![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
323 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
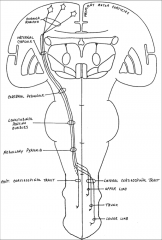
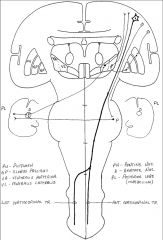
Posterior column-medial lemniscal pathway
|
Carries info about proprioception, vibration sense, and fine touch. Primary sensory neuron (dorsal root) --> ascends via ipsilateral white matter dorsal column --> synapse w/ dorsal column nuclei medulla --> secondary sensory neuron decussates --> synapse in the thalamus --> project to the primary somatosensory cortex in the postcentral gyrus
|
|
|
|
Anterolateral pathway
|
Carries info about pain, temperature sense, and crude touch. Primary sensory neuron (dorsal roots) --> synapse in gray matter of the spinal cord --> secondary sensory neuron decussates and ascends in anterolateral white matter (spinothalamic tract) --> synapse in thalamus --> project to the primary somatosensory cortex in the postcentral gyrus
|
|
|
|
Which sensory input does not pass through the thalamus?
|
Olfactory
|
|
|
|
Components of the diencephalon
|
Thalamus, hypothalamus, epithalamus
|
|
|
|
Monosynaptic stretch reflex
|
Reflex arc that begins with muscle spindles (sense stretch) --> transmission to sensory neurons --> dorsal root --> synapse in spinal gray matter with lower motor neurons (LMN's), causing contraction.
|
|
|
|
Deep tendon reflex
|
Muscle stretch reflex arc that begins with muscle spindles sensing stretch. Response can be routed via a monosynaptic stretch reflex (direct to LMN) and via interneurons (inhibitory). Tested clinically by tapping tendon with reflex hammer.
|
|
|
|
CN I
|
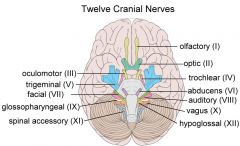
Olfactory nerve. Sensory.
Fxn: smell. |
|
|
|
CN II
|
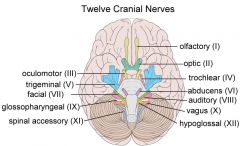
Optic nerve. Sensory.
Fxn: sight. |
|
|
|
CN III
|
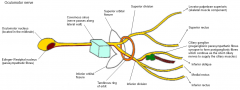
Oculomotor nerve. Motor.
Fxn: Eye movement (SR, IR, MR, IO), pupillary constriction (PS: E-W nucleus, muscarinic-R), accommodation, eyelid opening (levator palpebrae). |
|
|
|
CN IV
|
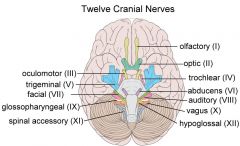
Trochlear nerve. Superior oblique muscle; causes the eye to move downward and to rotate inward (depression and intorsion)
|
|
|
|
CN V
|
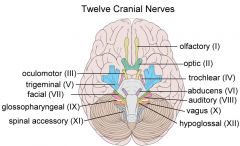
Trigeminal nerve. Sensations of touch, pain, temperature, vibration, and joint position for the face, mouth, nasal sinuses, and meninges; muscles of mastication; tensor tympani muscle.
|
|
|
|
CN VI
|
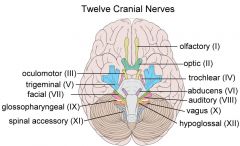
Abducens nerve. Lateral rectus muscle; causes abduction (outward movement) of the eye
|
|
|
|
CN VII
|
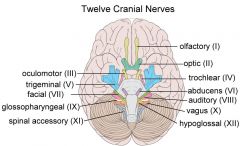
Facial nerve. Muscles of facial expression; also stapedius muscle and part of digastric; taste from anterior 2/3 of tongue; sensation from a region near the ear; parasympathetics causing lacrimation and supplying the submandibular and sublingual salivary glands
|
|
|
|
CN VIII
|
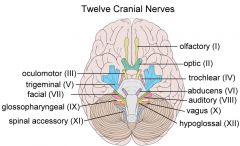
Vestibulocochlear nerve. Hearing; vestibular sensation.
|
|
|
|
CN XI
|
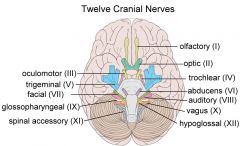
Glossopharyngeal nerve. Stylopharyngeus muscle; taste from posterior 1/3 of tongue; sensation from posterior pharynx, and from a region near the ear; chemo- and baroreceptors of the carotid body; parasympathetics to the parotid gland
|
|
|
|
CN X
|
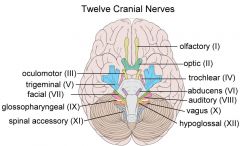
Vagus nerve. Pharyngeal muscles (swallowing); laryngeal muscles (voicebox); parasympathetics to the heart, lungs, and digestive tract up to the splenic flexure; taste from epiglottis and pharynx; sensation from the pharynx, posterior meninges, and a region near the ear; aortic arch chemo- and baroreceptors
|
|
|
|
CN XI
|
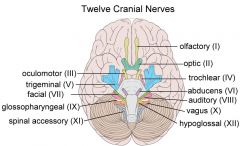
Spinal Accessory nerve. Sternomastoid muscle; upper part of the trapezius muscle.
|
|
|
|
CN XII
|
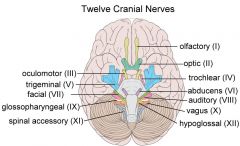
Hypoglossal nerve. Intrinsic muscles of the tongue.
|
|
|
|
From what does the CNS form?
|
Wall of the neural tube
|
|
|
|
Where does the ventricular system of the brain originate?
|
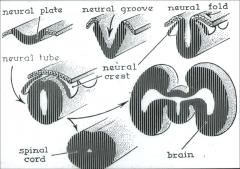
The lumen of the embryonic neural tube
|
|
|
|
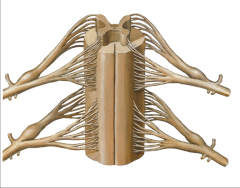
Dorsal/ventral roots vs dorsal/ventral rami
|
Roots are unimodal (they only carry information in one direction). Rami carry both afferent and efferent information.
|
|
|
|
Major types of neuron interconnections
|
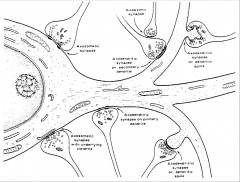
Axoaxonic, axosomatic, axodendritic
|
|
|
|
Embryologic origins of afferent cells, efferent cells, and association cells
|
Afferent cells (bipolar and pseudounipolar) derive from neural crest cells. Efferent cells (multipolar) come from basal lamina. Association cells come from alar lamina.
|
|
|
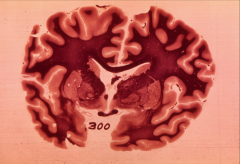
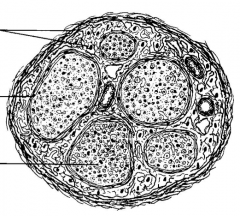
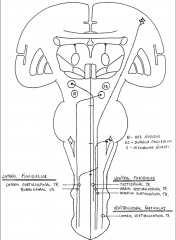
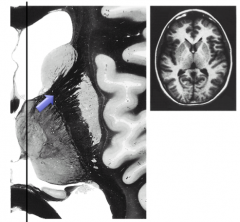
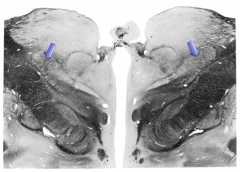
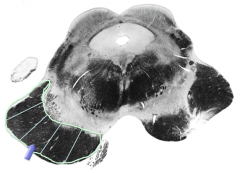
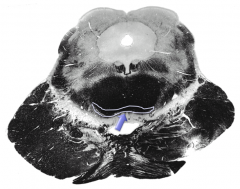
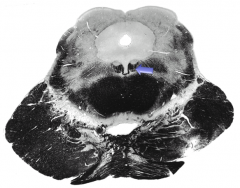
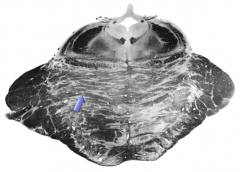
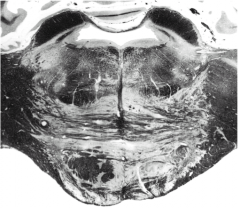
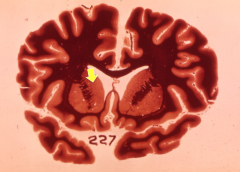
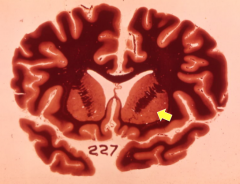
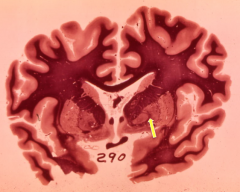
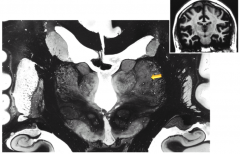
What kind of image is this?
|
Myelin stained cross section.
|
|
|
|
Describe the 3 primary brain vesicles and the 5 secondary brain vesicles.
|

|
|
|
|
Oligodendrocytes
|
Glial cells that provide myelination to neurons in the CNS
|
|
|
|
Nissl body
|
Granules of RER with ribosomes attached that are located in neurons
|
|
|
|
What kinds of things move by orthograde transport?
|
Neurotransmitters, AA's, and membrane proteins. They travel via kinesin motor proteins.
|
|
|
|
What kinds of things move by retrograde transport?
|
Trophic factors/growth factors, viruses
|
|
|
|
Axon hillock
|
Junction between the cell body and the axon. Typically not covered by myelin or oligodendrocytes. More susceptible to changes in local ion concentrations. Site of departure of an action potential.
|
|
|
|
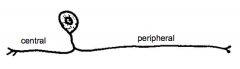
How do you name the arms of pseudounipolar and bipolar neurons?
|
Peripheral and central processes.
|
|
|
|
Myelinated vs unmyelinated (structurally)?
|
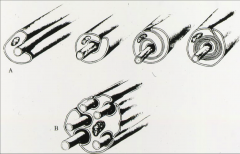
B. Unmyelinated axons are just "invaginations" into the Schwann cells (note they are not within the cytoplasm). i.e Remak Bundles
|
|
|
|
Astrocyte functions
|
Circumscribe the CNS (glia-pia membrane), induce blood brain barrier, buffer K+, regulated glutamate and glycogen in the brain, guide neurons during development, react to injury
|
|
|
|
How do astrocytes buffer potassium?
|
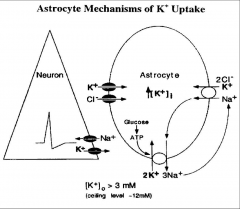
Astrocytes have many K+ channels and pick up the K+ ions that neurons release. There is also intra-astrocytic movement of K+ down its concentration gradient.
|
Bonus: when glial cells get sick and die, neurons can't survive.
|
|
|
How do astrocytes regulate glutamate?
|
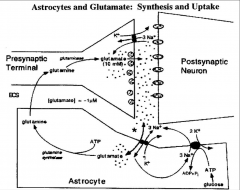
Glutamatergic neurons release glutamate into the synaptic space. The glutamate is picked up by astrocytes, converted to glutamine, and given back to the presynaptic bouton.
|
|
|
|
Excitotoxicity
|
Path. by which neurons are damaged by excessive stimulation by NT's, e.g. glutamate.
|
|
|
|
How do astrocytes regulate glucose?
|
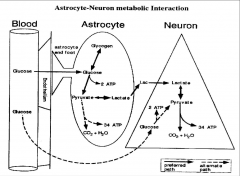
Most transfer of glucose from blood to CNS happens through astrocytes (they virtually envelop all of endothelial cells).
|
|
|
|
Two types of astrocytes
|
Protoplasmic astrocytes --> grey matter, more numerous.
Fibrous astrocytes --> white matter. |
|
|
|
Two types of oligodendrocytes
|
Fascicular --> white matter
Perineuronal --> grey matter |
|
|
|
Internodal segment
|
A segment of myelinated axon between 2 nodes of Ranvier
|
|
|
|
How do oligodendrocytes and Schwann cells differ in the number of internodal segments they can make?
|
ODC's can make an internodal segment on many different axons in the CNS, but SC's can only wrap one axon (1 internodal segment) in the PNS
|
|
|
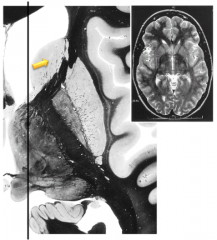
What is the dark purple material?
|
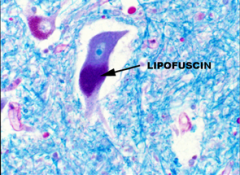
Lipofuscin granules are lipid-filled waste products that can collect around neurons (as well as other cell types).
|
|
|
What is this?
|
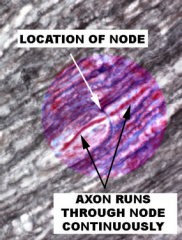
Longitudinal view of nerve, with two internodal segments shown with a node of Ranvier between them.
|
|
|
|
From which pharyngeal arches does the viscerocranium develop?
|
1st and 2nd
|
|
|
|
What are the nerve supplies to the pharyngeal arches?
|
1st = trigeminal (V), 2nd = facial (VII), 3rd = glossopharyngeal (IX), 4-6th = vagus (X).
|
Mnemonic: when you eat something bad, you 1) chew 2) make a face 3) swallow
|
|
|
What are the 5 prominences that come together to form the nose?
|
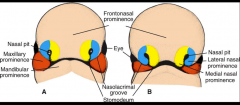
Frontonasal prominence, lateral nasal prominence, medial nasal prominence, maxillary prominence, mandibular prominence
|
|
|
|
What are the skeletal derivatives of pharyngeal arch 1?
|
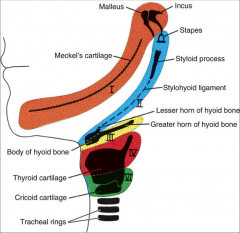
Meckel's cartilage, malleus, incus
|
|
|
|
What are the skeletal derivatives of pharyngeal arch 2?
|
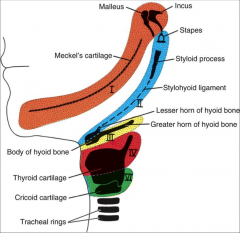
Lesser horn of hyoid bone, styloid process, stapes
|
|
|
|
At what level in the brain does the directional naming convention change?
|
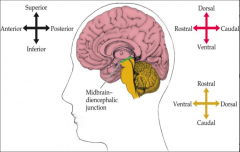
Between the diencephalon and the midbrain.
|
|
|
|
The lumen of the primitive mesencephalon becomes what adult structure?
|
Cerebral aqueduct
|
|
|
|
Where does the cervical flexure occur in the primitive brain?
|

Between the caudal end of the myelencephalon and the rostral end of the spinal cord
|
|
|
|
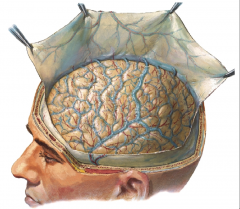
Name the layers of tissue that one would have to pass through to reach the arachnoid mater superiorly.
|
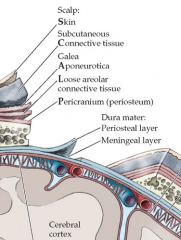
SCALP + calvarium + dura mater
|
|
|
|
Where does the middle meningeal artery enter the skull? Where does it travel? What does it supply?
|
Enters through the foramen spinosum; runs in the epidural space; supplies the dura mater.
|
|
|
|
Which arteries make up the circle of Willis?
|
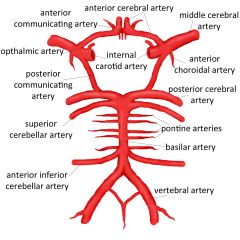
Anterior cerebral aa, anterior communicating, internal jugular aa, posterior communicating aa, posterior cerebral aa
|
|
|
|
The dura mater is "glued" to the skull by what?
|
Sharpey's fibers
|
|
|
|
What is the most vulnerable part of the calvarium to fracture?
|
Pterion - very thin, and also at risk for damaging the meningeal artery
|
|
|
|
What part of the dura dissects due to injection of fluid or subdural hematoma?
|
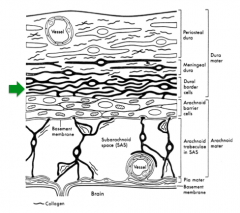
The deep layer of the meningeal dura because it has fibroblasts but not collagen. The more superficial layers of the dura have collagen and are very difficult to dissect.
|
|
|
|
What is the tentorial notch?
|
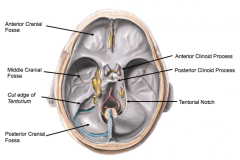
Also called the tentorial incisura, it is the opening between the right and left leaves of the tentorium cerebelli. The hindbrain passes through it. With increased ICP, structures may herniate through it, e.g. uncal herniation.
|
|
|
|
Where are cerebral veins located?
|
Subarachnoid space
|
|
|
|
What cell-cell contact is made between the menginges and brain parenchyma?
|
Pia mater - to - glial cell contacts. Pia mater does not contact neurons.
|
|
|
|
What are the two layers of the pia mater?
|
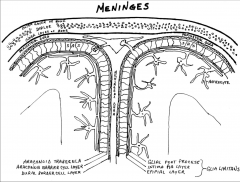
Epipia layer - collagen and fibroblasts.
Intima pia layer - reticular and elastic, in contact with glia |
|
|
|
Meningiomas are tumors of what layers of the meninges?
|
Leptomeninges
|
|
|
|
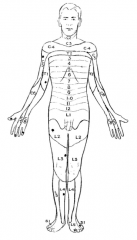
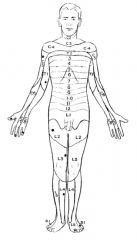
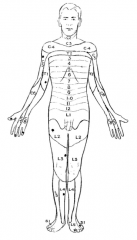
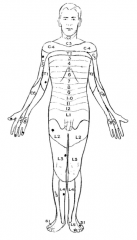
What is a dermatome?
|
A peripheral region innervated by sensory nerve fibers from a single nerve root.
|
|
|
|
Which of the two systems of ascending tracts is more primitive and of lower velocity?
|
The anterolateral system, which transmits pain, temperature, and crude touch.
|
|
|
|
GSE
|
General somatic efferent. Cells that give rise to axons that innervate striated muscles.
|
|
|
|
GVE
|
General visceral efferent. Autonomic neurons that synapse with a postganglionic cell which eventually innervate smooth muscle and glands.
|
|
|
|
SVE
|
Special visceral efferent. Cells that give rises to axons that innervate structures of the branchial arches, e.g. facial muscles, mastication, pharyngeal muscle. These cells are only found in the brainstem.
|
|
|
|
What are the two types of cells located in the dorsal root?
|
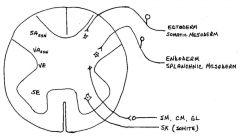
Somatic afferents (from ectoderm and somatic mesoderm derived cells) and visceral afferents (from endoderm and splanchnic mesoderm derived cells).
|
|
|
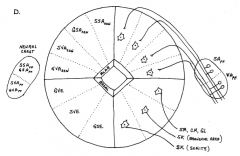
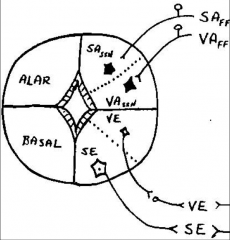
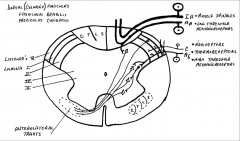
What is shown here (conceptually)?
|
These are the columns of cells in the CNS that are derived from neural crest, alar lamina, and basal lamina. The basal lamina has 3 sub groups: GSE, GVE, and SVE. The alar lamina has 4 sub groups: general/visceral, somatic/special afferent association cells. Not all cell columns are present at each level of the spinal cord/brain stem.
|
|
|
|
Dendritic spread
|
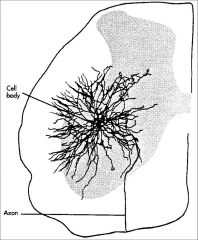
The area where one nerve can communicate/synapse with another nerve is not just localized to the soma (axosomatic). It can be anywhere throughout the postsynaptic nerve's dendritic spread which may branch extensively throughout gray matter and even some white matter.
|
|
|
|
Divergence
|
The functional idea that a neuronal axon can branch and synapse with multiple cells.
|
|
|
|
Convergence
|
The functional idea that one neuron can receive synapses from multiple difference neuronal axons.
|
|
|
Name the CT coverings of a nerve fiber and brief function.
|
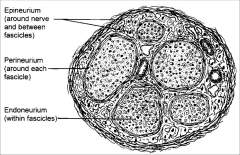
Endoneurium gives substance to surrounding nerve axons and capillaries. Perineurium sequesters groups of axons, is water tight, and forms the "blood-nerve barrier". Epineurium acts a protective layer around the nerve.
|
|
|
|
What is the conduction speed of alpha motor neuron?
|
70-120 m/s
|
|
|
|
Shoulder abduction
|
*C5, C6 via the axillary neve
|
|
|
|
Elbow flexion
|
C5, *C6 via the musculocutaneous nerve
|
|
|
|
Elbow extension
|
C6, *C7 via the radial nerve
|
|
|
|
Wrist extension
|
*C6, C7 via the radial nerve
|
|
|
|
Wrist flexion
|
*C7, C8 via the median nerve
|
|
|
|
Finger extension
|
*C7, C8 via the radial nerve
|
|
|
|
Finger flexion
|
C8, T1 via the median/ulnar nerves
|
|
|
|
Finger abduction
|
*T1 via the ulnar nerve
|
|
|
|
What are the two fiber bundles of the posterior columns, and from which regions of body do the nerves inside them come?
|
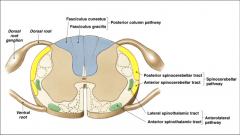
Gracile fasciculus - sacral to T6.
Cuneate fasciculus - T6 up and cervical. The lower extremity is represented medially (gracile) and the upper extremity is represented laterally (cuneate) within the posterior columns. |
|
|
|
Monoamines
|
E.g. dopamine, NE, serotonin. NT's with an amino group and aromatic group--derived from aromatic amino acids.
|
|
|
|
MAO
|
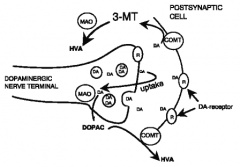
Monoamine oxidase enzyme degrades monoamine NT's (DA, NE, S).
|
|
|
|
COMT
|
Catechol-O-methyl transferase enzymes degrades catecholamine NT's (NE, DA).
|
|
|
|
AChE
|
Acetylcholinesterase enzyme degrades acetylcholine.
|
|
|
|
Benzodiazepines
|
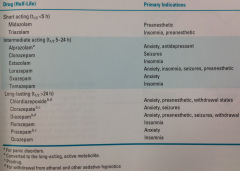
Sedative-hypnotic drug that binds to BZ receptor (part of GABA-A receptor). MOA: Increases GABA affinity and freq. of GABA-stimulated chloride channel opening. Leads to hyperpolarization. Rx orally for anxiety (short-term) and traditionally sleep disorders. Also, Rx for seizures, withdrawal states. Incr. lipid solublity, more rapid onset. Cleared by hepatic metab. SE: daytime drowsiness, sedation, ataxia, depressed respiration, *enhance CNS depression in combo with EtOH
|
|
|
|
Diazepam
|
Valium®. Benzodiazepine tranquilizer. Rx for anxiety, preanesthetic, seizures, withdrawal states, muscle relaxation. Long lasting, t1/2 > 24 hr.
|
|
|
|
Alprazolam
|
Xanax®. Benzodiazepine tranquilizer. Rx for anxiety, antidepression.
|
|
|
|
Temazepam
|
Restoril®. Benzodiazepine tranquilizer. Rx for insomnia.
|
|
|
|
Phenobarbital
|
Barbiturate, CNS depressant. Rx for anticonvulsant, sedative/hypnotic. MOA: acts allosterically on GABA-A receptors to potentiate and prolong effect of GABA. No real margin of safety. Very long acting (t1/2 ~ 2-7 days).
|
|
|
|
Valproate semisodium
|
Depakote®, divalproex sodium. Rx for manic episodes bipolar, epilepsy. MOA: possible GABA agonist. SE: teratogenic, liver disease.
|
|
|
|
Zolpidem
|
Ambien®. Nonbenzodiazepine sedative-hypnotic that acts on BZ receptor, potentiating GABA-A receptor. Rx for insomnia. In the class of "Z drugs" for insomnia.
|
|
|
|
Eszopiclone
|
Lunestra®. Nonbenzodiazepine hypnotic. Rx for insomnia. In the class of "Z drugs" for insomnia.
|
|
|
|
Flumazenil
|
Benzodiazepine antidote. Rx for BZ overdose.
|
|
|
|
Inhibitory NT's bind to what kind of receptors to produce IPSP's?
|
Ligand-gated K+ or Cl- channels. Both types push the local potential towards hyperpolarization, making it more difficult to achieve threshold.
|
|
|
|
Nociception
|
Experience of stimuli that damage tissue
|
|
|
|
What's the function of the anterolateral pathway?
|
To initiate the cells needed for protection and repair due to the stimulus of tissue damaging events. One thing is to make you aware, but the system actually developed to protect you from harm first.
|
|
|
|
4 component operations of the ascending (sensory) system
|
1. Transduction
2. Transmission 3. Perception/Localization 4. Interpretation |
|
|
|
Lissauer's tract
|
Posterolateral tract. Contains Adelta and C fibers from dorsal rootlets entering spinal cord. Through this tract, these afferent fibers can ascend or descend 3 segments before entering gray matter.
|
|
|
|
By the time afferent fibers from Adelta and C cross the midline, where in the spinal cord are they located relative to the segment it entered?
|

They are about 2 segments upward when they have crossed the midline and entered the anterolateral column.
|
|
|
|
How does encapsulation affect a sensory nerve ending?
|
It lowers the threshold potential and allows for more sensitive nerve endings.
|
|
|
|
What enters Lissauer's tract?
|
A-delta and C fibers. NOT A-beta or Ia or Ib or II (muscle spindles)
|
|
|
|
1) The central processes of afferent A-delta and C fibers synapse in which Rexed laminae?
2) And the cell bodies that provide the synapses (2nd order) are located in which laminae? |
1) I, II, V (A delta) and I, II (C fibers)
2) all but II and IX |
|
|
|
What is the somatotopic organization of the anterolateral column?
|
Sacral is dorsolateral and cervical is ventromedial.
As the fibers enter the anterolateral column they enter laterally first. |
|
|
|
The medial part of VPL receives synaptic input from which dorsal fasciculus?
|
Fasciculus cuneatus
|
|
|
|
Stereognosis
|
The faculty of perceiving and understanding the form and nature of objects by the sense of touch--via the lemniscal system. The absence of this ability is astereognosis or tactile object agnosia.
|
|
|
|
Why is the tuning fork placed on bone?
|
To entrap the Pacinian corpuscle against a hard surface so that the cutaneous tissue above it doesn't absorb all the vibration.
|
|
|
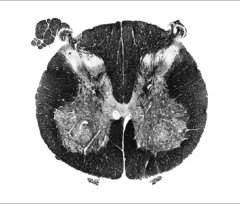
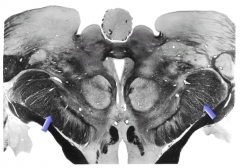
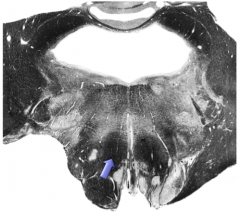
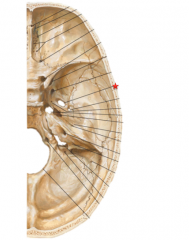
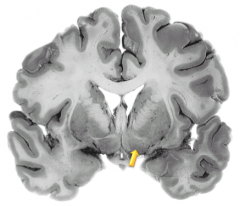
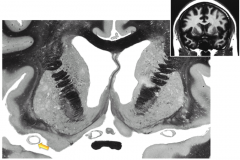
What segment is this? Why?
|
~ S1. The ventral horn is large (limb enlargement) and the dorsal columns are relatively small (not much of the lemniscal column has been added).
|
|
|
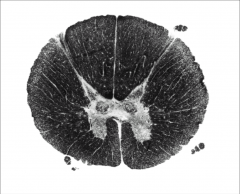
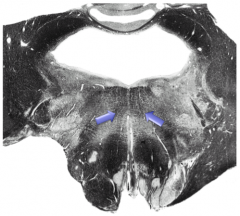
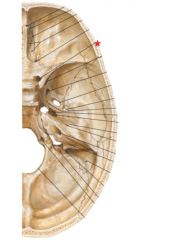
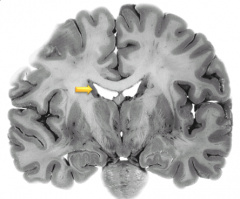
What segment is this? Why?
|
~T2 to T6 probably. The ventral horn is relatively small (so we are not looking at a limb region). The dorsal columns and anterolateral columns are relatively large so we are higher up the spinal cord. Also, we see a lateral horn (IML) which is sympathetic preganglionic cell bodies that are ONLY located between T1 and L2
|
|
|
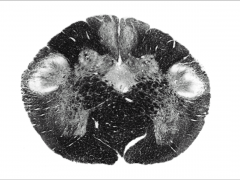
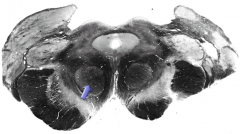
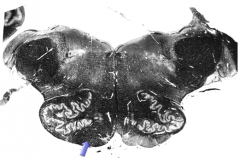
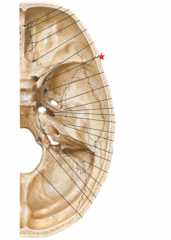
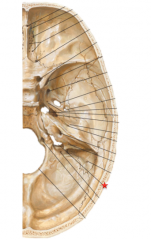
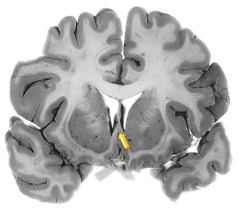
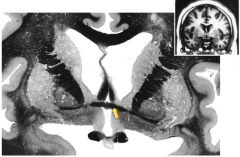
What region is this? Why?
|

Pyramidal decussation is present, therefore we are in the caudal part of the caudal medulla. Also present are the nucleus gracilis and nucleus cuneatus.
|
|
|
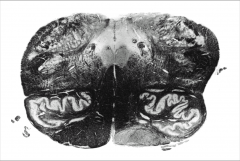
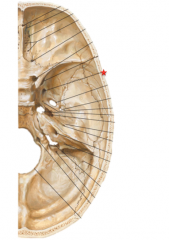
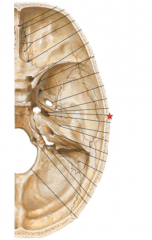
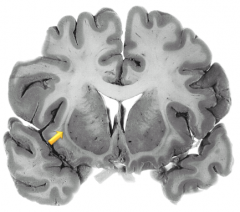
What region of is this? Why?
|

Inferior olivary nucleus is present therefore we are at lower border of rostral medulla.
|
|
|
|
Where is the distribution of the C5 dermatome?
|
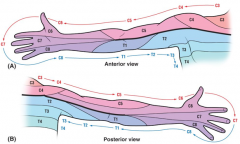
Lateral aspect of arm (e.g. superior aspect of abducted arm).
|
|
|
|
Where is the distribution of the C6 dermatome?
|
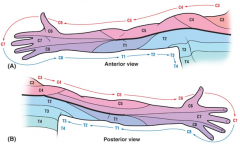
Lateral forearm and thumb
|
|
|
|
Where is the distribution of the C7 dermatome?
|
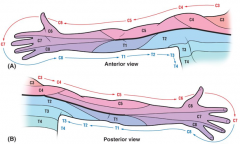
Middle and ring fingers (or middle three fingers) and the center of the posterior and anterior forearm.
|
|
|
|
Where is the distribution of the C8 dermatome?
|
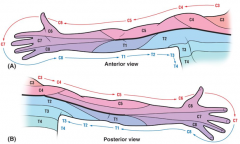
Little finger, medial side of hand and forearm
|
|
|
|
Where is the distribution of the T1 dermatome?
|
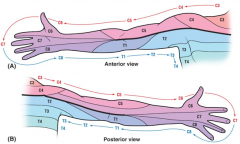
Medial aspect of the forearm and inferior arm
|
|
|
|
Where is the distribution of the L1 dermatome?
|

Inguinal/suprapubic region
|
|
|
|
Which spinal nerve innervates the lateral calf region
|

L5
|
|
|
|
Which spinal nerve innervates the lateral foot region?
|

S1
|
|
|
|
What are the nerve roots for the lateral cutaneous nerve of the thigh?
|
L2-L3
|
|
|
|
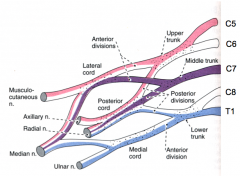
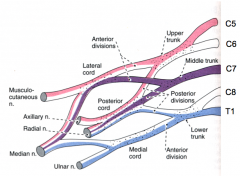
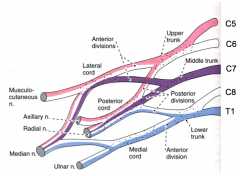
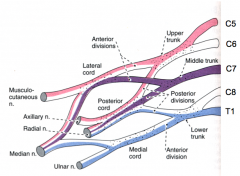
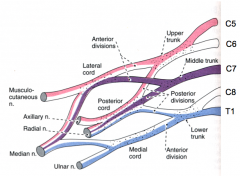
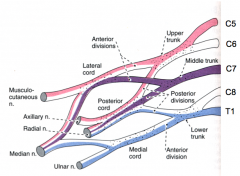
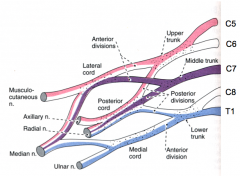
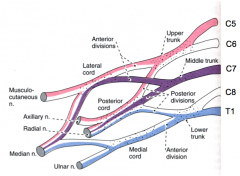
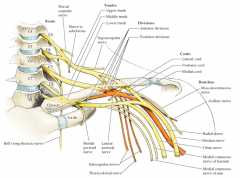
What are the 3 trunks of the brachial plexus and which nerves give rise to them?
|
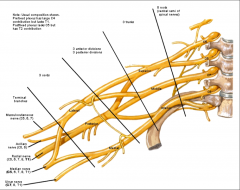
Superior is from C5, C6 ventral rami. Middle is from C7. Inferior is from C8, T1.
|
|
|
|
What are the 3 cords of the brachial plexus and which nerve structures give rise to them?
|
Lateral cord comes from 1 branch off the superior trunk and 1 branch off the middle trunk. Posterior cord comes from 1 branch off the superior, middle, and inferior trunks. Medial cord comes from the continuation of the anterior division of inferior trunk.
|
|
|
|
Where is the lower body located in the motor homunculus?
|

Medial to the arms, near the sagittal fissure.
|
|
|
|
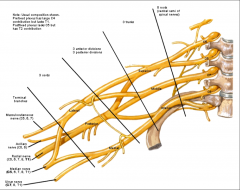
Describe the layout of the internal capsule and its bordering structures.
|
V-shaped, "pointing medially". Anterior limb is bordered by globus pallidus and putamen laterally and the caudate nucleus medially. The genu is the knee or bend. The posterior limb is bordered by the globus and put laterally and the diencephalon medially.
|
|
|
|
Describe the spatial relationships of the posterior columns fibers as they cross the midline in the medulla.
|
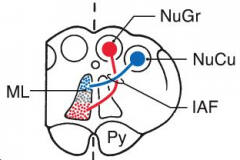
In the posterior column, FGr is medial and FCu is lateral. After synapsing with their respective nuclei, Gr moves ventrally and Cu moves dorsally via the interarcuate fibers.
|
|
|
|
Renshaw cells
|
Inhibitory interneurons in the spinal cord that receive their afferent input from collateral branches of nearby efferent cells. These cells are "unique" because they are interneurons that are activated by efferent cells rather than afferent or descending neurons.
|
|
|
|
Where are LMN cell bodies that innervate trunk flexors and extensors located?
|

Medially inside the ventral horn
|
|
|
|
All LMN's are located in which Rexed lamina? Where is it located?
|
Lamina IX are "islands" within the ventral horn. There is somatotopic organization within the lamina IX islands in which axial innervation is medial and limb innervation is lateral.
|
|
|
|
Which muscle fiber type (white/red) are more sensitive to disuse atrophy?
|
Red fiber type
|
|
|
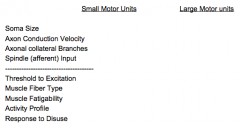
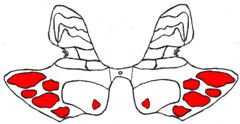
Compare/contrast motor unit size
|
|
|
|
|
What type of nerve fiber innervates the periequatorial region of a muscle spindle?
|
Type II fiber -- afferent fiber from secondary nerve endings (predominantly nuclear chain fibers) of the muscle spindle
|
|
|
|
What does the "total convergence/total divergence" idea mean for Ia fibers?
|
The Ia fibers from muscles spindles in a given muscle diverge and converge to monosynaptically "communicate" with all LMN's of that muscle.
|
|
|
|
Which spinal nerves does the knee-jerk reflex test?
|
L3 - L4 specifically, because this is the portion of the femoral nerve (L2 - L4) that innervates the quadriceps.
|
|
|
|
Why is normal muscle tone maintained when passive muscle lengthening occurs?
|
The alpha motor neuron activity stimulated by Ia afferents is counterbalanced by alpha motor inhibition from GTO's.
|
|
|
|
Define muscle tone
|
The level of activity (contraction) seen in resting skeletal muscle. "Resting" means some motor units are activity but not sufficient to produce movement. I.e. a muscle's resistance to passive stretch during a resting state
|
|
|
|
UMN lesions are characterized by:
|
Weakness, spasticity (clasped-knife phenomenon), hyperreflexia, primitive reflexes and the Babinski sign. Primitive reflexes include the grasp, suck and snout reflexes.
|
|
|
|
LMN lesions are characterized by:
|
Weakness, hypotonia, hyporeflexia, atrophy and fasciculations.
|
|
|
|
Fasciculations
|
Fine movements of the muscle under the skin; indicative of lower motor neuron disease. They are caused by denervation of whole motor units leading to ACh hypersensitivity at the denervated muscle. Atrophy of the affected muscle is usually concurrent with fasciculations.
|
|
|
|
Eccentric contraction
|
Sarcomeres get longer as you contract because the opposing force is greater than what the muscle is generating.
|
|
|
|
Concentric contraction
|
Sarcomeres get shorter as you contract because the force of muscle contraction is greater than the opposing load.
|
|
|
|
Which type of afferent nerve fiber supplies secondary endings in the muscle spindle?
|
Type II afferent
|
|
|
|
If gamma neuron firing goes down, spindle sensitivity goes...?
|
Down. By decreasing gamma motor neuron activity, the spindle is allowed to relax and become "less sensitive to stretch".
|
|
|
|
What's the goal of alpha/gamma coactivation in maintaining muscle tone?
|
To maintain a constant afferent Ia pulse in order to keep the same number of motor units active throughout a full range of passive motion.
|
|
|
|
Why are the lower limb reflexes more brisk than upper limb reflexes?
|
Lower limb reflexes (especially the extensors) are modified to be brisk, automatic reflexes because they are working on anti-gravity muscles.
|
|
|
|
What are some characteristics of automatic behaviors (responses/reflexes)?
|
relatively simple;
relatively predictable response to a specific stimulus; relatively independent of "higher centers"; not typically or greatly affected by alterations in consciousness |
|
|
|
Pronator drift
|

When holding arms outwards and supinated, the arm (contralateral to the lesion in the brain due to stroke) drifts to a mid-pronated position. This is due to spasticity in the pronator muscle.
|
|
|
|
Spasticity
|
A motor disorder involving UMN's characterized by a velocity-dependent increase in tonic stretch reflexes (muscle tone) and exaggerated phasic muscle stretch reflexes.
|
|
|
|
Muscle reflex latency
|
How long after the stimulus does the reflex response occur? Not observable clinically, but can see it with nerve conduction studies. Demyelinating diseases can manifest this way.
|
|
|
|
Muscle reflex amplitude
|
How great is the response with a standardized stimulus? Compare bilaterally.
|
|
|
|
Muscle reflex spread
|
Does the stimulus cause alpha motor neuron activity in other muscles besides the one being tested? E.g. crossed-adductor reflex. By tapping the patellar tendon, the other leg adducts.
|
|
|
|
Muscle reflex duration
|
How long does the elicited reflex (contraction) occur? E.g. hanging reflexes.
|
|
|
|
Plantar reflex
|
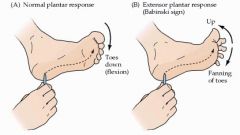
Stroking of the lateral foot and across the plantar base of the toes. Normally, the toes should flex and curl inward. Abnormally, the Babinski sign is the extension and fanning of the toes in response to the plantar stimulus. This is due to a UMN lesion is adults, and can be normal in infants < 1 y/o.
|
|
|
|
Which afferent fibers mediate the second, burning pain, warm, dull pain, itching, and sensual touch?
|
C fibers
|
|
|
|
Which afferent fibers mediate the first/fast pain, sharp pain, cold and pressure sensation?
|
A delta fibers
|
|
|
|
What is the midbrain tectum?
|
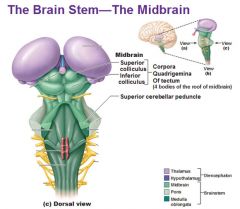
Literally, the "roof" of the midbrain. Located in the dorsal mesencephalon (midbrain)-- it consists of superior and inferior colliculi (i.e. or the nuclei residing within these "bumps").
|
|
|
|
Who talks to the magnocellular cells of the red nucleus?
|
Cortex, globus pallidus, cerebellum.
|
|
|
|
What's the general role of the cerebellum in communicating with motor neuron pathways?
|
The cerebellum determines the sequences of events (EPSP's and IPSP's) in time to achieve a specific motor task.
|
|
|
|
What's the general role of the basal ganglia in communicating with motor neuron pathways?
|
The basal ganglia determine which LMN's you need to sends EPSP's and IPSP's to in order to achieve a specific motor task.
|
|
|
|
Describe the pathway of the rubrospinal tract.
|
The tract begins in the red nucleus (midbrain), crosses midline at ventral tegmental decussation, and descends contralaterally in the lateral funiculus (along with the lateral corticospinal tract). Note, some collateral branches terminate early in the pons and medulla.
|
|
|
|
What is the major target of rubrospinal innervation?
|
Upper limb proximal flexor muscles. Although it does go to flexors in the lower limb.
|
|
|
|
Where do tectospinal fibers decussate?
|
Dorsal tegmental decussation
|
|
|
|
What's the boundary between the medulla and the spinal cord, and where is it located?
|
Cervicomedullary junction, located at the foramen magnum
|
|
|
|
Where do fibers in the anterior corticospinal fibers cross the midline?
|
Mostly at the segmental level via interneurons rather than crossing at the pyramidal decussation.
|
|
|
|
What are the 3 regions that UMN's can be found in the frontal cortex?
|
Precentral gyrus, premotor cortex, supplementary cortex.
|
|
|
|
For corticospinal UMN's, the most rostral decussating fibers come from where in the cortex?
|
Upper limb (lateral cortex). The upper limb ends up medial in the lateral tract and the lower limb is lateral.
|
|
|
|
Betz cells
|
Very large neurons in the primary motor cortex, but only make up 4% of corticospinal cells. These tend to go to the distal musculature of the limb and synapse with alpha motors without interneurons.
|
|
|

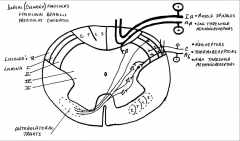
What is this diagram showing?
|
Not everyone has a "textbook" pattern of pyramidal decussation. Most normal is 85% decuss/15% ipsilateral. However, 3% of people don't decussate at all, and 13% of people decussate completely (leaving no anterior pathway).
|
|
|
|
Corticospinal UMN's are influenced by:
|
1) cortical-cortical connections (e.g. frontal lobe, what's the goal?, write a program)
2) cortico-ponto, ponto-cerebellar, cerebellar-thalamic, thalamic-cortical (control WHEN in time that EPSP's and IPSP's need to fire to achieve a particular muscle movement) 3) cortico-strio, strio-pallido, pallido-thalamic, thalamocortico (WHICH muscles need to contract/relax) |
|
|
|
Corticospinal fibers passing through the cerebral peduncle (midbrain)
|
|
|
|
Genu of the internal capsule.
|
|
|
|
VPL nuclei
|
|
|
|
Cerebral peduncles
|
|
|
|
Red nucleus
|
|
|
Where are the corticospinal fibers located? What proportion of corticospinals make up this region?
|
1 million out of 4 million in that "fifth" of the peduncle. In total, the peduncle has ~20 million axons.
|
|
|
|
Ventral tegmental decussation
|
|
|
|
MLF (medial longitudinal fasciculus). Interconnects the occulomotor, trochlear, and abducens nuclei so that we get conjugate eye movements.
|
|
|
|
Longitudinal pontine bundles. These are formed by axons of the tightly compacted cerebral peduncles being separated by the pontine nuclei into less compact bundles.
|
|
|
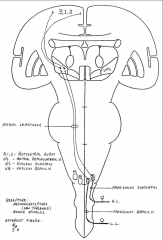
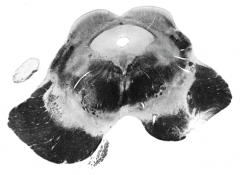
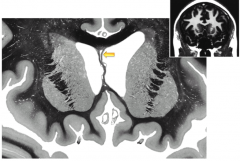
Where is this slice from?
|
Caudal pons. 4th ventricle, inferior cerebellar peduncle, pontine nuclei and longitudinal pontine bundles (some of which are coalescing to soon become pyramids)
|
|
|
|
Medial lemniscus
|
|
|
|
Tectospinal fibers
|
|
|
|
Medullary pyramid
|
|
|
|
Erb's palsy
|
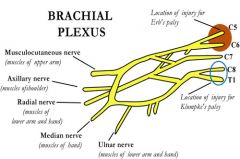
Nerve injury to C5-C6 roots, with the suprascapular, musculocutaneous, and axillary being damaged most often. Loss of elbow flexion, supination, leads to "waiter's tip". Shoulder dystocia during childbirth is a common cause.
|
|
|
|
Klumpke's palsy
|
Primarily affects the lower roots of the brachial plexus (C8 - T1). Leads to weakness of the intrinsic hand muscles and flexors of the wrist and fingers. "Klumpke the monkey hung from a tree".
|
|
|
|
Nerve branches of the posterior cord of the brachial plexus
|
ARTS: axillary, radial, thoracodorsal, subscapular (upper and lower).
|
|
|
|
5 parts of the brachial plexus
|
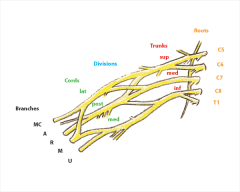
Roots, Trunks, Divisions, Cords, Branches. Mnemonic: Russell Trigonis Drinks Cold Beers.
|
|
|
|
Nerve roots of lumbosacral plexus
|
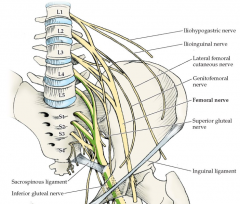
L1 - S4
|
|
|
|
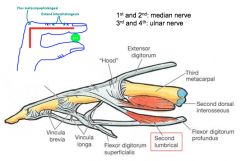
What are the motor actions and sensory innervations of the median nerve?
|
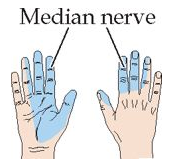
Motor: Thumb flexion and opposition, flexion of digits 2 and 3, wrist flexion and abduction, forearm pronation.
|
|
|
|
What are the motor actions and sensory innervations of the ulnar nerve?
|
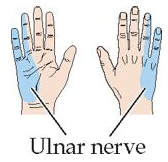
Motor: Finger adduction and abduction other than thumb; thumb adduction; flexion of digits 4 and 5; wrist flexion and adduction
|
|
|
|
What are the motor actions and sensory innervations of the musculocutaneous nerve?
|
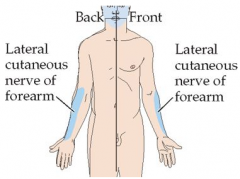
Motor: Flexion of arm at elbow, supination of forearm
|
|
|
|
3 nerves acting on the thumb movement
|
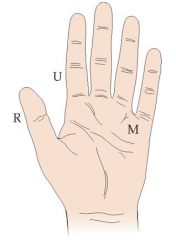
Radial: abducts thumb (plane of palm)
Ulnar: adducts thumb (plane of palm) Median: opposes thumb, and abducts thumb (perp. to plane of palm) |
|
|
|
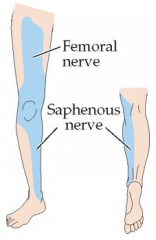
What are the motor actions and sensory innervations of the femoral nerve?
|
Motor: Leg flexion at the hip, leg extension at the knee
|
|
|
|
What are the motor actions and sensory innervations of the obturator nerve?
|

Motor: Adduction of the thigh
|
|
|
|
What are the motor actions and sensory innervations of the tibial nerve?
|
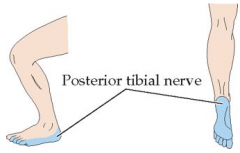
Motor: Foot plantar flexion and inversion, toe flexion
|
|
|
|
What are the motor actions and sensory innervations of the superficial peroneal nerve?
|
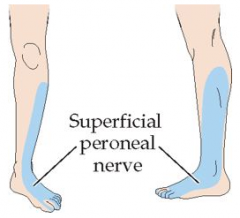
Motor: Foot eversion
|
|
|
|
What are the motor actions and sensory innervations of the deep peroneal nerve?
|
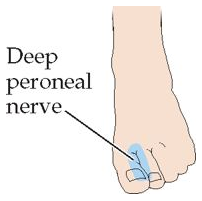
Motor: Foot dorsiflexion, toe extension
|
|
|
|
What innervates the hamstring muscles (for knee flexion)?
|
Sciatic nerve
|
|
|
|
What are the conduction speeds for A-delta and C fibers?
|
A-delta fibers: 15 - 30 m/s
C fibers: 0.5 - 2 m/s |
|
|
|
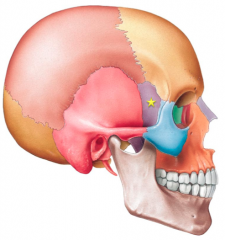
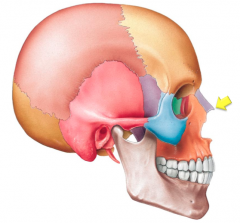
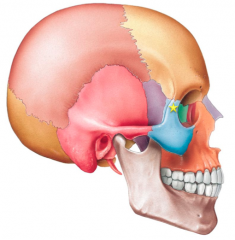
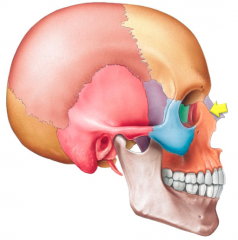
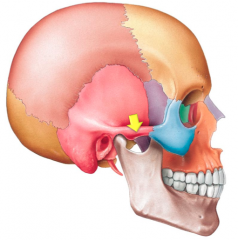
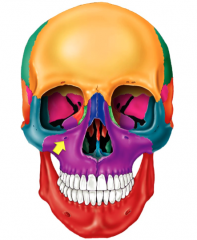
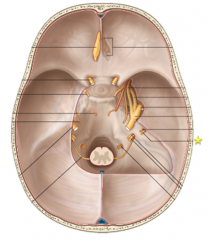
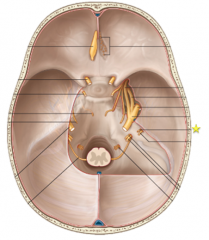
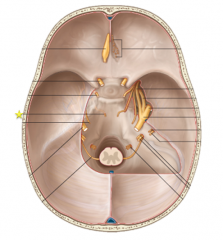
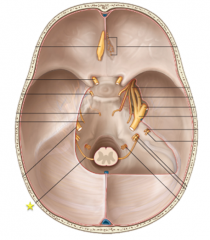
Foramen Ovale:
Mandibular nerve (V3), Accessory Meningeal Artery, Lesser Petrosal nerve |
|
|
|
Optic canal:
Optic nerve (CNII), opthalmic artery |
|
|
|
Superior orbital fissure:
Oculomotor nerve (CNIII), trochlear nerve (CNIV), abducens nerve (CNVI), opthalmic nerve (V1), superior opthalmic vein |
|
|
|
Foramen rotundum:
Maxillary nerve (V2) |
|
|
|
Jugular foramen:
Glossopharyngeal nerve (IX), Vagus nerve (X), Accessory nerve (XI), Sigmoid sinus, Posterior meningeal artery, inferior petrosal sinus |
|
|
|
Foramen lacerum:
Greater petrosal nerve, internal carotid (via the carotid canal) |
|
|
|
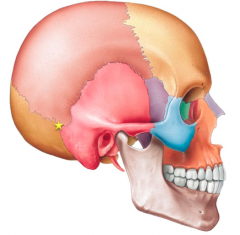
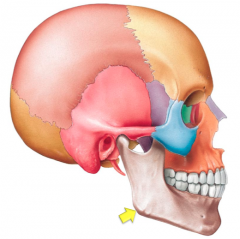
Asterion
|
|
|

|
Glabella
|
|
|
|
Gonion
|
|
|
|
Greater wing of sphenoid
|
|
|
|
Rhinion
|
|
|
|
Hoffman's reflex
|
Test for UMN lesion - Flicking the middle finger to check for reflex contraction of the thumb or index finger. The positive response is abnormal if asymmetric and could be a normal finding if symmetric (e.g. hyperreflexia). Ex. testing for cervical myelopathy.
|
|
|
|
Frontal process of the zygomatic bone
|
|
|
|
Frontomaxillary suture
|
|
|
|
Zygomatic process of the temporal bone
|
|
|
|
Infraorbital foramen
|
|
|

|
Frontonasal suture
|
|
|

|
Middle nasal concha
|
|
|

|
Greater palatine foramen
|
|
|
|
The anterior spinal artery supplies what portion of the spinal cord?
|

ASA supplies anterior 2/3 and PSA's supply posterior 1/3.
|
|
|
|
Artery of Adamkiewicz
|
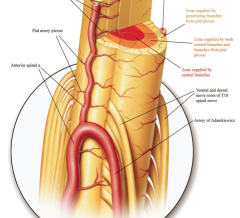
A branch off of the thoracic aorta (variable) that supplies the anterior spinal artery (as an "anterior segmental medullary artery). Provides blood supply to anterior cord below T11-T12.
|
|
|
|
CN VIII, Vestibulocochlear nerve passing through the internal acoustic meatus
|
|
|
|
CN VII, Facial nerve passing through the internal acoustic meatus
|
|
|
|
CN VI, Abducens nerve - will pass through the superior orbital fissure.
|
|
|
|
CN XI, Spinal accessory - will pass through the jugular foramen.
|
|
|
|
Nerve roots of femoral nerve
|
L2 - L4
|
|
|
|
Nerve roots of common peroneal nerve
|
L4 - S2
|
|
|
|
Nerve roots of sciatic nerve
|
L4 - S3
|
|
|
|
Nerve roots of tibial nerve
|
L4 - S3
|
|
|
|
Nerve roots of superficial peroneal nerve
|
L5 - S2
|
|
|
|
Nerve roots of deep peroneal nerve
|
L4 - L5
|
|
|
|
Nerve roots of dorsiflexion
|
L4*, L5
|
|
|
|
Nerve roots of toe extension
|
L4, L5*
|
|
|
|
Nerve roots of plantar flexion
|
L5, S1*, S2
|
|
|
|
Nerve roots of toe flexion
|
S2, S3
|
|
|
|
Nerve roots of foot eversion
|
L5*, S1*, S2
|
|
|
|
Nerve roots of superior gluteal
|
L4 - S1
|
|
|
|
Nerve roots of inferior gluteal
|
L5 - S2
|
|
|
|
Nerve roots of obturator nerve
|
L2 - L4
|
|
|
|
Nerve roots of finger extension
|
C7*, C8
|
|
|
|
Thumb abduction in the plane of the palm
|
Radial nerve (C7*, C8)
|
|
|
|
Finger abduction
|
Ulnar nerve (C8, T1*)
|
|
|
|
Lumbricals: function and innervation
|
Flexion of the metacarpophalangeal joints, extension of the interphalangeal joints.
|
|
|
|
You suspect a C5 radiculopathy. Where do you suspect sensory abnormalities? Where do you suspect muscle weakness?
|
The region of sensory abnormality would be in the shoulder and lateral arm. The main weaknesses associated with C5 would be deltoid (abduction), infraspinatus (lateral rot. of arm), and some biceps (elbow flexion).
|
|
|
|
You suspect a C6 radiculopathy. Where do you suspect sensory abnormalities? Where do you suspect muscle weakness?
|
The region of sensory abnormalities would be in the first and second fingers and the lateral forearm. The mains weaknesses associated with C6 would be biceps (elbow flexion) and wrist extensors.
|
|
|
|
You suspect a C7 radiculopathy. Where do you expect sensory abnormalities? Where do you suspect muscle weakness?
|
The region of sensory abnormalities would be in the third finger. The main weaknesses associated with C7 would be triceps (elbow extension).
|
|
|
|
You suspect a L4 radiculopathy. Where do you expect sensory abnormalities? Where do you suspect muscle weakness?
|
The region of sensory abnormalities would be on the knee and medial leg. The main weaknesses associated with L4 would be iliopsoas (hip flexion), quadriceps (knee flexion) and ankle dorsiflexion.
|
|
|
|
Epidural hematoma
|
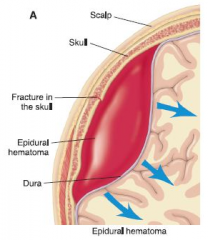
Rupture of middle meningeal artery (branch of maxillary artery), often secondary to fracture of temporal bone. Lucid interval. Rapid expansion under systemic arterial pressure --> transtentorial herniation, CN III palsy. CT shows "biconvex disk" not crossing suture lines. Can cross falx, tentorium.
|
|
|
|
Subdural hematoma
|
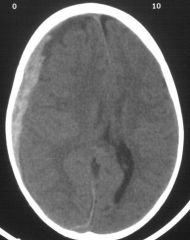
Rupture of bridging veins. Slow venous bleeding (less pressure = hematoma develops over time). Seen in elderly individuals, alcoholics, blunt trauma, shaken baby (predisposing factors brain atrophy, shaking, whiplash). Crescent-shaped hemorrhage that crosses suture lines. Midline shift. Gyri are preserved, since pressure is distributed equally. Cannot cross falx, tentorium.
|
|
|
|
Subarachnoid hemorrhage
|
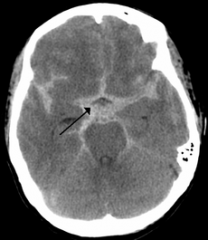
Rupture of an aneurysm (usually berry aneurysm in Marfan's, Ehlers-Danlos, ADPKD) or an AVM. Rapid time course. Patients complain of "worst headache of my life." Bloody or yellow (xanthochromic) spinal tap. 2-3 days afterward, risk of vasospasm due to blood breakdown (not visible on CT, treat with nimodipine) and rebleed (visible on
CT) |
|
|
|
Impaired function of multiple nerve roots below L1 or L2 is called _______.
|
Cauda equina syndrome
|
|
|
|
You suspect a L5 radiculopathy. Where do you expect sensory abnormalities? Where do you suspect muscle weakness?
|
The region of sensory abnormalities is the lateral leg, dorsum of the foot and the big toe. The main weaknesses associated with L5 are gluteus medius (hip abduction), foot dorsiflexion, big toe extension, foot eversion and inversion.
|
|
|
|
You suspect an S1 radiculopathy. Where do you expect sensory abnormalities? Where do you suspect muscle weakness?
|
The region of sensory abnormalities is the lateral foot, small toe, and the plantar surface of the foot (except for big toe area). The main weaknesses associated with S1 are the posterior leg muscles (plantar flexion) and gluteus maximus (hip extension) .
|
|
|
|
Pinprick of the big toe tests which spinal nerve root?
|
L5
|
|
|
|
The superolateral thigh contains which spinal nerve's autonomous zone?
|
S2
|
|
|
|
Where is the L3 autonomous zone?
|
Medial thigh superior to the knee
|
|
|
|
Where is the L4 autonomous zone?
|
Medial leg, midway between knee and ankle
|
|
|
|
The lateral border of the foot contains which spinal nerve's autonomous zone?
|
S1
|
|
|
|
Hemiplegia
|

Total paralysis of the arm, trunk, and leg on one side of the body. Most common cause is stroke.
|
|
|
|
Absent pin prick sensation on the skin of the palmer surface of the left long finger?
|
Left side C7 radiculopathy
|
|
|
|
At what level of the brainstem do the axons of the gracile nuclei and cuneate nuclei cross the midline?
|
Rostral part of the caudal half of medulla
|
|
|
|
Topesthesia
|
The ability to localize light touch
|
|
|
|
Graphesthesia
|

Tactual ability to recognize writing on the skin
|
|
|
|
Sensory extinction
|
Extinction to simultaneous sensory stimulation (ESS) is a clinical phenomenon in which a patient perceives a unilateral sensory stimulus presented in isolation but fails to perceive the same stimulus when presented simultaneously with a second stimulus
|
|
|
|
Describe the 5 muscle strength grades
|
5/5: full ROM against gravity w/ max resistance
4/5: full ROM against gravity w/ some resistance 3/5: full ROM against gravity w/ no resistance 2/5: full ROM w/o gravity 1/5: palpable or visible contraction w/ little or no movement 0/5: no palpable or visible muscle contraction |
|
|
|
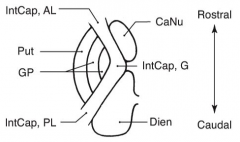
Components of striatum
|
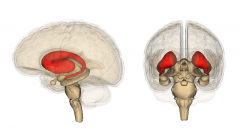
Putamen and caudate nucleus
|
|
|
|
Components of corpus striatum
|
Putamen, caudate nucleus, globus pallidus
|
|
|
|
Components of lenticular nucleus
|
Putamen and globus pallidus
|
|
|
|
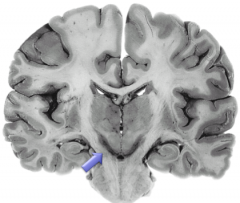
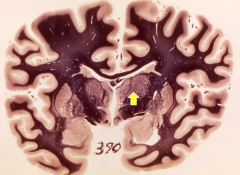
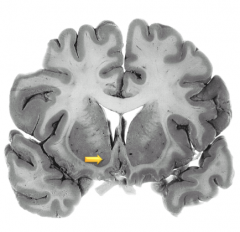
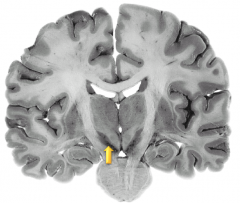
Caudate nucleus from a coronal slice that is relatively rostral because the caudate nucleus is fairly thick here.
|
|
|
|
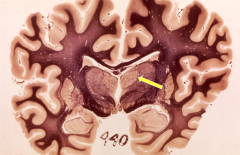
Putamen
|
|
|
|
Internal medullary lamina of the globus pallidus. This is a coronal slice at the level of the optic chiasm.
|
|
|
|
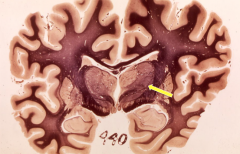
Thalamus. This is a coronal slice at a level posterior to the optic chiasm. The internal capsule (posterior limb) is seen. Also seen superficially and inferior are the mammilary bodies, hypothalamus, and 3rd ventricle.
|
|
|
|
Internal medullary lamina of the thalamus
|
|
|
|
External medullary lamina of the thalamus
|
|
|
|
What does the internal medullary lamina of the thalamus separate?
|
Medial nuclear group and the lateral nuclear group
|
|
|
|
Describe the major functions of the cerebellum vs. basal ganglia.
|
Cerebellum - plays major roles in the timing of motor activities and in rapid, smooth progression from one muscle movement to the next. Also helps control the intensity of muscle contraction when the muscle load changes and controls the necessary instantaneous interplay between agonist and antagonist muscle groups.
Basal ganglia - help to plan and control complex patterns of muscle movement, controlling relative intensities of the separate movements, directions of movements, and sequencing of multiple successive and parallel movements for achieving specific complicated motor goals. |
|
|
|
3 anatomical lobes of the cerebellum
|
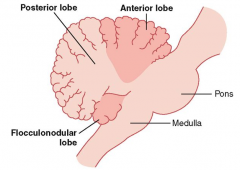
Anterior, posterior, and flocculonodular
|
|
|
|
Striatum efferents use which neurotransmitter?
|
GABA
|
|
|
|
GPe and GPi efferents use which neurotransmitter?
|
GABA
|
|
|
|
The primary fissure of the cerebellum separates which 2 lobes?
|
Anterior and posterior
|
|
|
|
Which fissure separates the posterior lobe of the cerebellum from the flocculonodular?
|
Posterolateral fissure
|
|
|
|
5 cell types of the cerebellar cortex?
|
Stellate cells, basket cells, purkinje cells, golgi cells, and granule cells
|
|
|
|
Name the layers of the cerebellar cortex (from superficial to deep).
|
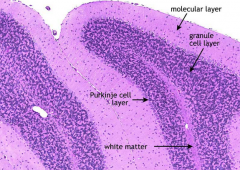
Molecular layer (few cells) --> Purkinje cells --> Granular layer (many cells)
|
|
|
|
Types of cells in the granular layer of the cerebellum
|

Golgi cells and granule cells
|
|
|
|
Types of cells in the molecular layer of the cerebellum
|

Stellate cells (tend to be more superficial), and basket cells (closer to purkinje cells)
|
|
|
|
Rigidity
|
Increased resistance throughout the range of movement, in both directions, which is not rate-dependent.
|
|
|
|
Lead pipe vs. cogwheel rigidity
|
Cogwheel (gamma) rigidity: Rachety pattern of resistance and relaxation as the examiner moves the limb through its full range of motion
Lead-pipe rigidity: State of stiffness & inflexibility that when an increase in muscle tone causes a sustained resistance to passive movement throughout the whole range of motion, with no fluctuations. |
|
|
|
Hypomimia
|
Reduced degree of, or a "masked" facial expression. Often seen in PD
|
|
|
|
Indirect pathway of basal ganglia
|
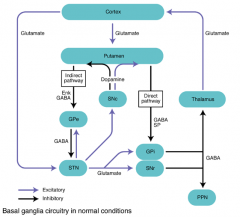
Putamen to GPe (inhibitory), GPe to subthalmic nucleus (inhibitory), STN to GPi (excitatory), GPi to thalamus (inhibitory), thalamus to cortex (excitatory). A normally stimulated indirect pathway inhibits motor activity. Normal DA input on indirect pathway stimulates motor activity.
|
|
|
|
Direct pathway of basal ganglia
|
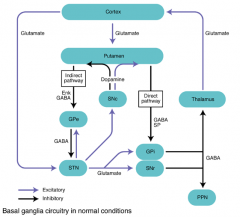
Putamen to GPi (inhibitory), GPi to thalamus (inhibitory), thalamus to cortex (stimulatory). A normally stimulated direct pathway stimulates motor activity. Normal DA input on direct pathway stimulates motor activity.
|
|
|
|
The subthalmic nucleus projects what kind of neurons to the GPi?
|
Glutamatergic (stimulatory)
|
|
|
|
Nucleus accumbens
|
|
|
|
Septal nuclei
|
|
|
|
Claustrum
|
|
|
|
Ventral pallidum. Contains the cells of Meynert.
|
|
|
|
Caudate nucleus
|
|
|
|
Substantia nigra
|
|
|
|
Septum pellucidum. The lateral side is ependymal lined and the medial side is pia.
|
|
|
|
Middle cerebral artery lying in the Sylvian fissure (between the frontal and temporal lobes).
|
|
|
|
Anterior commissure
|
|
|
|
Ventral anterior nuclei of the thalamus
|
|
|
Where are the cell bodies whose axons terminate here?
|
Predominantly in the frontal lobe
|
|
|

If you destroy this structure, signs and symptoms will occur on which side?
|
Ipsilateral (right)
|
|
|
|
Not being able to smell after head injury?
|
Damage to the olfactory filia (being sheared off at the cribiform plate) due to inertia.
|
|
|
|
What do Bowman's glands do in the olfactory epithelium?
|
They secrete mucous so that olfactory molecules can be dissolved in order to activate chemoreceptors on the cilia.
|
|
|
|
Which cell in the olfactory bulb has the predominant task of sending olfactory information back to the brain?
|
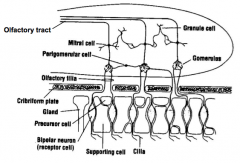
Mitral cells
|
|
|
|
Primary olfactory cortex
|
Located in the lateral olfactory gyrus which surrounds the lateral olfactory stria. Only perceive odorants when they activate cells here.
|
|
|
|
"Double inhibitory" system of olfaction?
|
There are inhibitory neurons in the olfactory bulb AND in the olfactory tract that project back to the bulb that inhibit olfaction sense.
|
|
|
|
Scotopic vision
|
The vision of the eye under low light (monochromatic, low acuity). Mediated by rod cells. Most sensitive around 498 nm (blue-green).
|
|
|
|
Photopic vision
|
The vision of the eye under well-lit conditions (color perception, high acuity). Mediated by cone cells.
|
|
|

|
Anisocoria (unequal pupil size)
|
|
|

|
Scotoma - a circumscribed region of visual loss
|
|
|
|
Homonymous defect
|

See 4, 5, 6, 7.
Homonymous - same visual defect in both eyes. |
|
|
|
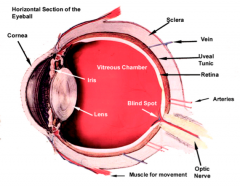
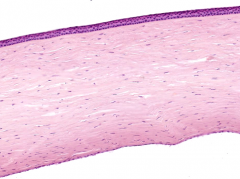
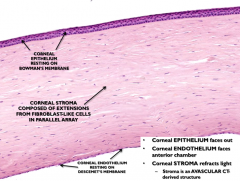
Corneoscleral tunic
|
Outer "housing", principally collagenous. Route by which blood vessels get in/out and form choroid. Cornea is the chief refractory structure (60-70%). External ocular muscles attach to this tunic.
See 3rd side... |
|
|
|
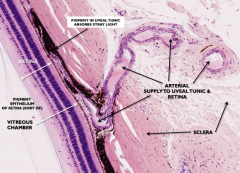
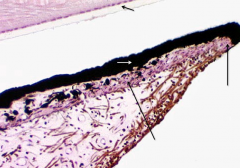
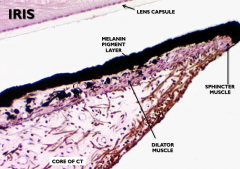
Uveal tunic
|
Supportive tunic: focusing mechanism (lens), light adjustment (iris), reflection dampening, nourishment of retina (choroid), production and removal of aqueous (ciliary body/processes)
|
|
|
|
|
|
|
|
Bowman's membrane
|
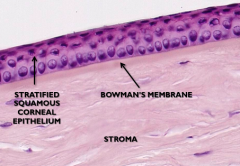
Located between superficial epithelium and stroma. Strong collagen fibers help the cornea keep its shape.
|
|
|
|
Drainage of aqueous humor
|
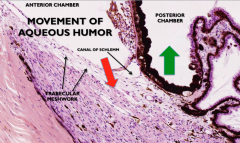
AH is removed via the canal of Schlemm. Blockage of this can lead to glaucoma.
|
|
|
|
|
|
|
|
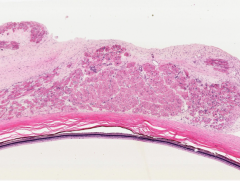
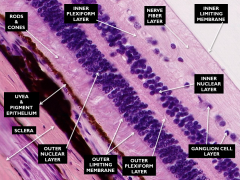
9 layers of the retina
|
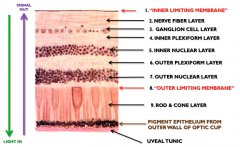
Also, see 3rd side...
|
|
|
|
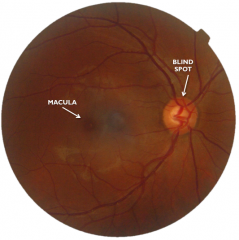
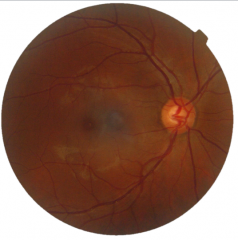
Fundus of right eye: blind spot is also nasal to macula.
|
|
|
|
Optic disc
|
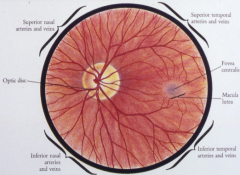
aka (optic papilla)
-disc diameter – 1.5 mm -nasal half – thicker and pinker -temporal half – lighter and sharper -physiologic cup – < 30-40% disc diameter -cup/disc ratio – 3-4/10 Retinal Vessels veins – slightly larger than arteries and may pulsate arteries – “silver wire” appearance |
|
|
|
How does an increase in intracranial pressure affect the physiological cup of the eye?
|
The increased CSF pressure pushes the optic nerve back towards the optic cup causing optic papilladema. It may elevate the physiologic cup (flattening the concavity).
|
|
|
|
What are the variations of the optic chiasm as it relates to the hypophysis?
|
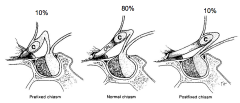
|
|

