![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
(o)
|
|
|
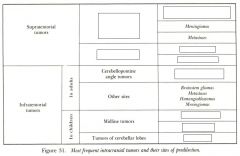
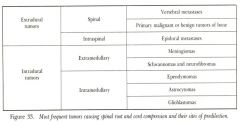
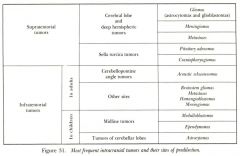
2. The student will be able to correlate brain tumors and their usual anatomic compartments.
3. The student will be able to provide examples of brain tumors that are more or less common in younger and older patients. (o) |
|
|
|
midline tumors and tumors of cerebellar lobes are more common in adults or kids?
|
kids
|
|
|
this is the Fastest-growing and most lethal brain tumor in astrocytoma series
Infiltrates and spreads widely within brain, so surgery cannot entirely remove Surgery still warranted for biopsy, with or without de-bulking and insertion of Gliadel wafer Radiation therapy usually applied * |
Glioblastoma Multiforme
|
|
|
this brain tumor is chiefly in adults 30-50, has Intermediate growth rates depending on grade, can sit dormant for years with no effect. Radiation therapy can be applied, but is usually reserved for when the tumor is perceived as growing because there is a lifetime limit to how much can be given.
|
Cerebral Astrocytomas
|
|
|
Usually the slowest growing brain tumors, but can eventually crowd the brain.
Often discovered as an incidental finding on a scan done for another reason Are usually calcified and are therefore very recognizable on CT scans. |
Meningiomas
|
|
|
please give an example that fits each of the following:
A fast-growing intracranial tumor displaces brain. A slow-growing intracranial tumor replaces brain |
A fast-growing intracranial tumor displaces brain. (Examples: glioblastoma multiforme, metastases.)
A slow-growing intracranial tumor replaces brain. (Example: typical meningioma.) |
|
|
Most frequent incidence between ages of 30 and 50
Also calcify and usually show this on CT scans. Intermediate growth rate, and is usually "managed" (surgery, RT) rather than cured Glial cell in origin |
Oligodendrogliomas
|
|
|
Can be hormonally active or disruptive
Can compress optic chiasm from below and produce visual field losses Often removed surgically through the nose and sphenoid sinus |
Pituitary Adenomas
|
|
|
Usually arise from the 8th cranial nerve as Schwannomas
Auditory symptoms (unilateral hearing loss and tinnitus) are prominent Meningiomas and other tumors can also appear in this location |
Cerebellopontine Angle Tumors
|
|
|
Comprise about 1/3 of childhood posterior fossa tumors
Predilection for cerebellar vermis Though malignant, they are highly radio-sensitive |
Medulloblastomas
|
|
|
posterior fossa tumor of childhood
Often encapsulated Complete surgical extirpation often possible |
Cerebellar Astrocytoma
|
|
|
2 of the most common primary cancers in existence are what? so what can this lead to?
(o) |
breast and Lung
can lead to brain (intermediate tenancy to go to the brain) |
|
|
The student will be able to describe more and less common sources of metastatic brain tumors.
aka what are the most and least likely to go to the brain*** (o) |
Prostate: DOES NOT go to brain
Melanoma: GOES TO BRAIN (very high propensity) |
|
|
The student will be able to describe treatments for tumors of the nervous system as well as their optimum applications and limitations. What are the options (4)
(o) |
High-dose corticosteroids
Surgery Radiation therapy Chemotherapy |
|
|
How do high dose corticosteroids help treat brain tumors?
(o) |
Buys time by shrinking the edema around the tumor deposit, rather than affecting the tumor itself.
Effective against extracellular edema, but not intracellular edema, such as that seen in ischemia. A typical starting dose is dexamethasone 10 mg, followed by 4 mg q.i.d |
|
|
how does radiation therapy help treat CNS tumors?
(o) |
RT is usually palliative--to shrink but not eliminate tumor deposits
For brain metastases, RT is sufficiently effective that the patient usually dies of non-CNS complications before CNS complications. The treatment itself can damage the CNS. |
|
|
When do you often see chemotherapy for CNS tumor treatment?
(o) |
Usually reserved for glioblastoma multiforme (Fastest-growing and most lethal brain tumor in astrocytoma series
Infiltrates and spreads widely within brain, so surgery cannot entirely remove) IV administration is complicated by intact blood-brain barrier blocking entry into CNS. BCNU (carmustine) given IV probably crosses BBB to some extent. Gliadel® wafers (also carmustine) can be implanted within the tumor bed. |

