![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
97 Cards in this Set
- Front
- Back
|
Stroke definition |
Sudden loss of neurological function caused by an interruption of the blood flow to the brain |
|
|
Stroke types |
Ischemic stroke Haemorrhagic stroke |
|
|
Ischemic stroke |
A clot blocks or impairs blood flow |
|
|
Haemorrhagic stroke |
Blood vessels rupture and leak in or around the brain |
|
|
Clinical picture of hemiplegia |
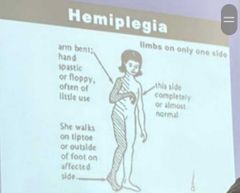
Muscular hypertonia typical patter spasticity In UL in LL |
|
|
Recovery is fastest when? |
In the first weeks after onset |
|
|
Why Recovery is fastest In the first weeks after onset? |
Due to: Reduction of edema Absorption of damaged tissue Improved circulation that allows intact neurons to regain function |
|
|
Pts can continue to make measurable gains at what rate? For how long? |
At a reduced rate for months or years after insult |
|
|
Plasticity? |
Synap plasticity may result from changes at existing synapses or from alterations in the number of functional synaptic connections |
|
|
Important indicators of movement recovery |
-initial level of motor dysfunction -time interval between paralysis and return of movement |
|
|
Subject with unilateral neglect are ... achievers at functional tasks of independence |
Poor |
|
|
It was suggested that patients with .... and .... had a negative influence on functional indepe |
Generalized poor attention and unilateral neglect |
|
|
Process of recovery is .... and characteristized by .... |
Multi-dimensional Individual variability |
|
|
The following determinants relate to a poor functional outcome |
1.sever disability on admission 2.advanced age 3. previous stroke 4. Urinary and bowel incontinence 5. Visuo-spatial deficits |
|
|
Physiotherapy management of stroke include 3 steps |
Assessment Planning Intervention |
|
|
Assessment |
|
|
|
Assessment of stroke should include |
Assessment of consciousness Physical Assessment ( equilibrium and coordination test, motor and sensory test) Cognitive assessment ( language, perception, memory) Visual assessment (field defects) Urinary impairments (urinary incontinence) |
|
|
In Planning (goal setting) , it's important to include |
Short term Medium term Long term goals |
|
|
In Planning (goal setting) the target must be |
Neither too difficult nor too easy, |
|
|
In Planning (goal setting), initially the target is ... and then change to ...., and finally .... |
-survival -recovery from impairments, getting home -returning to work and social activities |
|
|
The motor relearning model of stroke rehabilitation focus on assessing... or ... |
Motor programmer or preplanned patterns of movement |
|
|
Three main strategies underlying the motor relearning model are |
1. The elimination of unnecessary msc activity 2. Feedback of information about performance 3. Practice, |
|
|
The stroke patient needs to regain... before .... |
Trunk control before functional use of extremities can be attempted |
|
|
Currently assessment in most intervention studies is focused on ... rather than ... |
Presence or absence of certain functional tasks rather than the quality of coordination pattern |
|
|
Therapeutic technique exist for increasing msc tone in flaccid patient or inhibiting spasticity in spastic patient |
Brinnstorm approach Neurodevelopment techniques Rood techniques Functional electrical stimulation (FES) electromyography (EMS) biofeedback |
|
|
Physiotherapy for specific related problems of stroke (problem solving approach) in acute phase |
Medical attention directed at identifying and controlling stroke related problems as well as assessing individual impairments and disabilities which may lead to specific intervention: -respiratory and circulatory problems -raised intracranial pressure -dysphagia -orofacial dysfunction -ischemic heart disease -pyrexia -pressure areas -epileptic seizures -psychological problems -cognitive problems -soft tissue complications -pain of the shoulder -perceptual problems |
|
|
Basic physical therapy strategies of stroke in acute stage of recovery |
-adequate ROM bed mobility -rolling -Bridging -sitting techniques as tolerated |
|
|
Early recovery stage (flaccid stage) goals |
1.minimoze effect of tone abnormalities 2.maintain full ROM and prevent deformities 3. Improve respiratory, circulatory and oromotor activities 4.early mobility 5.promote awareness and active movement of hemiplegic side 6.improve trunk control 7.psychological support 8. Prevent respiratory, circulatory,urinary and skin complications |
|
|
Early recovery stage (flaccid stage) method |
1. Positioning and turning 2. rom exercise 3. Respiratory and circulatory exercise 4. Early mobility through: -repeated passive movements -active assisted exercises -rhythmic initiation technique |
|
|
Extroceptive and proprioceptive stimuli through reflexogenic and synergetic patterns as a bridge to functional recovery examples |
Flexor withdrawal reflex Extensor thrust Crossed extensor reflex Philipson reflex Symmetrical tonic neck reflex Asymmetrical tonic neck reflex Tonic lumbar reflex |
|
|
Associated reactions:
|
- e.g.
– Movement of one side of U.L produce the same response of contralateral side. - Movement of one side of L.L produces the opposite response of Contralateral side - Soque’s phenomena - Raimest’s phenomena. - Homolateral synkinesis |
|
|
Homolateral synkinesis
|
- Flexion of arm produces flexion of leg and extension of arm producesextension of L.L
|
|
|
Raimest’s phenomena.-
|
Resistance of abductors or adductors of L.L. produces the same response of contralateral side.
|
|
|
Soque’s phenomena:
|
Elevation of hemiplegic upper extremity produces extension and abduction of fingers
|
|
|
Weight transference technique:• All these techniques can be applied from the following Positions with the sameorder
|
1• Prone on elbow
2 • Prone on hand 3• Quadriped position 4 • Sitting 5 • Kneeling and half kneeling positions 6 • Plantigrade position 7• Standing against wall 9• Standing away from wall |
|
|
1- Faradic current → used for
|
facilitating innervated ms
|
|
|
2- Galvanic current → used to
|
facilitate denervated ms
|
|
|
Middle stage of recovery ‘’spastic stage’’Goals:
|
➢ Minimize the effect of spasticity.
➢ Maintain ROM and preventdeformities.➢ Strength weak muscles. ➢ Prevent abnormal movementsynergies. ➢ Prevent abnormal posturaladjustments ➢ Promote functional use ofhemiplegic side. ➢ Promote selective movement controlout of synergies. ➢ Improve postural control andbalance. ➢ Develop independent bed mobilityand transfer. ➢ Develop independent A.D.L. ➢ Improve cardio respiratory endurance |
|
|
position quadribed importance
|
1- Weight bearing
2- Approximation 3- Improve proximal stability 4- Improve co-ordination for patients {disk(cervical or lumbar) and hemiplegic} 5- Improve tremors + abnormal patterns of movement 6- Improve hip trunk control 7- Equilibrium / posture |
|
|
Middle stage of recovery ‘’spastic stage’’ Methods
|
1. Tone re-education procedure
2. Motor control training out of synergies : |
|
|
1. Tone re-education procedure;
Different techniques can be used for controlling spasticity either: |
1. local inhibitory techniques
2,General inhibitory techniques 3-Functional activities training 4-Positioning of patient : 5-Proprioceptive Training for upper Extremities 6- Quadruped stabilization on a balance board 7-Proprioceptive training for lower extremities 8-The dynamic proprioceptivere-education 9-Balance and control proprioceptive exercises |
|
|
local inhibitory techniques as
|
- prolonged stretch
- inhibitory pressure -low frequency vibration -prolonged icing -topical anaesthesia - iontophoresis -sensory stimulation |
|
|
General inhibitory techniques as :
|
-slow vestibular stimuli
-inverted position - neutral warmth -maintain pressure - slow stroking. -Reflex inhibiting positions of Bobath can be used successively to control andreverse abnormal patterns of movements through proximal and distal keypoints of control. |
|
|
2. Motor control training out of synergies :
|
-Start with eccentric contraction (it is easier than concentric contraction produce more tension and less metabolic costs ).
-The 2nd step is isometric contract (holding different parts of ROM). -The 3rd step is concentric contraction. |
|
|
Functional activities training
|
-Rehabilitation During late stages of recovery
-Promote skill level of motor control -Normal timing - Normal gait . -Normal manipulation of hand dexterity. -Promote normal cardiopulmonary endurance. |
|
|
Positioning of patient : Bed positions
|
:- Lying on affected side
- Lying on unaffected side -Sitting up position -Sitting in bed - Lying on back |
|
|
Proprioceptive Training for upper Extremities ;Types of exercises used for upper extremity proprioceptive training
|
1. Balance training
2.Kinetic chain exercises 3. Sport-specific maneuvers 4. PNF 5. Polymeric 6. Ballistic stretching |
|
|
Balance training
|
One major category of proprioceptive exercise is balance training These exercises help to train the proprioceptive system in a mostly static activity Activities or exercises in weight bearing using unstable supporting surface, profiteer, Swiss ,ball balance board are example of balance training in the upper extremity
|
|
|
.Kinetic chain exercises
|
Open-chain : manual resistance exercises with rhythmic are also considered ,proprioceptively enriched. In either case resistance can be modified, depending on pain, as the patient progresses stabilization
|
|
|
Quadruped stabilization on a balance board
|
-Four closed-chain exercises have been described to stimulate co-activationin the : shoulder push-ups horizontal abduction on a slide ,board andtracing circular motions on a slide board with the dominant and nondominant arms -These exercises accommodate for the individual’s tolerance to joint loads byprogressing from a quadruped to a push-up position -Wall push-ups : are also useful and can be proprioceptively enhanced byhaving a physical therapist or resistance band provide resistance to thepatient’s .back |
|
|
. Ballistic stretching
|
uses the momentum of a moving body or a limb in an attempt to force it beyond its normal range of motion This is „stretching or warming” ,”up by bouncing into or out of a stretched ,position using the stretched muscles as a spring which pulls you out of the stretched ,position .
|
|
|
Sport-specific maneuvers.
|
rehabilitation is incomplete until maneuvers specific to the sport and the athlete's position in the sport can be performed maximally and without pain .or loss of function Starting sport-specific maneuvers with weighted resistance (eg, swinging a weighted tennis racket or baseball bat), Functional positions, "such as overhead throwing, should be incorporated and are more sport-specific
|
|
|
PNF
|
Proprioceptive neuromuscular facilitation : These techniques may be definedas methods of promoting or hastening the response of the neuromuscular mechanism through stimulation of the .proprioceptors Emphasis is placed on the application of maximal resistance through out the range of ,motion using many combinations of motions in a pattern format Motion is first performed in the strongest part of the ,range with progression toward the weaker parts of the range of motion The patterns used are spiral and diagonal in character and closely resemble the movements used in sports and in occupational activities
|
|
|
Polymeric
|
-it is a quick powerful movement involving pre-stretching of a ,muscle followed by a shortening cycle
- The stretch shortening cycle occurs when elastic „loading through a quick eccentric muscular „contraction is followed by a burst of concentric muscular contraction |
|
|
. Ballistic stretching
|
it uses the momentum of a moving body or a limb in an attempt to force it beyond its normal range of motion This is „stretching or warming” ,”up by bouncing into or out of a stretched ,position using the stretched muscles as a spring which pulls you out of the stretched ,position .
|
|
|
Proprioceptive training for lower extremities
|
it improves a patient’s static and dynamic .equilibriumThe static proprioceptive re-education is begun when patients proceed toweight bearing without crutches and consists of six stages:
|
|
|
Proprioceptive training for lower extremities 6 stages
|
1. Recovery of sense of body position muscle contraction and joint
2. movement Transition from bilateral to unilateral activities 3. Transition from eyes-open to eyes-closed activities 4. Transition from activities on a stable support, such as the- ground, to unstable surfaces, such as a soft mattress, a trampoline and Freeman’s boards, or more modern equipment, such as the kinesthetic ability trainer 5. Throwing and catching a football to take the patient’s mind off active control of his balance 6. Balance recovery exercises are carried out different joint positions to evoke different responses from the tendon and muscle receptors |
|
|
The dynamic proprioceptive re-education is indicated for patients
|
needing to resume sports that involve ,running jumping, landing sudden changes of direction and twisting movements During such ,sports athletes are obviously able to lose and then regain ,balance and avoid falls and accidents that might occur by adjusting their posture so as to in a execute harmonious movements necessarily brief space of time
|
|
|
Early dynamic joint stabilization exercises : begin with |
balance training and partial weight bearing on stable ,surfaces progressing to partial weight bearing on unstable .surfaces Balancing on unstable surfaces is initiated once full weight bearing is .achieved Exercises such as “kickers” also require balance and can begin on stable ,surfaces progressing to unstable platforms
|
|
|
Eccentric loading is accomplished by activities such as
|
forward and backward stair climbing or backward downhill walking Strength and balance exercises can be combined and executed with light external forces to increase the level of difficulty
|
|
|
Plyometric activities such as low-impact hopping may commence once
|
weight bearing is achieved
|
|
|
Double-leg bounding is an effective intermediate ,exercisebecause
|
the uninvolved limb can be used for .assistance
|
|
|
why Stretch-shorteningexercises are a necessary component for conditioning the neuromuscularapparatus
|
to respond more quickly and forcefully permitting eccentric deceleration then developing explosive concentric contractions
|
|
|
The dynamic proprioceptive re-education examples
|
-tretch-shortening exercises are a necessary component for conditioning the neuromuscular apparatus -Double-leg bounding is an effective intermediate ,exercise -Plyometric activities such as low-impact hopping may commence -Eccentric loading is accomplished by activities -The dynamic proprioceptive re-education |
|
|
The dynamic proprioceptive re-education consists -:of seven stages
|
1. Slow exercises followed by quicker movement
2. Exercise with limited effort followed by exercises requiring greater strength 3. Exercises requiring volition, followed by exercises done freely 4. Progress from walking to jogging 5. Running and sprinting 6. Jumping and changes of direction 7. Twirling and twisting around the injured or operated knee |
|
|
Balance and control proprioceptive exercises
|
1. Stand on one leg2. Stand on one leg with eyes closed3. Stand on one leg – throw and catch a ball4. Stand on one leg – bend and straighten knee5. Stand on one leg- pick up item from floor6. Hold knee dip - throw and catch a ball7. Stand on one leg - move other leg to side, front and back8. .Push up onto toes (2 legs) and hold .9. Push up onto toes with eyes closed10. Push back onto heels, balance and hold .11. Push up on toes on one leg
Walking proprioceptive exercises12. Walk forward along a straight line13. Walk on tip toes along straight line14. Walk backwards along straight line15. Side step along straight line16. Walk sideways crossing one foot over other (Cariocas)17. Walk fast in one direction, quickly changing direction at intervals Running proprioceptive exercises18. Run fast in one direction19. Run backwards and do sidesteps .20. Fast crossovers (Cariocas)21. Run in figure of eight – make it smaller and smaller22. Hopping on spot23. Hop forwards and backwards – stop .24. Between hops .Hop in zigzags.25. Hop on and off step26. Do triple jump – run, hop, jump and land |
|
|
Running proprioceptive exercises
|
18. Run fast in one direction19. Run backwards and do sidesteps .20. Fast crossovers (Cariocas)21. Run in figure of eight – make it smaller and smaller22. Hopping on spot23. Hop forwards and backwards – stop .24. Between hops .Hop in zigzags.25. Hop on and off step26. Do triple jump – run, hop, jump and land
|
|
|
Walking proprioceptive exercises
|
12. Walk forward along a straight line13. Walk on tip toes along straight line14. Walk backwards along straight line15. Side step along straight line16. Walk sideways crossing one foot over other (Cariocas)17. Walk fast in one direction, quickly changing direction at intervals
|
|
|
Balance need :
|
Cerebellum
- Vestibular - Vision -Sensory -Motor |
|
|
The incidence of hemiplegic shoulder pain ranges from
|
50% to 84 %
|
|
|
Shoulder pain in hemiplegia ( post stroke), is symptom or diagnosis ?
|
, is symptom Not diagnosis
|
|
|
Management of hemiplegic shoulder pain ( HSP) Must first
|
determine the exact cause of the pain which will then direct treatment
|
|
|
hemiplegic shoulder pain Neurological deficits
|
such as sensory loss, visual field deficits,communication disorders, loss of body image, and sensory-integrativedisorders affect the prognosis for upper limb function. These deficits in combination with motor loss and abnormal muscle tonemay increase the risk of HSP
|
|
|
Soft Tissue Injury in hemiplegic shoulder pain
|
Repeated lifting, transfer and accumulated micro trauma leading to soft tissue injury (sprain & strain)
|
|
|
Glenohumeral joint misalignment
|
Initial period of flaccid paralysis in >90% of individuals Weakness ofshoulder muscles && gravitational pull tend to result in inferiorsubluxation. Weakness in am lateral rotators while lifting the arm up mayresult in missiles getting impinged between bones. Weight of unsupportedarm may cause traction on various UE nerves
|
|
|
Other general causes hemiplegic shoulder pain
|
- Adhesive capsulitis Rotator cuff rupture
-Brachial plexus and peripheral nerve -Shoulder-hand syndrome Thalamic pain. |
|
|
Shoulder Pain Indicators Poor Prognostic Indicators
|
Scapular mal-alignment (x-ray recommended)
-Passive Range Of Motion abduction <90°. Lateral rot <60° -Neglect (Hemi-neglect) - Sensory loss (thalamic syndrome) |
|
|
Management of Shoulder Pain
|
Management can be difficult and response may be unsatisfactory so prevent is key
Measures should be taken immediately following stroke to minimize the potential for the development of shoulder pain |
|
|
Prevention of Shoulder Pain BENEFICALIMPACT
|
Preventing shoulder pain may impact quality of life(mood, cognition, physical and social). Research evidence shows that earlyawareness of potential injuries to the shoulder joint structures reduced thefrequency of shoulder-hand syndrome from 27% to 8%. The shoulder-handsyndrome usually involves joint inflammation resulting from trauma, whichcoincides with increased arterial blood flow.
|
|
|
Shoulder Pain Management Joint protection strategies should be used during the early or flaccid stage ofrecovery to prevent or minimize shoulder pain. These include:
|
Positioning and supporting the arm during rest Protecting and supporting the am during functional mobility. Protecting and supporting the anm during wheelchair use by using a hemi-tray or arm trough. During the flaccid stage slings can be used to prevent injury: however, beyond the flaccid stage the use of slings remains controversial
|
|
|
Transfers Guidelines for protecting the affected arm
|
-Never pull on the affected arm.
-Avoid lifting the person from under their arms. -Do not force painful range of movements of the affected arm |
|
|
Shoulder slings :
|
Using slings only when the patient moves throughout the transfers When the patient is seated remove the sling and support the affected arm a solid structure (e lap tray, tabletop, Pillow)
|
|
|
Shoulder Pain Management
|
-Overhead pulleys and shoulder wheels should not be used
- The arm should not be moved more than 90 degrees of shoulder flexionor abduction, unless the scapula is upwardly rotated and the humerus islaterally rotated. - Patients and staff should be educated to correctly handle the involvedarm For example, excessive traction should be avoided during assistedmovements such as transfer. -sheet is recommended |
|
|
It's Your Arm!!
|
- Be your own advocate. Speak up!
-Don't let others lift under your affected arm or lift it above 90°. -Use transfer belts - Make sure you educate and tell others: (Caregivers- Family members- Friends- Health professionals _) |
|
|
Botox
|
Intramuscular Botulinum Toxin-A Reduces Hemiplegic Shoulder Pain Intramuscular injection of infraspinatus, pectoralis and subscapularis muscles
|
|
|
Kinesio tape
|
Is Strapping/Kinesiological Taping for the Painful Hemiplegic Shoulder an Effective Intervention?
|
|
|
Avoidance of Impingement During Passive Exercise
|
Exercises with flexed elbow
|
|
|
hydrotherapy |
j |
|
|
Management Strategies
|
Improper positioning in bed, lack of support when upright, and/or pulling on the hemiplegic arm when transferring, all contribute to subluxation.
|
|
|
24 Hour Arm Supports
|
-Pillows in bed and sitting
-Car transfers: tray soft lap top -Half lap trays : 1. Medial, lateral and posterior blocks 2-Different options: there is no one clear leader 3-Function needs to be considered! (Transfers / Doorway widths / Wheelchair mobility ) |
|
|
Plasticity of the nervous system
|
-fundamental for learning and relearning
-rehabilitation interventions -evolving in parallel with basic and clinical neuroscience |
|
|
mirror therapy |
h |
|
|
kinesio tape |
g |
|
|
Knee stability in hemiplegia During Flaccidity
|
: continuous overstress on posterior components of theknee joint sufficient to cause knee pain at rest and movement.
-Stasis of synovial fluid promote early degenerative changes and stimulationof pain receptors. - pressure pain mainly in side lying position -Vigorous passive movement. -Old knee O.A -Joint deformity |
|
|
Knee stability in hemiplegia During spastic stage :
|
- Assist W.B
- Over stress on ACL -Weak hamstring - Joint deformity -Pain of non-affected knee |
|
|
Knee stability in hemiplegia During spastic stage : management
|
Mobilization increased quadriceps strength and the increase persisted for30 minutes.
-Increasing knee joint mobility may remove neuromuscular inhibition on thequadriceps and thus enhance muscle strength. -Electrical stimulation - Mobilization -Kinesio taping -Strengthening ex |
|
|
general consideration |
اخر صفحتيم في لملخص |

