![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
69 Cards in this Set
- Front
- Back
|
When does neurolation begin in embryogenesis? Explain the formation of the neuro tube.
|
Neurolation occurs in the 3rd week after gastrulation. The notochord induces the overlying ectoderm to form the neuroectoderm. The neuroectoderm forms the neuro plate which fold to form the neuro tube. Neuro crest cells form from neuroectoderm at the lateral lips outside neuro tube.
|
|
|
1) What is the result of the anterior neuropore failing to close?
2) What is the result of the caudal neuropore failing to close? |
1) Anencephaly - polyhydroamnious and increases AFP.
2) Spina bifida - normal levels of amniotic fluid with increased AFP. |
|
|
1) What does alar plate of the neural tube give rise to?
2) What does the basal plate of the neural tube give rise to? |
1) Sensory neuroblasts of the dorsal horn.
2) Motor neuroblasts of the bentral and lateral horns. |
|
|
What structures, aside from the neural tube, arise from the neuroectoderm?
|
Optic nerve and retina (only nerve to be affected by MS), pineal gland, neurohypophysis, glial cells (this does not include microglial - phagocytes)
|
|
|
What do neural crest cells form?
|
Ganglia in the PNS; sensory (primary sensory); ANS postganglionic; adrenal medulla; melanocytes; Schwann cells; pia and arachnoid mater; pharyngeal arch cartilage; odontoblasts; parafollicular cells; AP septum; endocardial cushions.
|
|
|
What are the primary and secondary vesicles of the neural tube?
|
Prosencephalon (*telencephalon - cerebral hemisphere, caudate, putamen, amygdaloiid claustrum, olfactory bulbs, hippocampus; *diencephalon - thalamus, hypothalamus, neurohypophysis, pineal gland, globus pallidus, optic chiasm, optic tract, optic nerve).
*Mesencephalon - midbrain. Rhombencephalon (*metencephalon - pons, cerebellum; *mylencephalon - medulla). |
|
|
Explain the pathology in the subtypes of spina bifida:
1) Occult 2) Meningocele 3) Meningomyelocele 4) Rachischisis |
1) Defect in vertebral arch - failed fusion of lamina - no spinous process. Normal AFP.
2) Vertebral defect - dura and arachnoid project through the vertebral defect; cysts with CSF. Elevated AFP; normal neurology. 3) Meninges and spinal cord project through the vertebral defect; elevated AFP. 4) Posterior neuropore fails to development during week 4. |
|
|
Explain the anatomy of the brain ventricles and how they communicate.
|
Lateral ventricles pass CSF to the 3rd ventricle via the foramen of Monro. The 3rd ventricle, found in the midline within the diencephalon, communicates with the 4th via the cerebral aqueduct (Sylvius). The 4th ventricle is located on the dorsal surface of the pons and ventral surface of the cerebellum. The fourth ventricle allows CSF to access the subarachnoid space via the Foramen of Luschka (2) and foramen of Magendie (median aperture).
|
|
|
Explain the following:
1) Hydrocephalus 2) Communicating hydrocephalus 3) Noncommunicating hydrocephalus |
1) Excess volume or pressure of CSF, producing ventricular dilation.
2) Oversecretion of CSF without obstruction in the ventricles or lack of absorption through the arachnoid granulations (Choroid papilloma, meningitis). 3) Obstruction at foramen Monro, Sylvian, or Luschka/Megendie. |
|
|
What is a nissel stain?
|
A nissel stain shows where rough endoplasmic reticulum is located, therefore it stains the gray matter of the spinal cord.
|
|
|
What cord segment is test by:
1) Knee reflex 2) Ankle 3) Biceps 4) Tricepts 5) Forearm |
1) L2-L4
2) S1 3) C5-C6 4) C7-C8 5) C5-C6 |
|
|
Outline the pathway of the lateral corticospinal tract.
|
Cortex (primary motor in the precentral gyrus) - posterior limb of internal capsule - crus cerebri (midbrain) - base of pons - pyramids (medulla) - pyramidal decussation (90%) - lateral corticospinal tract - ventral horn - synapse.
|
|
|
What are the sign and symptoms of an upper motor neuron and lower motor neuron lesion?
|
UMN : LMN
Spastic paralysis: flaccid paralysis Increased muscle : decreased muscle Babinksi+ : Babinski- Hyperreflexia : hyporeflexia Increased tone : fasiculations -> hypotonia Decreased speed of voluntary movement : loss of voluntary Disuse atrophy : atrophy Large area: small area Contralateral : ipsilateral |
|
|
Sensory pathways:
Describe the purpose and location of neuron cell bodies of the dorsal column. Describe the purpose and location of neuron cell bodies of the anterolateral (spinothalamic) system. |
Dorsal: discriminative touch, proprioception, vibration, pressure. 1st neuron cell body in DRG, 2nd in medulla (decussate), 3rd in thalamus.
Spinothalamic: pain/temp. 1st neuron cell body in DRG, 2nd in spinal cord (decussate), 3rd in thalamus. |
|
|
Describe the pathway of the dorsal column - medial lemniscal system.
|
Pacinian/Meissner/muscle spindles - 1st neuron transverses dorsal columns (fasiculus gracilis - lower limb; cuneatus - upper limb (T5 up)) - synapse on 2nd neurons in medulla - decussate in the medial lemniscus - synapse on the 3rd neurons in thalamus - synapse on postcentral gyrus in cortex.
|
|
|
What is the role of the spincerebellar pathway?
|
Convey proprioceptive information from skeletal muscle to the cerebellum. There are two pathways: dorsal and cuneo. Cell bodies of dorsal are found in Clarke's nucleus. Cell bodies of cuneo are found in cuneate nucleus.
|
|
|
What spinal cord tract is affected by Friedreich ataxia? What are the symptoms of this disease?
|
FA is usually inhertied as an AR disorder. The spinocerebellar tracts, dorsal columns, corticospinal tracts and cerebellum maybe involved. Ataxia is the initial symptom.
|
|
|
What column(s) is affected by:
1) Tabes dorsalis 2) Poliomyelitis 3) Amyotrophic lateral sclerosis 4) Anterior spinal artery occlusion |
1) Bilateral dorsal column signs below lesions. Paresthesia, pain, polyuria.
2) Lower motorneurons in the ventral horn - hyporeflexia and flaccid paralysis. 3) UMN (ventral horn) and LMN (corticospinal tract) 4) Corticospinal tracts (bilateral spastic paralysis) and spinothalamic tracts (bilateral pain/temp loss) |
|
|
If a patient has antibodies to intrinsic factor, what spinal cord tracts are affected?
|
Subacute combined degeneration has a vitamin B12 deficiency. Most often the dorsal columns and lateral corticospinal tracts lose myelin and result in bilateral spastic paresis and a bilateral alteration of touch, vibration, and pressure sensation below the lesion site.
|
|
|
What causes syringomyelia and what spinal cord tract is damaged?
|
This is caused by cavitation of the central canal, usually in the cervical spinal cord. This causes destruction of spinothalamic fibers (crossing over). when the cavitation expands, lower motor neurons in the ventral horns are compressed.
|
|
|
Brown-Sequard syndrome results from a hemisection of the cord resulting in a lesion of each of the three main neural systems: principle motor, dorsal, and spinothalamic. What are the hallmarks of these hemisections?
|
Lesions of corticospinal tract - ipsilateral spastic paresis.
Lesions of the dorsal column - ipsilateral loss of proprioception, two point discrimination, vibration. Lesions of the spinothalamic - contralateral loss of pain and temp. |
|

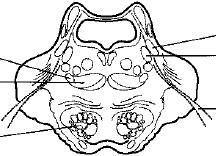
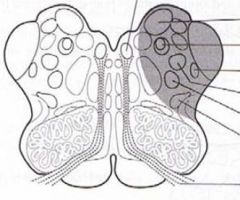
What level of the spinal cord is this?
|
Thoracic - because of the presence of the structure at F - lateral horn of the gray matter containing preganglionic sympathetic neurons.
|
|

What is the structure labeled g? And what cranial nerves arise from the structure?
|
G = pons.
Midbrain: III and IV Pons: V, VI, VII, VIII Medulla: IX, X, XII Spinal cord: XI |
|
|
What CNS structure lies directly above the superior colliculi (part of midbrain involved with visual reflexes)? A tumor of this structure results in Parinaud syndrome - paralysis of upward gaze and noncommunicating hydrocephalus.
|
Pineal gland.
|
|
|
What cranial nerve is injured when a patient has anosmia and CSF rhinorrhea?
|
Fracture to the cribiform plate causes CSF rhinorrhea and loss of function of the olfactory nerve (CN I).
|
|
|
What functions of the eye are controlled by CN III?
|
SR, IR, MR (adducting muscles), IO (elevation/abduction).
Constricts pupil - sphincter pupillae. Accomidation - ciliary muscle. Raise eyelid - levator palpebrae superioris. |
|
|
What cranial nerves are involved in movie the eye?
|
III - all other eye muscles (SR, MR, IR, IO)
IV - trochlear: superior oblique. VI - abducens - lateral rectus: abducts eyes. |
|
|
What are the sensory cranial nerves? Motor CNs? Mixed CNs?
|
Sensory: I, II, VIII (vestibulocochlear).
Motor: III, IV (trochlear), VI (abducens), XI (accessory), XII (hypoglossal). Mixed: V (trigeminal), VII (facial), IX (glossopharyngeal), X (vagus). |
|
|
What is unique about the trigeminal nerve?
|
Has three separate divisions: V1 (ophthalmic), V2 (maxillary), and V3 (mandibular).
|
|
|
What cranial nerve is damaged when a patient develops dry eyes?
|
Facial nerve (VII) which innervates the lacrimal gland. Additionally, salivary glands, (nasal and palatine glands.
Other symptoms: mouth droops, cannot use expressive muscles (ipsilateral), taste from anterior two thirds of tongue, and loss of blink reflex. |
|
|
What are corticobulbar axons? Why does severing a corticobulbar axon not lead to any paralysis? There is an exception, what is it?
|
UMN axons that innervate LMN of the cranial nerves. Bulb refers to brainstem. LMN of CNs are driven by both hemispheres; they have bilaterality. The exception: only the divisions of the facial nerves that wrinkle the forehead and shuts the eye are bilateral. Muscles around the nose/mouth innervated by the facial nerve are contralateral.
|
|
|
How do you test the integrity of the glossopharyngeal nerve?
What signs indicate damage to the facial nerve (X)? What signs indicate damage to the hypoglossal nerve (XII)? |
Sensory part of gag reflex.
Dysphagia, nasal speech, uvula deviates away from affected side. Horner's. Tongue deviates toward the lesion. |
|
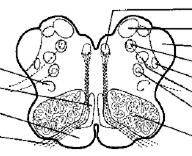
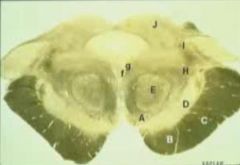
What section of brainstem is this?
|
Upper pons. The diagnostic feature is the large space which marks the 4th ventricle.
|
|
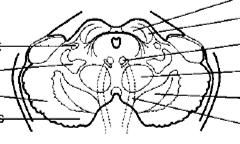
What section of the brainstem is this?
|
This is the upper medulla, which is apparent because of the olive (shaded region).
|
|
What are the diagnostic features of this section of brainstem?
|
This is the midbrain which contains the central canal and the two colliculi at the top.
|
|

This is the section of the brainstem. What is the structure at e?
|
This is a section of the lower medulla. E is the axons of corticospinal tract decussating. a = nucleus gracilis, b = nucleus cuneatus, c = spinal tract, d = spinothalamic tract
|
|

What cranial nerve is leaving at A?
|
This is a section of the midbrain. CN III leaves at point A.
B - corticobulbar axons. C - corticospinal tract. D - substantia nigra. E - red nucleus. |
|
|
Unilateral vestibular nerve or nucleus lesion may result in a vestibular nystagmus. Describe the slow and fast component of the nystagmus movements of the eye.
|
In a pathological vestibular nystagmus, the initial slow phase is the response to the pathology and the fast phase is the correction attempt made by the cortex in response to the pathology. If there is a left sided lesion: the right vestibular nuclei is unopposed and slowly moves the eyes to the left: the cortex corrects this by moving the eyes to the right fast. Note the fast component is away from the lesion.
|
|
|
How does the caloric test measure the integrity of the vestibulo-ocular reflex? (hint: cows).
|
Cool water introduced into the left external auditory meatus mimics a lesion on that side and the fast component will be away from the left. Warm is same side. Cold; opposite; warm; same.
|
|
|
A unilateral lesion to the descending hypothalamic fibers results in what condition?
|
Horner syndrome on the ipsilateral side.
|
|
|
The cortex projects to the PPRF (paramedian pontine reticular formation) which projects to the abducens nucleus. From the abducens nucleus, a nerve projects to the MLF (medial longitudinal fasciculus) and also the CN VI. The MLF projects to the occulomotor nucleus of the contralateral eye. If the right CN VI is cut, how will looking to the right be affected?
|
The right eye will not be able to abduct. The left eye will still be able to adduct.
|
|
|
What cerebral artery is used to supply:
1) Midbrain 2) Medial pons 3) Lateral pons 4) Medial medulla 5) Lateral medulla |
1) Posterior cerebral artery
2) Paramedian or pontine arteries 3) Anterior inferior cerebellar artery 4) Anterior spinal 5) Posterior inferior cerebellar artery |
|
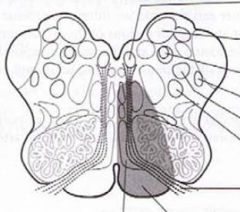
The shaded area has been infarcted. What will the symptoms be?
|
Its the medulla because of the olive area. Medial medullary syndrome (anterior spinal artery) : contralateral spastic hemiparasis (pyramidal), damage to CN XII (tongue protruding to affected side), contralateral loss of proprioception, touch, vibration (dorsal column).
|
|
Occlusion of the posterior inferior cerebellar artery leads to Wallenburg syndrome. Signs/symptoms?
|
Lateral medulla:
Contralateral loss of pain/temp (spinothalamic) and ipsilateral Horners (descending hypothalamic fibers - runs with spinothalamic). Loss of ipsilateral pain/temp to face (spinal V - trigeminal). Vertigo (CN VIII) - nystagmus away from lesion side. Ipsilateral paralysis of vocal cord, dysphagia, palate drop (CN IX and X). |
|
|
What cranial nerves are affected when the:
1) Paramedian (pontine arteries) are occluded 2) Anterior inferior cerebellar artery |
1) Medial pons - CN VI - results in internal strabismus (medial deviated eyeball due to failure to abduct).
2) VII - ipsilateral facial paralysis; VIII - hearing loss |
|
What nerve is affected in Weber syndrome (medial midbrain)?
|
Posterior cerebral artery has been occluded. CN III is the most commonly affected nerve: mydriasis (loss of parasympathetic axons out of Edinger-Westfal) , ptosis, lateral strabismus. Other areas affected: corticobulbar (contralateral lower face spastic hemiparesis), contralateral spastic hemiparesis of upper limb (corticospinal tract).
|
|
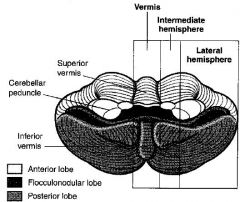
What are the function of the vermis, l. hemisphere, and flocculonodular lobe?
|
Vermis/intermediate zone - ongoing motor execution (input: spinal cord)
Hemisphere - planning (input: cortex) Flocculonodular lobe - balance and eye movement (input: CN VIII). |
|
|
What are the major afferent fibers of the cerebellum and where do they project?
|
Mossy fibers (vestibulo-, spino-, pontocerebellar tracts) enter ICP (peduncle) and MCP and excite granule cells.
Climbing fibers (olivocerebellar) enter ICP and excited Purkinje cells. |
|
|
What are the layers of the cerebellum and what are the major cells?
|
The three layers of the cerebellum are: molecular (axons of granule cells), Purkinje layer, and granule cell layer.
Cells: Purkinje, stellate, basket, golgi are all inhibitory (GABBA). Granule is excitatory (glutamate). Purkinje cell are the only axons that leave the cerebellar cortex. |
|
|
When patients have cerebellar lesions, what side of the body will the patient tend to fall towards?
|
Unilateral lesions of the cerebellum will result in a patient falling toward the side of the lesion. Why? Because the cerebullum crosses over to the contralateral side of the cortex and then the corticospinal fibers leaving the cortex cross back over at the level of the brainstem.
|
|
|
What is the hallmark of a cerebellum lesion? Also define:
1) Dysmetria 2) Dysdiadochokinesia 3) Scanning dysarthria |
Ipsilateral tremor when voluntary movements are performed - this occurs when there is a lesion in the hemisphere.
1) Past pointing - inability to stop at proper place. 2) Inability to perform alternating movements. 3) asynergy of the muscles responsible for speech results in patients dividing words into syllables. |
|
|
What is the result of a vermal lesion in the cerebellum? How does it differ from a lesion to the dorsal column?
|
Vermal lesions result in difficulty maintaining posture, gait, balance (ataxia gate). In dorsal column lesions, they will sway with their eyes closed (Rhomberg sign). In vermal lesions, patients sway with their eyes open.
|
|
|
What are the anterior vermis Purkinje cells particularly vulnerable to?
How are posterior vermis Purkinje cells commonly damaged? |
Thiamie deficiency that develops in alcoholics - gait ataxia.
Medulloblastomas or ependymomas - truncal ataxia. |
|
|
Besides intentional tremor, dysdiadochokinesia, dysmetria, and scanning dysarthria, what other signs/symptoms may occur in a cerebellum lesion.
|
Gaze dysfunction with nystagmus and the fast component toward the side of the lesion. Hypotonia with flabby muscles and reduced reflexes - this occurs in acute injuries to the deep cerebellar nuclei.
|
|
|
The thalamus serves as the major relay center for ascending tactile, visual, auditory information, and motor control from basal ganglia and cerebellum, as well as consciousness sates. What are the main groups of the thalamus?
|
Anterior nuclear group - part of limbic system.
Medial nuclear group - part of limbic. Ventral groups: motor nuclei (VA - globus pallidus, substantia nigra; VL - globus pallidus and dentate); sensory nuclei (VPL - somatosensory/nociceptive info; VPM - trigeminal pathway; medial geniculate nucleus - auditory; lateral geniculate nucleus - vision) |
|
|
What is thalamic pain syndrome? What part of the thalamus does it affect?
|
Posterior cerebral artery occlusion ( due to lacunar stroke) could lead to damage to the ventral nuclear group. Patients present with burning, aching pain in contralateral limbs of body. It is resistant to analgesic medications.
|
|
|
Where does neuronal degeneration take place in the hypothalamus in patients with thiamine deficiency? (Hint: only grossly identifiable feature of the hypothalamus).
|
Korsakoff: mammillary bodies - projects inferiorly from the hypothalamus just posterior to the infundibulum. Clinical features: anterograde and retrograde amnesia + confabulations.
|
|
|
1) What anatomical nuclei in the hypothalamus synthesize ADH and oxytocin?
2) What anatomical nuclei in the hypothalamus receives retinal input to help regulate the circadian rhythm? |
1) Paraventricular nucleus and supraoptic nucleus.
2) Suprachiasmatic nucleus. The output of this nucleus influences the pineal gland (produces melatonin). |
|
|
What anatomical nuclei is responsible for the release of hormones which enter capillaries in the hypophyseal-portal veins that act on the anterior pituitary?
|
The arcuate nucleus of the hypothalamus.
|
|
|
1) Which hypothalamic nuclei influence food intake?
2) What does the anterior and posterior hypothalamic zones control? |
1) Ventromedial nucleus - satiety center. Lateral hypothalamic zone - feeding center.
2) Anterior - responds to heat by dissipating it. Posterior - responds to cold. |
|
|
What gland is situated above the 4th ventricle and is part of the epithalamus? What is the role of this gland?
|
Pineal gland - synthesizes melatonin which plays the role in growth, development and circadian rhythms. Suprachiasmatic relays information to the pineal. Increased light decreases melatonin synthesis.
|
|
|
The basal ganglia initiate and provide gross control over skeletal muscle movements. What are the major components of the basal ganglia?
|
Striatum: caudate nucleus and the putamen.
External and internal segments of the globus pallidus. Substantia nigra. Subthalamic nucleus. |
|

What are the structures of the basal ganglia b, c, d?
|
a = anterior limb of internal capsule.
b = head of the caudate nucleus. c = putamen. d = globus pallidus. e = anterior commisure. f = optic chiasm. g = lateral ventricle. |
|

|
a = thalamus
b = caudate nucleus c and d = internal capsule g = putamen |
|
|
Basal ganglia: in the direct pathway, the cortex excites (via glutamate) the striatum which stimulate GABA neurons that inhibit the globus pallidus (i). Where does the GP(i) project to?
|
1) Normally the GP(i) tonically inhibits the thalamus. By inhibiting this inhibition the net effect of the direct pathway is to excite the neurons in the VA and VL of the thalamus. This is referred to as disinhibition.
|
|
|
Basal ganglia: in the indirect pathway, the cortex stimulates the striatum which inhibits the GP(e) with GABA. The GP(e) normally inhibits the subthalamic nucleus which stimulates the GP(i) with glutamate. Whats the net result?
|
The disinhibition allows the subthalamic nucleus to excite the GP(i) which acts to inhibit the thalamus (VL and VA regions). This is antagonistic to the direct pathway.
|
|
|
What is the role of the substantia nigra in the direct and indirect pathway?
|
The substantia nigra contains the cell bodies of dopaminergic neurons that project to the striatum. Dopamine stimulates the direct basal ganglia pathway via D1 and inhibits the indirect pathway via (D2).
|
|
|
Huntington's results in the degeneration of GABA neurons leading to chorea (dance like movements, mostly bilateral). Where in the basal ganglia does this degeneration often occur?
|
In the striatum at the head of the caudate nucleus
|
|
|
Pathology of what part of the basal ganglia leads to:
1) Hemiballismus 2) Parkinsonism 3) Huntington's 4) Athetosis |
1) Subthalamic nucleus
2) Substantia nigra 3) Striatum (in the caudate) 4) Striatum and thalamus |

