![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
Overview. |
pH measurement of acidity or alkalinity of the blood. its proportional to the number of hydrogen ions (H+) in the blood. The more H+ present, the lower the pH is. The fewer H+ present, the higher pH is. |
|
|
The Respiratory Buffer Response |
CO2 is carried in the blood to the lungs, where excess CO2 combines with water (H2O to form carbonic acid (H2CO3) The blood pH will change according to the level of carbonic acid present. this triggers the lungs to either increase or decrease rate and depth of ventilation until the appropriate amt of CO2 has been reestablished. |
|
|
The Renal Buffer Respons |
In an effort to maintain the pH of blood normal, the kidneys excrete or retain bicarb (HCO3-) as the blood pH decreases, the kidneys will compensate by retaining HCO3- and as pH rises, they will excrete HCO3- thru urine. |
|
|
ACID BASE DISORDERS |
Respiratory Acidosis Respiratory Alkalosis Metabolic Acidosis Metabolic Alkalosis |
|
|
Respiratory Acidosis |
pH < 7.35 and PaCO2 > 45 what is it? accumulation of CO2 (lots of carbonic acid) so caused by Hypoventilation (head injury, meds that depress CNS, SCI, pulmonary disorders) s/s: drowsy, unresponsive correction: increase ventilation |
|
|
Respiratory Alkalosis |
pH >7.45 and PaCO2 <35 what is it? blowing off too much CO2. caused by a condition that causes hyperventilation (anxiety, feat, pain, fever, sepsis, pregnancy, meds) s/s: light head, numbness, confusion, blurred, dry mouth, spasms Treatment: treat underlying cause |
|
|
Metabolic Acidosis |
pH <7.35 and HCO3- <22 what is it? increase in acids (other than CO2) or deficit of base in the bloodstream. caused by diarrhea, renal failure, DKA, starvation |
|
|
Metabolic Alkalosis |
pH >7.45 and HCO3- >28 what is it? an excess of a base or a loss of acid within the body can cause this. causes are ingestion of antacids, excess use of bicarb, or loss of acids from vomiting, gastric suctioning, too many diuretics, or high lvls of aldosterone. |
|
|
LAB VALUES: Chemistries |
NA: 136-145 CA: 9.0-10 CHLORIDE: 98-106 HCO3: 21-28 K: 3.5-5.0 PO4: 3.0-4.5 MAG: 1.3-2.1 |
|
|
LAB VALUES: Cholesterol/Glucose/ Liver/Pancreatic Enzymes |
STOMACH PH: 1.5-2.5 AMMONIA: 15-110 BILIRUBIN: total 0.-1.0, unconjugated 0,2-0,8, conjugated 0.1-1 urine specific gravity 1.015-1.030, urine pH 4.6-8.0, BUN 10-20, CR 0.6-1.2 Cholesterol: total <200; LDL (bad) <100; HDL >40; trig <150 Liver Enzymes: ALT: 8-20; AST 5-40; total protein 6-8 Pancreatic Enzym: amylase 56-90, lipase 0-100, prothrombin time 0.8-1.2 Glucose: (fasting) 70-110, postprandial 70-140, HbA1c <6% |
|
|
LAB VALUES: |
WBC: 5-10k MCV 80-90; MCH 27-31; TIBC 250-460; Iron f60-160 m80-180 PLT: 150-450k HGB: f12-16, m14-18 HCT: f 37-47%; m42-52% |
|
|
LAB VALUES: Coagulation |
PT (coumadin) 1.5-2 norm , 11-14 seconds therapeutic aPTT (Heparin): 1.5-2 norm, 16-40 therapeutic INR(coumadin) : 0.9-1.2 norm , 2-3 therapeutic D-Dimer: 0.42-2.33 or 0-250 Fibrinogen levels: 170-340 Fibrin degradation products: <10 |
|
|
LAB VALUES: Inflammatory Markers |
CRP (C reactive Protein) <3 ESR (erythrocyte sediment rate) 0-22 |
|
|
FLUID AND ELECTROLYTE DISORDERS... |
Sodium Potassium Calcium Magnesium |
|
|
SODIUM |
•Themajor cation in the ECF •Regulatedby aldosterone and ADH •Foundin most body secretions •Functions1.Maintainsblood volume and BP2.Essentialin the electrical transmission of nerve impulses3.Helpmaintain the acid-base balance of the blood4.Vitalcomponent of sodium-potassium pump |
|
|
Hyponatremia causes, s/s |
•Serumsodium less than 135 mEq/L •Causes:adrenal insufficiency, water intoxication, SIADH or losses by vomiting,diarrhea, sweating, diuretics •Manifestations:poor skin turgor, dry mucosa, headache, decreased salivation, decreased BP,nausea, abdominal cramping, neurologic changes |
|
|
Hyponatremia medical and nursing management |
•Medical management: water restriction, sodium replacement •Nursing management: assessment and prevention, dietary sodium and fluid intake, identify and monitor at-risk patients, effects of medications (diuretics, lithium) |
|
|
Hypernatremia: causes, s/s |
•Serumsodium greater than 145mEq/L •Causes:excess water loss, excess sodium administration, diabetes insipidus, heat stroke, hypertonic IVsolutions •Manifestations:thirst; elevated temperature; dry, swollen tongue; sticky mucosa; neurologicsymptoms;restlessness; weakness •Note:thirst may be impaired in elderly or the ill
|
|
|
Hypernatremia: Nursing and Medical Mgmt |
•Medical management: hypotonic electrolyte solution or D5W •Nursing management: assessment and prevention, assess for OTC sources of sodium, offer and encourage fluids to meet patient needs, provide sufficient water with tube feedings |
|
|
POTASSIUM |
•Themost common cation in ICF •Functions1.Facilitatesnerve impulse conduction 2.Essentialfor the normal electrical activity of the heart 3.Keyrole in skeletal and smooth muscle contraction, making it important for normaldigestive and muscular functioning 4.Assistin making protein using amino acids 5.Aidsin the regulation of acid-base balance |
|
|
Hypokalemia: causes, s/s |
•Below-normalserum potassium (<3.5 mEq/L), may occur with normalpotassium levels with alkalosis due to shift of serum potassium into cells •Causes:GI losses, medications, alterationsof acid-base balance, hyperaldosterism, poor dietary intake •Manifestations:fatigue, anorexia, nausea, vomiting, dysrhythmias, muscle weakness and cramps, paresthesias, glucose intolerance, decreasedmuscle strength, DTRs |
|
|
Hypokalemia: medical and nursing mgmt |
•Medical management: increased dietary potassium, potassium replacement, IV for severe deficit •Nursing management: assessment, severe hypokalemia is life-threatening, monitor ECG and ABGs, dietary potassium, nursing care related to IV potassium administration |
|
|
Hyperkalemia: causes, s/s |
•Serumpotassium greater than 5.0 mEq/L •Causes:usually treatment related, impaired renal function, hypoaldosteronism, tissue trauma, acidosis •Manifestations:cardiac changes and dysrhythmias, muscle weakness with potential respiratoryimpairment, paresthesias, anxiety, GI manifestations |
|
|
Hyperkalemia: medical and nursing mgmt |
•Medical management: monitor ECG, limit dietary K, cation-exchange resin (Kayexalate), IV bicarb , IV calcium gluconate, regular insulin & hypertonic dextrose IV, b-2 agonists, dialysis •Nursingmgmt: assess K levels, mix IVs containing K+ well,monitor meds/e, K diet restrictions •Saltsubstitutes, medications may contain potassium •K-sparingdiuretics may cause elevation of K- dont use w renal pts |
|
|
Hypokalemia causes, s/s |
•Below-normalserum potassium (<3.5 mEq/L), may occur with normalpotassium levels with alkalosis due to shift of serum potassium into cells •Causes:GI losses, medications, alterationsof acid-base balance, hyperaldosterism, poor dietary intake •Manifestations:fatigue, anorexia, nausea, vomiting, dysrhythmias, muscle weakness and cramps, paresthesias, glucose intolerance, decreasedmuscle strength, DTRs |
|
|
Hypokalemia: medical and nursing mgmt |
•Medical management: increased dietary potassium, potassium replacement, IV for severe deficit •Nursing management: assessment, severe hypokalemia is life-threatening, monitor ECG and ABGs, dietary potassium, nursing care related to IV potassium administration |
|
|
CALCIUM |
•Mostabundant cation in human body •Functions 1.Assistsin building strong bones and teeth 2.Facilitatesblood clotting 3.Essentialfor nerve impulse transmission 4.Keyrole in skeletal and cardiac muscle contraction and relaxation, making itimportant for normal heart and muscular functioning 5.Assistin the activation of certain enzymes |
|
|
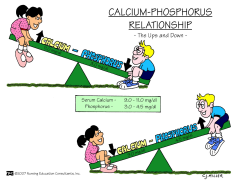
Cal-Phos Relationship |
|
|
|
Hypocalcemia: causes, s/s |
•Serumlevel less than 8.5 mg/dL, must be considered in conjunctionwith serum albumin level •Causes:hypoparathyroidism, malabsorption, pancreatitis, alkalosis, massivetransfusion of citrated blood, renal failure, medications, other•Manifestations:tetany, circumoral numbness, paresthesias, hyperactive DTRs, Trousseau’ssign, Chovstek's sign, seizures, respiratory symptoms ofdyspnea and laryngospasm, abnormal clotting, anxiety |
|
|
Hypocalcemia: medical and nursing mgmt |
•Medicalmanagement: IV of calcium gluconate, calcium and vitamin Dsupplements; diet •Nursingmanagement: assessment, severe hypocalcemia is life-threatening,weight-bearing exercises to decrease bone calcium loss, patient teachingrelated to diet and medications, and nursing care related to IV calciumadministration |
|
|
Hypercalcemia: causes, s/s |
•Serumlevel greater than10.2 mg/dL •Causes:malignancy and hyperparathyroidism, bone loss related to immobility •Manifestations:muscle weakness, incoordination, anorexia, constipation, nausea and vomiting,abdominal and bone pain, polyuria, thirst, ECG changes, dysrhythmias
|
|
|
Hypercalcemia: medical and nursing mgmt |
•Medical management: treat underlying cause, fluids, furosemide, phosphates, calcitonin, biphosphonates •Nursing management: assessment, hypercalcemic crisis has high mortality, encourage ambulation, fluids of 3 to 4 L/d, provide fluids containing sodium unless contraindicated, fiber for constipation, ensure safety |
|
|
MAGNESIUM 1/2 |
•2nd most abundant cationin the body and is required for muscle relaxation after contraction •Severemag deficiency can result in low levels of calcium, potassium, and phosphate inthe blood •Functions1.Maintainsnormal muscle function, nerve function, and heart rhythm2.Supportsa health immune system and aids in the regulation of blood coagulation3.Powersthe sodium-potassium pump and aids in converting ATP to ADP for energy release |
|
|
MAGNESIUM 2/2 |
•Actssynergistically with calcium in hundreds of reactions in the body•Isrequired for calcium and vitamin B12 absorption•StimulatesPTH secretion and fights tooth decay by binding calcium to tooth enamel•Has asedative effect on the neuromuscular junction, which decreases acetylcholinerelease, causing smooth muscle relaxation |
|
|
Hypomagnesemia: causes, s/s, medical mgmt |
•Serum<1.8 mg/dL, evaluate in conjunction withserum albumin •Causes:alcoholism, GI losses, enteral or parenteral feeding deficient in magnesium,medications, rapid administration of citrated blood; contributing causesinclude DKA, sepsis, burns, hypothermia •Manifestations:neuromuscularirritability,muscle weakness, tremors, athetoid movements, ECG changes and dysrhythmias, alterations in mood and level ofconsciousness, increasedtendon reflexes •Medicalmanagement: diet, oral magnesium, magnesium sulfate IV |
|
|
Hypomagnesemia: Nursing mgmt |
•Nursingmanagement: assessment, ensure safety, patient teaching related to diet,medications, alcohol use, and nursing care related to IV magnesium sulfate •Hypomagnesemia often accompanied by hypocalcemia–Needto monitor, treat potential hypocalcemia •Dysphasiacommon in magnesium-depleted patients–Assessability to swallow with water before administering food or medications |
|
|
Hypermagnesemia |
•Serumlevel greater than 2.3 mg/dL •Causes:renal failure, DKA, excessive administration of magnesium •Manifestations:flushing, lowered BP, N/V, hypoactive reflexes, drowsiness, muscleweakness, depressed respirations, ECG changes, dysrhythmias •Medicalmanagement: IV calcium gluconate, loop diuretics, IV NS of RL,hemodialysis •Nursingmanagement: assess, no meds with mag,no OTC with mag |

