![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
202 Cards in this Set
- Front
- Back
|
PT comes in with headache or other acute neuro findings in the ER
What is the first imaging study you want to use? ****** |
NON CONTRAST CT
|
|
|
What is one key reason why CT is better than MRI?
*** |
it is good for quick evaluation of acute bleeding: Excellent for acute intracranial hemorrhage
(also, MRI might require pre-approval for access) |
|
|
where do epidural bleeds most commonly occur
|
fronto-temporal area
|
|

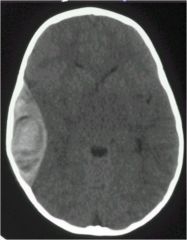
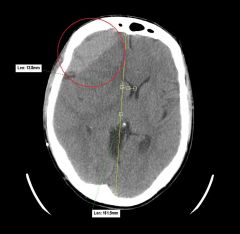
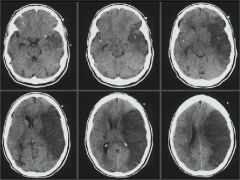
What is this? Where is it occuring
|

Epidural bleed
frontal lobe |
|
|
what are the Hounsfield units for:
water bone air blood Fat |
0 = water density
+ 1000 = bone -1000 = air + 60 – +80 = blood - 5 to –12 = fat |
|
|
T1 vs T2 on MRI?
|
T1 = the “anatomic” sequence
T2 = the “pathology” sequence On T1 water is dark black On T2 water is bright white |
|
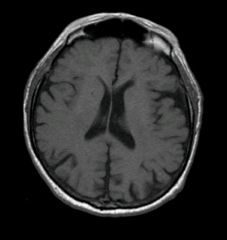
T1 or T2?
What 4 things are black on this type of image? |
T1
Cortical bone Bone Moving blood Fluid |
|
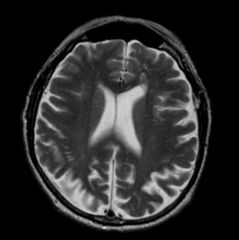
T1 or T2
|
T2
|
|
|
Which study, MRI or CT can detect ischemic injusry 24-36 hours earlier than the other?
|
MRI
|
|
|
This imaging study has no bone artifact (especially in the posterior fossa), and is better at assessment of tumors, white matter, and disease/early edema?
|
MRI
|
|
|
Which imaging study (CT or MRI) has unchanged multi-planar capability?
** |
MRI
|
|
|
A 26 y/o patient presents to the ED after being struck by a softball bat. You want to rule our intracranial hemorrhage. You order:
A. CT B. MRI |
CT (no contrast)
Cranial bone will be white |
|
|
Which modality is best for evaluating white matter disease?
A. CT B. MRI |
MRI
|
|

CT or MRI?
|
MRI
|
|
type of image? Path?
|
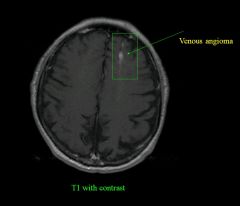
|
|
|
what normally causes an epidural hematoma?
Subdural? |
epi: skull fracture
sub: direct blow to the head w change in lvl of conciousness |
|
|
What happens in shear injuries?
|
diffuse axonal injury
can be due to rotational injury (not necessarily blow to a head) |
|
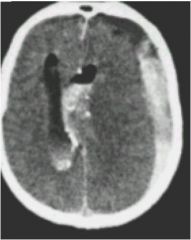
path?
will it cross sutural lines? what blood vessel causes it? |
epidural hematoma
DOESN'T CROSS SUTURAL LINES assoc with skull fracture due to arterial tear (middle meningeal artery) |
|
|
epidural hematoma vs subdural hematoma
which crosses suture lines? |
epidural hematoma :DOESN'T CROSS SUTURAL LINES
Sub: does |
|
|
for an epidural hematoma, at what amount of bleeding do you have to consider operative tx?
|
less than 5mm: NON OPERATIVE
greater than 5mm: drain |
|

|
epidural hematoma in kid
|
|
|
describe some of the characteristics of subdural hematomas (shape, blood source, who it happens to)
|
crecentic,
bridging veins, old people who fall |
|
|
SDH more common with ____ while
EDH more common with _____ (cause of injury) |
SDH more common with falls
EDH more common with MVA |
|
|
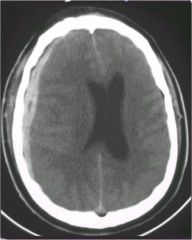
Subdural Hematoma
|
|
|
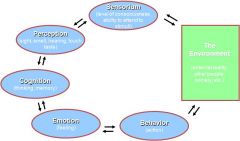
Define the purpose of the Mental Status Exam
(o) |
Examination of neuropsychiatric functioning
Comprehensive description of a patient’s appearance, behavior, thinking, feeling, etc. Meaningful only in the context of other baseline data (e.g., history, physical / neurologic exam) Ex. Tearful patient may be reacting to stress or pain, be depressed, have neurological disease, or other cause The MSE ≠ MMSE |
|
|
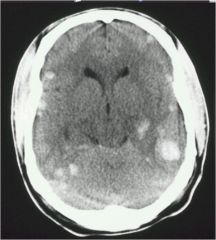
there are 3 densities seen on CT with a SDH..what are they and what are the time frames assoc with them
|
Acute 0 to 3-4 days hyperdense
Subacute 3 to 20 days isodense Chronic > 20 days hypodense |
|
|

SDH
|
|
|
epidural hematoma
|
|
|
this type of injury Occur with rapid acceleration/deceleration
Usually involves large WM tracts: corpus callosum, brainstem and deep white matter Occurs at gray-white matter interface due to slight differences in mass Minor differences in tissue inertia |
Shear Injuries
|
|
|
Intraparenchymal hemorrhage from shear injuries
|
|
|
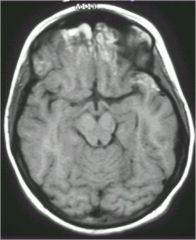
MRI showing
intra parenchymal hemorrrhage |
|
|
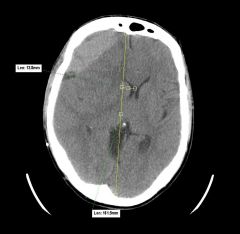
Left Middle Cerebral Artery Infarction with midline shift:
what is the most useful landmark for measuring midline shift? |
Most useful landmark for measuring midline shift: Septum Pellucidum
note:This type of edema is called cytotoxic edema cytotoxic edema visible on CT and MRI |
|
|
what is key to remember about cytotoxic edema?
|
Affects both gray and white matter
|
|
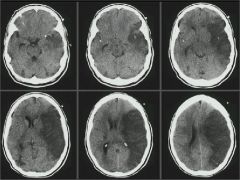
History: stroke symptoms
|
cytotoxic edema
|
|
|
Explain how the Mental Status Exam is performed
(o) |
By observation
i.e., many areas assessed while obtaining the history e.g., speech, behavior, affect By asking relevant questions to elicit symptoms that usually cannot be observed e.g., hallucinations, paranoid ideation, mood By performing cognitive screening tests e.g., MMSE, other bedside tests |
|
|
vasogenic edema is found where?
cytogenic? causes? *** |
vasogenic edema: CONFINED TO WHITE MATTER (tumor or infection)
where cytogenic could be in white or gray (infarct or stroke) |
|
|
SUMMARY SLIDE
CT is 1st in the emergent setting to rule out hemorrhage. MRI is more sensitive for edema, tumors, infections and white matter disease. Be able to distinguish SDH from EDH. Be able to distinguish cytotoxic (stroke) from vasogenic (tumor or infection) |
CT is 1st in the emergent setting to rule out hemorrhage.--FAST
MRI is more sensitive for edema, tumors, infections and white matter disease.--CONTRAST MAKES IT EVEN MORE SENSITIVE Be able to distinguish SDH from EDH.--SDH more cresentic, covers further distance, not confined by sutures Be able to distinguish cytotoxic (stroke-effects both grey and white matter) from vasogenic (tumor or infection--just in white matter) |
|
|
Identify the major components of the Mental Status Exam
(o) |
General appearance, attitude (toward the examiner), and behavior
Motor activity (overactivity, underactivity, abnormal movements, catatonia) Speech Mood and affect Thought process (form) and content Perception Cognitive function Insight and judgment |
|
|
What is the difference btw catatonia, catalepsy, and cataplexy?
*** |
Catatonia: motor symptom: Dx by any two of the following: a. motor immobility, b. motor excitement, c. negativism or mutism, d. posturing, stereotypies or mannerism, e. echolalia (parroting) or echopraxia (miming)
Catalepsy: feature of catatonia, waxy flexibility (muscular rigidity and fixity of posture regardless of external stimuli, as well as decreased sensitivity to pain.) Cataplexy: sudden loss of muscle tone leading to collapse, related to narcolepsy |
|
|
describe the following mood/affects
Constricted/Restricted (flat) Labile Expansive |
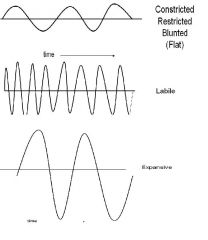
|
|
|
define the following disturbances in thought process:
Circumstantiality Tangentiality Looseness of associations Verbigeration “Word Salad” Neologisms Clang associations |
Circumstantiality (excessive detail but gets to point)
Tangentiality (never gets to point of message) Looseness of associations (ideas loosely connected) Verbigeration (meaningless repetition of words/phrases) “Word Salad” (incoherent collection of words/phrases) Neologisms (creation of new words) Clang associations (rhyming/punning; no logical connection) |
|
|
describe circumstantial thought
*board fodder |

|
|
|
Describe Tangential thought
* |

|
|
|
Describe flight of ideas
***** |

|
|
|
what is the difference between hypnagogic and hypnopompic hallucinations? are these pathological or non pathological?
*** |
Nonpathological: hypnagogic (when you go to sleep), hypnopompic (when you wake up)
Pathological: Auditory, visual, tactile, olfactory, gustatory, somatic |
|
|
what are
Perceptual disturbances? (4) **** |
include:
hallucinations, derealization (where I am at doesn't feel real, i am floating in the space I am in), depresonalization (feel like you are floating outside of yourself), déjà vu |
|
|
One-half of all lifetime cases of mental illness begin by age...
|
14
three-quarters by age 24. |
|
|
on the MMSE what score points to cognitive problems?
|
less than 20
|
|
|
Recognize the difference between the Folstein MMSE and the mental status examination
(o) note: answer extrapolated from Wiki |
The mini–mental state examination (MMSE) or Folstein test is a brief 30-point questionnaire test that is used to screen for cognitive impairment. It is commonly used in medicine to screen for dementia. It is also used to estimate the severity of cognitive impairment at a given point in time and to follow the course of cognitive changes in an individual over time, thus making it an effective way to document an individual's response to treatment.
Mental status is way more in depth |
|
|
What are illusions (with respect to perceptual disturbances?)
** |
misinterpretation of real stimuli
|
|
|
Define psychiatric illness
(o) |
Any of various conditions characterized by impairment of an individual's normal cognitive, emotional, or behavioral functioning, and caused by social, psychological, biochemical, genetic, or other factors, such as infection or head trauma.
Also called emotional illness, mental illness, mental disorder. |
|
|
what is the difference btw primary and secondary psychiatric disorders?
|
Primary psychiatric disorders
No underlying medical disorder to account for the diagnosis Not caused by medication Not caused by substance abuse or withdrawal Secondary psychiatric disorders Due to a medical condition Due to a medication(s) Due to substance abuse or withdrawal |
|
|
Identify the domains of psychiatric illness (6)
(o) |
Some People Can Eat Bad Eggs
|
|
|
Identify the classification systems used to diagnose psychiatric illness
(o) |
Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR)
Published by the American Psychiatric Association (2000) Most recent update of criteria: DSM-IV (1994) Current DSM bases diagnostic codes on ICD-9-CM International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) Published by the US government in 1979 Official coding system in the US for all diseases (Ch.5 Mental Dis) Revises codes annually but has not kept up with diagnostic changes in the DSM |
|
|
What is an important thing to remember about the DSM IV and diagnosis it gives
**** |
Contains a listing of psychiatric disorders, diagnostic codes, and criteria for each disorder
Also contains text with information about the disorder (e.g., associated features, prevalence, course, familial patterns, age-,culture- and gender-specific features, differential diagnosis) ***Does NOT contain information about presumed etiology or treatment**** |
|
|
Describe the DSM-IV-TR multiaxial diagnostic system
(o) |
Axis I: Clinical Disorders (psychiatric)
Axis II: Personality disorders and traits, mental retardation, prominent defense mechanisms Axis III: General Medical Conditions Axis IV: Psychosocial and environmental problems (stressors) Axis V: Global Assessment of Functioning (1-100 scale) EXAMPLE Axis I 296.22 Major Depressive Disorder, single episode, moderate 305.00 Alcohol Abuse Axis II 301.6 Dependent Personality Disorder Axis III Hepatitis B Axis IV Threat of job loss Axis V GAF = 45 (current) |
|
|
explain why most mechanisms of action given the neuropharmacologic drugs are approximations.
(o) |
Entire mechanism is generally unknown. Approximations of
CNS mechanism made from information regarding effects of drugs in isolated systems. CNS as a “Black Box” Extrapolation from biochemical events to behavior is difficult. |
|
|
Identify the components of a psychiatric evaluation
(o) |
History (Identifying Data/Reason for admission or evaluation, Past Psychiatric History, Substance History, Mental Status Exam)
Exam (neuro/mental) Radiological and lab |
|
|
SUMMARY SLIDE FOR LECTURE 2 OF PSYCH
|
Psychiatric symptoms can be seen in many conditions
The etiology of most primary psychiatric disorders is not known Diagnosis is based primarily on history and mental status exam Physical exam, neurologic exam, lab, and other studies are performed to rule out possible non-psychiatric causes of psychiatric symptoms The DSM-IV-TR increases reliability of diagnosis |
|
|
define what is meant by specific mechanism of action.
(o) |
A specific drug action affects a recognized protein target, i.e., a receptor, an ion channel, an enzyme, or a transporter.
|
|
|
describe the various events in synaptic transmission which might be altered by drugs
(o) |

|
|
|
The student will be able to explain and account for differences in brain-injury patterns caused by high- and low-velocity missiles.
(o) |
k.e.= ½ m v2
so the faster the traveling bullet (military weapon) will be more likely to kill you than a slow moving bullet (civilian weapon) |
|
|
please define a concussion
(o) |
Diffuse, physiological and microscopic insult, with or without diffuse axonal injury
Usually defined as involving a period of confusion or unconsciousness, even if just brief Numerous common associated symptoms, e.g. headache, dizziness, irritability, emotionality, poor concentration |
|
|
what is the difference between a neurotransmitter and a neuromodulator?
(o) |
Neurotransmitter – a substance which is released locally and causes a change in post-synaptic potential.
Neuromodulator – a substance which acts to modify the response of the synapse to a neurotransmitter. (make a stimulus stronger or weaker) |
|
|
highschool football player gets hit on the head in the second half of the game and dies. Why did this happen? this is an example of?
* |
You look back and see that the kid got hit on the head in the 1st half but it was dismissed or not realized
the SECOND IMPACT SYNDROME says that the brain is waaayyyy more vulnerable to a 2nd injury this is more common in younger ppl |
|
|
recognize the substances which have been proposed to act as CNS neurotransmitters
(o) |
Acetylcholine
Amino acids Biogenic amines Peptides Purines (ATP, adenosine) Nitric acid Endocannabinoids |
|
|
differentiate between ionotropic and metabotrophic receptors.
(o) |
Ionotropic receptors (also known as ligand-gated ion channels) are associated with ion channels, and change ionic conductance.
Mediate fast, short effects. Metabotropic receptors are coupled with enzymes via G-proteins and other intermediates. Mediate slow, long effects. |
|
|
describe the blood brain barrier and its implications in drug therapy (what are the characteristics that regulate diffusion of substance through capillaries)
(o) |
A term used to describe diffusional barriers retarding the passage of substances from the central circulation to nerve cells.
Characteristics which regulate diffusion of substances through capillaries are: Molecular weight Lipid solubility Ionization at physiological pH (ionized drugs are not lipid soluble) |
|
|
Little Johnny gets hit in the head during a game and gets knocked out. Mom and Dad bring him to you and ask if he can play the next game in 2 days. What do you tell them
|
have to be at least a week of no symptoms before they can resume play
|
|
|
pleas define a brain contusion..where do they tend to occur?
(o) |
Focal hemorrhages within brain tissue
Big enough to see with naked eye in a pathology specimen or as an area of intensity (whiteness) on a CT scan Tend to occur around edges of brain, particularly at base of cerebrum and in anterior temporal lobes |
|
|
describe a subdural hematoma including the location, and appearance on CT initially and chronically
(o) |
Traumatic hemorrhage from veins inside dura but outside brain
This behaves like an actual space, so, acutely, blood runs from anterior to posterior pole The hematomas appear initially white (X-ray dense) on CT Over time, the hematomas get diluted and resorbed, and become less X-ray dense |
|
|
describe an epidural hematoma including the location, and appearance on CT initially and chronically...what is the cause?
(o) |
Traumatic hemorrhage from meningeal arteries inside skull but outside dura
This is a potential space through which the fresh blood dissects from edge to edge, creating a lens-shaped hematoma that does not extend from pole to pole (the subdural does) The hematomas appear white (X-ray dense) on CTs acutely, but become less dense as they dilute and resorb |
|
|
please describe the Glasgow Coma scale, including the 3 aspects, and scoring ranges
|
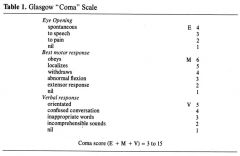
|
|
|
define epilepsy...
incidence? |
2 or more unprovoked seizures
incidence is highest in kids and old folk |
|
|
in-between epileptic seizures, what is a common finding on EEG?
|
Spikes
|
|
|
What happens in an absence seizure? clinically and EEG
(o) |

Clinic: pt suddenly stops responding/no eye contact for about 7 seconds and then just resumes back to normal (full recovery)
EEG: sudden spiking in all leads, quick onset, quick ending |
|
|
What happens in a tonic-clonic seizure? clinically and EEG
(o) |

Clinic: abrupt onset with no warning, pt starts arching back (tonic) and then clonic (shaking all over), NO IMMEDIATE RECOVERY, pt might have pissed themselves, bit their tongue, want to go to bed--this is what you classically think of as a seizure
EEG: sudden rapid hashy spiking (tonic) in all leads, followed by spike then pause, spike then pause (in all leads) leading to the jerkiness (clonic). When the seizure ends, the EEG is not completely normal (shows the disorientation when it ends) |
|
|
What happens in a Partial Simple Seizure? clinically and EEG
(o) |

specific to what brain area is affected
for example, a pt could have a left motor seizure causing a right arm tremor. Pt is wide awake, aware of the symptoms, but can't stop them EEG: Will only see irregular activity in certain leads (that correspond to one side of the brain, thus focal) |
|
|
What happens in a Partial Complex Seizure? clinically and EEG
(o) |
occurs in the Temporal lobe
usually clouding of consciousness EEG: Will only see irregular activity in certain leads (that correspond to one side of the brain, thus focal) Can occur in 4 places: anterior-deja vu/psychic symptoms Sylvian- Epigastric sensation, movement of mouth and face Mid-temporal - auditory hallucinations, depersonalization posterior temporal-Complex visual hallucinations |
|
|
a pt says every now and then I keep seeing a pack of wild dogs that nobody else can see...what is this?
|
Partial-Complex Seizure
|
|
|
what is common and similar in Absence and Partial Complex Seizures
Consider: brain involvement Age of pt Duration Sx recalled by pt Movements or behaviors After-effects EEG pattern Underlying Cause Effective Tx TEST!!!!!!!!!!!!!!!!!!!!!!!!! |
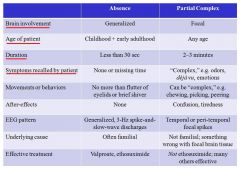
ONLY THING SHARED: STARING AND DECREASED RESPONSIVENESS
|
|
|
The student will be able to correlate the age of onset of first seizure with likely underlying causes.
Consider: Idiopathic Febrile Birth Injury Metabolic Infection Trauma Tumor Stroke (o) |
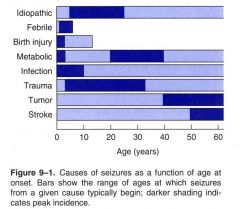
|
|
|
The student will be able to describe the means and rationale for investigation of a new seizure disorder by history, examination and ancillary testing.-JUST READ
(o) |
CBC—is there an elevated white count to imply infection?
Chemistries—especially glucose, sodium, calcium, renal function tests and liver function tests. Brain imaging to look for macroscopic focal disease, such as tumor, stroke, arteriovenous malformation or developmental anomaly. An MRI scan including coronal sections through the medial temporal lobes is ideal, but there are circumstances in which a CT is substituted, e.g. when the patient is restless, claustrophobic or has a pacemaker. An EEG, preferably sleep-deprived to increase sensitivity. Does the EEG show abnormalities, especially spikes, highly associated with seizures? If so, are they focal or generalized? |
|
|
pt presents with multiple cognitive deficits including memory impairment, aphasia, apraxia (arm won't do what you tell it to), agnosia (trouble remembering what objects are), or trouble in executive functioning (have trouble cooking). What do they have?
(o) |
Alzheimer's Dz
note: the shrinking effect on the brain is bigger due to age than Alzheimers (like an 80 year old with AD would have a larger brain than a normal 90 year old) |
|
|
on a PET scan, what will be a difference seen in a pt with Alzheimer's dz?
|
less activity posteriorly
|
|
|
amyloid plaques are commonly seen on silver stain in what? what is another pathological finding of this problem?
|
Alzheimer's Dz
Neurofibrillary Tangles (used to be neurotubules, will be in the cells) |
|
|
What are 2 pharmacological tx for AD?
|
Acetylcholinesterase Inhibitors [Examples: Donepezil (Aricept) Galantamine (Reminyl, Razadyne)
Rivastigmine (Exelon)] --used in mild to moderate disease NMDA (Glutamate) Receptor Blocker (Memantine (Namenda))-- Moderate level of disease |
|
|
Progressive dementia clinically similar to Alzheimer’s disease
Early, prominent involvement of frontal and temporal lobes (“frontotemporal dementia”) (o) |
Pick's Disease
will find Pick Bodies intracellularly note: PET scan will show less activity in the frontal and temporal lobes (who'da thought) |
|
|
Hypokinesia/akinesia
Bradykinesia Rigidity (not to be confused with spasticity or paratonia) Stooped posture Small-stepped gait “Rest” tremor, typically unilateral or asymmetric area all seen in what? |
Parkinsonism
|
|
|
associated with degeneration of substantia nigra cells containing intracellular Lewy bodies
(o) |
Parkinson's Disease
|
|
|
Usual fluctuations in cognitive function, involving alertness and attention
Visual hallucinations are common Will also have movement problems Pathologically, intracellular Lewy bodies appear diffusely in the cerebral cortex (o) |
Dementia with Lewy Bodies
Clinically resembles a blend between Alzheimer’s and Parkinson’s diseases note: in Parkinson's, the Lewy Bodies are mostly in the Substantia Nigra |
|
(o)
|
|
|
|
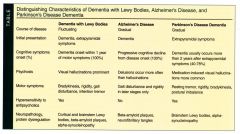
flip for a comparison of dementia with Lewy Bodies, Alzheimer's Disease, Parkinson's
|
|
|
|
pt presents to your office due to changes in mood. Upon walking you notice that they seem to flick their hand, or kind of dance around. What is this? Genetics?
(o) |
Huntington’s Disease
Autosomal dominant with high penetrance Abnormal gene on chromosome 4 note: the dancing/flicking movement is known as CHOREA |
|
|
What change in the brain would you see in a pt with Huntington's disease?
|
Absence of the Caudate Nucleus
|
|
|
A rapidly progressive, fatal dementia involving prominent motor symptoms, such as rigidity, clumsiness, and myoclonic jerks
A transmissible “spongiform” encephalopathy involving abnormal proteins called prions Diagnosed with certainty only by brain biopsy (o) |
Creutzfeldt-Jakob Disease
|
|
|
What are the 3 categories of Creutzfeldt-Jakob Disease? Which are we most concerned about?
|
Sporadic CJD appearing without known risk factors accounts for 85% of cases.
Hereditary CJD involves positive family history or positive testing for a genetic mutation. 5-10% of U.S cases. Acquired CJD involves transmission by exposure to brain or nervous system tissue. 1% of cases. (****transmission from open wounds, retina transplant, etc) |
|
|
Increased levels of CSF protein 14-3-3 would give you the diagnosis of?
|
Creutzfeldt-Jakob Disease
|
|
|
inflammatory demyelinating plaques in the central nervous system is the hallmark of what?
(o) |
Multiple Sclerosis (MS)
has to do with OLIGODENDROCYTES (not Schwann--peripheral) |
|
|
T1 “Black Holes” and brain atrophy can be seen in what?
|
Multiple Sclerosis
note: Gilenya ™ - Fingolimod is the first oral pill tx for MS |
|
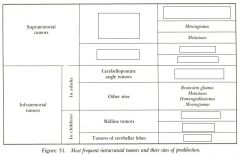
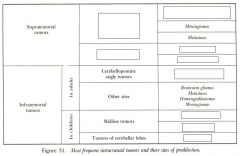
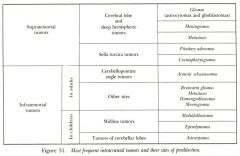
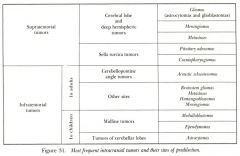
2. The student will be able to correlate brain tumors and their usual anatomic compartments.
3. The student will be able to provide examples of brain tumors that are more or less common in younger and older patients. (o) |
|
|
|
midline tumors and tumors of cerebellar lobes are more common in adults or kids?
|
kids
|
|
|
this is the Fastest-growing and most lethal brain tumor in astrocytoma series
Infiltrates and spreads widely within brain, so surgery cannot entirely remove Surgery still warranted for biopsy, with or without de-bulking and insertion of Gliadel wafer Radiation therapy usually applied * |
Glioblastoma Multiforme
|
|
|
this brain tumor is chiefly in adults 30-50, has Intermediate growth rates depending on grade, can sit dormant for years with no effect. Radiation therapy can be applied, but is usually reserved for when the tumor is perceived as growing because there is a lifetime limit to how much can be given.
|
Cerebral Astrocytomas
|
|
|
Usually the slowest growing brain tumors, but can eventually crowd the brain.
Often discovered as an incidental finding on a scan done for another reason Are usually calcified and are therefore very recognizable on CT scans. |
Meningiomas
|
|
|
please give an example that fits each of the following:
A fast-growing intracranial tumor displaces brain. A slow-growing intracranial tumor replaces brain |
A fast-growing intracranial tumor displaces brain. (Examples: glioblastoma multiforme, metastases.)
A slow-growing intracranial tumor replaces brain. (Example: typical meningioma.) |
|
|
Most frequent incidence between ages of 30 and 50
Also calcify and usually show this on CT scans. Intermediate growth rate, and is usually "managed" (surgery, RT) rather than cured Glial cell in origin |
Oligodendrogliomas
|
|
|
Can be hormonally active or disruptive
Can compress optic chiasm from below and produce visual field losses Often removed surgically through the nose and sphenoid sinus |
Pituitary Adenomas
|
|
|
what are some of the important areas that can be damaged by occluding the middle cerebral arteries?
|
Broca/Wiernicke's
Motor/Sensory cortex Frontal eyelid Optic radiation... others |
|
|
Comprise about 1/3 of childhood posterior fossa tumors
Predilection for cerebellar vermis Though malignant, they are highly radio-sensitive |
Medulloblastomas
|
|
|
posterior fossa tumor of childhood
Often encapsulated Complete surgical extirpation often possible |
Cerebellar Astrocytoma
|
|
|
2 of the most common primary cancers in existence are what? so what can this lead to?
(o) |
breast and Lung
can lead to brain (intermediate tenancy to go to the brain) |
|
|
The student will be able to describe more and less common sources of metastatic brain tumors.
aka what are the most and least likely to go to the brain*** (o) |
Prostate: DOES NOT go to brain
Melanoma: GOES TO BRAIN (very high propensity) |
|
|
The student will be able to describe treatments for tumors of the nervous system as well as their optimum applications and limitations. What are the options (4)
(o) |
High-dose corticosteroids
Surgery Radiation therapy Chemotherapy |
|
|
How do high dose corticosteroids help treat brain tumors?
(o) |
Buys time by shrinking the edema around the tumor deposit, rather than affecting the tumor itself.
Effective against extracellular edema, but not intracellular edema, such as that seen in ischemia. A typical starting dose is dexamethasone 10 mg, followed by 4 mg q.i.d |
|
|
how does radiation therapy help treat CNS tumors?
(o) |
RT is usually palliative--to shrink but not eliminate tumor deposits
For brain metastases, RT is sufficiently effective that the patient usually dies of non-CNS complications before CNS complications. The treatment itself can damage the CNS. |
|
|
When do you often see chemotherapy for CNS tumor treatment?
(o) |
Usually reserved for glioblastoma multiforme (Fastest-growing and most lethal brain tumor in astrocytoma series
Infiltrates and spreads widely within brain, so surgery cannot entirely remove) IV administration is complicated by intact blood-brain barrier blocking entry into CNS. BCNU (carmustine) given IV probably crosses BBB to some extent. Gliadel® wafers (also carmustine) can be implanted within the tumor bed. |
|
|
anterior cerebral artery blockage can lead to problems where
|
leg and foot of motor and sensory
|
|
|
Posterior cerebral artery occlusion will give you what major problem?
|
visual deficits
|
|
|
non-traumatic Subarachnoid Hemorrhage is normally due to what?
|
aneurysm
|
|
|
where do aneurysms typically occur? (berry)
|
close to the circle of willis
most in Anterior communicating (like in marfans) |
|
|
besides trauma, what are the 2 major causes of intraparenchymal hemorrhage?
(o) |
Hypertension-associated
Arterio-venous malformation (AVM) note: this is literally bleeding into brain tissue |
|
|
where do Charcot-Bouchard microaneursyms occur? how are these different from Berry aneurysms
* |
on penetrating arteries (deep in the brain, leading to areas like the basal ganglia)--assoc with intraparenchymal hemorrhage
different from saccular (Berry) aneurysms occurring near the circle of Willis. assoc with subarachnoid hemorrhage |
|
|
large wedge shaped damage vs small pockets of damage...
please list what type of vessels were damaged (o) |
Wedges: large vessels
small pockets/lacunae: small (will be in penetrating arteries |
|
|
what is the difference between an embolism and thrombosis
(o) |
embolism: some garbage from upstream got dislodged, then it gets stuck in the brain
thrombosis: clot...can lead to breaking off and causing an embolism so: embolism arises from somewhere else, thrombus occurs from the site |
|
|
what is most commonly going to cause an embolism?
|
Atrial fibrillation
(irregularly irregular) |
|
|
what is the concept of ischemic penumbra?
* |
There is a central core of forever-lost brain cells that no treatment can revive surrounded by a larger zone of sick brain cells that may or may not recover – depending on acute management.
|
|
|
in stroke, what effect can blood sugar have on acute stoke management?
|
Too high can be damaging!!
|
|
|
what are some of the modifiable atherosclerotic risk factors? 4 (+1 non-modifiable)
(o) |
Blood pressure
Blood sugar Lipids (statin drug) Smoking note: Family History |
|
|
shortly after stroke it is important to monitor BP. If it is really high what should you do? Should you let a pt walk right away?
|
we lost autoregulation, so be careful not to drop BP too aggressively-->can extend the stoke
so if their BP is high, don't worry about it for the immediate time being also, don't let them walk, they may have an unsafe drop in BP |
|
|
if you are going to give a drug for acute treatment of thrombotic stroke, which of the following would you use?
t-PA heparin aspirin |
ASPIRIN has small benefit acutely
note: heparin would be good to prevent DVT from bed rest |
|
|
what commonly causes stroke for old and young folks?
(o) |
old folks: atherosclerosis or emboli from heart
young folks: congenital heart/great vessel defects; hypercoaguable states, migraine with aura + smoking + contraceptives |
|
|
Giant Cell Arteritis
Tumor Subarachnoid Hemorrhage Subdural Hematoma Epidural Hematoma Medication Overuse Headaches are examples of what type of headache? (o) |
Secondary Headaches
|
|
|
a pt shows up with really bad headaches and insists they have a tumor that is causing it. You respond..
|
they are extremely rare, and not likely the cause of your headache
|
|
|
What is a medication overuse headache?
(o) |
person needed to take medicine for a headache
they took it too often for a long enough time you transform it into a 2ndary headache that is more difficult to treat headaches will occur everyday, present throughout the whole day, and is mild to moderate. It worsens when the medication is discontinued |
|
|
an elderly female presents to your office with a unilateral headache, jaw claudication and impaired vision. What does this pt have? is this a primary or secondary headache? FIRST AID REVIEW: What is the tx??
(o) |
Giant cell arteritis
secondary High dose steroids |
|
|
Migraine without Aura
Migraine with Aura Tension-Type Headaches Cluster Headaches are what kind of headaches? (o) |
Primary
|
|
|
pt presents with a unilateral headache that feels like it is "pulsing". They say it is aggravated with activity and they have some nausea. They say they only have light sensitivity some of the times when this occurs...what is it?
|
Migraine without aura
|
|
|
what are some of the common triggers for migraines?
|
Hormonal – menstruation, ovulation, OCP, HRT
Dietary – alcohol, nitrite-laden meat, MSG, aspartame, chocolate, aged cheese, missing a meal Psychological – stress, post-stress let-down, anxiety, worry, depression Physical/Environmental – glare, flashing lights, visual stimulation, fluorescent lighting, odors, weather changes, high altitudes Sleep-related – lack of sleep, excessive sleep Miscellaneous – head trauma, physical exertion, fatigue Drugs – NTG, histamine, reserpine, hydralazine, ranitidine, estrogen |
|
|
what is the most common aura in migraines with aura? some examples?
|
VISUAL
scotomas (blind spots), photopsia (unformed flashes of light), fortification spectra (scintillating zig-zag lines), distortions in shape and size. In “retinal migraine,” these occur unilaterally instead of bilaterally. |
|
|
what are the 5 types of migraine auras?
|
Visual: scotomas (blind spots), photopsia (unformed flashes of light), fortification spectra (scintillating zig-zag lines), distortions in shape and size. In “retinal migraine,” these occur unilaterally instead of bilaterally.
Somatosensory: unilateral paresthesias (spontaneous sensations) or hypesthesia (decreased perception of applied stimuli). Motor: hemiparesis. Language: aphasia (impairment of language comprehension or expression). Brainstem: loss or change in level of consciousness, diplopia, tinnitus or hearing loss, vertigo, dysarthria, ataxia, bilateral sensory or motor symptoms. |
|
|
pt comes in with a mild/moderate pressing headache that is bilateral. It does not get worse with activity and there is no nausea associated with it...what is this?
(o) |
Tension type headache
THE ANTI MIGRAINE (pretty much the opposite: no light sensitivity, no nausea, doesn't get worse with activity) |
|
|
what does the "cluster" refer to in cluster headache?
|
The "cluster" means clustering in time (not location)
|
|
|
pt presents with recurrent headaches occurring around the the eye lasting for about 15 minutes to 2 hours. He says the pain is intense but then goes away. What is this?
(o) |
Cluster headache
|
|
|
Clumsiness in greater proportion than loss of power
Babinski sign present (immediate) Spasticity (delayed) Increased tendon reflexes (delayed) Little if any atrophy what type of lesion? (o) |
Upper motor neuron lesion
|
|
|
what is Spasticity...what is it associated with (upper or lower mn)
(o) |
A unidirectional increase in muscular tone
Involves increased tone in “anti-gravity” muscles In the upper extremities, resistance to stretching out biceps, but not triceps In the lower extremities, resistance to stretching out quadriceps but not hamstrings seen in upper motor neuron |
|
|
What is Rigidity? what is it seen in?
(o) |
Seen in Parkinson’s disease and other extrapyramidal disorders
A bi-directional increase in tone to passive range of motion The resistance to passive range of motion is relatively independent of degree of force or rate of speed |
|
|
What is Paratonia? commonly seen in?
(o) |
feels like the pt is trying to stop you from moving the limb
Commonly seen in dementia Also known as gegenhalten (to hold against) A bidirectional resistance to passive range of motion that increases with force and rate of movement, as if voluntary |
|
|
Loss of power in greater proportion than clumsiness
Hypotonia Muscle atrophy Muscle fasciculations what type of lesion? (o) |
Lower Motoneuron
|
|
|
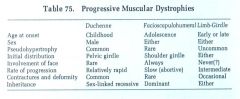
Compare Duchenne, Facioscapulohumeral, and Limb girdle Muscular dystrophies for the following characteristics:
Age of onset Sex Pseudohypertorphy Initial distribution Involvement of the face Rate of progression Contractures and deformity Inheritance (o) |
|
|
|
what is the genetic defect in duchenne muscular dystrophy?
|
Dystrophin gene on short arm of X chromosome codes for dystrophin protein, which is a cytoskeletal structural protein.
this is damaged |
|
|
a boy presents to your office and on physical exam you note that their calves are pretty toned. Mom says that when the boy is on the ground he does this strange thing where he arches his back and climbs his way off the ground...what is this called? sign of?
|
Gower's sign
in Duchenne |
|
|
you are in your neuro office and examining a young lady patient who has issues with smiling. You ask her to smile and she physically can't. Her forehead is unwrinkeld and the corners of her mouth do not curl. On physical exam, you note winging of the scapula. What does this pt have?
|
Facioscapulohumeral Muscular Dystrophy
One key gene is on the long arm of chromosome 4. The function of the gene product is as yet unknown. |
|
|
a man presents to you with a seemingly triangular face. On a hunch, you hit their hypothenar eminence with your reflex hammer and it causes their thumb to move towards their pinky. To confirm what you think, you have the pt squeeze your hand and tell them to open it as soon as you tell them. When you say go, their hand stays in a grip...what do they have? What is the genetics going on?
|
Myotonic Dystrophy
A gene near the centromere of chromosome 19 codes for myotonic dystrophy protein kinase. In M.D. dozens to hundreds of “CTG” repeats occur in the gene. The transcribed mRNA gets trapped within the cell’s nucleus. |
|
|
what happens in Myasthenia gravis physiologically?
(o) |
antibodies to the AChR
|
|
|
pt presents to your office with muscle weakness. They say they are fine in the morning, but by the end of the day they have drooping eyelids, jaw drop, and drooling...what do they likely have?
|
MG
|
|
|
what are some of the associated dz with MG? what is the most important one?
|
THYMOMA (malignant mediastinal tumor)
thyroid disease widespread immune complex disease |
|
|
what is a polyneuropathy
(o) |
Bilaterally symmetric
Distinct from mononeuropathy and multiple mononeuropathies so the key is that you have to have the deficit on the same spot on both sides mulitple mononeuorpathies would be like radial on one side, ulnar on the other poly is like whole left and right hand (stocking and glove is a common characteristic of polyneuopathy) |
|
|
Distal-greater-than-proximal weakness
Distal-greater-than-proximal numbness A “stocking-glove” pattern of weakness, numbness or both “Length-dependent” neuropathy Disrupts DTRs more than other forms of lower-motoneuron weakness this describes? (o) |
Polyneuropathy
the longer the axon the worse it is affected |
|
|
Werdnig-Hoffman is a motoneuron disease affecting what population?
* |
NEONATES
you will see characteristic FROG LEG position and floppy baby (other thing that causes floppy baby? Botulin toxin) BABIES WILL NOT HAVE REFLEXES |
|
|
a 60 year old man presents to your office and says that he cannot do routine tasks such as going up steps, getting out of a chair, or swallowing. You note widespread atrophy. What do you suspect...
|
Amyotrophic Lateral Sclerosis
ALS |
|
|
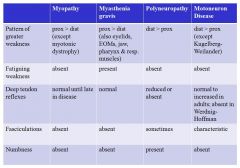
note: here is the prime example for the following
myopaty=duchenne motor neuron dz= ALS |
|
|
of the following, which will have a MARKEDLY increase CK level?
Myopathy MG Polyneuropathy Motorneuron disease |
Myopathy
(think duchenne's muscular dystrophy) |
|
|
|
|
|
. The student will be able to measure and record visual acuity according to generally agreed upon conventions
|
Eye chart for visual acuity testing. Standard distances are 20 feet for a wall chart and 14 inches for a hand-held card.
Read down to the smallest characters possible or until reaching the 20/20 line, whichever comes first. The acuity is the last line correctly read. say they read like all of the letters but miss 1 or 2 you say 20/20 minus (assuming they read at the 20 20 line) |
|
|
a cut at the optic nerve would cause what visual problem?
|
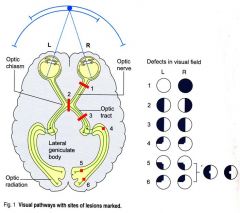
|
|
|
a cut at the optic chiasm would cause what visual problem?
|
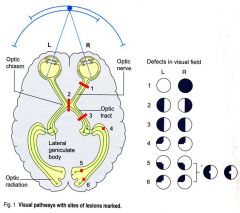
|
|
|
a cut at the right optic tract would cause what visual problem?
|
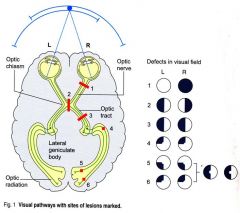
left homonomous hemianopia
|
|
|
right temporal damage could cause what visual damage?
|
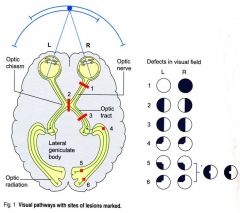
4
|
|
|
post central gyrus=?
pre=? |
post central=somatosensory
pre= motor |
|
|
please diagram the light reflex pathway...is this PNS or SNS?
|
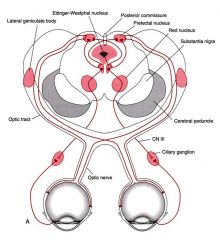
CN II
pretectal nucleus Edinger Westphal nucleus ciliary ganglion contract pupil (This is PNS) |
|
|
please diagram out the sympathetic pathway for pupilary dilation
|

ipsilateral hypothalamus
synapse at T1 (IML) travel up the sympathetic chain and to the apex of the lung (look out for horners) goes to carotid bifurcation but then sends to the pupil for dilation |
|
|
how can a tumor of the apex of the lung lead to pupil issues?
|
this is horner's syndrome due to a pancoast tumor
you will see a constricted pupil because the sympathetics (which would normally dilate the pupil) stop at the apex of the lung and are disrupted by the tumor |
|
|
pt presents with a droopy eyelid and constricted pupil...
|
ipsilateral sympathetic chain issue--HORNERS
miosis-small pupil ptosis- droppy eyelid |
|
|
please list the primary and secondary action of the extraocular muscles. consider what would happen with a lesion
|
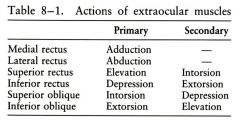
|
|
|
What do CN 6 and 4 do?
|
LR6SO4
LR (lateral rectus) connected to CN 6 SO (superior oblique) connected to CN 4 Remaining EOMs and levator palpebrae connected to CN 3 |
|
|
right lower face is weak, upper face is fine
is this an upper or lower motor neuron problem (o) |
UPPER
|
|
|
right lower face is weak, upper face is also weak
is this an upper or lower motor neuron problem (o) |
LOWER
|
|
|
The student will be able to grade muscular strength according to the MRC (Medical Research Council) scale.
(o) |
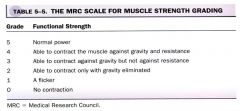
|
|
|
functions of the insular lobe
|
emotions, drives, drug addiction etc
|
|
|
just list the cranial nerves and their functions
|
* I-Olfactory nerve,
* II-Optic nerve, * III-Oculomotor nerve, * IV-Trochlear nerve/pathic nerve, * V-Trigeminal nerve/dentist nerve * VI-Abducens nerve, * VII-Facial nerve, * VIII-Vestibulocochlear nerve/Auditory nerve, * IX-Glossopharyngeal nerve, * X-Vagus nerve, * XI-Accessory nerve/Spinal accessory nerve and * XII-Hypoglossal nerve. |
|
|
Dorsal horn is associated with what?
Ventral? |
Dorsal: Sensory
Ventral Motor |
|
|
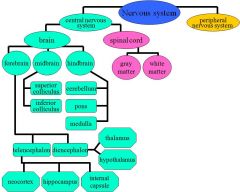
consider the locations of white and gray matter in the spinal cord and brain (which is deep and which is superficial in each)
|
spinal cord: gray matter deep
brain: gray matter superficial |
|
|
what is the difference btw the gracile and cuneate fasiculate
|
Gracile: carries axons from lower extremities
cuneate: upper (t6 and up) REMEMBER: Feet in the grass Part of the DCML pathway for sensory info (proprioception, vibration, fine touch) |
|
|
please diagram out the DCML pathway...what info does this carry?
|
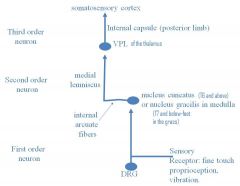
|
|
|
please diagram out the Anterior Lateral System, and list what it carries
|
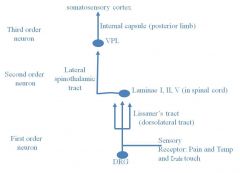
|
|
|
Please diagram out fine touch and vibration of the face
|
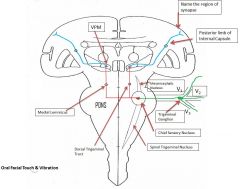
|
|
|
please diagram orofacial pain and temp
|
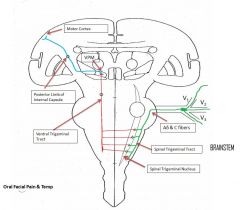
|
|
|
The left optic tract carries info from what visual field?
|
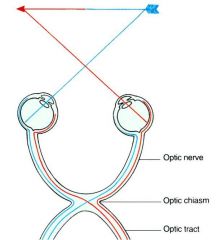
right visual field
|
|
|
where will superior visual field info end up?
|
inferior calcarine fissure
(remember they also travel inferior in the meyers loop) |
|
|
a pituitary tumor causes pressure on the optic chiasm...what will this lead to?
****TEST |
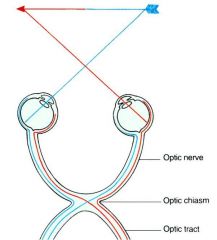
Bitemporal hemianopia
Will only be able to see info from medial visual fields (peripheral vision lost-->tunnel vision) |
|

|

|
|
|
pt falls off their bike and was not wearing a helmet. They now say that they have lost vision just in the very center of each eye...what is going on?
|
Central scotomas
|
|
|
diagram out the corticospinal and corticobulbar tracts
|
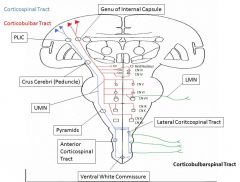
|
|
|
pt has flaccid paralysis...what is the problem
|
lower motor neuron
|
|
|
pt has spastic paralysis...what is the problem?
|
upper motor neuron
|
|
|
middle cerebral artery damage will lead to issues in what structure
|
face
comes out of sylvian fissure and branches like a tree |
|
|
anterior cerebral artery damage will lead to issues in what structure
|
legs and feet
|
|
|
describe the role of the Direct pathway and the indirect pathway in the basal ganglia
**TEST |
Direct pathway: starting movement
indirect pathway: stopping movement |
|
|
which pathway (direct or indirect) encourages GPm activity...what does this do?
|
INDIRECT
GPm has tonic inhibition of the thalamus (which is always wanting to activate movement...it's like GO GO GO) thus the indirect by activating GPm will stop movement (this is the key thing to remember) note: in the direct pathway, you inhibit GPm so inhibiting the inhibition leads to activity |
|
|
FIRST AID REVIEW QUESTION
abdominal pain radiating to the back, weight loss, migratory thrombophlebitis and obstructive jaundice should make you think what? |
Pancreatic adenocarcinoma
more common in pancreatic head aggressive (prognosis is 6 months or less) CEA and CA19-9 tumor markers assoc with Cigarettes and chronic pancreatitis but not EtOH |
|
|
FIRST AID REVIEW QUESTION
What are some of the causes of aplastic anemia? |
Radiatoin and drugs (Benzene, chloramphenicol, alkylating agents, antimetabolites)
Viral agents (B19 parvo, EBV, HIV, HCV) Fanconi's anemia Idiopathic |

