![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
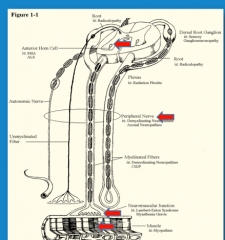
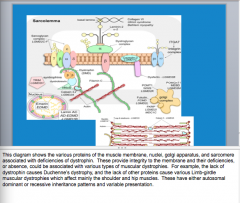
What type of diseases occur at each arrow? |
Top = anterior horn = motor neuron disease (motor axons and muscle fibers innervated by them affected) = spinal muscular atrophy and amyotrophic lateral sclerosis
Next to top = peripheral neuropathies = motor axons + nerves that carry pain, proprioceptive sensations, autonomic fibers => autonomic problems
Neuromuscular junction = disorders of neuromuscular transmission = myasthenia gravis
Muscle fiber = myopathies (muscular dystrophy) |
|

Left right
What is the most common symptom of neuromuscular disease? |
Left = Gower's sign Right = myopathy symmetric proximal muscle atrophy
Weakness |
|
|
What muscles are primarily affected in myopathic disease?
What is shown as a sign of proximal muscle atrophy? |
Proximal muscle => atrophy and weakness
Winged scapula (from previous card) |
|

What muscles are affected in polyneuropathies? What about sensation and reflexes?
What neuropathies affect individual nerves? |

|
|

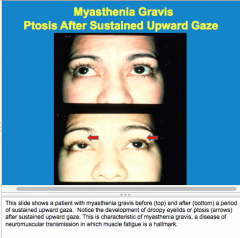
What is the sign? What is the disease? What type of disease? |
|
|
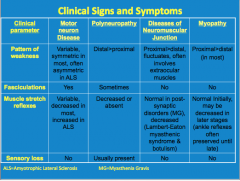
Review |
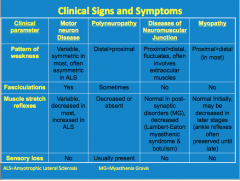
Review |
|
|
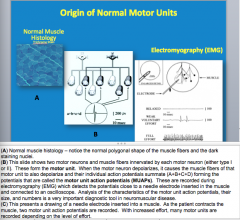
What forms the motor unit?
What are the motor unit action potentials?
|
|
|
|
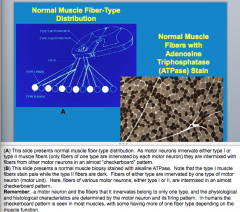
What are the two types of motor neurons and muscle fibers?
A motor neuron and the fibers that it innervates belong to only one type (true or false)? |
|
|
|
What happens to a muscle when it loses its innervation (by trauma to its axon)? |

|
|
|
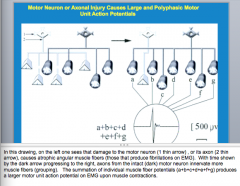
What happens when a particular type of axon becomes damaged? What is this called? Will the total number of action potentials be increased or decreased? Will the motor unit action potentials become larger or smaller? |

|
|
|

|
|
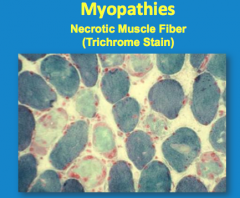
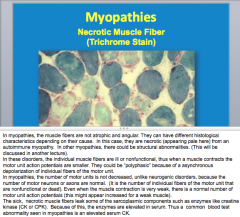
Are the muscle fibers atrophic and angular in myopathies? How do they appear here?
Is the number of motor units decreased in myopathies?
What do the dead fibers leak? |
|
|
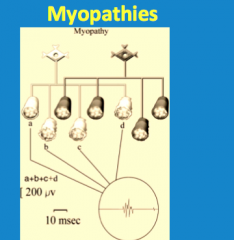
Comment on the state of the motor neurons and axons and the muscle fibers. |
Normal axon and neurons, sick muscle fibers => decreased motor unit action potential
Polyphasic because the damaged individual fibers fire asynchronously |
|
|
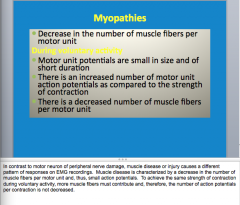
Myopathies:
_________ in the number of muscle fibers per motor unit.
During voluntary activity:
Motor unit potentials are _______ in size and of _____ duration. There is a(n) ________ number of motor unit action potentials as compare dot the strength of contraction. There is a _______ number of muscle fibers per motor unit. |
|
|
|
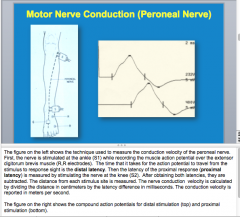
How are conduction velocities calculated? |
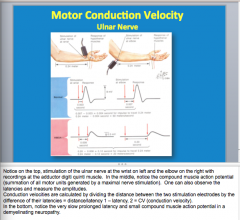
Dividing the distance between two stimulation electrodes by the difference of their latencies |
|
|

|
|
Look over |
Look over |
|
|
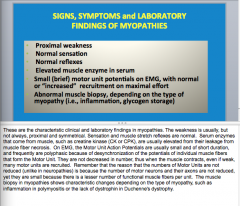
What are the sign, symptoms, and lab finding of myopathies? |
|
|
|
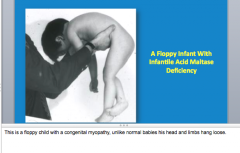
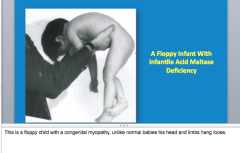
What are some examples of congenital myopathies? How are the babies described? |
|
|
|
What are some examples of muscular dystrophies? Are they hereditary and progressive? What are some caused by dysfunction of? |

|
|
|
How are myotonic dystrophies characterized? Are they also hereditary and progressive? What is difficulty of relaxing contracted muscle called? |
|
|
|
|
|
|
Lack of dystrophin causes what? Lack of other proteins cause various Limb-girdle muscular dystrophies which affect movement of what? |
|
|
What are these called? |
Muscular dystrophies |
|
|
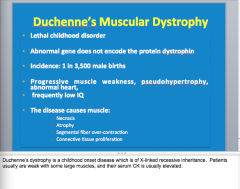
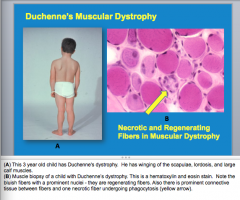
Duchenne's Muscular Dystrophy:
Lethal or not (age) How is muscle affected, heart and brain? What is the inheritance? What is elevated? |
|
|
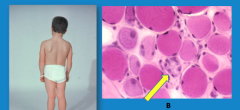
What three things do you see on the boy with muscular dystrophy?
What is the arrow pointing to? |
|
|
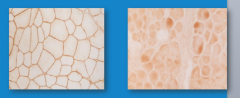
Left and right? |
Left = normal staining in muscle membrane
Right = abnormal muscle without dystrophin from a child with Duchenne's dystrophy |
|
|
What is the pathogenesis of muscle atrophy from lack of dystrophin? |

|
|
|
|
|
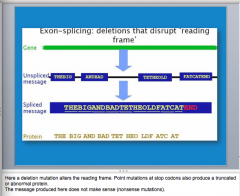
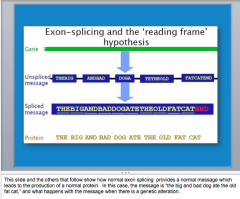
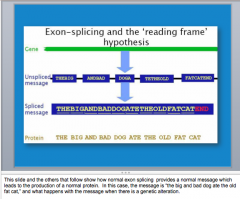
Nonsense mutation = altered reading frame |
|
|
|
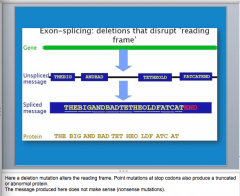
What is the effect of exon skipping? |
|
|
|
What is morpholino? Effect when it is injected into a dystrophic mouse muscle? |

|
|
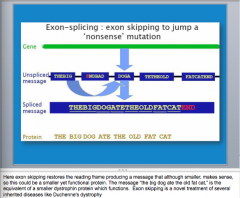
What are some differences between Becker and Duchenne muscular dystrophy? |
Age = older Disease = milder Lordosis and calf hypertrophy Muscle fibers still have protein (no dystrophin absence) |
|
|
What are myotonic dystrophies characterized by? What is the genetic defect?
What is the difference in proximal myotonic dystrophy? |
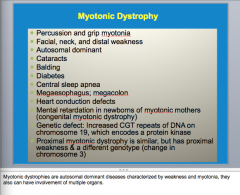
Weakness and myotonia |
|
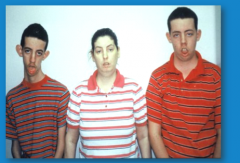
What is the disease? Why do the kids look worse? |
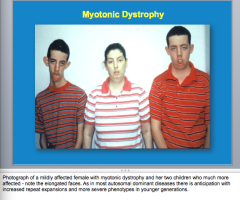
AD = increased repeat expansions |
|
|
Are inflammatory myopathies acquired? What are some causes? |
|
|
|
What are metabolic myopathies caused by? What are these often present with? |
Enzyme deficiencies that block metabolic pathways. |
|
|
What happens in McArdle's disease? |
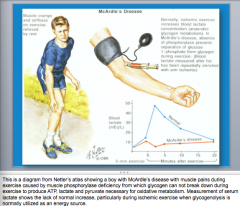
Pain during exercise from muscle phosphorylase deficiency => glycogen cannot break down during exercise to produce ATP, lactate, and pyruvate necessary for oxidative metabolism |
|
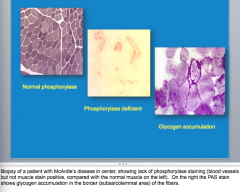
What is shown in the last two? What is the disease? |
|
|
|
What might patients develop in endocrine myopathies (think wimpy)? What findings are not specific?
What do hypoparathyroid patients present with? High levels of what? |
|
|
|
What are some toxins that can cause myopathies? |
|
|
|
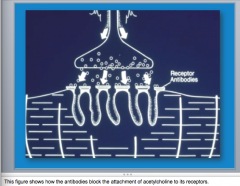
What are the components of neuromuscular transmission that can be affected by presynaptic or postsynaptic disorders? |
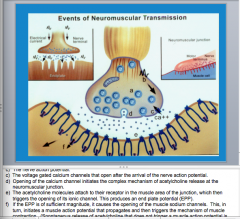
1. Acetylcholine vesicles in nerve terminal 2. Nerve action potential 3. Voltage gated calcium channels 4. Opening of calcium channel => acetylcholine release 5. Acetylcholine molecules attach to their receptor in the muscle area of the junction => triggers opening of ionic channel 6. EPP => open in of muscle sodium channels |
|
|
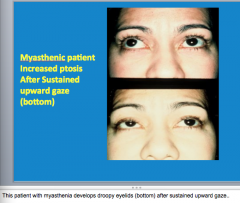
Is myasthenia gravis acquired? What is it characterized by? Is the patient typically weaker at the end of the day or the beginning of the day? |
|
|
|
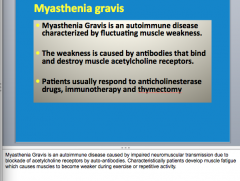
What type of disease is Myasthenia gravis? What is it caused by (antibodies that do what)?
What does it respond to (drugs and treatments)? |
|
|
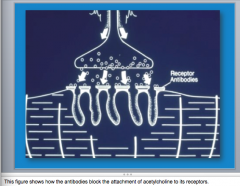
Antibodies block acetylcholine |
|
|

Disease? |
|
|
|
What is edrophonium or tensilon? |
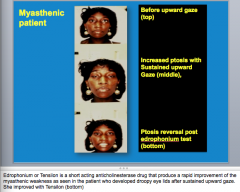
|
|
|
Which is myasthenia, myasthenic syndrome, normal? |
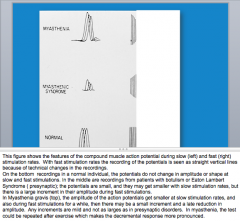
Normal does not change shape or amplitude
Top = get smaller at slow stimulation rates |
|
|
What are some treatments for myasthenia gravis? |
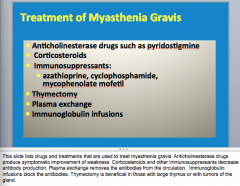
|
|
|
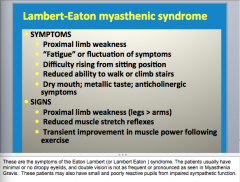
Signs/symptoms of Eaton Lambert Syndrome: |
Lung tumor Antibodies block RELEASE of acetylcholine (block presynaptic voltage gated calcium channels) Difficulty climbing stairs, decreased salivary production (nicotinic and muscarinic receptors affected)
Depressed reflexes of disease => may improve during a few repetitive taps |
|

|
|
|
|
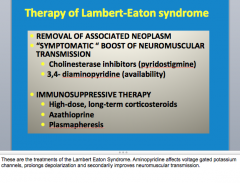
What are the treatments of Lambert-Eaton syndrome?
Remove something, drugs, immune system |
|

