![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Ok again Hupka will give us some questions and we will do his objectives.....
|
let's begin
|
|
|
|
Preanesthetic medications - drugs given generally prior to anesthesia (includes drugs given during or after) in order to:
Decrease anxiety without producing excessive drowsiness Facilitate a rapid, smooth induction without prolonging emergence Provide amnesia for the perioperative period Relieve pre-and post-operative pain Minimize undesirable side effects of anesthetics (e.g. PONV) |
Common Preanesthetic Agents
Drug Class Benzodiazepine: Generic Name: Diazepam and Modazolam Common Preanesthetic Agents Drug Class: Antihistamines generic name: Hydroxyzine Desired Effect: Sedation Desired Effect: Reduce anxiety, Sedation, Amnesia, “Conscious sedation” |
|
|
|
Common Preanesthetic Agents
Drug Class: Opioid Analgesics Generic Name: Morphine, Meperidine, Fetanyl, Remifentanil Dersired Effect: Sedation to decrease tension, anxiety, and provide analgesia |
Common Preanesthetic Agents
Drug Class: Phenothiazines Generic Name: promethazine Desired Effect: Sedation, antihistaminic, antiemetic, decreased motor activity |
|
|
|
Common Preanesthetic Agents
Drug Class: Anticholinergics Generic name: atropine and glycopyrollate Desired effect: Inhibit secretions, bradycardia, vomiting, and laryngospasms |
Common Preanesthetic Agents
Drug Class: GI Drugs generic name: ondansetron , cimetidine, & metoclopramide Desired Effect: Antiemetic, Decrease gastric acidity, Decrease stomach contents |
|
|
|
Which Anticholinergic is better at crossing the BBB and causing effects: Inhibit secretions, bradycardia, vomiting, and laryngospasms:
Atropine or Glycopyrollate? EXAM***** |
Atropine
|
|
|
|
know this picture....EXAM
|
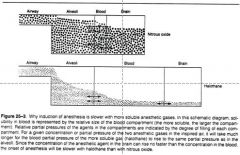
Molecules have to disolve to get to the brain.
The alveoli drug should match the brain drug Have to fill up the blood compartment. smaller compartments are easier to fill up If NOT blood soluble have faster effect |
|
|
|
Uptake, Distribution and Elimination of Anesthetic Gases
During administration of an anesthetic The concentration rises most rapidly in tissues with high blood flow (brain), and lags in tissues with lower flow (fat and muscle) Many tissues don’t reach an equilibrium status during surgery EXAM**** |
Safety, Potency, and Efficacy:
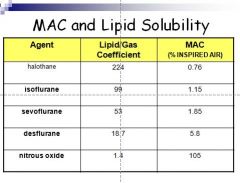
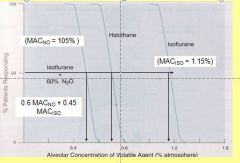
Potency: Relative potency of anesthetic gases expressed as MAC EXAM****** MAC (minimal alveolar concentration) MAC = the Minimal Alveolar Concentration that will block movement in response to incision in 50% of patients (sort of like an ED50) MAC expressed as % of inspired air MAC best correlates inversely with lipid/gas partition coefficient (the greater the lipid solubility the lower the MAC) The MAC for most inhalation anesthetics is < 2% of inspired air Relative potency = 1/MAC Smaller the MAC the more potent the anesthetic is MAC values are additive |
|
|
|
At what stage of anethesia are most surgeries done?
|
Stage 3
EXAM***** |
|
|
|
With Inhalation Anesthetic Agents
What do you need to be really careful about? EXAM**** |
General pharmacological effects
Cardiovascular: myocardial depressants |
|
|
|
With Inhalation Anesthetic Agents
What drug will NOT cause Malignant Hyperthermia? |
triggered by exposure to volatile gaseous inhalation anesthetics and succinylcholine -
N2O is not a trigger**** EXAM***** |
|
|
|
What Inhalation Anesthetic Agents drug is most likely to cause Hepatotoxicity?
|
Halothane
EXAM***** |
|
|
|
What drug's main unwanted effects is Adrenocortical suppression?
|
Etomidate
EXAM**** |
|
|
|
What Intravenous Anesthetic Agents can be used as a Antiemetic (An antiemetic is a drug that is effective against vomiting and nausea.)
|
Propofol
EXAM**** |
|
|
|
what Intravenous Anesthetic Agents main unwanted effects are Psychotomimetic effects following recovery?
|
Ketamine
EXAM***** |
|
|
|
What Intravenous Anesthetic Agent produces good analgesia and amnesia. Also causes Bronchodilation?
|
Ketamine
EXAM***** |
|
|
|
What Intravenous Anesthetic Agents Is good for Amnesia?
|
Midazolam
EXAM***** |
|
|
|
IV anesthetic drug mechanisms:
What drug primarily produces its effects by binding non-competively to the NMDA receptor site to inhibit the excitatory NT glutamate |
Ketamine = glutamate antagonist
EXAM***** |
|
|
|
How do IV anesthetic drugs thiopental, midazolam, propofol, etomidate work?
|
thiopental, midazolam, propofol, etomidate
primarily produce their anesthetic effects by enhancing the efficacy of GABA at GABAA chloride ionophore EXAM***** |
|
|
|
What drug causes:
Causes a direct cerebral vasoconstriction that results in decrease CBF and CMRO2 and as a result an elevated ICP is lowered |
Etomidate
EXAM**** |
|
|
|
What drug will you see Myoclonic movements are common is association with induction and emergence?
|
Etomidate
EXAM***** |
|
|
|
What drug has Good amnesic properties and is Often combined with opioid for ‘conscious sedation’
Availability of specific receptor antagonist = flumazenil |
Midazolam
EXAM***** |
|
|
|
1. Explain what is meant by MAC, indicate its significance, and the physical characteristic it best correlates with
|
Relative potency of anesthetic gases expressed as MAC
MAC (minimal alveolar concentration) MAC = the Minimal Alveolar Concentration that will block movement in response to incision in 50% of patients (sort of like an ED50) MAC expressed as % of inspired air |
|
|
|
MAC best correlates inversely with lipid/gas partition coefficient
(the greater the lipid solubility the lower the MAC) The MAC for most inhalation anesthetics is < 2% of inspired air |
Relative potency = 1/MAC
Smaller the MAC the more potent the anesthetic is MAC values are additive |
|
|
|
Image of MAC and Lipid Solubility
|
|
|
|
|
Combining agents to reduce the MAC of each
|
|
|
|
|
What are some factors that may increase MAC?
|
Hyperthermia
Hypernatremia Hyperthyroidism Chronic alcohol abuse Increased CNS norepinephrine levels (MAO inhibitors, cocaine, ephedrine, acute amphetamine intoxication) |
|
|
|
Some factors that decrease MAC
|
Increasing age
Metabolic acidosis Certain Drugs Hypothermia Hypotension Hyponatremia |
|
|
|
2. Indicate which of the inhalation anesthetics has significant analgesic properties
|
Anesthetic gases – only one is Nitrous Oxide which has good analgesic properties (others don’t)
|
|
|
|
3. Explain induction and recovery times and potency based upon physical properties of general anesthetics.
|
speed of induction and emergence (recovery)
determined by the rate of change of the partial pressure (concentration) of the gas in the brain Speed of induction best correlated with blood/gas partition coefficient (inverse correlation) determined by the partial pressure of the gas in arterial blood which is related to alveolar concentration So concentration in brain related to alveolar concentration |
|
|
|
Uptake, Distribution and Elimination of Anesthetic Gases
Image |
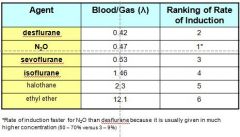
Rate of induction faster for N2O than desflurane because it is usually given in much higher concentration (50 – 70% versus 3 – 9%)
|
|
|
|
Summary:
During administration of an anesthetic: its concentration in blood rises toward that in the inspired gas Tissue concentrations rise to approach the concentration in the arterial blood |
The concentration rises most rapidly in tissues with high blood flow (brain), and lags in tissues with lower flow (fat and muscle)
Many tissues don’t reach an equilibrium status during surgery |
|
|
|
4. Describe the proposed mechanism(s) of action of inhalation anesthetics
|
don't know how they work
Anesthesia probably has no unitary mechanism but may involve Sufficient enhancement of inhibition Inhibition of excitation A combination of the two |
|
|
|
The GABAA receptor complex seems to be the primary target for most of GA and many IV anesthetics
They may act indirectly to enhance GABA’s effect to increase chloride conductance at lower concentrations Act directly as agonists to open the chloride channel |
Inhalation anesthetic
Primary agents used today: Nitrous oxide (N2O)* Sevoflurane** |
|
|
|
Theories of Anesthetic Action:
GABAA-Chloride channel complex (GABAA ) Common specific target for Anxiolytics hypnotics general and IV anesthetics, antiepileptics |
All don’t fit the mechanism
Spinal glycine receptors targets for some GA effects Actions to increase chloride conductance to produce hyperpolarization Ketamine and nitrous oxide seem to act by inhibiting glutamate NMDA receptors or central acetylcholine receptors |
|
|
|
5. Indicate the physiological indices for "surgical" anesthesia (Stage III plane 3) and anesthetic overdose (Stage IV).
|
Depth of Anesthesia
Signs and stages of anesthesia originally developed for diethyl ether Stage III: Used for most Sx Pupillary light reflex present no eye movement still breathing No response to skin incision Stage IV: Imminent death Apnea appears Pupil is completely dialated muscle tone is flaccid |
|
|
|
6. Compare and contrast the pharmacological properties, and uses of etomidate, ketamine, propofol and midazolam. Consider mechanisms, induction and recovery, as well as potential adverse effects
|
etomidate:
Fast onset, fairly fast recovery Excitatory effects during induction and recovery, Adrenocortical suppression No significant effects on cardiovascular and respiratory system. Injection site pain Propofol Fast onset, very fast recovery Cardiovascular and respiratory depression. Pain at injection site Most common induction agent. Rapidly metabolized; possible to use as continuous infusion. Injection pain. Antiemetic |
|
|
|
Ketamine
Slow onset, after-effects common during recovery Psychotomimetic effects following recovery, Postoperative nausea, vomiting and salivation Produces good analgesia and amnesia. Bronchodilation. Increased HR, BP, CO. No injection site pain |
Midazolam
Slower onset than other agents Minimal CV and resp effects Little respiratory or cardiovascular depression. No injection pain. Good amnesia. |
|
|
|
Etomidate.....most likely to cause PONV
Also.......... Myoclonic movements are common is association with induction and emergence |
7. Explain the concept of balanced anesthesia
Combination or balanced anesthesia no single anesthetic agent meets the ideal so, a combination of drugs is used to take advantage of their best properties minimize the undesirable side effects |
|
|
|
8. Define "dissociative" anesthesia and name the drug used to produce it.
|
Dissociative – ketamine
Produces a ‘dissociative anesthesia’ Chemically related to PCP Analgesia, immobility, amnesia No loss of consciousness but like in a trance with eyes open and cataleptic Patient may appear to be awake but does not respond to sensory stimuli Used for minor surgical and diagnostic procedures especially in children |
|
|
|
Ketamine
Almost no respiratory depression with significant bronchodilation properties Unique =unlike other IV anesthetic drugs stimulates CV system Unlike other anesthetic agents can be given by IM route (useful for anesthetizing children who resist IV or inhalation) |
9. Compare isoflurane, desflurane, and sevoflurane in respect to: recovery time, extent of metabolism, heart rate, and respiratory irritation. Which agents are most likely to produce emergence delirium in children?
isoflurane (Forane) – commonly used anesthetic for adults, inexpensive, pungent odor, inexpensive |
|
|
|
desflurane (Suprane) – similar to isoflurane except for more rapid emergence, and more irritating to airway, expensive
|
sevoflurane (Ultane) – similar to desflurane except not irritating to airway, one of the best!! Expensive!
Isoflurane: recovery time,- moderate extent of metabolism, - 0.2% heart rate,- increased respiratory irritation - significant |
|
|
|
Desflurane
recovery time - very fast extent of metabolism, - 0.02& heart rate,- increased respiratory irritation - significant |
Sevoflurane
recovery time, - FAST extent of metabolism, - 3-6% heart rate, - Stable Ketamine........... Delirium, hallucinations, vivid dreams and irrational behavior during recovery (emergence delirium) respiratory irritation - NO |
|
|
|
10. Know which substance of abuse ketamine is related to.
|
Chemically related to PCP
|
|
|
|
11. Explain what is meant by "induction anesthesia" and name the IV agents primarily used for this procedure
|
Propofol
Most frequently used induction agent Good induction and maintenance agent Rapid onset of action and short recovery time Possesses antiemetic properties |
|
|
|
12. Explain the mechanism behind propofol’s brief duration of CNS effects following IV bolus administration
Propofol Short recovery time attributed to redistribution and rapid clearance from plasma by metabolism (mainly glucuronidation) little hangover Considered safe for use in pregnant women Propofol and opioids thought to act synergistically |
13. Explain why in spite of the fact that the general inhalation anesthetics have a low Therapeutic Index they still can be safely used to produce anesthesia.
Therapeutic indices (TI) for most general anesthetics is among the lowest of drugs (2- 4) accurate control of dosage is necessary for safe use |
|
|
|
14. Explain what is meant by "incomplete anesthetic", indicate which anesthetic gas is considered and incomplete anesthetic.
|
Nitrous oxide is an incomplete anesthetic
it can’t produce all stages of anesthesia without producing hypoxia (MAC = 105) N2O has less efficacy than a complete anesthetic |
|
|
|
15. Compare propofol, etomidate, and ketamine for their effects on systemic blood pressure and heart rate.
|
propofol, - decrease systemic BP, Decrease HR
etomidate, - No change in systemic BP, No change in HR ketamine - Increase in systemic BP, increase in HR |
|
|
|
16. Describe the use of pre anesthetic medications. Be able to list the most commonly used agents and their desired effects
|
See earlier
|
|
|
|
17. Describe malignant hyperthermia and relate it to general anesthetics. Indicate which of the neuromuscular blocking agents is also capable of triggering this adverse effect. Indicate the drug most frequently used to manage MH. Indicate which inhalation anesthetic does not trigger MH.
|
Malignant Hyperthermia (MH):
Rare life-threatening emergency condition Management involves: IV administration of dantroline discontinuation of triggering agents supportive treatment must be instituted quickly triggered by exposure to volatile gaseous inhalation anesthetics and succinylcholine - N2O is not a trigger Signs and symptoms usually develop in an hour after exposure and include hyperthermia (110+ degrees) muscle rigidity metabolic acidosis |
|
|
|
All drugs can cause MH
|
18. Explain what is meant by ‘irregularly descending anesthesia’ and the importance of this concept.
General pharmacological effects CNS: dose - dependent depression of all portions of CNS Order of sensitivity (most to least) is RAS and cortex → hippocampus → basal ganglia → cerebellum → spinal cord → medulla (irregularly descending anesthesia) |
|
|
|
19. Indicate for which of the IV anesthetics flumazenil would be most useful to recover from overdosage
|
Midazolam
|
|
|
|
20. Indicate the pros and cons of the inhalation anesthetics isoflurane, desflurane, sevoflurane, and N2O.
|
Isoflurane:
Pros: Inexpensive Little metabolism No significant systemic tox Maintains CO because of vasodilation Con: Pungent odor Airway irritant Trigger of MH Desflurane Pros:Fast uptake and eliminate Stable molecules Little metabolism No significant systemic tox Cons: airway irritant Sympathetic stimulant Expensive Rapid increase in inspired conc may trigger tachycardia and hypertension Trigger of MH |
|
|
|
sevoflurane
Pros: Fast uptake and eliminate Nonpungent Good for inhalation induction CV effects similar to isoflurane Cons:3 – 5% metabolized but no hepatic or renal tox Reacts with soda lime Increases serum fluoride conc Expensive Trigger of MH |
N2O
Pros: Analgesic Fast uptake Fast eliminate Nonpungent Little CV or respiratory depression Cons: High conc. Required Teratogenic Diffusion hypoxia Expands into closed air spaces |
|
|
|
21. Given blood/gas partition coefficients, lipid/gas partition coefficients indicate which anesthetic is most likely to induce anesthesia most rapidly and which is most potent.
|
Smaller the MAC the more potent the anesthetic is
Most Potent: halothane Most Rapid: N20 speed of induction and emergence (recovery) determined by the rate of change of the partial pressure (concentration) of the gas in the brain determined by the partial pressure of the gas in arterial blood which is related to alveolar concentration So concentration in brain related to alveolar concentration Speed of induction best correlated with blood/gas partition coefficient (inverse correlation) |
|
|
|
22. Dexmedetomidine is an IV agent that has a unique mechanism of action. Indicate that mechanism of action and indicate some of the unique properties of this agent as compared to propofol and ketamine
|
Dexmedetomidine:
Central acting α2 agonist Profound sedation with anxiolytic and analgesic properties Slower onset and longer acting than midazolam and propofol Minimal respiratory depression but has potential for bradycardia and hypotension Changes in respiration similar to those observed during natural sleep Wake up with clear clear consciousness Decreases propofol, opioid, inhalation anesthetic dose requirements |
|

