![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
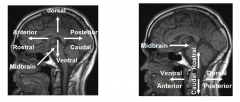
Orientation in the Nervous System
|
|
|
|
Redlich-Obersteiner's
|
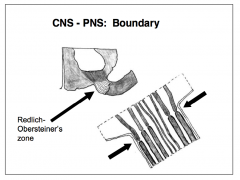
- Transitional zone between the CNS and PNS
- Marked by the basal lamina of the surrounding Schwann cell, the myelinating cell of the peripheral nervous system |
|
|
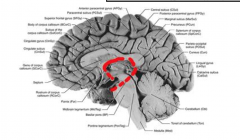
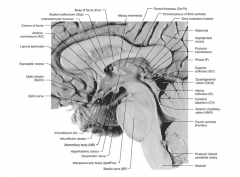
Five parts of the brain
|

During development, the forebrain (prosencephalon: diencephalon and telencephalon) flexes at its junction with the mesencephalon until its rostro- caudal axis corresponds to a line between the frontal and the occipital poles (in the anterior-posterior plane)
|
|
|
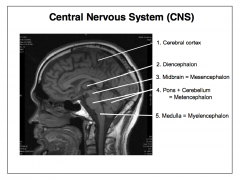
Telencephalon
|
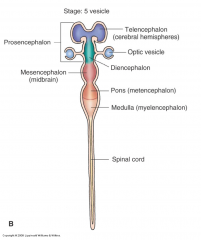
- Lateral ventricles
- Derived from rostral prosencephalon - Cerebral hemispheres - Cerebral cortex - Basal ganglia - Foramina of Monro - Closely tied to olfactory nerves - Planning, driving of motor activity, perceptual and cognitive functions |
|
|
Diencephalon
|
- Interbrain – derived from the caudal prosencephalon
- Thalamus = relaying, modulating sensory input, cortical activity - Hypothalamus (and pituitary) = homeostasis - Subthalamus = motor and sensory - Epithalamus = endocrine - 3rd ventricle - CN II |
|
|
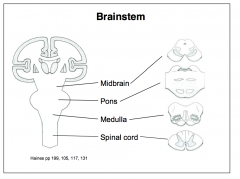
Mesencephalon
|
- Midbrain
- Tegmentum (floor: including cerebral peduncles or crus cerebri) - Tectum (roof: corpora quadrigemina or superior and inferior colliculi) - Cerebral aqueduct - CN III and IV - Function = motor system, eye movements, alertness/arousal |
|
|
Metencephalon
|
- Derived from the rhombencephalon
- Pons = motor from cortex, respiration, taste, sleep/wake - Cerebellum (cerebellar hemispheres and vermis) = somatosensory from spinal cord, posture & balance, smoothes and coordinates movement - Rostral fourth ventricle - CNs V - VIII |
|
|
Myelencephalon
|
- Derived from the rhombencephalon
- Medulla oblongata = respiration, B.P., motor activity of mouth - Caudal fourth ventricle - Foramina of Magendi and Luschka - Central canal of the medulla is continuous with the spinal central canal - CNs IX - XII |
|
|
5 parts of brain - MRI
|
|
|
|
Cerebral Hemispheres
|
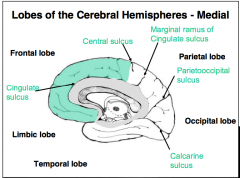
- Cortex, white matter, basal ganglia, amygdala and hippocampal formation
- Divided into: frontal, parietal, temporal, occipital, limbic and insular lobes |
|
|
Layers of the Cerebral Cortex
|
Major portion (about 90%) of the cerebral cortex bears 6 layers, with each distinguishable by a characteristic size
|
|
|
Layer I -- Molecular (plexiform) layer
|
- Very few neuronal somata
- Apical dendrites of cells - deeper cortical layers - Axons passing through or making connections |
|
|
Layer II -- External granular layer
|
- Small granule cells (local interneurons that inhibit other cortical cells) and some slightly larger pyramidal cells
- Communications with ipsilateral cortical areas (via association fibers) |
|
|
Layer III -- External pyramidal layer
|
- Small-to-medium-sized pyramidal neurons projecting from the cortex
- Communications with homotopic contralateral cortices (via commissural fibers) |
|
|
Layer IV -- Internal granular layer
|
- No pyramidal neurons
- Interneurons receiving ascending sensory (thalamocortical) input - projecting to layers II/III - Dense band of tangential axons that form the outer band of Baillarger, which is hypertrophic and visible to the naked eye in a discrete occipital region (forming the stria Gennari of the striate cortex) |
|
|
Layer V -- Internal pyramidal (ganglionic) layer
|
- Medium-to-very-large pyramidal neurons.
- Major source of cortical output to the brainstem and spinal cord - Contains a dense band of tangential axons (i.e., inner band of Baillarger) |
|
|
Layer VI -- Multiform layer
|
- Assortment of cell types, including a few pyramidal cells
- Small cells receive input from the thalamus and from cortical layers II, III, and V. - Axons of the cells in this layer project to superficial cortical layers and also subcortically |
|
|
Circuitry of Cerebral Cortex
|
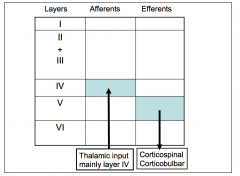
- Largest pyramidal cells are found in layer V of primary motor cortex and can make synaptic connections with caudal spinal motor neurons
- Axons of most thalamo-cortical neurons end in layer IV |
|
|
BASAL GANGLIA
|
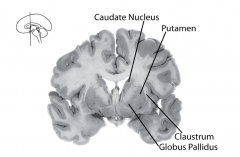
- Groups of neurons that are concerned with the initiation and organization of movement
- Includes: - Caudate nucleus - Putamen - Globus pallidus - Claustrum - Lie close to the lateral ventricles |
|
|
Striatum
|
caudate nucleus + putamen
|
|
|
Lentiform nucleus
|
putamen + globus pallidus
|
|
|
Thalamus
|
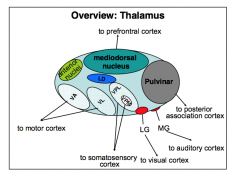
Relays virtually all sensory input to sensory cortices. It also processes output from the basal ganglia and cerebellum to regulate the motor cortex and hence movement.
|
|
|
Hippocampus
|
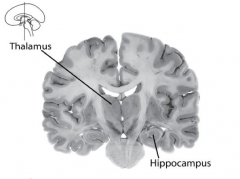
Processes much sensory information that is destined for long-term storage in memory within cortical circuitry.
|
|
|
Amygdala
|
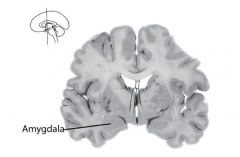
Participates in emotional regulation, perhaps assigning an emotional valence to memory.
|
|
|
Association White Matter
|
- Myelinated axons carrying information from one cortical region to another within the same cerebral hemisphere contribute to association white matter.
- e.g. Repeating the spoken word typically requires transmission of signals from the left temporal lobe to the left frontal lobe via a band of association white matter called the arcuate fasciculus |
|
|
Commissural
|
- Information must also pass from a cortical zone in one hemisphere to a homotopic site in the opposite hemisphere.
- e.g. Correctly naming an unseen object placed in the left hand requires transmission of information from the right parietal lobe to the left - The largest cerebral commissure is the corpus callosum |
|
|
Projection
|
- The cerebral cortex must also interact with subcortical sites
- e.g. Somatosensory input reaches the parietal lobe via white matter projections arising from the thalamus. |
|
|
Brainstem
|
|
|
|
Spinal Cord
|
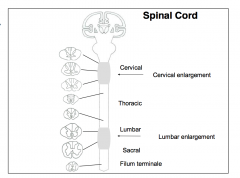
|
|
|
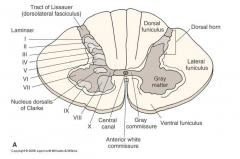
Spinal Cord Cross–section
|
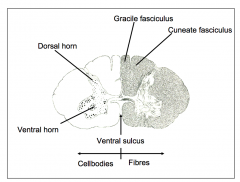
|
|
|
Distribution of White and Grey Matter in Cord
|
- White matter contains myelinated axons carrying commands in descending tracts from the brain to the spinal cord. It also contains ascending axons carrying sensory information from the cord to the brain.
- Grey matter comprises neuronal cell bodies and dendrites. Spinal gray matter may control muscular activity. Other pockets of spinal gray matter process sensory information. |
|
|
Spinal Nerves
|
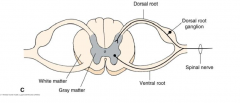
The typical spinal nerve is formed by the union of dorsal and ventral nerve roots. Since the dorsal root, arising from its dorsal root ganglion, carries sensory fibers and the ventral root carries motor fibers, the unified spinal nerve is functionally mixed.
|
|
|
Peripheral Nerve Functions
|
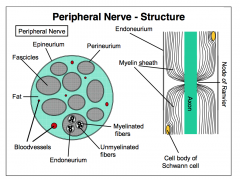
- Carry both sensory and motor information
- Sensory information travels along axons of afferent neurons - Motor information travels along the axons of the lower motor neurons innervating skeletal muscle - All cranial nerves, except CN II, are peripheral nerves |
|
|
Communication between CNS and PNS
|
• Corticobulbar Tract - motor
• Corticospinal (lateral and anterior) tract - motor • Reticulospinal (lateral and medial) tract - motor • Rubrospinal Tract – motor • Vestibulospinal (lateral and medial) Tract - motor • Dorsal Column/Medial Lemniscal System - sensory • Anterolateral System (spinothalamic tract) - sensory |
|
|
Corticospinal Tract
|

- Starts in the frontal lobe - relevant cell bodies in layer 5 of the cerebral cortex project their axons to the spinal
- Many fibers forming the corticospinal tract end in the ventral horn of the spinal cord to interact with spinal motor neurons that will innervate muscle. |
|
|
Conventional (Native) X-Ray Imaging
|
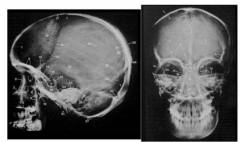
Native X-ray diagnostics indirectly show pathologies of the brain and spinal cord
|
|
|
Pneumoencephalography
|

a small amount of cerebrospinal fluid is drained and replaced with air. The air travels towards the cranium in an upright patient and will reduce the radiodensity of the ventricles.
|
|
|
Cerebral Angiography
|
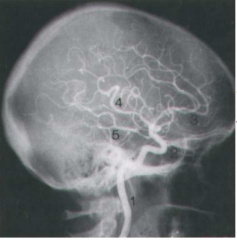
X-ray representation of blood vessels with contrast medium applied through a catheter.
|
|
|
Myelography
|
Contrast agent administered via lumbar puncture.
|
|
|
CT
|
- X-rays pass from a rotating source around the head (or
other body part), with unabsorbed X-rays reaching a rotating detector - After a rotation, the X-ray source and detectors are moved to a new plane, creating a new slice (tome). - CT can differentiate bone, white matter, gray matter and fresh blood - Infarctions and intracranial hemorrhages are readily detected by CT |
|
|
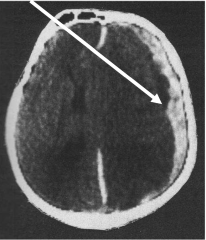
Epidural Hemorrhage
|
- Biconvex accumulation of blood
|
|
|
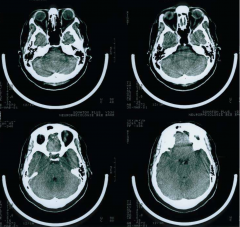
Subarachnoid Hemorrhage
|

Blood in the subarachnoid space
|
|
|
Subdural Hemorrhage
|
- Reflect trauma-induced tearing of the dura or tiny cerebral veins that traverse the dura
- Crescent shape |
|
|
MRI - T1
|
- Strong in fatty tissue
- CSF = dark - T1 MRI differentiates gray-white and shows detail - Infarctions are visible |
|
|
T1 MRI with Contrast
|

Paramagnetic gadolinium reveals perforations in the blood brain barrier, such as those surrounding tumors
|
|
|
T2 MRI
|
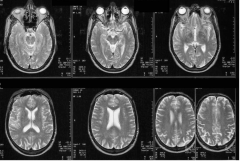
- CSF = bright white.
- Weak differentiation of white and gray. - Edema and neuropathology |
|
|
T2-weighted MRI
|
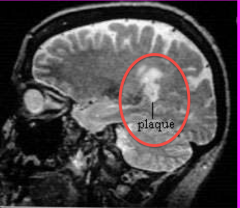
A specialized MRI scan called FLAIR may better reveal lesions from multiple sclerosis than a standard T2-weighted scan.
|
|
|
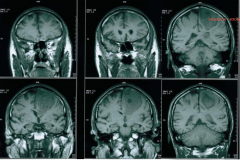
Comparison of T1, T1 w/Contrast and T2-Weighted
|
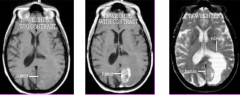
|
|
|
Positron Emission Tomography (PET)
|
- Evaluation of the distribution of radioactive isotopes by a computational method (like CT, MRI) to show metabolism (e.g., glucose) in the brain.
- Radiotracer (e.g., 18F-deoxyglucose -- short half-life) is taken up by the neurons like glucose but not metabolized accumulation (marker for glucose metabolism). |
|
|
Single Photon Emission Computerized Tomography (SPECT)
|
- Evaluation of the distribution of radioactive isotopes by a computation method (like CT, MRI) to show perfusion in the brain
- NOT metabolism - Injection of a radiotracer, for instance 99mTc or 123I. |
|
|
Spinal Cord
|
|
|
|
Lateral Surface of the Brain
|

|
|
|
Insula
|

|
|
|
Olfactory Cortex
|
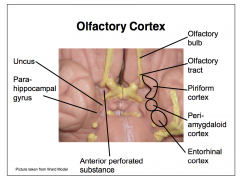
|
|
|
Fornix
|
|
|
|
Ventricular system
|
|
|
|
Epidural Hemorrhage
|
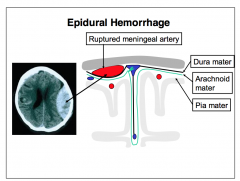
Epidural hemorrhages
commonly reflect the traumatically induced rupture of meningeal arteries (e.g., middle meningeal artery), with a fractured bone cutting the vessel. During the episode, blood forces the stiff periosteal dura to separate from the skull, yielding a characteristic biconvex mass adjacent to the fracture. Pressure arising from the accumulating blood compresses/distorts the brain. Dangers typically peak within hours of arterial involvement but may go unrecognized. |
|
|
Subdural Hemorrhage
|
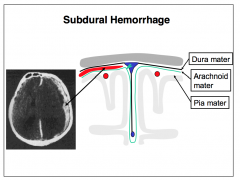
Subdural hemorrhages
commonly reflect trauma- induced ruptures of the delicate veins that traverse the meningeal layer of the dura from the subarachnoid space. Bleeds arising from tearing of the meningeal dura are also subdural. Because the pressure in the venous system is much lower than in the arterial system, crescent-shaped subdural masses of blood often develop slowly before manifestations arise (e.g., hours-to-weeks). |
|
|
Subarachnoid
Hemorrhage |
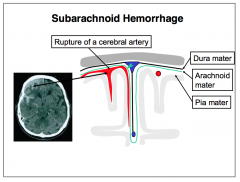
Many arteries reside between the arachnoid and pia mater (surrounded by CSF within the subarachnoid space). These vessels may rupture with trauma or spontaneously (in cases of aneurysm). The leaking blood assumes a tree-like appearance, while following the sulci.
|
|
|
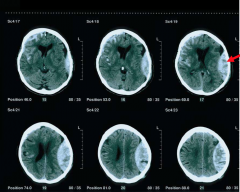
Intracerebral Hemorrhages
|
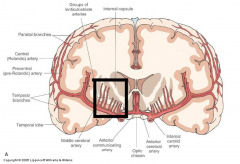
ntracerebral hemorrhages reflect rupture of intraparenchymal branches of subarachnoid arteries, such as the lenticulostriate arteries (indicated by black box), which branch from the middle cerebral artery, supplying the internal capsule and basal ganglia.
|
|
|
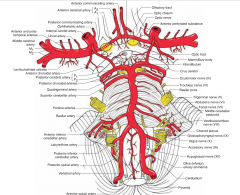
Internal Carotid
|
The internal carotid arteries ascend through the deep neck, the carotid canals of the petrous bones, and the cavernous sinus. They emit the ophthalmic and posterior communicating arteries. They divide, terminating as the anterior and middle cerebral arteries
|
|
|
Vertebral arteries
|
- 1st branches of the subclavian arteries
- Ascend through the transverse foramina of the upper 6 cervical vertebrae and enter the skull through the foramen magnum - Emit the posterior inferior cerebellar arteries (PICA), which usually spawn the posterior spinal arteries - The vertebral arteries then emit the anterior spinal artery before unifying to form the basilar artery |
|
|
Basilar Artery
|
- Gives rise to the anterior inferior cerebellar arteries (AICA).
- The superior cerebellar arteries arise from the basilar artery, just before to its bifurcation |
|
|
Anterior and middle cerebral arteries
|
Anterior and middle cerebral arteries are the terminal divisions of the internal carotid artery - reach ventral surface of brain just lateral to the optic chiasm
|
|
|
Inferior View of Vessels
|
|
|
|
Middle Cerebral
|
- Middle cerebral artery extends laterally in lateral fissure over the insula, sending branches to the lateral aspect of frontal, temporal, and parietal lobes
- Emits lenticulostriate arteries - basal ganglia and the internal capsule - These arteries are particularly vulnerable to rupture and are a major source of intracerebral (periventricular) hemorrhage. |
|
|
Blood Supply - Lateral View
|
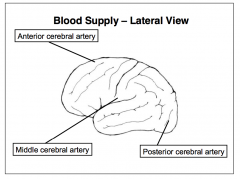
- e.g. Occlusion of the left middle cerebral artery often yields language deficits, as this artery normally supplies cortical regions subserving verbal and literal elements of speech
|
|
|
Arterial Supply of the Spinal Cord
|
Two posterior spinal arteries supply the dorsal and lateral aspect of the spinal cord, and one anterior spinal artery supplies the ventral cord
|
|
|
Epidural anesthesia
|
olutions of anesthetics can be injected into the epidural space where they cause conduction block of adjacent spinal nerves.
|
|
|
Epidural (extradural) hemorrhage:
|
- Results from trauma to the side of the head where the skull is relatively thin and vulnerable to fracture
- Damage to the underlying vessel, the middle meningeal artery, causes the dura mater to separate from the inner aspect of the bone |
|
|
Aneurysm
|
- Local dilation of the wall of an artery
- The majority occur near branches of vessels (mostly the internal carotid artery or its branches). |
|
|
Third Ventricle
|
- Thin vertical cavity, occupying the midline between the diencephalic hemispheres
- Roof = choroid plexus and the body of the fornix - Lateral walls = thalami, hypothalami, and subthalami - Basal hypothalamic structures = floor - Lamina terminalis and anterior commissure = anterior wall - Epithalamus = posterior wall |
|
|
4th Ventricle
|
It is connected to the third ventricle by the mesencephalic cerebral aqueduct, which is frequently involved in obstructive hydrocephalus.
|
|
|
Choroid Plexus
|
- Rich network of blood vessels of the pia mater that projects into each ventricle to form a semi-permeable filter between arterial blood and the CSF
- Layer of ependyma covers the plexus and lines the ventricles - Stretches within the lateral ventricles from the temporal horn through the interventricular foramen into roof of the third ventricle |
|
|
CSF
|
- Clear and low in glucose, protein, K+, Ca++ and cells relative to serum.
– CSF is high in Na+, Cl- , and Mg++ relative to serum - 140mL = normal |
|
|
Circulation of CSF
|
1. Lateral ventricles - 3rd ventricle via interventricular foramina (of Monro)
2. 3rd ventricle - cerebral aqueduct 3. Cerebral aqueduct - 4th ventricle 4. Small amounts of CSF trickle between the fourth ventricle and the central canal 5. Exits 4th ventricle into the subarachnoid space via the foramina of Luschka (lateral) and Magendie (medial) - Extraventricular CSF follows the subarachnoid space. |
|
|
Reabsorption of CSF
|
- Returns to the venous system through small membranous villi, the arachnoid granulations, located along the superior sagittal sinus
- Arachnoid villi react to pressure gradients between the subarachnoid space and venous system to form one- way valves, ensuring the unidirectional movement |
|
|
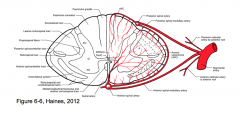
Sinuses
|
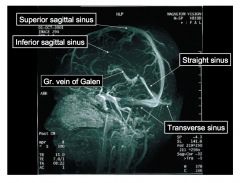
|

