitis, aka Pott's Disease
|
|
|
What are the implications of Pott's Disease?
|

- Granulomatous process involves vertebral bodies and discs
- Causes epidural abscess - Cord compression and vertebral collapse - Epidural extension of the granulomatous inflammation (arrows) |
|
|
What is the cause of neurosyphilis?
|
Tertiary stage (months / years) of Treponema pallidum infection
|
|
|
How common is neurosyphilis in patients with a syphilis infection?
|
~10% of untreated patients develop tertiary syphilis
|
|
|
What are the major forms of Neurosyphilis (tertiary stage of Treponema pallidum infection)?
|
- General paresis (paretic neurosyphilis)
- Meningovascular disease - Tabes dorsalis |
|
|
What happens in the General Paresis form of Neurosyphilis (tertiary stage)? Symptoms?
|
- Meningoencephalitis: thickened meninges (see cloudiness) and atrophic brain
- Meninges and parenchyma contain lymphocytes, plasma cells, and microglia in the perivascular space (can then spread into the parenchyma) - Gradual impairment of cognition and attention |
|
|
What happens in the Meningovascular form of Neurosyphilis (tertiary stage)? Symptoms?
|
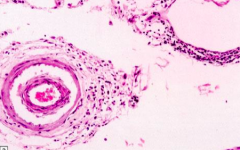
Chronic meningitis and multifocal arteritis:
- Severe at base of brain - Causes infarcts and hydrocephalus - Meninges and arteries/arterioles contain lymphocytes and plasma cells with collagenous thickening of wall and eventual occlusion - Often causes focal neurologic deficits due to vascular compromise secondary to arteritis |
|
|
Which form of neurosyphilis is similar in appearance to TB?
|
Meningovascular type
- Severe at base of brain - Causes infarcts and hydrocephalus - Meninges and arteries/arterioles contain lymphocytes and plasma cells with collagenous thickening of wall and eventual occlusion |
|
|
What happens in the Tabes Dorsalis form of Neurosyphilis (tertiary stage)? Symptoms?
|
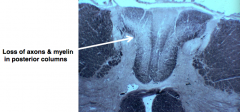
- Chronic inflammation in dorsal roots and ganglia with loss of neurons and associated degeneration of POSTERIOR COLUMNS (axons and myelin)
- Lightening pains or paresthesias in affected roots - Eventual loss of position / vibration sense - shuffling broad-based gait |
|
|
What are the specific organisms that cause VIRAL (meningo)encephalitis?
|
- Arbovirus
- Herpes virus (Herpes Simplex 1, Herpes Simplex 2, CMV, Varicella-Zoster) - HIV - Progressive multifocal leukoencephalopathy (PML) |
|
|
What are the general features of VIRAL (meningo)encephalitis?
|
- Perivascular lymphocytes
- Microglial nodules - Neuronophagia |
|
|
What is the characteristic microscopic appearance of VIRAL (meningo)encephalitis?
|
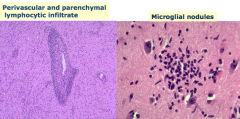
- Perivascular and parenchymal lymphocytic infiltrate
- Microglial nodules - Neuronophagia |
|
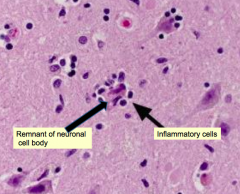
What does this image show? What is it a sign of?
|
Neuronophagia - sign of VIRAL (meningo)encephalitis
|
|
|
What is the most common cause of sporadic acute viral encephalitis in temperate climates?
|
Herpes simplex virus type 1
|
|
|
What are the symptoms of a Herpes simplex virus type 1 infection in the CNS?
|
- Headache
- Fever * Mood, memory, behavior abnormalities - Drowsiness - Coma |
|
|
Where does Herpes simplex virus type 1 affect the brain?
|
Focal abnormalities in the frontal or temporal lobes
|
|
|
What happens to the CSF in a Herpes simplex virus type 1 infection of the CNS? Diagnostic?
|
- Increased pressure
- Lymphocytic pleocytosis - Elevated protein - PCR for HSV1 DNA |
|
|
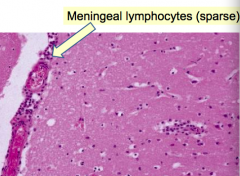
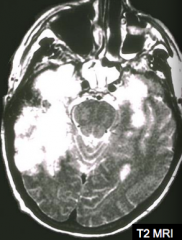
What are the acute findings of acute Herpes simplex virus type 1 encephalitis?
|
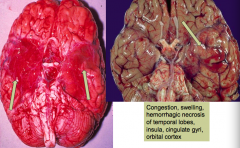
- Congestion and swelling
- Hemorrhagic necrosis of temporal lobes, insula, cingulate gyri, and orbital cortex |
|
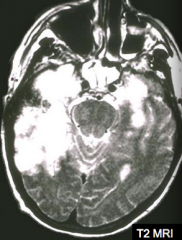
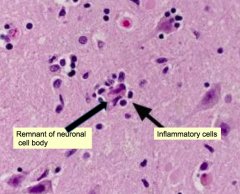
If your patient has this MRI and presents with mood, memory, and behavioral abnormalities, what should you consider? How should you confirm this diagnosis?
|
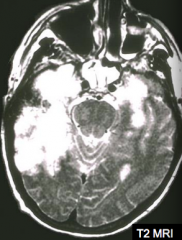
Herpes simplex virus type 1 infection
- PCR for HSV1 DNA in the CSF |
|
|
What are the microscopic findings of acute Herpes simplex virus type 1 encephalitis?
|
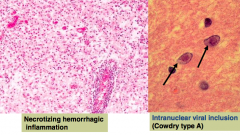
- Necrotizing hemorrhagic inflammation
- Intranuclear viral inclusions (Cowdry type A) |
|
|
Who is more commonly affected by Herpes Simplex Virus type 2 infection of the CNS? Implications?
|
Neonates passing through the birth canal in a mother with an active HSV2 infection (causes meningitis)
|
|
|
What is the most common opportunist viral infection in AIDS patients that can infect the CNS?
|
Cytomegalovirus (CMV)
|
|
|
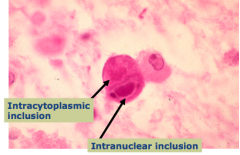
What happens with a Cytomegalovirus (CMV) infection of the CNS?
|
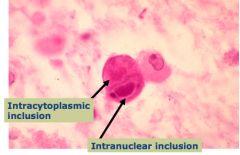
Subacute encephalitis
- Microglial nodules - Cytomegalic cells contain viral inclusions - may be either intranuclear or intracytoplasmic |
|
|
What causes a Varicella Zoster infection of the CNS? Where? What happens?
|
- Reactivation of latent virus residing in the sensory ganglia
- Vesicles form in dermatome distribution - Followed by scar and pain - Dorsal root ganglia or sensory cranial nerve ganglia contain lymphocytes, sometimes with necrosis |
|
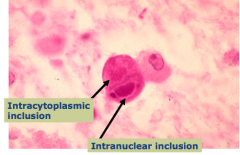
What causes this?
|
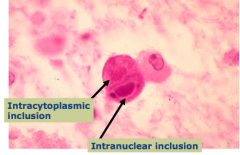
Cytomegalovirus (CMV) infection
|
|
|
What are some important causes of epidemic encephalitis? How do you identify the specific virus?
|
Arboviruses:
- West Nile - Eastern, Western Equine - Venezuelan - St. Louis - California * Identify the specific virus with PCR |
|
|
What kind of virus is HIV?
|
- RNA virus
- Retrovirus |
|
|
What cells are most commonly infected in CNS by HIV? Types of involvement?
|
- Microglia are the most common cells infected in the CNS by HIV
Types of involvement: - HIV meningitis - HIV encephalitis / leukoencephalopathy - Vacuolar myelopathy |
|
|
How/when does an HIV meningitis present?
|
During acute flu-like illness at time of seroconversion
|
|
|
How/when does an HIV encephalitis / leukoencephalopathy present?
|
Present in >75% of autopsied HIV patients
|
|
|
What are the signs / symptoms of HIV encephalitis / leukoencephalopathy?
|
AIDS dementia complex:
- Cognitive and behavioral deterioration - Eventually dementia, ataxia, and tremor |
|
|
What happens to the brain with HIV encephalitis / leukoencephalopathy?
|
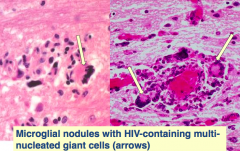
- Slight diffuse atrophy
** Classic lesion: microglial nodule containing multinucleated microglial cells (that contain HIV virus) - Also perivascular lymphocytes, patchy demyelination, and astrocytosis |
|
|
What is the classic sign of an HIV infection in the brain?
|
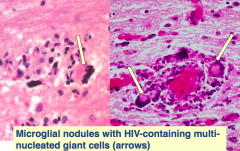
HIV encephalitis / leukoencephalopathy:
- Microglial nodules with HIV-containing multi-nucleated giant cells (arrows) |
|
|
What causes progressive multifocal leukoencephalopathy? Who is affected by it?
|
- Caused by JC virus - polyomavirus
- Occurs in immunocompromised hosts (often AIDS patients) |
|
|
What cells are affected by progressive multifocal leukoencephalopathy?
|
Oligodendrocytes
|
|
|
What is necessary to cause progressive multifocal leukoencephalopathy?
|
- Must have serologic evidence of prior JC virus infection by adolescence (most are infected with this by adolescence)
- JC virus is re-activated with immunosuppression |
|
|
What is the gross and microscopic appearance of progressive multifocal leukoencephalopathy?
|
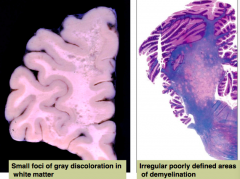
- Small foci of gray discoloration in white matter (leuko - white matter)
- Irregular, poorly defined areas of demyelination |
|
|
What is the characteristic inclusion in progressive multifocal leukoencephalopathy? Which cells are affected?
|
Oligodendrocytes
|
|
|
What are the causes of fungal (meningo)encephalitis?
|
- Candida
- Mucor - Aspergillus - Cryptococcus - Histoplasma - Coccidiodes - Blastomyces |
|
|
Who is typically affected by fungal (meningo)encephalitis?
|
- Commonly occur in immunocompromised hosts
- Occasionally occur in immunocompetent hosts |
|
|
What are the patterns of damage by fungal (meningo)encephalitis?
|
- Chronic meningitis
- Parenchymal invasion (encephalitis) - Vasculitis (especially Aspergillus and Mucor) - which can cause hemorrhagic infarcts |
|
|
What does Aspergillus brain infection look like?
|
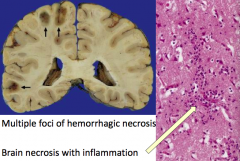
- Multiple foci of hemorrhagic necrosis
- Brain necrosis with inflammation |
|
|
Where does Aspergillus often infect in the brain?
|
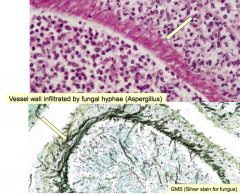
Vessel wall is often infiltrated by fungal hyphae
|
|
|
Where does Cryptococcus neoformans infect?
|
- Affects lungs first usually
- Spreads hematogenously to the brain |
|
|
Who is affected by Cryptococcus neoformans?
|
Most often in immunosuppressed patients, but may occur in immunocompetent hosts
|
|
|
Where is Cryptococcus neoformans found?
|
Found in soil and bird excreta
|
|
|
What are the main forms of Cryptococcus neoformans in the CNS?
|

- Meningitis with or without brain parenchymal cysts (encephalitis)
- Abscesses (Cryptococcomas) |
|
|
What happens to the CSF with a Cryptococcus neoformans infection? How do you diagnose infection?
|
- CSF contains lymphocytes, high protein, and normal or reduced glucose
- India ink stains allows for identification of the organism (by negative staining of the capsule) - Assay for presence of Cryptococcal antigen is more sensitive |
|
|
What is the gross appearance of a brain infected by Cryptococcus neoformans?
|
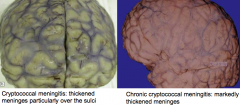
(Picture looks like all forms of meningitis)
- Cryptococcal meningitis: thickened meninges particularly over the sulci - Chronic cryptococcal meningitis: marked thickening of meninges - Multiple intraparencymal cysts (also called soap bubbles) secondary to gelatinous capsular material (distinctive) |
|
|
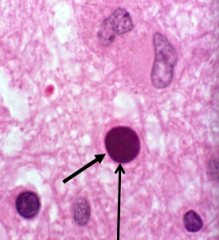
What is the histologic appearance of Cryptococcus meningitis?
|
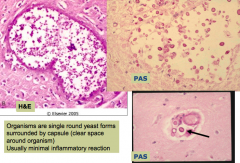
- Organisms are single round yeast forms surrounded by a capsule (clear space around organism = bottom right picture)
- Usually minimal inflammatory reaction |
|
|
What parasite can infect the CNS?
|
Single-celled organisms
- Amoeba - Plasmodium (Malaria) - Toxoplasma gondii (protozoa) - Trypanosoma (sleeping sickness) - Cysticercus (Taenia solium) |
|
|
Who is affected by parasite infections of the CNS?
|
Both immunocompetent and immunosuppressed (where infection is more severe)
|
|
|
What do parasites that infect the nervous system cause?
|
- Meningoencephalitis
- Abscesses |
|
|
Who are the hosts for Toxoplasma gondii (protozoa)? Who is infected?
|
- Humans are the intermediate host
- Cats are the definitive host - More important infection in immunocompromised hosts (especially AIDS patients) - Uncommon in healthy adults |
|
|
How do you get infected with Toxoplasma gondii?
|
- Infection secondary to ingestion of contaminated food (cat feces) or raw/undercooked meat from another intermediate host (sheep/pig)
- Congenital infection: transmission to fetus if infection occurs during pregnancy |
|
|
What is the most common cause of mass lesions in CNS in AIDS patients?
|
Toxoplasma gondii - an important infection in immunocompromised hosts, especially AIDS patients
|
|
|
What happens to the brain in a person infected with Toxoplasma gondii?
|
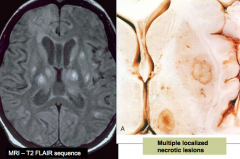
Multiple localized necrotic lesions
- Organisms are found within pseudo cysts or free in tissue |
|
|
What is the histologic appearance of Toxoplasma gondii?
|
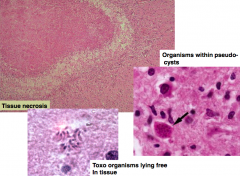
- Tissue necrosis
- Toxo organisms can be found within pseudocysts or lie free in tissue |
|
|
What causes epidural and subdural empyemas?
|
- Usually bacterial (staph or strep commonly)
Can be due to local extension of infectious process from: - Frontal or mastoid sinusitis - Otitis media - Trauma - Osteomyelitis - Surgical procedure |
|
|
What is the approach to assessing a possible CNS infection?
|
- Localize symptoms and signs
- Identify exposures and travel history - Routine labs - Neuro imaging - Lumbar puncture - Need for empiric therapy |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam What is the most likely diagnosis and microbial etiology? |
Acute meningitis (based on presentation)
- Most likely etiology: Streptococcus pneumoniae (most common cause of bacterial meningitis) |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam IF he was older (~66 year old) or was an alcoholic, what would be the more likely microbial etiology? |
Listeria monocytogenes
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam IF he had AIDS and had symptoms for a couple of weeks, what would be the more likely microbial etiology? |
Cryptococcus neoformans
- Meningitis presents for a few weeks and may present with focal deficits (usually a CN deficit) and also increases intracranial pressure (could also be Tuberculosis, but would need other risk factors) - People who have been sick for a few weeks do not have bacterial meningitis (they would have died if they had it that long ago without being treated) |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam IF he was a neurosurgery patient, what would be the more likely microbial etiology? |
Staphylococci (epidermidis is the #1 cause of wound infections or aureus)
Also could be: - G- rods that cause nosocomial infections: E. coli Caused because they don't have the normal protective barriers d/t surgery |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam IF he was a freshman college student living in a dorm, what would be the more likely microbial etiology? |
Neisseria meningitidis (meningococcal meningitis)
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam IF he presents not quite as sick and in the SUMMER, what would be the more likely microbial etiology? |
Enteroviruses: echovirus and coxsackie (Aseptic Meningitis)
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam IF he was an Asian immigrant who has been sick for a few weeks, what would be the more likely microbial etiology? |
Mycobacterium tuberculosis (Asia has a greater incidence of TB)
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam (And in all of the "what if" situations) What do you want to do next? |
* Lumbar Puncture - need to see what their spinal fluid looks like
- Exception: CT or MRI in certain situations (if the person is at risk for herniation) Increased risk for herniation, if: - Increased intracranial pressure - Patients who are immune compromised - Patients with focal neuro deficits imply a space occupying lesion that could cause increased intracranial pressure |
|
|
What are the clues for the etiology of meningitis?
|
- Age (infant vs child vs adult vs elderly)
- Acuity and severity - Time of year - Other symptoms that indicate a systemic infection - Risk factors and immunologic status (travel, exposures, HIV, immunosuppressive therapy) - CSF findings |
|
|
How does the acuity / severity help you determine the etiology of the CNS infection?
|
- Bacterial: few days and rapid
- Viral: several days, subacute - TB / Fungal: weeks to months, chronic |
|
|
When is a viral CNS infection more common?
|
Late summer and early fall
|
|
|
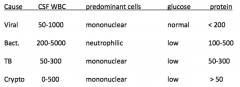
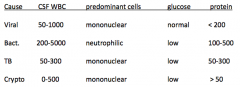
What are the Lumbar Puncture signs of a viral CNS infection?
- CSF WBC - Predominant cells - Glucose - Protein |
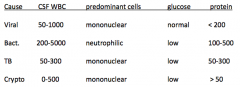
- CSF WBC: 50-1000
- Predominant cells: mononuclear - Glucose: normal - Protein: <200 |
|
|
What are the Lumbar Puncture signs of a bacterial CNS infection?
|
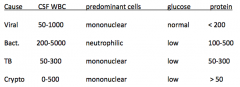
- CSF WBC: 200-5000
- Predominant cells: neutrophilic - Glucose: low - Protein: 100-500 |
|
|
What are the Lumbar Puncture signs of a TB CNS infection?
|
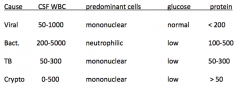
- CSF WBC: 50-300
- Predominant cells: mononuclear - Glucose: low - Protein: 50-300 |
|
|
What are the Lumbar Puncture signs of a Crypto CNS infection?
|
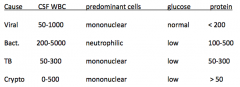
- CSF WBC: 0-500
- Predominant cells: mononuclear - Glucose: low - Protein: >50 |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs How does this help you in differential diagnosis? |
- High WBC count with almost all PMNs indicates a bacterial meningitis
- Low glucose tells you it is serious - Protein being high tells you there is something wrong (non-specific) |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs What if the differential was 85% mononuclear? |
Fungus (Cryptococcus)
- Not viral because normal glucose - Less likely TB because WBC >400 |
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs What if the CSF glucose was 75? |
Viral meningitis (or could be a partially treated bacterial meningitis)
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs What other tests do you want? |
- Culture
- Gram stains |
|
|
If the Lumbar Puncture glucose is normal, what do you suspect as the etiology?
|
Virus
|
|
|
If the Lumbar Puncture results shows predominantly neutrophilic cells, what do you suspect as the etiology?
|
Bacteria
|
|
|
How do you distinguish TB from Crypto (fungus) as the cause of meningitis based on Lumbar Puncture?
|
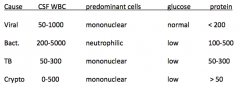
- TB will have WBC < 300 and protein < 300
- Crypto may have WBC from 0-500 and protein >50 |
|
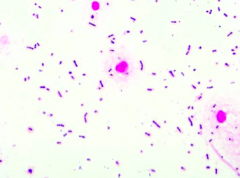
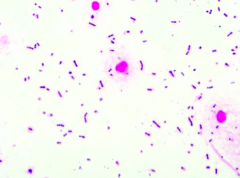
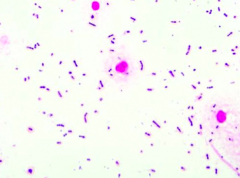
Case 1:
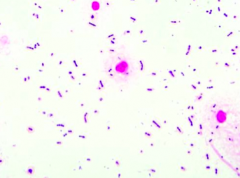
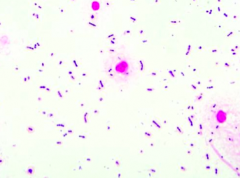
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs CSF Gram stain is shown. Cultures are pending. What do you think is the diagnosis? |
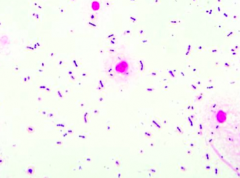
Purple cocci in pairs and short chains: Strep pneumo
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs CSF Gram stain is shown. Cultures are pending. What would you do next in terms of therapy and why? |
Start IV Ceftriaxone, Vancomycin, and Corticosteroids
- Ceftriaxone is the preferred agent for pneumococcal meningitis - Vancomycin is in case it is a penicillin-resistant pneumococcus - Corticosteroids are to reduce pathologic inflammation |
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs CSF Gram stain is shown. Cultures are pending. Would you wait until culture and susceptibility results return to select the appropriate antimicrobial therapy? Why or why not? |
No - this would be malpractice - they could die while you wait
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs CSF Gram stain is shown. Cultures are pending. Would you give IV ceftriaxone, vancomycin, and corticosteroids? Why or why not? |
Yes:
- Ceftriaxone is the preferred agent for pneumococcal meningitis - Vancomycin is in case it is a penicillin-resistant pneumococcus - Corticosteroids are to reduce pathologic inflammation |
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs CSF Gram stain is shown. Cultures are pending. Would you start PO rifampin, isoniazid, pyrazinamide, ethambutol, and corticosteroids? Why or why not? |
No - this would be the treatment for TB
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs CSF Gram stain is shown. Cultures are pending. Would you start IV amphotericin B? Why or why not? |
No - this would be for empiric fungal coverage
|
|
|
How do you treat streptococcus meningitis?
|
Start IV Ceftriaxone, Vancomycin, and Corticosteroids
- Ceftriaxone is the preferred agent for pneumococcal meningitis - Vancomycin is in case it is a penicillin-resistant pneumococcus - Corticosteroids are to reduce pathologic inflammation |
|
|
How do you treat TB meningitis?
|
PO: rifampin, isoniazid, pyrazinamide, ethambutol, and corticosteroids
|
|
|
How do you treat fungal meningitis?
|
IV amphotericin B
|
|
|
Case 1:
- 43 yo male presents in December w/ 2 days of worsening fever, headache, stiff neck - Also seems very sleepy - No known sick contacts, no allergies or meds - Up to date on vaccines - Febrile to 102.4 and somnolent w/ meningismus (nuchal rigidity) - Non-focal neuro exam Lumbar Puncture results: - Protein 156 - Glucose 21 (serum 106) - WBC 429 w/ differential of 99% PMNs IF the Gram stain was negative and the patient was 66 years old or alcoholic, what would you do next in terms of therapy and why? |
Start IV Ceftriaxone, Vancomycin, and Corticosteroids
- Ceftriaxone is the preferred agent for pneumococcal meningitis - Vancomycin is in case it is a penicillin-resistant pneumococcus - Corticosteroids are to reduce pathologic inflammation Add high dose IV ampicillin to the empiric regimen to cover for Listeria monocytogenes |
|
|
What can be done to try to prevent bacterial meningitis?
|
Immunizations for pneumococcus, meningococcus, and H. influenzae
|
|
|
Why do you give corticosteroids for bacterial meningitis?
|
Reduces pathologic inflammation - improves outcomes
|
|
|
What are the principles of therapy for CNS infections?
|
- Prompt initiation of empiric coverage, especially if bacterial etiology suspected
- High doses with frequent dosing because blood-brain barrier lowers levels (CSF penetration is essential for activity) - Cidal agents are needed instead of static (because not a lot of WBCs typically in the CSF) |
|
|
Case 2:
- 62 yo female brought to ED in December by family because she has been acting crazy for a few days - Auditory hallucinations and bizarre behavior - Also complains of headache - Afebrile and no stiff neck - Arousable but disoriented and uncooperative w/ exam - No focal neuro deficits, PMHx, and not on meds What is wrong and what is the most IMPORTANT microbial etiology (not necessary most likely? |
Encephalitis - most likely HSV (predilection for temporal lobes)
|

