![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What type of degeneration entails these features?
-occurs after severe nerve injury? -basement membrane of the nerve is still intact, but the axon itself becomes dysfunctional in both directions (distal and proximal), but more distally |
Wallerian Degeneration
|
|
|
|
_____________is when the muscle fibers are not lined up longitudinal and symmetrical to each other. Instead, they may turn on end and line up in all different directions relative to each other (similar to dropping toothpicks or playing with pick-up sticks)
|
Mechanical Dearangement
|
|
|
|
What diagnostic exam done on muscle shows the following:
1.Fibrillation potentials 2.Positive sharp waves 3.Fasciculations 4.Fiber type conferred by re-innervating neuron-->fiber type grouping occurs and motor unit size increases with the configuration changes. |
EMG
|
|
|
|
-Attacks anterior horn cells
-Presents as mild viral infection (pharyngitis or gastroenteritis) |

Polio
|
|
|
|
Clinical Presentation:
-LMN injury -Muscle atrophy & fasiculations -Loss of reflexes -Gait abnormality -Bulbar (brainstem) & respiratory paralysis |

Polio
|
|
|
|
-UMN & LMN disorder
-Affects anterior horn cells and corticospinal tract -most common motor disease |

ALS
|
Amyotrophic means loss of muscle and sclerosis means whitening which is seen on the lateral tract
|
|
|
What is the difference between the lesions involved in Polio and the lesions involved in ALS?
|
Polio: involves a LMN lesion
ALS: involves both a UMN and LMN lesion |
|
|
|
Symptoms:
1.weakness 2.neck extensor weakness 3.early fatigue 4.atrophy 5.diaphragm often affected so breathing/speech difficulty 6.swallowing difficulty 7.HYPERreflexia 8.Fasiculations 9.No plateau of symptoms 10.No reversal of symptoms 11.NO SENSORY LOSS, BOWEL/BLADDER SYMPTOMS, EXTRA-OCULAR MUSCLE INVOLVEMENT, OR DEMENTIA. Dementia may coexist with the disease, but is not caused by the disease. |

ALS
|
|
|
|
10% familial-autosomal dominant
-on the long arm of chromosome 21 -causes a mutation in the synthesis of Cu/Zn superoxide dismutase -cell death may be from free radical formation |

ALS
|
|
|
|
Legs lay externally rotated with a lack of muscle tone and movement in babies.
|
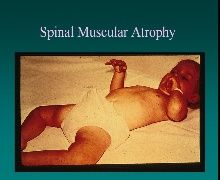
Floppy Baby Sydrome
|
|
|
|
-Sudden Onset
-Widespread peripheral NS disease -Autoimmune mediated with antibodies to myelin, and results in segmental demyelination of nerves, axonal injury, denervation, atrophy, axonal regeneration, and remyelination |

Guillian-Barre Syndrome (Acute Inflammatory Demyelinating Polyneuropathy)
|
|
|
|
-A patient has a recent history of viral illness, and is now having weakness in the distal limbs that is noted due to tendency to drop things, difficulty running, possible sensory loss, as well as some autonomic dysfunction. His motor symptoms are more severe than his sensory symptoms. Also, the patient is having weakness in the extraocular and bulbar distribution. The patient is currently in the ICU. The attending you are working with is worried that his respiratory muscles could be impaired next. What disease does this patient have?
|

Guillian-Barre Syndrome
|
|
|
|
With what illness does 90% of maximal paralysis occur within 4 weeks?
|

Guillian-Barre Syndrome
|
|
|
|
-Increased levels of protein, and decreased levels of cells=Albuminocytological Dissociation
-(Note: This is the opposite result of an infection) |

You do a spinal tap of a patient with Guillian-Barre Syndrome. What does the CSF show?
|
|
|
|
This disease is characterized by a chronic demyelination and remyelination, with periods of remission.
-It affect not only the peripheral nerves, but the nerve roots at the cervical spinal level. -This version is more symmetrical in terms of its sensory and motor tendencies. It can look like ALS. |

Guillian-Barre Syndrome (CHRONIC INFLAMMATORY DEMYELINATING POLYRADICULOPATHY (CIDP))
|
|
|
|
-Neuropathy associated with prolonged hospitalization
-Generally characterized by motor weakness with the cranial nerves are spared -Nerve conduction studies will NOT show significant slowing |

Critical Illness Polyneuropathy
|
|
|
|
-Virus will hang out in the DRG until there is suppression of the immune system, or increased stress, at which time the virus will reactivate and cause a skin rash along the associated dermatome.
|

Varicella-Zoster Virus Infection (Shingles)
|
|
|
|
-progessive nerve injury, muscle wasting in lower extremities
-process includes segmental demyelination, remyelination, and connective tissue proliferation, proliferation of the nerve -pts. have "Champaign Bottle" legs (distal legs are thin, thighs are normal in size) -severe weakness in plantarflexion & dorsiflexion -Hammer toe is common with this disease |

Charcot Marie Tooth (HMSN 1)
|
|
|
|
-Chromosome 17 gene duplication.
-Autosomal dominant |

Charcot Marie Tooth (HMSN 1)
|
Think of hammer toed kids with hammer toed parents!!
|
|
|
-most common cause of peripheral neuropathy
-microangiopathy & focal atherosclerosis |

Diabetic Neuropathy
|
|
|
|
-Nutritional impairment of nerves characterized by an accumulation of sorbitol, and a depletion of myo-insitol, both of which result in ischemia or infarction of nerves.
-Also, mononeuropathies of CN3 and CN6, affecting the eye. |

Diabetic Neuropathy
|
|
|
|
-Neuropathies are typically symmetrical
-Sensory is usually lost first, and usually in the feet first -Pts. present with low back pain since the dorsal roots of the lumbar spine can be injured. |

Diabetic Neuropathy
|
|
|
|
Dorsal Column is involved in a condition known as Psuedotabes-->a wide and somewhat ataxic gait dysfunction.
|

Diabetic Neuropathy
|
|
|
|
-One of the most toxic causes of neuropathy.
-Causes severe anemia, due to the binding of sulfhydryl groups in enzymes, which decreases the incorporation of heme into RBCs. This causes a decrease in survival of the RBC, and thus anemia. -Causes segmental demyelination of nerves leading to wrist or foot drop. -Nerve conduction studies will show very slowed conduction velocity. |

Lead Poisoning
|
|
|
|
-A nutritional neuropathy.
-Presents as distal sensorimotor axonal neuropathy, characterized as a wide based gate with aching calves and pain in the legs and feet. Other symptoms include fragile skin and muscle tenderness. |

B1 thiamine deficiency: alcholic polyneuropathy
|
Prognosis is good if alcohol is eliminated.
|
|
|
-Unilateral hearing loss
-It is visualized as a well circumscribed tumor that is attached to the nerve and is highly vascularized. -Tx is surgical |
Schwannoma: Usually affects the 8th cranial nerve at the cerebello pontine angle.
|
|
|
|
-more sensory than motor and begin in the lower extremities.
-deposition of abnormal proteins and elevated circulation of polyclonal IgG antibodies are a couple of key identifiers of this disorder. |
Paraneoplastic Disorders
|
|
|
|
What are the 3 hereditary non-inflammatory muscular diseases?
|
Duchenne's, Becker's, and Myotonic
|
|
|
|
-Caused by a chromosome depletion for dystrophin, which normally provides scaffolding for muscle cells
-X-linked recessive disorder, results of spontaneous mutations -Loss of stabilization for actin and membrane proteins. This basically disables the muscle's ability to contract. -Affects skeletal and cardiac muscle. |

Duchenne's Muscular Dystrophy
|
|
|
|
-Elevated levels of creatine kinase and aldolase will be seen-->these are muscle cell substrates that are not used b/c the muscle doesn't contract.
-Other symptoms include motor and gait problems, contractures, cognitive problems, decreased pulmonary function (due to respiratory muscle weakness), while the ocular muscles remain intact. |

Duchenne's Muscular Dystrophy
|
|
|
|
-The microscopic observance of the lack of dystrophin is the defnitive characteristic of this disorder!
-Without dystrophin there is a loss of structure, and muscle cells fall completely apart. There is a great deal of fibrosis between cells, and the borders of cells are obscured. |

Duchenne's Muscular Dystrophy
|
|
|
|
-Muscle in children with this disorder often feel hardened and rope-like.
-This disorder causes proximal weakness and children use gower's maneuver to get up off the floor. |

Duchenne's Muscular Dystrophy
|
|
|
|
1.In what type of dystrophy is dystrophin absent?
2.In what type of dystrophy is dystrophin present but abnormal? |
1.Duchenne's
2.Becker's |
|
|
|
-This is a much miler form of dystrophy where dystrophin is abnormal, but NOT absent.
|
Becker's X-linked Muscular Dystrophy
|
|
|
|
-Attacks the muscles of the face and results in a long drawn out face due to weakness. Other symptoms are frontal balding and cataracts.
-Microscopically you will see "ring fibers" which is a tissue disruption in the muscle cell that goes along with this disorder. |
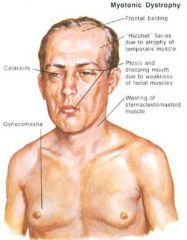
Myotonic Disorder
|
|
|
|
An immune mediated disease in which antibodies bind to ACh receptors and therefor block the binding of ACh.
|
Myasthenia Gravis
|
|
|
|
Binds to snare proteins and prevents the release of ACh from the nerve terminal.
|
Botulinum Toxin
|
|
|
|
A 50 y/o man developed double vision and drooping eyelids. His symptoms were worse at the end of the day. He had some difficulty chewing. What disease does he have?
|
Myasthenia Gravis
|
|
|
|
-Limited to skeletal muscle
-Usually begins in ocular and pharyngeal muscles. -75% of these patients have a thymic hyperplasia which is sometimes treated by removing the thymus. |
Myasthenia Gravis
|
|
|
|
-Diagnosis of this disorder is made with Endrophonium.
-Tx for this disorder involves ACE Inhibitor, immunosuppression, and thymectomy. |
Myasthenia Gravis
|
|

